Abstract
Huntingtin, the protein that when mutated causes Huntington disease (HD), has many known interactors and participates in diverse cellular functions. Mutant Htt (mHtt) engages in a variety of aberrant interactions that lead to pathological gain of toxic functions as well as loss of normal functions. The broad symptomatology of HD, including diminished voluntary motor control, cognitive decline, and psychiatric disturbances, reflects the multifaceted neuropathology. Although currently available therapies for HD focus on symptom management, the autosomal dominant cause and the adult onset make this disease an ideal candidate for genetic intervention. A variety of gene therapy approaches have been tested in mouse models of HD, ranging from those aimed at ameliorating downstream pathology or replacing lost neuronal populations to more upstream strategies to reduce mHtt levels. Here the authors review the results of these preclinical trials.
Keywords: autophagy, intrabody, neurotrophin, RNAi, silencing, viral vector
Huntington disease (HD) is caused by the expansion of a polyglutamine (polyQ) tract in exon 1 of the multifunctional protein Htt. Affected individuals have more than 36 glutamine repeats, and longer polyQ tracts correlate with earlier onset and increased disease severity (Huntington’s Disease Collaborative Research Group 1993). Expanded polyQ Htt induces degeneration and eventual loss of susceptible neuronal populations in the striatum and cortex. Chief among these are striatal medium spiny neurons (MSNs), whose population undergoes an early and severe loss. The deficit in neurons and their processes results in a dramatic atrophy of the putamen and caudate nucleus, as well as cortical thinning (Rosas and others 2008). HD usually presents in midlife with chorea, dementia, and weight loss, with death typically occurring 15 to 20 years after symptom onset (Walker 2007). Although the appearance of gross motor deficits or dementia is commonly referred to as disease onset, carriers of expanded polyQ in HD can display psychiatric symptoms such as anxiety, depression and obsessive compulsive disorder, mild cognitive impairments of episodic memory and executive function, and fine motor deficits years to decades before defined clinical onset (Biglan and others 2009; Duff and others 2007). Elevated levels of proinflammatory cytokines are also present in serum at least 16 years prior to motor symptom onset, reflecting the role of inflammation in this disease (Bjorkqvist and others 2008).
The simple genetic nature and autosomal dominant transmission of HD should facilitate therapy development. Unlike multicause, predominately idiopathic neurodegenerative diseases such as Alzheimer and Parkinson diseases, identification of premanifest mutation carriers and thus presymptomatic treatment initiation is possible for HD. This allows for neuroprotective strategies rather than more complicated restorative methods or techniques for coping with existing neuronal loss. Nonetheless, the therapies currently available to HD patients, which include selective serotonin reuptake inhibitors (SSRIs) and atypical antipsychotics for psychiatric disturbances and tetrabenazine for chorea, offer only moderate symptom relief and have no effect on disease progression (De Marchi and others 2001; Huntington Study Group 2006).
In striking contrast to the simplicity of HD genetics, the convoluted disease mechanisms in this disorder have hindered development of disease-modifying therapies. The Htt protein is a large, promiscuous protein that is known to associate with many molecular partners, including proteins, DNA, and mRNA, as well as cellular components that include the endoplasmic reticulum (ER), mitochondria, microtubules, the plasma membrane, and endocytic, synaptic, and autophagic vesicles (Imarisio and others 2008). Wild-type Htt (wtHtt) is a jack of all trades, playing roles in numerous, seemingly unrelated processes that include transcriptional regulation, apoptosis suppression, ER stress signaling, calcium homeostasis, axonal transport, endocytosis, and synaptic transmission (Zuccato and others 2010). In HD, mHtt fails to adequately perform these essential roles and also acquires toxic functions related to accumulation, aggregation, and sequestration of essential proteins, as well as aberrant interactions. This combination of loss and gain of function creates a network of cellular dysfunction that leads to impaired proteolysis, transcriptional regulation, intracellular trafficking, mitochondrial metabolism, calcium signaling, and synaptic activity (Imarisio and others 2008; Ramaswamy, Shannon, and others 2007). Consequently, there is a wide variety of potential HD therapeutic targets—from the mHtt protein itself to myriad downstream factors, many of which have been evaluated for gene therapy efficacy in mouse models of HD.
Downstream Targets
Neurotrophic Factor Delivery
Neurotrophic factors are secreted growth factors that can enhance differentiation, function, and survival of neurons. Ectopic expression of neurotrophic factors mediated either by viral vectors or the transplantation of genetically modified cells has shown some promise in the treatment of mouse models of HD.
Nerve growth factor (NGF) is the prototypical neurotrophin that not only promotes neuronal survival but can also down-regulate Htt expression in cultured striatal neurons (Haque and Isacson 2000). NGF delivery by transplantation of transfected neural stem cells (NSCs) is neuroprotective when administered prior to injection of quinolinic acid (QA), an N-methyl-d-aspartate (NMDA) receptor agonist that induces excitotoxicity and neuropathology similar to that found in HD (Martinez-Serrano and Bjorklund 1996). Transplantation of mesenchymal stem cells (MSCs) genetically engineered to overexpress NGF into the striatum of four-month-old YAC128 mice (a transgenic model expressing full-length mHtt) results in moderate improvements in rotarod and clasping behavior but no increase in striatal neuron number or expression of dopamine and cyclic-AMP-regulated phosphoprotein (DARPP-32), a marker of healthy MSNs (Dey and others 2010).
Brain-derived neurotrophic factor (BDNF), which is required for differentiation and survival of striatal MSNs, is reduced in the human HD striatum. Expression of BDNF is activated by wtHtt, a function that is lost with polyQ expansion (Zuccato and Cattaneo 2007). Viral delivery of BDNF to the striatum of rats prior to injection of QA is neuroprotective, resulting in reduced cell loss and lesion volume (Bemelmans and others 1999; Kells and others 2004). Astrocytes cultured from transgenic mice expressing BDNF driven by the glial fibrillary acid protein (GFAP), astrocyte-specific promoter, increase their BDNF production in response to inflammatory insults. When grafted into the striatum of nude mice one week or one month before QA injection, these cells produce excess BDNF, which reduces lesion volume and prevents neuronal death, as measured by NeuN, a marker of neuronal nuclei. This neuroprotection is selective, resulting in increased DARPP-32-positive MSNs and parvalbumin-positive but not choline acetyltransferase–positive interneurons. In addition, BDNF-expressing astrocyte grafts in unilaterally lesioned animals decrease apomorphine-induced rotation, indicating that function is preserved in the protected neurons (Giralt and others 2010). The beneficial effects of ectopic BDNF expression have also been demonstrated in the YAC128 transgenic model of HD. In four-month-old mice, striatal injection of MSCs harvested from mouse femurs and transfected to produce BDNF results in improved clasping and rotarod performance. At 13 months of age, BDNF-MSC-grafted mice have displayed more NeuN- and DARPP-32-positive striatal neurons than unmodified MSC-grafted or vehicle-injected mice, illustrating the long-term benefit of this treatment (Dey and others 2010).
