Abstract
A Behavioral Model of Health Services Utilization approach was used to examine the impact of comorbid mental illness on mortality of veterans admitted to Veterans Affairs Medical Centers in fiscal year 2001 with a primary diagnosis of congestive heart failure (n= 15,497). Thirty percent had a psychiatric diagnosis, 4.7% died during the index hospitalization and 11.5% died during the year following discharge. Among those with mental illness, 23.6% had multiple psychiatric disorders. Multivariable logistic regression models found dementia to be positively associated with inpatient mortality. Depression alone (excluding other psychiatric disorders) was positively associated with one-year mortality. Primary care visits were associated with a reduced likelihood of both inpatient and one-year mortality. Excepting dementia, VA patients with a mental illness had comparable or higher levels of primary care visits than those having no mental illness. Patients with multiple psychiatric disorders had more outpatient care than those with one psychiatric disorder.
INTRODUCTION
Congestive heart failure (CHF) is the most common cause of hospital admission among the elderly, with direct and indirect costs in the US exceeding $33 billion.1 Estimated one-year mortality rates among Medicare beneficiaries hospitalized for CHF range from 29 to 36%.2 Medicare CHF research has documented that mental illness is associated with increased hospital utilization and cost.3 Furthermore, the National Heart Failure project found that 17% of Medicare heart failure patients had a mental diagnosis and that mental illness was associated with slightly worse inpatient care and higher mortality rates.4
Although depression and anxiety are the mental illnesses most commonly linked to poor CHF outcomes,5 dementia6 and schizophrenia7 have also been linked to poor cardiac outcomes. Lifestyle factors of those with mental illness, such as high smoking rates, use of alcohol and other drugs, and less physical activity may contribute to increased mortality.8 There may also be direct biological influences of mental illness, such as changes in immune system response.9 Individuals with severe mental illness tend to delay cardiac care10 and those with mental disorders have been found to under use evidence-based cardiovascular services.11
Given that heart failure is the number one reason for discharge among veterans served by the Department of Veteran Affairs Health Administration (VA), many efforts have been implemented to identify and apply best clinical practices in order to improve outcomes.12 The combination of heart failure and mental illness is of special concern to the VA since roughly one-third of VA patients in medical treatment have at least one psychiatric diagnosis.13 In addition, beyond the co-occurrence of psychiatric and medical diagnoses, many VA patients have multiple psychiatric diagnoses. For example, a survey in 10 VA primary care clinics found that 36% of depressed patients screened positive for Posttraumatic Stress Disorder (PTSD).14 Another VA study found that heart disease patients with multiple mental diagnoses had greater impairment and increased distress than veterans with only one type of mental diagnosis.15
Surprisingly, some VA research has found that psychiatric diagnosis among heart failure patients is associated with a decreased risk of mortality.16 Possible explanations suggested by those authors were increased vigilance of psychiatric patients or a greater likelihood of admitting lower severity CHF patients due to the mental illness.16 In response to inconclusive findings and these special concerns of the VA, we have examined the influence of comorbid psychiatric illnesses on mortality among veterans hospitalized for congestive heart failure. We wanted to examine the relationship of mental illness to in-hospital and one-year mortality, explore differences based on type of psychiatric diagnosis, and consider the influence of multiple psychiatric diagnoses. We also assessed whether differences in healthcare utilization might explain differences in mortality rates.
The Behavioral Model of Health Services Utilization17 provides the conceptual framework for examining the impact of mental illness on the health services utilization and mortality of veterans with congestive heart failure. This Model has been used within the VA to examine mental health services18, 19 and the relationship between mental illness and clinical severity of patients with CHF or pneumonia.16 It has also been used to examine context and heart failure management of Medicare patients.2 The Behavioral Model acknowledges that the general environment, including the healthcare system’s availability and characteristics, provides the context for health status and healthcare utilization. Socio-demographics such as age, gender, and race may predispose individuals to use health services, while enabling factors such as insurance and income facilitate utilization. Personal need factors, represented by the presence or severity of a medical condition may play a large role in utilization and subsequent outcomes. This model is graphically portrayed in Figure 1, where it is assumed that mortality is partially a function of prior health care behavior, including primary care. The Behavioral Model has been expanded to include vulnerable domains in order to better study disadvantaged populations.20 Mental illness is generally considered a personal predisposing factor in this expanded vulnerable domain model.
Figure 1.
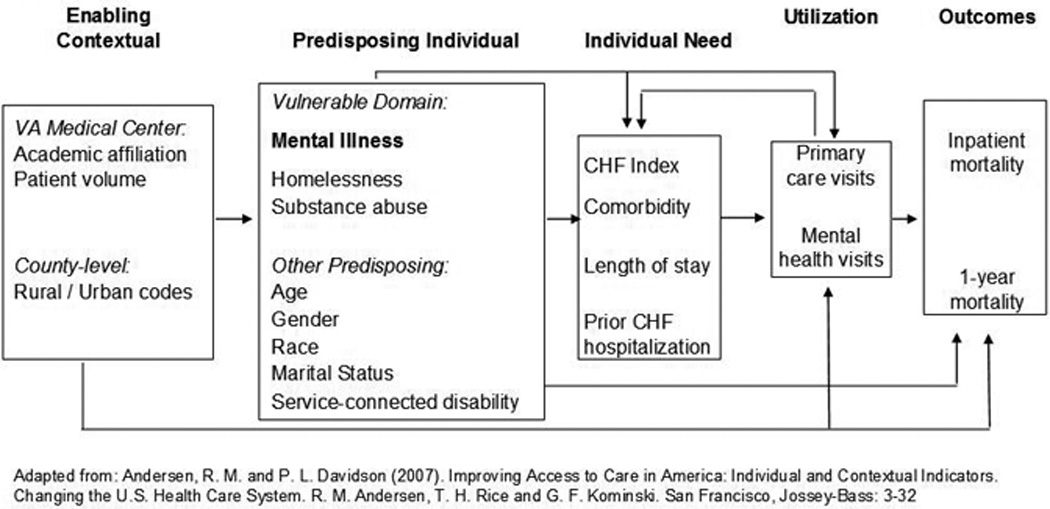
Behavioral Model of Health Services Use Measurement Model.
METHODS
STUDY SAMPLE
Patient-level data were extracted from the Department of Veteran Affairs National Patient Care Database in July of 2003 after obtaining approval from the UCLA and Greater Los Angeles VA Institutional Review Boards.21 Analysis was conducted on 15,497 veterans admitted to VA Medical Centers during fiscal year (FY) 2001 with a primary diagnosis of congestive heart failure. Heart failure was defined consistent with other VA heart failure research.22 Congestive heart failure (ICD-9-CM codes of 428.0, 428.1 or 428.9) was present in 94.9% of subjects, while hypertensive heart disease with CHF (402.01, 402.11, and 402.91) was found in 3.6% of subjects. The remaining subjects had rheumatic heart failure (398.91) or hypertensive heart and renal disease with CHF (404.01, 404.03, 404.11, 401.13, 404.91 or 404.93). The index hospitalization was defined as the first inpatient service in FY 2001 in which heart failure was the primary diagnosis. All outpatient and inpatient records for those veterans between FY 2000 and FY 2002 were also extracted.