Cilliary neurotrophic factor (CNTF), a member of the interleukin (IL)–6 or neuropoietic cytokine family, promotes the survival of a broad range of neuronal types, including those most susceptible to mHtt-induced toxicity (Ip and Yancopoulos 1996). Although neuroprotective in QA rat models of HD (De Almeida and others 2001; Emerich and others 1996; Régulier and others 2002), CNTF has shown no benefit and, in some cases, a detriment in HD transgenic mice. Lentiviral delivery of CNTF into YAC72 mice results in excellent striatal expression for up to one year following surgery. Although no exacerbation of behavioral deficits is found in treated animals, reduced DARPP-32 expression and NeuN-positive cells as well as increased GFAP expression are seen in the striatum of both wild-type and YAC72-treated mice (Zala and others 2004). Moreover, adeno-associated virus (AAV) delivery of CNTF into the striatum of 10-week-old R6/1 mice results in earlier onset of rotarod deficits. In addition, this treatment increases body weight loss and reduces expression of striatally enriched genes such as DARPP-32 and preproenkephalin in both transgenic and wild-type mice (Denovan-Wright and others 2008). These studies indicate that long-term overexpression of CNTF is not well tolerated, and therefore this neurotrophic factor is not a good candidate for gene therapy in HD.
Glial cell line–derived neurotrophic factor (GDNF) is produced in the developing striatum and is expressed by adult striatal projection neurons as well as interneurons (Pérez-Navarro and others 2000). Viral- and cell-mediated delivery of GDNF prior to QA injection is neuroprotective in rats (Kells and others 2004; Pérez-Navarro and others 1999; Pérez-Navarro and others 1996). Transplantation of NSCs transfected to produce GDNF protects against QA toxicity in nude mice, resulting in moderately reduced loss of NeuN-positive striatal neurons and reduced amphetamine-induced rotation (Pineda and others 2006). When given after symptom onset, lentiviral delivery of GDNF to four- to five-week-old R6/2 mice has no effect on rotarod, clasping, or open field behavior. Intranuclear inclusions, BrdU staining, and neuronal cross-sectional area are also unaffected in these animals (Popovic and others 2005). However, presymptomatic AAV-GDNF delivery to five-week-old N171-82Q transgenic mice significantly delays onset of clasping and rotarod deficits. At 16 weeks of age, compared with untreated mice, the striata of treated mice have decreased inclusions and increased neuronal number with larger cross-sectional areas, although striatal volume loss is not improved (McBride and others 2006). Moreover, transplantation of GDNF-secreting mouse neural progenitor cells (NPCs) into 60-day-old N171-82Q mice following symptom onset results in delayed body weight loss and dramatic improvement in rotarod performance. GDNF-NPC transplantation also results in reduced inclusions and increased NeuN-positive cells in the striatum but no improvement in cortical thinning. Although some loss of tyrosine hydroxylase is seen in areas proximal to the graft, no loss of dopaminergic neurons is observed (Ebert and others 2010). Thus, GDNF can be a restorative as well as a preventative treatment.
Neuturin (Ntn), a member of the GDNF family, promotes survival of projection neurons that mediate hypo-kinetic movement, making it a logical candidate for the treatment of HD, a disease characterized by hyperkinetic movement (Alberch and others 2002). Cell-mediated delivery of Ntn protects projection neurons but not interneurons in QA-lesioned rat striata, which is the opposite effect seen with GDNF overexpression (Pérez-Navarro and others 2000). This indicates that although these neurotrophins share expression patterns and receptor family members, they have differential mechanisms of action. As MSNs, the most susceptible neurons in HD, are projection neurons, Ntn may be more suitable for HD gene therapy than GDNF. Viral-mediated delivery of Ntn into rats treated with the mitochondrial toxin 3-NP is neuroprotective and ameliorates motor deficits (Ramaswamy, McBride, and others 2007). AAV delivery of Ntn to the striatum of six-week-old N171-82Q mice results in increased stride length and delayed rotarod deficits and clasping compared to AAV-GFP- or vehicle-treated transgenic mice. Treatment with AAV-Ntn dramatically increases striatal neuron as well as layer 5 and 6 cortical neuron numbers. This therapy, however, has no effect on neuronal cross-sectional area, inclusion deposition, or mouse survival (Ramaswamy and others 2008). Interestingly, inclusion deposition and neuronal cross-sectional area are measures that are improved by GDNF treatment, indicating that there may be increased benefit of combining these very promising neurotrophic factor gene therapies.
Activation of Endogenous Neural Stem Cells
One approach to coping with neuronal loss is the activation of endogenous NSCs in the adult brain. One site of NSCs throughout life is within the subventricular zone (Taupin and Gage 2002). Delivery of adenoviral-BDNF (AdB) into the subventricular zone results in increased NSC proliferation and migration of newly formed cells into the striatum, although the majority of these cells differentiate into glia. Coexpression of noggin, an inhibitor of gliogenesis, pushes these newly generated cells toward a neuronal fate. Intraventricular delivery of BDNF and noggin (AdB/N) into R6/2 mice increases neurogenesis, leading to recruitment of new striatal MSNs, which project axons to their targets. AdB/N gene therapy also results in improved rotarod performance and increased spontaneous activity as well as a 17% increase in survival time (Cho and others 2007). It is remarkable that the new neurons “know where to go and what to do when they get there.” Because BDNF can stimulate the generation of several other types of neurons, it seems that the local environment in the damaged striatum contains the cues necessary for MSN differentiation.
Normalization of Calcium Signaling and Mitochondrial Function
Mitochondrial dysfunction in HD, which includes altered respiration, membrane potential, and metabolism, leads to disruption of calcium homeostasis, excess production of reactive oxygen species, and excitotoxicity (Damiano and others 2010). One of the ways that the mHtt protein induces energy dysregulation is by repressing transcription of PGC-1α, a regulator of mitochondrial metabolism. Lentiviral delivery of PGC-1α into the striatum of R6/2 mice completely prevents loss of individual neuronal volumes, supporting mitochondrial involvement in HD-related neurodegeneration (Cui and others 2006). Mitochondria from HD patient–derived lymphocytes display reduced calcium-buffering capacity, leading to excess cytosolic calcium (Panov and others 2002). This causes excitotoxicity and aberrant calcium signaling. Calmodulin (CaM), a regulatory protein that associates with mHtt, activates a number of enzymes upon calcium binding. Among these is transglutaminase, an enzyme that catalyzes covalent cross-linking of glutamine residues and possibly contributes to mHtt-induced toxicity. Intrastriatal, AAV-mediated delivery of a CaM fragment to R6/2 mice disrupts mHtt-CaM interaction, leading to a reduction in the level of transglutaminase-modified mHtt. AAV-CaM gene therapy also improves rotarod performance, gait, and hypoactivity, as well as deposition of inclusions and loss of neuronal size and body weight, although mouse survival is unaffected (Dai and others 2009). It will be of interest to determine the effects of this form of gene therapy in full-length models of HD.
Targeting mHtt
Increased Clearance
Considering the multiplicity of pathogenic mechanisms of HD, a more comprehensive, upstream therapeutic approach is to reduce mHtt protein levels by increasing its degradation. Removal of mHtt is less likely to have deleterious off-target effects and more likely to ameliorate all aspects of the HD phenotype than are therapies directed at downstream dysfunctions. Interventions that selectively reduce levels of mHtt while sparing the wt protein are preferable because long-term reduction of wtHtt may not be well tolerated. As mentioned at the outset, wtHtt protein is important for neuronal health throughout life, and mice with wtHtt conditionally knocked out in adulthood develop progressive motor impairment and neuropathology (Dragatsis and others 2000). Small-molecule-mediated increases in mHtt clearance have been unsuccessful thus far, ostensibly because of the elaborate and somewhat mysterious mechanisms of endogenous mHtt degradation. On the other hand, gene therapy approaches to selectively increase mHtt clearance have shown considerable promise.
One such approach uses viral-mediated delivery of intrabodies (iAbs), which are intracellularly expressed Ab fragments that recognize and bind Htt in living cells. Several anti-Htt iAbs have been developed as potential therapeutics, and the most promising of these reduce mHtt-induced toxicity by promoting its degradation. EM48 is an iAb that recognizes an epitope in the C-terminus of HDx1. Although this epitope is common to mutant and wtHtt, EM48 preferentially binds mHtt on Western blots, possibly because of polyQ expansion–induced conformational changes. Observations in a cellular model of HD reveal that EM48 binding increases the ubiquitination and subsequent degradation of mHtt. Intrastriatal Ad delivery of this iAb into R6/2 and N171-82Q mouse models results in increased Htt cleavage and reduced neuropil aggregates, demonstrating in vivo efficacy of EM48-enhanced mHtt degradation. EM48-treated N171-82Q mice also display improved gait and rotarod performance. However, EM48 gene therapy does not prevent loss of body weight or enhance the survival of these animals (Wang C-E and others 2008).
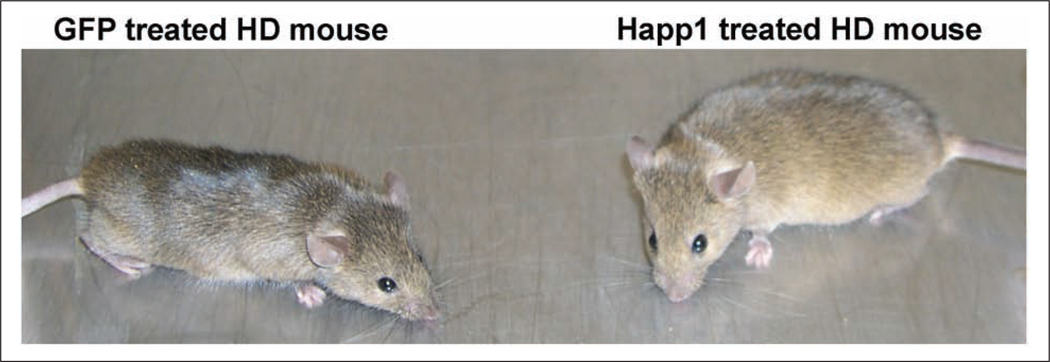
Another iAb, Happ1, binds the proline-rich region of Htt adjacent to the polyQ tract. Despite its recognition of wtHtt under denaturing conditions, Happ1 binding selectively increases the turnover of mutant but not wtHtt in cellular models of HD (Southwell and others 2008). This iAb-induced turnover involves enhanced calpain cleavage of mHtt (Southwell and others 2011). The target epitope of Happ1 is the site of multiple endogenous protein-protein interactions, which are enhanced by polyQ expansion, suggesting increased epitope availability in the context of mHtt (Passani and others 2000; Qin and others 2004; Steffan and others 2000). This is likely to be responsible for the selectivity of Happ1 action under native conditions. Intrastriatal AAV delivery of Happ1 is beneficial in five different mouse models of HD. In a unilateral, acute lentiviral-mHtt mouse model, Happ1 treatment prevents the amphetamine-induced rotation phenotype and reduces striatal lesion size and intensity as well as mHtt aggregation. In genetic HD models, Happ1 treatment improves rotarod and beam-crossing performance of R6/2, N171-82Q, YAC128, and BACHD mice and spontaneous climbing in YAC128 and BACHD mice. Happ1 treatment also normalizes open-field exploration in YAC128 and BACHD mice and object learning in YAC128 mice, demonstrating benefit in the psychiatric and cognitive dimensions of the HD-like phenotype. An object learning deficit in BACHD mice is unchanged by Happ1 treatment, however. Happ1 treatment also improves neuropathological measures, including ventricular enlargement in R6/2, YAC128, and BACHD mice and inclusion load in R6/2. Importantly, Happ1 gene therapy increases body weight and increases life span by 30% in the N171-82Q model (Fig. 1), although there is no benefit of Happ1 treatment in these outcomes in the more severe and earlier onset R6/2 model (Southwell and others 2009).
Figure 1.
Happ1 gene therapy improves body weight of N171-82Q Huntington disease (HD) model mice. The green fluorescent protein (GFP)–treated N171-82Q mouse (left) displays reduced body weight, hunched posture, and piloerection (ruffled coat), whereas the Happ1-treated N171-82Q mouse (right) displays normal body weight and appearance. The mice shown are male littermates.
The ability of anti-Htt iAbs to increase clearance of mHtt and subsequent therapeutic benefit can be improved by fusion to targeting sequences, which direct the degradation of the bound Htt-iAb complex. The iAb C4, which recognizes the N-terminus of HDx-1, reduces mHtt-induced toxicity and aggregation in cell culture, brain slice, and fly models of HD (Lecerf and others 2001; Murphy and Messer 2004; Wolfgang and others 2005), but AAV-mediated C4 gene therapy in R6/1 HD model mice confers only modest phenotypic benefit (Snyder-Keller, McLear and others 2010). A fusion protein of this iAb and a PEST signal sequence, a peptide rich in proline, glutamic acid, serine, and threonine, efficiently targets mHtt for proteasomal degradation. C4-PEST significantly reduces levels of both soluble and insoluble mHtt in cotransfected cultured striatal cells (Snyder-Keller, Butler and others 2010). It will be interesting to see how this modification affects C4 gene therapy efficacy in HD mice.
A different strategy for reducing mHtt levels involves induction of autophagy. Autophagy is a lysosomal degradation process for long-lived and misfolded cytoplasmic proteins that can selectively degrade mHtt (Sarkar and Rubinsztein 2008). Chemical induction of autophagy results in accelerated clearance of mHtt and subsequent therapeutic benefit in fly and mouse HD models (Ravikumar and others 2004; Rose and others 2010; Sarkar and others 2008). Drug-mediated global induction of autophagy, however, is not specific to Htt and could potentially have off-target effects, particularly over the extremely long treatment duration required for HD therapy. The lack of understanding of the regulation of endogenous, autophagy-mediated mHtt degradation hampers selective drug development, and therefore there is interest in gene therapy approaches. Specific targeting of mHtt for autophagic degradation has been demonstrated in the R6/2 mouse model by intrastriatal AAV-mediated delivery of an expanded polyQ binding peptide (QBP1), which binds mutant but not wtHtt. This peptide is fused to a synthetic HSC70 chaperone-binding motif (HSC70bm), which targets bound proteins to lysosomes for degradation. Artificial, chaperone-mediated, autophagic degradation of mHtt in these animals results in reduced levels of both aggregated and soluble mHtt protein in brain lysates and inclusions in transduced striata. QBP1-HSC70bm gene therapy improves clasping and rotarod performance and reduces striatal atrophy. This promising therapy also improves body weight and dramatically increases the survival of this very severe model (Bauer and others 2010). One would like to see this approach tested in a full-length mHtt model.