VARIABLES
Dependent variable
All-cause mortality in the year after index hospitalization discharge was determined by examining discharge status and date of death fields. This information in the Patient Treatment File is updated from other sources including the Veterans Benefits Administration Death Notice File, which has been shown to capture most veteran deaths.23 Hospitalization records were available for 95% of patients dying within the first year. The primary diagnosis of their final hospitalization was examined to see if cardiac reasons might be considered the primary reason for death (ICD-9 CM codes of 390–456: diseases of the circulatory system).
Primary predisposing individual variable
Patients were assigned to a psychiatric diagnosis category based on diagnoses recorded in the index CHF hospitalization as well as inpatient and outpatient services during the 12 months prior to the index CHF hospitalization. The psychiatrtic category selection was based on the VA study by Cradock-O-Leary et al. that examined psychiatric illness and medical utilization.24 Patients were noted as having dementia (ICD-9-CM 290 or 294), severe mental illness (schizophrenia: 295, post traumatic stress disorder: 309.81, or bi-polar disorder, 296.00–296.06 or 296.40–296.89), depression (remaining 296.xx, 300.4, or 311), and anxiety disorders (300.00–300.3, 308.3, or 309.21–309.28). For completeness sake, a category was created for other mental diagnoses, including personality and adjustment disorders and mental illness to due a medical condition (ICD-9 codes 293 through 316, excluding those already mentioned and excluding substance abuse). However, other mental illness was not discussed because of its heterogeneity. To account for multiple psychiatric diagnoses, we categorized patients as having only one of the five types of psychiatric diagnoses mentioned above, or in one of three groups of psychiatric comorbidity: dementia with another mental illness, serious mental illness with depression and/or anxiety, and depression with anxiety.
Other predisposing individual variables
These variables included age, categorically coded into five year increments based on mortality risk,25 ethnicity, gender and marital status. Vulnerable domain measures included substance abuse/dependence (based on ICD-9-CM codes 291–293 or 303–305 during inpatient or outpatient services within the prior year) and being homeless at any point in the year preceding the index admission as per outpatient records. Though having a service-connected condition greater than 10% could be considered an individual enabling variable since that places a veteran at a higher priority for VA services,26 we considered it as a predisposing variable since by definition all study subjects were users of inpatient services.
Enabling contextual variables
Prior VA research demonstrated geographic variation in treatment costs for CHF24 and geographic variations have been found in quality of care for heart failure.2 Thus, an environmental measure was obtained from the Area Resource File27 by recoding rural vs. urban distinction continuum codes developed by the US Department of Agriculture. One may assume that there is a greater availability of medical care both inside and outside of the VA system in more densely populated counties. The primary health system unit of measurement was the VA Medical Center, identified by a three digit station number. Medical center measures included affiliation with a medical school and size, based on number of veterans served in 2001.18 Larger hospitals and those with a medical school affiliation tend to have lower mortality and readmission rates,28 perhaps as a result of more specialized resources.
Individual need variables
Need or clinical severity was proxied primarily by the Congestive Heart Failure Index.29 This Index has been shown to be more predictive of mortality among heart failure patients than the better known Charlson Index30 and is based on patient age, whether they were transferred to another hospital at discharge, and a handful of inpatient diagnoses, including ventricular arrhythmia, hypotension, and shock. The calculated index was used as integers, top-coded at six. The more widely used Elixhauser method31 was also employed to account for clinical need. Dummy variables were generated to indicate presence of comorbid conditions commonly associated with inpatient mortality. This method has also been found to account for more variation in mortality than the Charlson Index.32
Health care utilization variables
Cardiac hospitalization in the year preceding the index hospitalization (yes/no) was obtained by examining the primary diagnoses of earlier hospitalization records. Length of stay during the index hospitalization was transformed by taking the natural logarithm to approximate normality assumptions. Primary care was measured by number of days in the outpatient records where services were provided at specific clinics, such as diabetes and geriatrics, identified in VA records by three-digit clinic stop codes (300–323, 350), as per another VA study that examined medical care among a mentally ill population.18 Services for both the year preceding and following the index hospitalization were recoded to 0, 1 to 4, 5 to 8, 9 to 15, and 16 or more, roughly following the lead of a recent study which found that 9 or more primary care among seriously ill CHF Medicare beneficiaries reduced inpatient utilization during the last year of life.33 Mental health visits (yes/no) were identified by clinic stop codes 500 to 599 for the year preceding and following hospitalization.
DATA ANALYSIS
The bivariate distribution of independent and dependent variables based on the presence of any psychiatric diagnosis was examined using the Chi-square test for categorical variables and t-test or analysis of variance for continuous variables. The distribution of selected patient characteristics by psychiatric category were also examined, with bivariate statistics computed between single and comorbid conditions, for example, dementia only versus dementia with another mental illness. Multivariable hierarchical logistic regression models were specified to test the occurrence (yes/no) of mortality, accounting for non-independence of contextual measures for patients within each VA Medical Center. Robust regression models were used due to observed heteroskedasticity in the dependent variables, resulting in slightly larger 95% confidence intervals for the odds ratios. The relative contribution of each component of the Behavioral Model to mortality was assessed by Receiver Operator Curve (ROC) analysis, successively entering each block of variables into the mortality regression models and observing changes in the Area Under the Curve.34 Model adequacy was confirmed by non-significant Hosmer-Lemeshow goodness-of-fit test statistics and collinearity did not appear to be a significant issue based on a review of Pearson correlation coefficients. Statistical analysis was done with Stata/SE software (version 11.0, StataCorp, College Station, Texas) and statistical significance was assessed using a traditional P value < 0.05.
RESULTS
One can see in Table 1 that approximately 30% of patients had any psychiatric diagnosis. Those with any psychiatric diagnosis were more likely to die during the index hospitalization and in the year following discharge. There were clearly differences in other predisposing characteristics. Those with a psychiatric diagnosis were more likely to be younger, female, White, to use substances, and to have a service-connected disability. On the other hand, they were less likely to be homeless. There were essentially no differences in contextual measures or clinical measures of severity between the two groups. However, patients with mental illness were more likely to have been hospitalized for heart failure, to have had more primary care visits in the year preceding the index hospitalization, and have had a longer length of stay during the index hospitalization.
Table 1.
Characteristics of patients based on psychiatric diagnosis.
| No psychiatric diagnosis |
Any psychiatric diagnosis |
||
|---|---|---|---|
| (n = 10,807) | (n = 4,690) | P value | |
| Other predisposing individual variables | |||
| Homeless (percent) | 6.4 | 3.8 | <0.001 |
| Substance Use/Abuse | 16.5 | 21.4 | <0.001 |
| Less than 65 years of age | 27.6 | 30.7 | <0.001 |
| 65 to 74 years | 32.9 | 28.4 | <0.001 |
| 75 to 79 years | 21.0 | 20.4 | 0.396 |
| 80+ years | 18.4 | 20.5 | 0.003 |
| White | 68.4 | 74.4 | <0.001 |
| Black | 22.8 | 18.4 | <0.001 |
| Other race | 8.7 | 7.3 | 0.003 |
| Female | 1.3 | 2.3 | <0.001 |
| Married | 48.3 | 48.4 | 0.880 |
| Service-Connected (SC) condition>10% |
19.3 | 31.4 | <0.001 |
| Metro County, greater than 1,000,000 | 48.4 | 47.9 | 0.575 |
| Metro County, less than 1,000,000 | 28.1 | 29.7 | 0.047 |
| Non-Metro County | 23.5 | 22.4 | 0.144 |
| No medical school affiliation | 8.6 | 8.9 | 0.618 |
| No. of veterans served in Fiscal Year 01 (1,000’s) Mean(SD) |
6.0 (2.9) | 6.0 (2.9) | 0.9217 |
| Individual need variables | |||
| Congestive Heart Failure (CHF) Index | |||
| 1 | 25.2 | 23.7 | 0.048 |
| 2 | 38.3 | 38.4 | 0.873 |
| 3 | 23.0 | 23.2 | 0.870 |
| 4 | 7.0 | 7.2 | 0.577 |
| 5 | 3.4 | 3.2 | 0.516 |
| 6 | 3.1 | 4.3 | 0.000 |
| Elixhauser comorbidities | |||
| Peripheral vascular disorders | 7.7 | 7.1 | 0.233 |
| Chronic pulmonary disease | 21.0 | 20.5 | 0.529 |
| Diabetes (no complications) | 32.2 | 30.7 | 0.083 |
| Diabetes (with complication) | 6.1 | 7.1 | 0.026 |
| Hyperthyroidism | 5.3 | 6.4 | 0.005 |
| Renal failure | 6.0 | 5.8 | 0.656 |
| Cancer (tumor) | 6.4 | 6.0 | 0.335 |
| Fluid and electrolyte disorders | 9.0 | 9.8 | 0.091 |
| Deficiency anemia | 16.0 | 15.0 | 0.087 |
| Hypertension | 42.8 | 41.3 | 0.077 |
| Obesity | 5.4 | 5.8 | 0.373 |
| Prior CHF hospitalization | 17.4 | 24.1 | <0.001 |
| Index hospitalization length of stay (log) mean(std dev) |
6.9 (9.4) | 7.7 (12.3) | <0.001 |
| Health care utilization | |||
| Year before index hospitalization | |||
| 0 primary care visits | 11.5 | 6.7 | <0.001 |
| 1 to 4 primary care visits | 24.7 | 22.7 | 0.008 |
| 5 to 8 primary care visits | 23.7 | 24.4 | 0.366 |
| 9 to 15 primary care visits | 23.4 | 25.9 | 0.001 |
| 16 or more visits | 16.7 | 20.3 | <0.001 |
| Any mental health visits | 4.8 | 49.3 | <0.001 |
| Year after index hospitalization+ | |||
| 0 primary care visits | 10.7 | 15.4 | <0.001 |
| 1 to 4 primary care visits | 23.2 | 24.8 | 0.043 |
| 5 to 8 primary care visits | 21.7 | 20.8 | 0.195 |
| 9 to 15 primary care visits | 24.5 | 22.1 | 0.002 |
| 16 or more visits | 19.8 | 16.9 | <0.001 |
| Any mental health visits | 8.9 | 36.2 | <0.001 |
| Outcomes | |||
| Died in index hospitalization | 4.2 | 6.0 | <0.001 |
| All-cause one-year mortalitya | 10.8 | 13.4 | <0.001 |
| Cardiac-specific one-year mortalitya | 3.8 | 4.7 | 0.013 |
Among those discharged alive from index hospitalization
Table 2 compares selected patient characteristics among those with psychiatric diagnosis. There were 1,086 patients with any dementia (7.0% of all patients), 962 (6.2% of all patients) with any serious mental illness, and 1,536 (9.9%) with any depression. Patients with serious mental illness had the highest prevalence of substance abuse and service-connected disability; but were also younger and had lower CHF Index scores. Those with dementia were older, had higher CHF Index scores, and were more likely to have no primary care after discharge.
Table 2.
Comparisons among those with any mental illness, based on psychiatric diagnoses.+
| Dementia | Dementia plus other |
SMI | SMI plus other |
Depres- sion |
Anxiety | Depres- sion and anxiety |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n=687) | (n=399) | (n=564) | (n=398) | (n=1,214) | (n=505) | (n=322) | ||||
| Other predisposing variables | ||||||||||
| Homeless (percent) |
7.3 | 2.0 | c | 5.7 | 4.3 | 2.6 | 3.4 | 1.6 | ||
| Substance Use/Abuse |
10.3 | 16.3 | b | 31.9 | 34.7 | 23.1 | 20.0 | 24.8 | ||
| Less than 65 years of age |
6.8 | 8.5 | 55.5 | 54.5 | 33.1 | 28.9 | 30.8 | |||
| 65 to 74 years | 21.4 | 23.6 | 23.6 | 22.6 | 33.0 | 32.3 | 32.9 | |||
| 75 to 79 years | 26.5 | 31.6 | 11.4 | 14.8 | 18.0 | 22.4 | 21.7 | |||
| 80+ years | 45.3 | 36.3 | b | 9.6 | 8.0 | 15.9 | 16.4 | 14.6 | ||
| White | 67.4 | 79.0 | c | 64.5 | 71.6 | a | 79.6 | 77.2 | 85.4 | a |
| Black | 23.9 | 15.3 | b | 29.6 | 19.4 | c | 13.3 | 15.4 | 8.4 | a |
| Other race | 8.7 | 5.8 | 5.8 | 9.0 | 7.2 | 7.3 | 6.2 | |||
| Married | 50.8 | 53.4 | 39.0 | 43.0 | 49.2 | 54.1 | 50.0 | |||
| Service- Connected (SC) condition>10% |