Silencing
The most upstream and direct strategy for the treatment of HD is silencing expression of mHtt mRNA, thus preventing generation of the toxic protein and all subsequent pathology. At least 10 RNAi gene therapy efficacy preclinical trials have been performed since 2005, using a variety of rodent models of HD. These studies, recently reviewed by Harper (2009), are briefly summarized here.
Intrastriatal AAV delivery of a short hairpin RNA (shRNA), HDsh2.1, in N171-82Q mice results in reduced inclusions and improved rotarod performance and gait but no change in loss of body weight (Harper and others 2005). Another shRNA, siHUNT-1, which targets the 5′UTR of Htt, delivered by AAV into the striatum of R6/1 mice, reduces inclusions and moderately improves clasping behavior and transcriptional dysregulation but not loss of body weight (Rodriguez-Lebron and others 2005). Postsymptomatic onset, intrastriatal AAV delivery of an shRNA in the HD190QG mouse model causes reduction of inclusion load and a modest restoration of DARPP-32 expression (Machida and others 2006). In an AAV-generated mouse model of HD, intrastriatal co-injection of mHtt plus cholesterol-conjugated small interfering RNA (siRNA), cc-siRNA-Htt, reduces inclusions, improves clasping and beam-crossing performance, and ameliorates neuronal loss but not neuronal shrinkage (DiFiglia and others 2007). Adenoviral delivery of an shRNA targeting HDx-1 in the striatum of R6/2 mice as well as an Ad-HDx-1 model of HD reduces transgene expression and inclusions (Huang and others 2007). Co-delivery of an shRNA, AAV-shHD2, along with AAV-HDx-1, ameliorates loss of NeuN- and calbindin-positive cells in the striatum of rats and normalizes asymmetric forepaw use in unilaterally injected animals (Franich and others 2008). The most positive results to date involve intraventricular delivery of a cholesterol-conjugated siRNA targeting HDx-1 in neonatal R6/2 mice, resulting in reduced mHDx-1 expression. Compared to control-treated mice, those receiving the HDx-1-siRNA display reduced inclusions, delayed clasping and loss of body weight, improved rotarod performance and spontaneous activity, reduced striatal atrophy, and an increase in longevity of 14% (Wang Y-L and others 2005).
Taken together, the RNAi results appear very promising. An important caveat of these studies is, however, that they have all employed species-specific RNAi reagents that only target human Htt. As a result, endogenous mouse Htt is not silenced, although it would be in comparable human HD applications. Some studies have found that nonspecific Htt silencing is relatively nontoxic in mice, resulting in gene expression changes but no overt behavioral phenotype (Boudreau and others 2009; Drouet and others 2009; McBride and others 2008). Nonspecific silencing has in fact been shown to confer therapeutic benefit in a transgenic mouse model of HD. AAV-mediated delivery of miRNA2.4 into the striatum of seven-week-old N171-82Q mice results in a 75% reduction of both human transgene and mouse endogenous Htt mRNAs. Compared to AAV-GFP- and vehicle-treated mice, miRNA-treated mice display improved rotarod performance and a trend toward increased survival but no change in loss of body weight (Boudreau and others 2009). This suggests that nonspecific Htt silencing would be a viable therapeutic option for human HD. The prolonged treatment duration required in humans and the general resistance to Htt-associated neurodegeneration in the mouse brain should be considered, however. If sensitivity to Htt-associated neuropathology were similar between mice and humans, heterozygous knock-in HD mice with polyQ lengths equivalent to those seen in patients would model human HD fairly closely. In actuality, these mice have no clear HD-related phenotype (White and others 1997), and to model human HD in mice, polyQ expansion lengths well above those seen in humans are used, often in the context of a highly toxic N-terminal fragment. For these reasons, allele-specific mHtt gene silencing that does not disrupt wtHtt expression will be preferable for therapeutic applications.
As the HD-causing mutation is an expansion of a normally occurring sequence, development of allele-specific silencing reagents has required ingenuity. Peptide and locked nucleic acid oligonucleotides targeting expanded CAG have shown modest success in selective mHtt silencing in cellular models of HD, although selectivity of these reagents declines in the absence of a large repeat length difference between the normal and mutant allele (Hu and others 2009). Nonetheless, the extremely focused therapeutic mechanism and the potential benefit to not only those afflicted with HD but to those with other CAG expansion diseases warrants further development and optimization of expanded CAG-targeting oligonucleotides. Allele-specific mHtt silencing could also be accomplished by targeting single-nucleotide polymorphisms (SNPs). Many SNPs that are enriched in expanded polyQ human Htt genes have been identified, and silencing reagents targeting a small number of these disease-associated SNPs could provide a therapeutic option for the majority of HD patients (Lombardi and others 2009; Pfister and others 2009; Warby and others 2009). Development of silencing reagents targeting these SNPs is currently under way, and gene therapy efficacy trials in rodent models of HD are eagerly expected in the near future.
Perspectives
It is apparent that a wide variety of gene therapy approaches display promise for prevention as well as treatment of HD symptoms. Several of these approaches also have potential application in other polyQ diseases, as well as in other neurodegenerative diseases that involve protein misfolding, such as Parkinson and Alzheimer diseases and the prionoses. What are the next steps toward human trials? In some cases, the gene therapies must be tested in full-length HD models. In other cases, the reagents must be optimized for use in humans. There is some debate as to the steps after that. One possibility is to test the reagents in animals with larger brains so as to optimize delivery of the vectors (Ciron and others 2009; Fiandaca and others 2009; Varenika and others 2009). Another possibility is to test the therapies for efficacy in nonhuman primates. This could be done using lentiviral delivery of mHtt (Palfi and others 2007). There are also genetic HD models being developed using monkeys, pigs, and sheep (Jacobsen and others 2010; Yang D and others 2010; Yang S-H and others 2008). It will also be extremely important to develop inducible viral vectors so that a transgene that turns out to be ineffective or harmful can be turned off.
Apart from the experimental hurdles that must be overcome, there is a psychological barrier unique to gene therapy in the brain that needs to be confronted. Many researchers believe that inserting genes into the brain is too dangerous and so only small-molecule approaches should be developed. This view reflects a widespread lack of awareness of the many gene therapy trials that are already ongoing or have been concluded in humans. These include trials of potential treatments for Parkinson and Alzheimer diseases as well as others (Christine and others 2009; Kaplitt and others 2007; Mandel 2010; Marks and others 2008). In general, such trials have shown that the safety of the surgery and vector delivery is not a cause for great concern, although new methods are still under development. There is also the issue of side effects; direct delivery of vectors into the brain avoids peripheral side effects, and gene therapies with high target specificity (as with iAbs, for instance) may avoid potential side effects of delivering small-molecule reagents to the periphery.
A daunting reality is that most of the therapies developed in mouse models of cancer, for instance, fail in human trials. For that reason alone, it is important that the wide variety of gene therapy approaches summarized here proceed in parallel toward human testing.
Table 1.