22.8 | 41.6 | c | 55.7 | 58.0 | 22.5 | 19.2 | 25.8 | ||
| Individual need variables | ||||||||||
| CHF Index | ||||||||||
| 1 | 8.6 | 11.3 | 37.2 | 35.9 | 25.4 | 23.0 | 23.0 | |||
| 2 | 42.8 | 39.4 | 33.2 | 36.9 | 40.0 | 39.0 | 40.4 | |||
| 3 | 27.7 | 34.1 | a | 17.9 | 17.3 | 21.6 | 24.4 | 23.9 | ||
| 4 | 11.5 | 8.3 | 6.0 | 4.8 | 6.0 | 6.7 | 5.3 | |||
| 5 | 4.8 | 3.0 | 1.8 | 2.0 | 2.5 | 2.8 | 3.7 | |||
| 6 | 4.7 | 4.0 | 3.9 | 3.0 | 4.4 | 4.2 | 3.7 | |||
| Elixhauser Comorbidities | ||||||||||
| Peripheral vascular disorders |
7.1 | 4.8 | 6.7 | 6.0 | 9.0 | 5.4 | 5.6 | a | ||
| Chronic pulmonary disease |
16.0 | 22.8 | b | 22.0 | 20.1 | 21.4 | 22.4 | 21.7 | ||
| Diabetes (no complications) |
28.5 | 29.6 | 31.0 | 33.2 | 32.2 | 27.3 | 29.5 | |||
| Diabetes (with complications) |
5.2 | 4.8 | 5.3 | 8.3 | 9.5 | 6.5 | 6.5 | |||
| Hyperthyroidism | 8.9 | 5.3 | a | 3.9 | 5.0 | 5.7 | 7.1 | 7.1 | ||
| Renal failure | 7.0 | 4.0 | a | 4.4 | 5.0 | 7.1 | 5.0 | 4.7 | ||
| Cancer (tumor) | 7.9 | 6.5 | 3.4 | 4.5 | 6.2 | 4.6 | 7.4 | |||
| Fluid and electrolyte disorders |
11.6 | 9.8 | 9.4 | 8.5 | 9.0 | 9.3 | 10.2 | |||
| Deficiency anemias |
15.3 | 18.0 | 13.3 | 11.3 | 14.9 | 13.9 | 16.8 | |||
| Hypertension | 40.0 | 40.1 | 41.3 | 44.5 | 42.6 | 40.0 | 40.7 | |||
| Obesity | 2.0 | 3.0 | 7.4 | 8.5 | 7.0 | 4.8 | 7.8 | |||
| Prior CHF hospitalization |
22.3 | 31.3 | b | 18.1 | 23.4 | a | 24.2 | 25.7 | 26.4 | |
| Index hospitalization LOS |
8.7 (13.9) |
8.6 (13.6) |
6.7 (7.3) |
6.8 (8.1) |
7.7 (11.5) |
7.2 (13.8) |
7.5 (18.1) |
|||
| Health care utilization | ||||||||||
| Year prior to index hospitalization | ||||||||||
| 0 primary care visits |
14.4 | 6.0 | c | 10.8 | 2.8 | c | 4.9 | 4.4 | 1.6 | a |
| 1 to 4 primary care visits |
33.3 | 26.3 | a | 26.6 | 19.6 | a | 20.1 | 16.8 | 15.8 | |
| 5 to 8 primary care visits |
21.4 | 22.8 | 24.8 | 23.4 | 24.5 | 27.7 | 29.2 | |||
| 9 to 15 visits | 17.5 | 26.8 | c | 20.4 | 32.9 | c | 29.1 | 25.2 | 30.1 | |
| 16 or more visits | 13.4 | 18.0 | a | 17.4 | 20.8 | 21.5 | 25.9 | 23.3 | ||
| Any mental health visits |
22.1 | 65.7 | c | 75.4 | 91.7 | c | 40.8 | 39.0 | 69.6 | c |
| Year after index hospitalization+ | ||||||||||
| 0 primary care visits |
31.8 | 23.4 | b | 12.5 | 9.7 | 11.3 | 11.3 | 10.6 | ||
| 1 to 4 primary care visits |
30.4 | 30.5 | 26.1 | 21.4 | 22.4 | 25.0 | 23.5 | |||
| 5 to 8 primary care visits |
17.8 | 17.9 | 23.1 | 19.1 | 21.5 | 22.5 | 19.3 | |||
| 9 to 15 primary care visits |
12.8 | 17.9 | a | 21.0 | 29.0 | b | 26.0 | 22.3 | 22.8 | |
| 16 or more visits | 7.2 | 10.4 | 17.3 | 20.9 | 18.9 | 19.0 | 23.8 | |||
| Any mental ealth visits |
12.9 | 42.3 | c | 60.0 | 71.3 | c | 31.0 | 27.6 | 52.1 | c |
| Outcomes | ||||||||||
| Died in hospital | 11.1 | 8.8 | 4.8 | 3.8 | 4.9 | 4.0 | 3.4 | |||
| All-cause one- year mortality |
20.3 | 13.5 | b | 11.4 | 8.6 | 13.2 | 13.4 | 8.7 | ||
| Cardiac-specific one-year mortality |
6.2 | 4.1 | 4.5 | 3.1 | 5.0 | 4.7 | 3.2 | |||
p<0.05,
p< 0.01,
p<0.001
Comparisons are dementia vs. dementia plus other psychiatric diagnosis; SMI vs. SMI plus depression and/or anxiety ; Depression vs. Anxiety vs. Depression & Anxiety
Among those having any psychiatric diagnosis, there were differences between those having just one type of illness and more than one, such as dementia only vs. dementia plus other mental illness. Not surprisingly, those with multiple psychiatric diagnoses were more likely to have received outpatient mental health care. There were racial differences across all categories, with Whites being more likely to have multiple psychiatric diagnoses. Most of the variation within specific mental health categories was between those having dementia only and those having dementia and another type of mental illness. For patients having dementia or serious mental illness, those with multiple psychiatric diagnoses were more likely to have been admitted for CHF in the year preceding index admission and had more primary care visits in the years before and after the index hospitalization. Psychiatric comorbidity within depression and anxiety did not influence frequency of primary care.
Table 3 presents the multivariable analysis examining the influence of mental illness on mortality during the index hospitalization and one-year mortality (both all cause and cardiac specific). Dementia, by itself or in combination with other psychiatric diagnoses, was the only mental illness positively associated with mortality during the index hospitalization (compared to heart failure patients without mental illness diagnoses). Depression by itself was positively associated with both all cause and cardiac-specific one-year mortality.
Table 3.