Summary of the Most Promising Gene Therapy Trials in Mice to Date
| Study | Therapeutic Reagent |
Mechanism of Action |
Delivery | HD Model(s) | Motor Performance |
Cognitive/ Psychiatric Performance |
Neuropathology | Body Weight |
Survival |
|---|---|---|---|---|---|---|---|---|---|
| Ebert and others 2010 | GDNF | Trophic support | NPC transplant | N171-82Q | RR | ND | Inclusions, striatal neuron count, no change cortical thinning | Transient increase | ND |
| Ramaswamy and others 2008 | Neurturin | Trophic support | IS-AAV | N171-82Q | RR, gait, clasping | ND | Striatal and cortical neuron count, no change inclusions or neuronal size | ND | No change |
| Cho and others 2007 | BDNF and noggin | Activates endogenous neural stem cells | ICV-Ad | R6/2 | RR, SA | ND | New striatal MSNs | Transient decrease | 17% increase |
| Dai and others 2009 | CaM fragment | Disrupts aberrant mHtt-CaM interaction | IS-AAV | R6/2 | RR, gait, hypoactivity | ND | Inclusions, neuronal size | Increase | No change |
| Southwell and others 2009 | Happ1 iAb | Selectively increases mHtt degradation | IS-AAV | Lentiviral | AIR | ND | Inclusions | ND | No deficit |
| R6/2 | RR, BC | ND | Inclusions, VE | No change | No change | ||||
| N171-82Q | RR, BC, clasping | ND | ND | Increase | 30% increase | ||||
| YAC128 | RR, BC, climbing | OF, OL | VE | No change | ND | ||||
| BACHD | RR, BC, climbing | OF, no change OL | VE | No change | ND | ||||
| Bauer and others 2010 | QBP1-HSC70bm | Targets mHtt for chaperonemediated autophagy | IS-AAV | R6/2 | Clasping, RR | ND | Inclusions, striatal atrophy | Increase | 30% increase |
| Wang Y-L and others 2005 | Cholesterol conjugated siRNA | Nonselectively silences Htt gene expression | ICV | R6/2 | Clasping, RR, SA | ND | Inclusions, striatal atrophy | Transient increase | 14% increase |
AAV = adeno-associated virus; AIR = amphetamine-induced rotation; BC = beam crossing; BDNF = brain-derived neurotrophic factor; GDNF = glial cell line–derived neurotrophic factor; HD = Huntington disease; ICV = intracerebroventricular; IS = intrastriatal; MSN = medium spiny neuron; ND = not determined; NPC = neural progenitor cell; OF = open-field exploration; OL = object learning; RR = rotarod; SA = spontaneous activity; siRNA = small interfering RNA; VE = ventricular enlargement.
Acknowledgments
Financial Disclosure/Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: research from our laboratory that is cited here was funded by the National Institute of Neurological Disease and Stroke and the Hereditary Disease Foundation.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
References
- Alberch J, Pérez-Navarro E, Canals JM. Neuroprotection by neurotrophins and GDNF family members in the excitotoxic model of Huntington’s disease. Brain Res Bull. 2002;57(6):817–822. doi: 10.1016/s0361-9230(01)00775-4. [DOI] [PubMed] [Google Scholar]
- Bauer PO, Goswami A, Wong HK, Okuno M, Kurosawa M, Yamada M, et al. Harnessing chaperone-mediated autophagy for the selective degradation of mutant huntingtin protein. Nat Biotech. 2010;28(3):256–263. doi: 10.1038/nbt.1608. [DOI] [PubMed] [Google Scholar]
- Bemelmans A-P, Horellou P, Pradier L, Brunet I, Colin P, Mallet J. Brain-derived neurotrophic factor–mediated protection of striatal neurons in an excitotoxic rat model of Huntington’s disease, as demonstrated by adenoviral gene transfer. Hum Gene Ther. 1999;10(18):2987–2997. doi: 10.1089/10430349950016393. [DOI] [PubMed] [Google Scholar]
- Biglan KM, Ross CA, Langbehn DR, Aylward EH, Stout JC, Queller S, et al. Motor abnormalities in premanifest persons with Huntington’s disease: the PREDICT-HD study. Movement Disord. 2009;24(12):1763–1772. doi: 10.1002/mds.22601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorkqvist M, Wild EJ, Thiele J, Silvestroni A, Andre R, Lahiri N, et al. A novel pathogenic pathway of immune activation detectable before clinical onset in Huntington’s disease. J Exp Med. 2008;205(8):1869–1877. doi: 10.1084/jem.20080178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreau R, McBride J, Martins I, Shen S, Xing Y, Carter B, et al. Nonallele-specific silencing of mutant and wild-type huntingtin demonstrates therapeutic efficacy in Huntington. Mol Ther. 2009;17(6):1053–1063. doi: 10.1038/mt.2009.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho S-R, Benraiss A, Chmielnicki E, Samdani A, Economides A, Goldman SA. Induction of neostriatal neurogenesis slows disease progression in a transgenic murine model of Huntington disease. J Clin Invest. 2007;117(10):2889–2902. doi: 10.1172/JCI31778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christine CW, Starr PA, Larson PS, Eberling JL, Jagust WJ, Hawkins RA, et al. Safety and tolerability of putaminal AADC gene therapy for Parkinson disease. Neurology. 2009;73(20):1662–1669. doi: 10.1212/WNL.0b013e3181c29356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciron C, Cressant A, Roux F, Raoul S, Cherel Y, Hantraye P, et al. AAV1-, AAV2- and AAV5-mediated human alpha-Iduronidase gene transfer in the brain of non-human primate: vector diffusion and bio distribution. Hum Gene Ther. 2009;20(4):350–360. doi: 10.1089/hum.2008.155. [DOI] [PubMed] [Google Scholar]
- Cui L, Jeong H, Borovecki F, Parkhurst CN, Tanese N, Krainc D. Transcriptional repression of PGC-1α by mutant huntingtin leads to mitochondrial dysfunction and neurodegeneration. Cell. 2006;127(1):59–69. doi: 10.1016/j.cell.2006.09.015. [DOI] [PubMed] [Google Scholar]
- Dai Y, Dudek NL, Li Q, Fowler SC, Muma NA. Striatal expression of a calmodulin fragment improved motor function, weight loss, and neuropathology in the R6/2 mouse model of Huntington’s disease. J Neurosci. 2009;29(37):11550–11559. doi: 10.1523/JNEUROSCI.3307-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiano M, Galvan L, Déglon N, Brouillet E. Mitochondria in Huntington’s disease. Biochim Biophys Acta. 2010;(1):52–61. doi: 10.1016/j.bbadis.2009.07.012. [DOI] [PubMed] [Google Scholar]
- De Almeida LP, Zala D, Aebischer P, Déglon N. Neuroprotective effect of a CNTF-expressing lentiviral vector in the quinolinic acid rat model of Huntington’s disease. Neurobiol Dis. 2001;8(3):433–446. doi: 10.1006/nbdi.2001.0388. [DOI] [PubMed] [Google Scholar]