Logistic regression models for mortality.
| Died in index hospitalization OR (95% CI) |
One year mortality+ OR (95% CI) |
Cardiac-specific one-year mortality OR (95% CI) |
||||
|---|---|---|---|---|---|---|
|
Primary predisposing individual variables |
||||||
| No mental illness | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| Dementia only | 2.09 (1.54–2.83) | c | 1.19 (0.94–1.51) | 1.10 (0.76–1.59) | ||
| Dementia plus any other mental illness |
1.74(1.13–2.70) | b | 0.80(0.57–1.12) | 0.82(0.47–1.44) | ||
| Serious mental illness (SMI) only | 1.44 (0.92–2.27) | 1.27 (0.93–1.74) | 1.46 (0.91–2.34) | |||
| SMI plus depression and/or anxiety | 1.00 (0.54–1.86) | 0.98 (0.66–1.46) | 1.09 (0.58–2.05) | |||
| Depression only | 1.18 (0.86–1.61) | 1.30 (1.07–1.59) | b | 1.37 (1.02–1.85) | a | |
| Anxiety only | 0.86 (0.51–1.43) | 1.27 (0.95–1.72) | 1.18 (0.74–1.88) | |||
| Depression and anxiety | 0.71 (0.36–1.40) | 0.74 (0.48–1.15) | 0.83 (0.42–1.62) | |||
| Other mental illness | 1.53 (1.02–2.31) | a | 1.41 (1.06–1.88) | a | 1.22 (0.77–1.93) | |
|
Other predisposing individual variables |
||||||
| Less than 65 years of age | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| 65 to 74 years | 1.55 (1.19–2.02) | b | 1.13 (0.95–1.34) | 1.05 (0.81–1.37) | ||
| 75 to 79 years | 1.44 (1.06–1.96) | a | 1.21 (1.00–1.48) | 1.16 (0.85–1.57) | ||
| 80+ years | 1.91 (1.41–2.58) | c | 1.27 (1.04–1.56) | a | 1.06 (0.77–1.46) | |
| White | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| Black | 0.73 (0.57–0.93) | a | 0.81 (0.69–0.94) | b | 0.75 (0.59–0.96) | a |
| Other race | 0.82 (0.59–1.16) | 0.84 (0.70–1.04) | 0.79 (0.55–1.15) | |||
| Female | 1.00 (0.50–1.96) | 1.07 (0.69–1.65) | 0.58 (0.23–1.44) | |||
| Married | 0.98 (0.83–1.15) | 1.18 (1.06–1.33) | b | 1.24 (1.04–1.48) | a | |
| Homeless | 1.42 (0.97–2.10) | 0.67 (0.52–0.86) | b | 0.62 (0.40–0.96) | a | |
| Substance Use/Abuse | 1.04 (0.82–1.32) | 0.95 (0.81–1.11) | 1.04 (0.82–1.31) | |||
| Service-Connected (SC) condition>10% |
1.15 (0.95–1.39) | 1.28 (1.12–1.46) | c | 0.97 (0.79–1.20) | ||
| Enabling contextual | ||||||
| Metro County, greater than 1,000,000 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| Metro County, less than 1,000,000 | 1.29 (0.98–1.69) | 0.75 (0.62–0.91) | b | 0.76 (0.56–1.03) | ||
| Non-Metro County | 1.18 (0.90–1.55) | 0.68 (0.56–0.82) | c | 0.75 (0.56–1.00) | ||
| VAMC has no medical school affiliation |
4.16 (0.34–51.62) | 2.18 (0.38–12.39) | 20.64 (0.62–68.72) | |||
| # of veterans served in Fiscal Year 01 (1,000’s) |
1.07 (0.66–1.72) | 1.10 (0.78–1.54) | 1.45 (0.67–3.11) | |||
| Individual need variables | ||||||
| CHF Index | ||||||
| 1 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| 2 | 1.81 (1.29–2.53) | b | 1.61 (1.33–1.94) | c | 1.28 (0.96–1.69) | |
| 3 | 2.75 (1.90–3.98) | c | 1.98 (1.59–2.46) | c | 1.66 (1.20–2.31) | b |
| 4 | 5.01 (3.33–7.54) | c | 2.27 (1.73–2.98) | c | 1.59 (1.04–2.42) | a |
| 5 | 9.01 (5.78–14.04) | c | 1.88 (1.32–2.68) | b | 1.00 (0.54–1.84) | |
| 6 | 13.79 (9.23–20.61) | c | 1.84 (1.32–2.57) | c | 1.61 (0.97–2.67) | |
| Elixhauser comorbidities | ||||||
| Peripheral vascular disorders | 0.87 (0.64–1.19) | 1.40 (1.17–1.68) | c | 1.23 (0.93–1.64) | ||
| Chronic pulmonary disease | 0.88 (0.72–1.07) | 0.88 (0.76–1.01) | 1.01 (0.81–1.25) | |||
| Diabetes (no complications) | 0.96 (0.80–1.16) | 1.12 (1.00–1.26) | 1.13 (0.94–1.36) | |||
| Diabetes (with complications) | 0.97 (0.68–1.40) | 1.38 (1.10–1.73) | b | 1.50 (1.07–2.09) | b | |
| Hyperthyroidism | 0.65 (0.45–0.93) | a | 1.29 (1.04–1.60) | a | 1.59 (1.17–2.17) | b |
| Renal failure | 1.55 (1.19–2.02) | b | 1.13 (0.89–1.42) | 1.27 (0.90–1.79) | ||
| Cancer (tumor) | 0.87 (0.63–1.21) | 1.21 (0.98–1.49) | 0.73 (0.50–1.07) | |||
| Fluid and electrolyte disorders | 1.65 (1.33–2.05) | c | 0.83 (0.68–1.01) | 0.72 (0.52–0.99) | a | |
| Deficiency anemia | 0.79 (0.63–0.99) | a | 1.06 (0.92–1.22) | 1.03 (0.83–1.29) | ||
| Hypertension | 0.51 (0.43–0.62) | c | 0.84 (0.75–0.94) | b | 0.79 (0.66–0.94) | b |
| Obesity | 1.00 (0.65–1.54) | 0.64 (0.47–0.86) | b | 0.58 (0.35–0.94) | a | |
| Prior CHF hospitalization | 2.41 (2.02–2.88) | a | 1.33 (1.17–1.51) | c | 1.24 (1.01–1.51) | a |
| Index hospitalization length of stay (log) |
N/A | 1.12 (1.05–1.20) | b | 1.08 (0.97–1.19) | ||
| Health care utilization+ | ||||||
| 0 primary care visits | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | |||
| 1 to 4 primary care visits | 0.66 (0.48–0.93) | a | 0.61 (0.53–0.71) | c | 0.96 (0.76–1.22) | |
| 5 to 8 primary care visits | 0.73 (0.52–1.02) | 0.29 (0.25–0.35) | c | 0.48 (0.36–0.63) | c | |
| 9 to 15 primary care visits | 0.66 (0.47–0.93) | a | 0.20 (0.16–0.24) | c | 0.24 (0.17–0.34) | c |
| 16 or more visits | 0.62 (0.43–0.89) | b | 0.11 (0.09–0.14) | c | 0.17 (0.11–0.25) | c |
| Any mental health visits | 0.96 (0.73–1.25) | 0.70 (0.58–0.85) | c | 0.66 (0.48–0.90) | a |
p<0.05,
p< 0.01,
p<0.001
For index mortality, utilization is for year preceding admission. For one-year mortality, utilization is for year following discharge among those discharged alive.
Consistent with other VA research, Black veterans were less likely to die than were White veterans.35 Increasing age was positively associated with index and one-year all cause mortality, but not cardiac-specific mortality. Mortality risk after discharge was greater among those who were married (unexpectantly)36 and those who were homeless. A modest contextual relationship was found in that those living in less populated counties had lower risk of all-cause one year mortality. As would be expected, nearly every individual need measure was associated with mortality. Receipt of primary care generally decreased the likelihood of mortality, with the strongest associations being following discharge.
Table 4 summarizes the logistic regression analyses. Comparison of the area under the curve for increasingly complete models allows one to see the relative contribution of each component of the Behavioral Model. Measures of individual need were the largest single contributor to explained variation for index mortality (during hospitalization), followed by other predisposing characteristics. However, predisposing characteristics were the single largest contributor to the all-cause mortality (in the year following the index hospitalization) model, followed by healthcare utilization measures. Contextual measures were the single largest contributor to explained variation of cardiac-specific mortality (in the year following the index hospitalization), followed by healthcare utilization and other predisposing characteristics.
Table 4.
Receiver Operator Curve (ROC) analysis of mortality logistic regression models+.
| Died in index hospitalizat ion |
All-cause one year mortality |
Cardiac – specific one year mortality |
||||
|---|---|---|---|---|---|---|
| Area Under the Curve |
Gain in AUC |
Area Under the Curve |
Gain in AUC |
Area Under the Curve |
Gain in AUC |
|
| No variables (random) | 0.5000 | 0.5000 | 0.5000 | |||
| Adding primary predisposing (mental illness) |
0.5630 | 0.0630 | 0.5424 | 0.0424 | 0.5342 | 0.0342 |
| Adding other predisposing variables |
0.6441 | 0.0811 | 0.6138 | .0714 | 0.5867 | 0.0525 |
| Adding enabling contextual | 0.6982 | 0.0541 | 0.6570 | 0.0432 | 0.6625 | 0.0758 |
| Adding individual need | 0.8093 | 0.1111 | 0.6994 | .0424 | 0.6963 | 0.0338 |
| Adding health care utilization | 0.8104 | 0.0011 | 0.7642 | .0648 | 0.7556 | 0.0593 |
Results from successively forcing in each block of variables. The final result represents the full models shown in Table 3.
DISCUSSION
In this national, cross-sectional sample of veterans hospitalized for congestive heart failure, a Behavioral Model of Health Services Utilization approach was used to examine the influence of comorbid mental illness on index mortality and one-year mortality. Our finding that roughly one-third of deaths were cardiovascular specific are consistent with a Medicare study which found that non-cardiovascular causes were responsible for 57% of inpatient costs in the year following heart failure discharge.37 Special attention was paid to the issue of multiple psychiatric diagnoses and the influence of outpatient care.
Dementia, whether by itself or in conjunction with another psychiatric diagnosis, was the only mental illness among heart failure patients found to be an independent risk factor for increased inpatient mortality. Our findings of an increased mortality risk (after adjusting for increased age and medical severity relative to all other veterans) is consistent with earlier research involving acute myocardial infarction (AMI) among Medicare patients6 -- patients with dementia had roughly twice the unadjusted mortality rate of those without dementia However, Sloan, et al. (2004) included more clinical measures than are included in our study and obtained less dramatic (though still significant) odds ratios. They also found that dementia patients were half as likely to receive invasive treatments as AMI patients not having dementia.
Depression, (without other psychiatric diagnoses) was found to be an independent risk factor for both all-cause and cardiac-specific one-year mortality. Patient behavior may be a potential reason for the greater impact of mental illness on longer-term mortality. Successful management of congestive heart failure usually requires major lifestyle changes (healthy diet, physical activity, symptom monitoring, medication, etc.) by patients and their families. Depression among CHF patients has been associated with not following these recommended diet / exercise / medication regimens.38
Receipt of primary care services during the year preceding admission was associated with reduced mortality during the index hospitalization and primary care in the year following discharge was associated with reduced risk of one-year mortality. Veterans with any mental illness were no less likely to have had primary care visits than those without a psychiatric diagnosis. The notable exception being patients diagnosed with dementia – they were less likely to receive primary care. These findings are consistent with others who have concluded that mental illness is not a major barrier to ambulatory care in the VA.18 Thus, it does not appear that differences in primary care visits contribute to the increased risk one-year mortality of veterans with mental illness.
Paradoxically, patients with more complex psychiatric needs, i.e., multiple types of mental illness, had comparable or even lower risk of one-year mortality than those having just one of the previously mentioned mental illnesses. The higher one-year mortality rates observed among those with only one type of psychiatric diagnosis is worthy of further research and suggests an area for improvement. Differences in physical health status generally did not appear to be a major factor among those with any mental illness, except that those with dementia only tended to be older and have more physical comorbidities compared to those with dementia and another psychiatric diagnosis.
The increased use of mental health services among those with multiple psychiatric diagnoses may have led to greater overall treatment of such individuals. These results are consistent with Kunik, et al. who found that veterans with dementia and another psychiatric diagnosis utilize more mental and physical health services than those with only dementia.39 Comparing single to multiple psychiatric diagnoses, we consistently found those with a single diagnoses were more likely to have had no primary care visits in the year preceding the index hospitalization: dementia 14.4% (single) vs. 6.0% (multiple), serious mental illness 10.8% (single) vs. 2.8% (multiple), and depression 4.9% (single) vs. 1.6% (multiple). Greater emphasis on linkage to outpatient care for those with dementia or serious mental illness might contribute to reduced mortality rates.
The fact that more than half of the heart failure patients with a serious mental illness were less than 65 years of age further underscores the need for patients with schizophrenia to be more aggressively monitored for cardiovascular health.7 Regular monitoring is especially important since those with serious mental illness are less likely to use primary care,40 though we found that patients with serious mental illness had comparable primary care utilization compared to those having no mental illness.
LIMITATIONS
This study employed a retrospective design using administrative data. Studies based on administrative data alone are subject to concerns about clinical credibility, since ICD-9-CM codes may not accurately and completely describe the patient’s clinical situation.41 This is true for both heart failure severity and mental illness. However, the trade-off for lack of clinical specificity is the generalizability of a large national sample. Furthermore, it has been shown that administrative data is nearly as good as medical record data in predicting heart failure aggregated mortality rates42 and our inpatient mortality results are similar to other VA researchers who combined administrative and laboratory data.16 It has been suggested that relationships between psychiatric diagnosis and CHF mortality are affected by whether one uses inpatient or outpatient data to classify patients.16 Since we used both inpatient and outpatient diagnoses, with receipt of mental health services as a covariate and a hierarchical assignment to categories, accounting for psychiatric comorbidity, we should have a more stable estimate of the true relationship between psychiatric illness and mortality.