- De Marchi N, Daniele F, Ragone MA. Fluoxetine in the treatment of Huntington’s disease. Psychopharmacology. 2001;153(2):264–266. doi: 10.1007/s002130000575. [DOI] [PubMed] [Google Scholar]
- Denovan-Wright EM, Attis M, Rodriguez-Lebron E, Mandel RJ. Sustained striatal ciliary neurotrophic factor expression negatively affects behavior and gene expression in normal and R6/1 mice. J Neurosci Res. 2008;86(8):1748–1757. doi: 10.1002/jnr.21636. [DOI] [PubMed] [Google Scholar]
- Dey ND, Bombard MC, Roland BP, Davidson S, Lu M, Rossignol J, et al. Genetically engineered mesenchymal stem cells reduce behavioral deficits in the YAC 128 mouse model of Huntington’s disease. Behav Brain Res. 2010;214(2):193–200. doi: 10.1016/j.bbr.2010.05.023. [DOI] [PubMed] [Google Scholar]
- DiFiglia M, Sena-Esteves M, Chase K, Sapp E, Pfister E, Sass M, et al. Therapeutic silencing of mutant huntingtin with siRNA attenuates striatal and cortical neuropathology and behavioral deficits. PNAS. 2007;104(43):17204–17209. doi: 10.1073/pnas.0708285104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragatsis I, Levine MS, Zeitlin S. Inactivation of Hdh in the brain and testis results in progressive neurodegeneration and sterility in mice. Nat Genet. 2000;26(3):300–306. doi: 10.1038/81593. [DOI] [PubMed] [Google Scholar]
- Drouet V, Perrin V, Hassig R, Dufour N, Auregan G, Alves S, et al. Sustained effects of nonallele-specific Huntingtin silencing. Ann Neurol. 2009;65(3):276–285. doi: 10.1002/ana.21569. [DOI] [PubMed] [Google Scholar]
- Duff K, Paulsen JS, Beglinger LJ, Langbehn DR, Stout JC. Psychiatric symptoms in Huntington’s disease before diagnosis: the Predict-HD Study. BiolPsychiat. 2007;62(12):1341–1346. doi: 10.1016/j.biopsych.2006.11.034. [DOI] [PubMed] [Google Scholar]
- Ebert AD, Barber AE, Heins BM, Svendsen CN. Ex vivo delivery of GDNF maintains motor function and prevents neuronal loss in a transgenic mouse model of Huntington’s disease. Exp Neurol. 2010;224(1):155–162. doi: 10.1016/j.expneurol.2010.03.005. [DOI] [PubMed] [Google Scholar]
- Emerich DF, Lindner MD, Winn SR, Chen E-Y, Frydel BR, Kordower JH. Implants of encapsulated human CNTF-producing fibroblasts prevent behavioral deficits and striatal degeneration in a rodent model of Huntington’s disease. J Neurosci. 1996;16(16):5168–5181. doi: 10.1523/JNEUROSCI.16-16-05168.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiandaca MS, Varenika V, Eberling J, McKnight T, Bringas J, Pivirotto P, et al. Real-time MR imaging of adeno-associated viral vector delivery to the primate brain. NeuroImage. 2009;47 Suppl 2:T27–T35. doi: 10.1016/j.neuroimage.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franich NR, Fitzsimons HL, Fong DM, Klugmann M, During MJ, Young D. AAV vector-mediated RNAi of mutant huntingtin expression is neuroprotective in a novel genetic rat model of Huntington’s disease. Mol Ther. 2008;16(5):947–956. doi: 10.1038/mt.2008.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giralt A, Friedman HC, Caneda-Ferron B, Urban N, Moreno E, Rubio N, et al. BDNF regulation under GFAP promoter provides engineered astrocytes as a new approach for long-term protection in Huntington’s disease. Gene Ther. 2010;17:1294–1308. doi: 10.1038/gt.2010.71. [DOI] [PubMed] [Google Scholar]
- Haque N, Isacson O. Neurotrophic factors NGF and FGF-2 alter levels of huntingtin (IT15) in striatal neuronal cell cultures. Cell Transplant. 2000;9(5):623–627. doi: 10.1177/096368970000900507. [DOI] [PubMed] [Google Scholar]
- Harper SQ. Progress and challenges in RNA interference therapy for Huntington disease. Arch Neurol. 2009;66(8):933–938. doi: 10.1001/archneurol.2009.180. [DOI] [PubMed] [Google Scholar]
- Harper SQ, Staber PD, He X, Eliason SL, Martins IH, Mao Q, et al. From the cover: RNA interference improves motor and neuropathological abnormalities in a Huntington’s disease mouse model. PNAS. 2005;102(16):5820–5825. doi: 10.1073/pnas.0501507102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J, Matsui M, Corey DR. Allele-selective inhibition of mutant huntingtin by peptide nucleic acid-peptide conjugates, locked nucleic acid, and small interfering RNA. Ann N Y Acad Sci. 2009;1175:24–31. doi: 10.1111/j.1749-6632.2009.04975.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang B, Schiefer J, Sass C, Landwehrmeyer GB, Kosinski CM, Kochanek S. High-capacity adenoviral vector-mediated reduction of huntingtin aggregate load in vitro and in vivo. Hum Gene Ther. 2007;18(4):303–311. doi: 10.1089/hum.2006.160. [DOI] [PubMed] [Google Scholar]
- Huntington Study Group. Tetrabenazine as antichorea therapy in Huntington disease: a randomized controlled trial. Neurology. 2006;66(3):366–372. doi: 10.1212/01.wnl.0000198586.85250.13. [DOI] [PubMed] [Google Scholar]
- Huntington’s Disease Collaborative Research Group. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell. 1993;72(6):971–983. doi: 10.1016/0092-8674(93)90585-e. [DOI] [PubMed] [Google Scholar]
- Imarisio S, Carmichael J, Korolchuk V, Chen C-W, Saiki S, Rose C, et al. Huntington’s disease: from pathology and genetics to potential therapies. Biochem J. 2008;412(2):191–209. doi: 10.1042/BJ20071619. [DOI] [PubMed] [Google Scholar]
- Ip NY, Yancopoulos GD. The neurotrophins and CNTF: two families of collaborative neurotrophic factors. Ann Rev Neurosci. 1996;19(1):491–515. doi: 10.1146/annurev.ne.19.030196.002423. [DOI] [PubMed] [Google Scholar]
- Jacobsen JC, Bawden CS, Rudiger SR, McLaughlan CJ, Reid SJ, Waldvogel HJ, et al. An ovine transgenic Huntington’s disease model. Hum Mol Genet. 2010;19(10):1873–1882. doi: 10.1093/hmg/ddq063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplitt MG, Feigin A, Tang C, Fitzsimons HL, Mattis P, Lawlor PA, et al. Safety and tolerability of gene therapy with an adeno-associated virus (AAV) borne GAD gene for Parkinson’s disease: an open label, phase I trial. Lancet. 2007;369(9579):2097–2105. doi: 10.1016/S0140-6736(07)60982-9. [DOI] [PubMed] [Google Scholar]
- Kells AP, Fong DM, Dragunow M, During MJ, Young D, Connor B. AAV-mediated gene delivery of BDNF or GDNF is neuroprotective in a model of Huntington disease. Mol Ther. 2004;9(5):682–688. doi: 10.1016/j.ymthe.2004.02.016. [DOI] [PubMed] [Google Scholar]