Results may not generalize to civilian populations since the VA historically treats a male clientele that is older, poorer, less educated and sicker than the general population.43 However, a recent analysis of Medicare data found that 39% of congestive heart failure patients had five or more non-cardiac comorbid conditions.44 With rising Medicare co-payments, income differences between elderly VA and Medicare patients may be less than during the time our data were collected. Furthermore, there have been advances in treatment and practice, for example, in 2007 the VA released primary care clinical guidelines for CHF management.45 However, a recent VA intervention study to improve behaviors, such as exercise, did not find a difference in one-year mortality.46 It is not clear if treatment changes in the last few years would substantially alter the findings regarding dementia and depression.
SUMMARY
This analysis, guided by the Behavioral Model of Health Services, of heart failure outcomes among veterans found that mental illness was associated with other personal characteristics that are independent predictors of mortality. As expected, individual need was a strong predictor of mortality. Most veterans received primary care, and greater receipt of primary care was associated with lower inpatient and one-year mortality. Dementia was positively associated with inpatient mortality and depression was positively associated with one-year mortality. Except for dementia, mental illness did not appear to be a barrier to primary care. This study further highlights the importance of mental illness on mortality for veterans with heart failure; but suggests, with the exception of dementia, that differences in patterns of primary care treatment are not responsible for the increased mortality risk of having a psychiatric diagnosis. Congestive heart failure patients with two or more types of mental illness do not have higher mortality rates than those with only one type of mental illness. A greater number of outpatient visits may partially explain that benefit.
ACKNOWLEDGMENTS
We thank Jim Mintz, PhD, for assistance in preliminary study design and obtaining data and Abdelmonem A. Afifi, PhD, for statistical advice in preparing the aecepted manuscript. The study was supported by the Department of Veterans Affairs (VA) Desert Pacific Mental Illness Research, Education, and Clinical Center (MIRECC). J.E.B, received funding from the Substance Abuse and Mental Health Services Administration (T26 OA00055-0I); R.M.A. and W.E.C, were supported in part by the UCLA-Drew Project Export, National Institutes of Health (NIH), National Center on Minority Health and Health Disparities (P20-MD00148-01), and the UCLA Center for Health Improvement in Minority Elders/Resource Centers for Minority Aging Research, NIH, National Institute of Aging, (AG-02-004).
REFERENCES
- 1.Fang J, Mensah GA, Croft JB, Keenan NL. Heart Failure-Related Hospitalization in the U.S., 1979 to 2004. Journal of the American College of Cardiology. 2008;52(6):428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 2.Havranek EP, Wolfe P, Masoudi FA, Rathore SS, Krumholz H, Ordin DL. Provider and Hospital Characteristics Associated with Geographic Variation in the Evaluation and Management of Elderly Patients with Heart Failure. Archives of Internal Medicine. 2004;164(11):1186–1191. doi: 10.1001/archinte.164.11.1186. [DOI] [PubMed] [Google Scholar]
- 3.Sayers SL, Hanrahan N, Kutney A, Clarke SP, Reis BF, Reigel B. Psychiatric comorbidity and greater hospitalization risk, longer length of stay, and higher hospitalization costs in older adults with heart failure. Journal of the American Geriatrics Society. 2007;55(10):1585–1591. doi: 10.1111/j.1532-5415.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 4.Rathore SS, Wang Y, Druss BG, Masoudi FA, Krumholz HM. Mental Disorders, Quality of Care, and Outcomes Among Older Patients Hospitalized With Heart Failure: An Analysis of the National Heart Failure Project. Archives of General Psychiatry. 2008;65(12):1402–1408. doi: 10.1001/archpsyc.65.12.1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.York KM, Hassan M, Sheps DS. Psychobiology of depression/distress in congestive heart failure. Heart Failure Review. 2009;14:35–40. doi: 10.1007/s10741-008-9091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sloan FA, Trogdon JG, Curtis LH, Schulman KA. The Effect of Dementia on Outcomes and Process of Care for Medicare Beneficiaries Admitted with Acute Myocardial Infarction. Journal of the American Geriatrics Society. 2004;52(2):173–181. doi: 10.1111/j.1532-5415.2004.52052.x. [DOI] [PubMed] [Google Scholar]
- 7.Marder SR, Essock SM, Miller AL, et al. Physical Health Monitoring of Patients With Schizophrenia. American Journal of Psychiatry. 2004;161(8):1334–1349. doi: 10.1176/appi.ajp.161.8.1334. [DOI] [PubMed] [Google Scholar]
- 8.Weitoft GR, Gullberg A, Rosen M. Avoidable Mortality Among Psychiatric Patients. Social Psychiatry and Psychiatric Epidemiology. 1998;33:430–437. doi: 10.1007/s001270050076. [DOI] [PubMed] [Google Scholar]
- 9.Redwine L, Wirtz P, Hong S, et al. A potential shift from adaptive immune activity to nonspecific inflammatory activation associated with higher depression symptoms in chronic heart failure patients. Journal of Cardiac Failure. 2009;15(7):607–615. doi: 10.1016/j.cardfail.2009.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laursen TM, Munk-Olsen T, Agerbo E, Gasse C, Mortensen PB. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Archives of General Psychiatry. 2009;66(7):713–720. doi: 10.1001/archgenpsychiatry.2009.61. [DOI] [PubMed] [Google Scholar]
- 11.Druss BG. Improving Medical Care for Persons With Serious Mental Illness: Challenges and Solutions. Journal of Clinical Psychiatry. 2007;68 suppl 4:40–44. [PubMed] [Google Scholar]
- 12.QUERI. Quality Enhancement Research Initiative Chronic Heart Failure Fact Sheet: VA Office of Research and Development. Health Services Research and Development Service; 2008. [Google Scholar]
- 13.Kominski G, Andersen R, Bastani R, et al. UPBEAT: The Impact of a Psychogeriatric Intervention in VA Medical Centers. Medical Care. 2001;39(5):500–512. doi: 10.1097/00005650-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Campbell DG, Felker BL, Liu CF, et al. Prevalence of depression-PTSD comorbidity: implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine. 2007;22(6):711–718. doi: 10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Booth BM, Blow FC, Cook CAL. Persistence of Impaired Functioning and Psychological Distress after Medical Hospitalization for Men with Co-Occuring Psychiatric and Substance Use Disorders. Journal of General Internal Medicine. 2001;16:57–65. doi: 10.1111/j.1525-1497.2001.05099.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abrams TE, Vaughan-Sarrazin M, Rosenthal GE. Variations in the Associations Between Psychiatric Comorbidity and Hospital Mortality According to the Method of Identifying Psychiatric Diagnoses. Journal of General Internal Medicine. 2008;23(3):317–322. doi: 10.1007/s11606-008-0518-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andersen RM, Davidson PL. Improving Access to Care in America: Individual and Contextual Indicators. In: Andersen RM, Rice TH, Kominski GF, Andersen RM, Rice TH, Kominski GF, editors. Changing the U.S. Health Care System. Ed 3. San Francisco: Jossey-Bass; 2007. pp. 3–32. [Google Scholar]