- Lecerf JM, Shirley TL, Zhu Q, Kazantsev A, Amersdorfer P, Housman DE, et al. Human single-chain Fv intrabodies counteract in situ huntingtin aggregation in cellular models of Huntington’s disease. PNAS. 2001;98(8):4764–4769. doi: 10.1073/pnas.071058398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi MS, Jaspers L, Spronkmans C, Gellera C, Taroni F, Di Maria E, et al. A majority of Huntington’s disease patients may be treatable by individualized allele-specific RNA interference. Exp Neurol. 2009;217(2):312–319. doi: 10.1016/j.expneurol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Machida Y, Okada T, Kurosawa M, Oyama F, Ozawa K, Nukina N. rAAV-mediated shRNA ameliorated neuropathology in Huntington disease model mouse. Biochem Biophys Res Comm. 2006;343(1):190–197. doi: 10.1016/j.bbrc.2006.02.141. [DOI] [PubMed] [Google Scholar]
- Mandel RJ. CERE-110, an adeno-associated virus-based gene delivery vector expressing human nerve growth factor for the treatment of Alzheimer’s disease. Curr Op Mol Ther. 2010;12(2):240–247. [PubMed] [Google Scholar]
- Marks WJJ, Ostrem JL, Verhagen L, Starr PA, Larson PS, Bakay RAE, et al. Safety and tolerability of intraputaminal delivery of CERE-120 (adeno-associated virus serotype 2-neurturin) to patients with idiopathic Parkinson’s disease: an open-label, phase I trial. Lancet Neurol. 2008;7(5):400–408. doi: 10.1016/S1474-4422(08)70065-6. [DOI] [PubMed] [Google Scholar]
- Martinez-Serrano A, Bjorklund A. Protection of the neostriatum against excitotoxic damage by neurotrophin-producing, genetically modified neural stem cells. J Neurosci. 1996;16(15):4604–4616. doi: 10.1523/JNEUROSCI.16-15-04604.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride JL, Boudreau RL, Harper SQ, Staber PD, Monteys AM, Martins IS, et al. Artificial miRNAs mitigate shRNA-mediated toxicity in the brain: implications for the therapeutic development of RNAi. PNAS. 2008;105(15):5868–5873. doi: 10.1073/pnas.0801775105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride JL, Ramaswamy S, Gasmi M, Bartus RT, Herzog CD, Brandon EP, et al. Viral delivery of glial cell line-derived neurotrophic factor improves behavior and protects striatal neurons in a mouse model of Huntington’s disease. PNAS. 2006;103(24):9345–9350. doi: 10.1073/pnas.0508875103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy RC, Messer A. A single-chain Fv intrabody provides functional protection against the effects of mutant protein in an organotypic slice culture model of Huntington’s disease. Mol Brain Res. 2004;121(1–2):141–145. doi: 10.1016/j.molbrainres.2003.11.011. [DOI] [PubMed] [Google Scholar]
- Palfi S, Brouillet E, Jarraya B, Bloch J, Jan C, Shin M, et al. Expression of mutated huntingtin fragment in the putamen is sufficient to produce abnormal movement in non-human primates. Mol Ther. 2007;15(8):1444–1451. doi: 10.1038/sj.mt.6300185. [DOI] [PubMed] [Google Scholar]
- Panov AV, Gutekunst C-A, Leavitt BR, Hayden MR, Burke JR, Strittmatter WJ, et al. Early mitochondrial calcium defects in Huntington’s disease are a direct effect of polyglutamines. Nat Neurosci. 2002;5(8):731–736. doi: 10.1038/nn884. [DOI] [PubMed] [Google Scholar]
- Passani LA, Bedford MT, Faber PW, McGinnis KM, Sharp AH, Gusella JF, et al. Huntingtin’s WW domain partners in Huntington’s disease post-mortem brain fulfill genetic criteria for direct involvement in Huntington’s disease pathogenesis. Hum Mol Genet. 2000;9(14):2175–2182. doi: 10.1093/hmg/9.14.2175. [DOI] [PubMed] [Google Scholar]
- Pérez-Navarro E, Åkerud P, Marco S, Canals JM, Tolosa E, Arenas E, et al. Neurturin protects striatal projection neurons but not interneurons in a rat model of Huntington’s disease. Neuroscience. 2000;98(1):89–96. doi: 10.1016/s0306-4522(00)00074-9. [DOI] [PubMed] [Google Scholar]
- Pérez-Navarro E, Arenas E, Marco S, Alberch J. Intrastriatal grafting of a GDNF-producing cell line protects striatonigral neurons from quinolinic acid excitotoxicity in vivo. Eur J Neurosci. 1999;11(1):241–249. doi: 10.1046/j.1460-9568.1999.00433.x. [DOI] [PubMed] [Google Scholar]
- Pérez-Navarro E, Arenas E, Reiriz J, Calvo N, Alberch J. Glial cell line-derived neurotrophic factor protects striatal calbindin-immunoreactive neurons from excitotoxic damage. Neuroscience. 1996;75(2):345–352. doi: 10.1016/0306-4522(96)00336-3. [DOI] [PubMed] [Google Scholar]
- Pfister EL, Kennington L, Straubhaar J, Wagh S, Liu W, DiFiglia M, et al. Five siRNAs targeting three SNPs may provide therapy for three-quarters of Huntington’s disease patients. Curr Biol. 2009;19(9):774–778. doi: 10.1016/j.cub.2009.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineda JR, Rubio N, Akerud P, Urban N, Badimon L, Arenas E, et al. Neuroprotection by GDNF-secreting stem cells in a Huntington’s disease model: optical neuroimage tracking of brain-grafted cells. Gene Ther. 2006;14(2):118–128. doi: 10.1038/sj.gt.3302847. [DOI] [PubMed] [Google Scholar]
- Popovic N, Maingay M, Kirik D, Brundin P. Lentiviral gene delivery of GDNF into the striatum of R6/2 Huntington mice fails to attenuate behavioral and neuropathological changes. Exp Neurol. 2005;193(1):65–74. doi: 10.1016/j.expneurol.2004.12.009. [DOI] [PubMed] [Google Scholar]
- Qin Z-H, Wang Y, Sapp E, Cuiffo B, Wanker E, Hayden MR, et al. Huntingtin bodies sequester vesicle-associated proteins by a polyproline-dependent interaction. J Neurosci. 2004;24(1):269–281. doi: 10.1523/JNEUROSCI.1409-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy S, McBride J, Han I, Berry-Kravis E, Zhou LH, Herzog CD, et al. Intrastriatal CERE-120 (AAV-neurturin) protects striatal and cortical neurons and delays motor deficits in a transgenic mouse model of Huntington. Neurobiol Dis. 2008;34(1):40–45. doi: 10.1016/j.nbd.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Ramaswamy S, McBride JL, Herzog CD, Brandon E, Gasmi M, Bartus RT, et al. Neurturin gene therapy improves motor function and prevents death of striatal neurons in a 3-nitropropionic acid rat model of Huntington’s disease. Neurobiol Dis. 2007;26(2):375–384. doi: 10.1016/j.nbd.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Ramaswamy SS, Shannon KMKM, Kordower JHJH. Huntington’s disease: pathological mechanisms and therapeutic strategies. Cell Transplant. 2007;16(3):301–312. doi: 10.3727/000000007783464687. [DOI] [PubMed] [Google Scholar]
- Ravikumar B, Vacher C, Berger Z, Davies JE, Luo S, Oroz LG, et al. Inhibition of mTOR induces autophagy and reduces toxicity of polyglutamine expansions in fly and mouse models of Huntington disease. Nat Genet. 2004;36(6):585–595. doi: 10.1038/ng1362. [DOI] [PubMed] [Google Scholar]
- Régulier E, Pereira de Almeida L, Sommer B, Aebischer P, Déglon N. Dose-dependent neuroprotective effect of ciliary neurotrophic factor delivered via tetracycline-regulated lentiviral vectors in the quinolinic acid rat model of Huntington’s disease. Hum Gene Ther. 2002;13(16):1981–1990. doi: 10.1089/10430340260355383. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Lebron E, Denovan-Wright EM, Nash K, Lewin AS, Mandel RJ. Intrastriatal rAAV-mediated delivery of anti-huntingtin shRNAs induces partial reversal of disease progression in R6/1 Huntington’s disease transgenic mice. Mol Ther. 2005;12(4):618–633. doi: 10.1016/j.ymthe.2005.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas D, Salat D, Lee S, Zaleta A, Hevelone N, Hersch SM. Complexity and heterogeneity: what drives the ever-changing brain in Huntington’s disease? Ann NY Acad Sci. 2008;1147:196–205. doi: 10.1196/annals.1427.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose C, Menzies FM, Renna M, Acevedo-Arozena A, Corrochano S, Sadiq O, et al. Rilmenidine attenuates toxicity of polyglutamine expansions in a mouse model of Huntington’s disease. Hum Mol Genet. 2010;19(11):2144–2153. doi: 10.1093/hmg/ddq093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S, Krishna G, Imarisio S, Saiki S, O’Kane CJ, Rubinsztein DC. A rational mechanism for combination treatment of Huntington’s disease using lithium and rapamycin. Hum Mol Genet. 2008;17(2):170–178. doi: 10.1093/hmg/ddm294. [DOI] [PubMed] [Google Scholar]
- Sarkar S, Rubinsztein DC. Huntington’s disease: degradation of mutant huntingtin by autophagy. FEBS J. 2008;275(17):4263–4270. doi: 10.1111/j.1742-4658.2008.06562.x. [DOI] [PubMed] [Google Scholar]
- Snyder-Keller A, Butler D, Messer A. Engineered antibody fragments can reduce Huntington’s disease phenotypes in vivo and in situ. Program no 859.21. San Diego, CA: Society for Neuroscience; 2010. Online. [Google Scholar]
- Snyder-Keller A, McLear JA, Hathorn T, Messer A. Early or Late-Stage Anti-N-Terminal Huntingtin Intrabody Gene Therapy Reduces Pathological Features in B6.HDR6/1 Mice. J Neuropath Exp Neurol. 2010;69(10):1078–1085. doi: 10.1097/NEN.0b013e3181f530ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwell AL, Bugg CW, Kaltenbach LS, Dunn DE, Butland SL, Weiss A, et al. Perturbation with intrabodies reveals that calpain cleavage is required for degradation of huntingtin exon 1. PLoS ONE. 2010;6(1):e16676. doi: 10.1371/journal.pone.0016676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwell AL, Khoshnan A, Dunn DE, Bugg CW, Lo DC, Patterson PH. Intrabodies binding the proline-rich domains of mutant huntingtin increase its turnover and reduce neurotoxicity. J Neurosci. 2008;28(36):9013–9020. doi: 10.1523/JNEUROSCI.2747-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southwell AL, Ko J, Patterson PH. Intrabody gene therapy ameliorates motor, cognitive, and neuropathological symptoms in multiple mouse models of Huntington’s disease. J Neurosci. 2009;29(43):13589–13602. doi: 10.1523/JNEUROSCI.4286-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffan JS, Kazantsev A, Spasic-Boskovic O, Greenwald M, Zhu Y-Z, Gohler H, et al. The Huntington’s disease protein interacts with p53 and CREB-binding protein and represses transcription. PNAS. 2000;97(12):6763–6768. doi: 10.1073/pnas.100110097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taupin P, Gage FH. Adult neurogenesis and neural stem cells of the central nervous system in mammals. J Neurosci Res. 2002;69(6):745–749. doi: 10.1002/jnr.10378. [DOI] [PubMed] [Google Scholar]
- Varenika V, Kells AP, Valles F, Hadaczek P, Forsayeth J, Bankiewicz KS, et al. Controlled dissemination of AAV vectors in the primate brain. Prog Brain Res. 2009;175:163–172. doi: 10.1016/S0079-6123(09)17511-8. [DOI] [PubMed] [Google Scholar]
- Walker FO. Huntington’s disease. Lancet. 2007;369(9557):218–228. doi: 10.1016/S0140-6736(07)60111-1. [DOI] [PubMed] [Google Scholar]
- Wang C-E, Zhou H, McGuire JR, Cerullo V, Lee B, Li S-H, et al. Suppression of neuropil aggregates and neurological symptoms by an intracellular antibody implicates the cytoplasmic toxicity of mutant huntingtin. J Cell Biol. 2008;181(5):803–816. doi: 10.1083/jcb.200710158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y-L, Liu W, Wada E, Murata M, Wada K, Kanazawa I. Clinico-pathological rescue of a model mouse of Huntington’s disease by siRNA. Neurosci Res. 2005;53(3):241–249. doi: 10.1016/j.neures.2005.06.021. [DOI] [PubMed] [Google Scholar]
- White JK, Auerbach W, Duyao MP, Vonsattel JP, Gusella JF, Joyner AL, et al. Huntingtin is required for neurogenesis and is not impaired by the Huntington’s disease CAG expansion. Nat Genet. 1997;17(4):404–410. doi: 10.1038/ng1297-404. [DOI] [PubMed] [Google Scholar]
- Yang D, Wang C-E, Zhao B, Li W, Ouyang Z, Liu Z, et al. Expression of Huntington’s disease protein results in apoptotic neurons in the brains of cloned transgenic pigs. Hum Mol Genet. 2010;19(20):3983–3994. doi: 10.1093/hmg/ddq313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S-H, Cheng P-H, Banta H, Piotrowska-Nitsche K, Yang J-J, Cheng ECH, et al. Towards a transgenic model of Huntington’s disease in a non-human primate. Nature. 2008;453(7197):921–924. doi: 10.1038/nature06975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zala D, Bensadoun J-C, Pereira de Almeida L, Leavitt BR, Gutekunst C-A, Aebischer P, et al. Long-term lentiviral-mediated expression of ciliary neurotrophic factor in the striatum of Huntington’s disease transgenic mice. Exp Neurol. 2004;185(1):26–35. doi: 10.1016/j.expneurol.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Zuccato C, Cattaneo E. Role of brain-derived neurotrophic factor in Huntington’s disease. Prog Neurobiol. 2007;81(5–6):294–330. doi: 10.1016/j.pneurobio.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Zuccato C, Valenza M, Cattaneo E. Molecular mechanisms and potential therapeutical targets in Huntington’s disease. Physiol Rev. 2010;90(3):905–981. doi: 10.1152/physrev.00041.2009. [DOI] [PubMed] [Google Scholar]