- 18.Desai MM, Rosenheck RA, Kasprow WJ. Determinants of Receipt of Ambulatory Medical Care in a National Sample of Mentally Ill Homeless Veterans. Medical Care. 2003;41(2):275–287. doi: 10.1097/01.MLR.0000044907.31129.0A. [DOI] [PubMed] [Google Scholar]
- 19.McCarthy JF, Blow FC, Kales HC. Disruptive behaviors in Veteran Affairs nursing home residents: How different are residents with serious mental illness? Journal of the American Geriatrics Society. 2004;52(12):2031–2038. doi: 10.1111/j.1532-5415.2004.52559.x. [DOI] [PubMed] [Google Scholar]
- 20.Gelberg L, Andersen RM, Leake B. The behavioral model for vulnerable populations: application to medical care use and outcome.s for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 21.Banta JE. PhD Dissertation. University of California Los Angeles; 2004. Utilization and Outcomes Among Inpatient Veterans Diagnosed With Congestive Heart Failure and Co-Morbid Mental Illness. UMI No. 3142463. [Google Scholar]
- 22.Yu W, Cowper D, Berger M, Kuebeler M, Kubal J, Manheim L. Using GIS to profile health-care costs of va quality-enhancement research initiative diseases. J Med Syst. 2004;28(3):271–285. doi: 10.1023/b:joms.0000032844.26308.95. [DOI] [PubMed] [Google Scholar]
- 23.Kubal JD, Cowper DC, Waight S, Hynes DM. VIRec Insights, no. 5. Hines, IL: VA Information Resource Center; 2000. A Primer on Major U.S. Mortality Databases Used in Health Services Researeh. [Google Scholar]
- 24.Cradoek-O’Leary J, Young AS, Yano EM, Wang M, Lee ML. Use of general medical services by VA patients with psychiatric di.sorders. Psyehiatr Serv. 2002;53(7):874–878. doi: 10.1176/appi.ps.53.7.874. [DOI] [PubMed] [Google Scholar]
- 25.Levirie SK, Sachs GA, Jin L, Meltzer D. A prognostic model for 1-year mortality in older adults after hospital discharge. Am J Med. 2007;120(5):455–460. doi: 10.1016/j.amjmed.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 26.Hines Edward J., Jr, editor. VIReC. The Medical SAS Inpatient Datasets - FY2000: A VIReC Resource Guide. VA Hospital. Hines, IL: Veterans Affairs Information Resource Center; 2001. [Google Scholar]
- 27.Bureau of Health Professions: Area Resource File (ARF) Access Sy.stem computer program. Fairfax, Virginia, Quality Resource Systems. 2004 [Google Scholar]
- 28.Stewart C, Demers C, Murdock D, et al. Substantial between-hospital variation in outcome following first emergency admission for heart failure. Eur Heart J. 2002;23:605–657. doi: 10.1053/euhj.2001.2890. [DOI] [PubMed] [Google Scholar]
- 29.Polanczyk CA, Rohde LE, Philbin EF, DiSalvo TG. A new casemix adjustment index for hospital mortality among patients with congestive heart failure. Med Care. 1998;36(10):1489–1499. doi: 10.1097/00005650-199810000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Polanczyk CA, Rohde LE, Dec GW, DiSalvo T. Ten-year trends in hospital care for congestive heart failure. Arch Intern Med. 2000;160:325–332. doi: 10.1001/archinte.160.3.325. [DOI] [PubMed] [Google Scholar]
- 31.Elixhauser A, steiner C, Harris DR, Coffey RM. Comorbodity measures for use with administartive data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Southern DA, Quan H, Ghali WA. Comparison of Elixhauser and Charlson/Deyo methods of comorbidity measurement in administratiave data. Med Care. 2004;42(4):355–360. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 33.Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can primary care visits reduce hospital utilization among medicare beneficiaries at the end of life. J Gen Intern Med. 2008;23(9):1330–1335. doi: 10.1007/s11606-008-0638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanley JA, McNeil BJ. The meaning and use of the area under the receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 35.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the veterans affairs health care system. JAMA. 2001;285(3):297–303. doi: 10.1001/jama.285.3.297. [DOI] [PubMed] [Google Scholar]
- 36.Sayers SL, Riegel B, Pawlowski S, Coyne JC, Samaha FF. Social support and self-care of patients with heart failure. Ann Behav Med. 2008;35(1):70–79. doi: 10.1007/s12160-007-9003-x. [DOI] [PubMed] [Google Scholar]
- 37.Whellan DJ, Grenier MA, Schulman KA, Curtis LH. Costs of inpatient care among Medicare beneficiaris with heart failure, 2001 to 2004. Circ Cardiovasc Qual Outcomes. 2010;3(1):33–40. doi: 10.1161/CIRCOUTCOMES.109.854760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jiang W, Alexander J, Cristpher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161(15):1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 39.Kunik ME, Snow AL, Molinari VA, et al. Healthcare utilization in dementia patients with psychiatric comorbidity. Gerontologist. 2003;43(1):86–91. doi: 10.1093/geront/43.1.86. [DOI] [PubMed] [Google Scholar]
- 40.Chwastiak LA, Rosenheck RA, Kazis LE. Utilization of primary care by veternas with psychiatric illness in the National Department of Veterans Affairs Health Care System. J Gen Intern Med. 2008;23(11):1835–1840. doi: 10.1007/s11606-008-0786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iezzoni LI. Data sources and implications: administrative data bases. In: Iezzoni LI, editor. Risk Adjustment for Measure Health Care Outcomes. Ann Arbor, MI: Health Administration Press; 1994. pp. 119–176. [Google Scholar]
- 42.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital preformance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113(13):1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 43.Rogers WH, Kazis LE, Miller DR, et al. Comparing the health status of VA and non-VA ambulatory patients: the veternas’ health and medical outcomes studies. J Ambul Care Manage. 2004;27(3):249–262. doi: 10.1097/00004479-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 44.Braunstein JB, Anderson GF, Gerstenblith G, et al. Noncardiac comorbidity increases preventable hospitalizations and mortality among medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42(2):1226–1233. doi: 10.1016/s0735-1097(03)00947-1. [DOI] [PubMed] [Google Scholar]
- 45.Department of Veterans Affairs. Pharmacy Benefits Management Strategic Healthcare Group and Meical Advisory Panel, Vterans Health Administration Department of Veterans Affairs Publication No. 00-0015. Washington, DC: VHA; 2007. Sep, PBM-MAP clinical practice guideline for the parmacologic management of chronic heart failure in primary care practice. [Google Scholar]
- 46.Copeland LA, Berg GD, Johnson DM, Bauer RL. An intervention for VA patients with congestive heart failure. Am J Manag Care. 2010;16(3):158–165. [PubMed] [Google Scholar]


