Abstract
Growing research has examined parental accommodation among the families of children with obsessive-compulsive disorder (OCD). However, these studies have utilized a parent-report (PR) version of a measure, the Family Accommodation Scale (FAS) that has never received proper psychometric validation. In turn, previously derived subscales have been developed via clinical rather than empirical evidence. This study aims to conduct a comprehensive psychometric analysis of the FAS-PR utilizing data collected from 96 youths with OCD. Exploratory factors analysis was conducted and revealed a 12-item scale yielding two separate, yet related subscales, Avoidance of Triggers (AT) and Involvement in Compulsions (IC). Subsequent analyses revealed good internal consistency and convergent and discriminant validity. These findings suggest that future research should seek to examine factors that may impact various facets to accommodation as well as the role these facets plays in predicting treatment outcome. Limitations are discussed.
Keywords: OCD, Accommodation, Assessment, Psychometrics
Research suggests that OCD runs a chronic and impairing course and affects between 1.5 and 2.2 million children in the United States (2% to 3% prevalence rate; Valleni-Basile et al. 1995; Zohar 1999) with a majority of these children also meeting diagnostic criteria for an additional psychiatric disorder (e.g., 75–84%) including attention-deficit hyper-activity disorder (ADHD), generalized anxiety (GAD) or other anxiety disorders, and tic disorders (Geller 2006). The disorder is associated with marked impairment in several areas of functioning, including academic performance, interpersonal relationships, and family functioning (Adams et al. 1994; Cooper 1996; Leonard et al. 1993; Toro et al. 1992).
It is commonly accepted that OCD can result in a marked, negative effect on both the child and their family (Waters and Barrett 2000). Some researchers have suggested that, within the context of the family, OCD demonstrates a bidirectional relationship. That is, families have an affect on and are affected by OCD suggesting that the interactions between the parent and child are of great importance (March 1995). In particular, the participation of family members in a child’s OCD-related rituals (i.e., accommodation) has received increasing attention.
The term accommodation is most often operationally defined as the participation of family member(s) in the ritual (s) of a child or adult with OCD. However, accommodation may take several forms, including aiding in completion of the ritual, facilitating avoidance of situations, events, or persons, or any other activity the family may perform in response to the individual’s OCD symptoms (Amir et al. 2000; Calvocoressi et al. 1995; Calvocoressi et al. 1999; Storch et al. 2007). Although this definition of accommodation is quite broad, it represents the current state of science’s understanding of this construct. Recently, Merlo et al. (2009) found that 88% of parents reported engaging in at least mild accommodation of their child’s OCD symptoms. Independent investigations have found similarly high rates of parental accommodation and suggest that accommodation is ubiquitous across the families of children with OCD (Mariaskin et al. 2007; Peris et al. 2008a, b).
Calvocoressi et al. (1999) developed a 12-item semi-structured, clinician-administered measure, the Family Accommodation Scale (FAS), to assess family accommodation among adults with OCD. The authors recruited 36 participant-relative dyads from three outpatient psychiatric clinics. Subsequent psychometric analyses revealed good internal consistency (α=0.82) and excellent reliability across raters (ICC for items ranged from 0.75 to 0.99). The scale demonstrated good convergent validity with measures of symptom severity (i.e., Yale-Brown Obsessive Compulsive Scale ([YBOCS]), family functioning (i.e., Family Assessment Device), and relative’s rejecting attitudes towards the participant (i.e., Five Minute Speech Sample) and also demonstrated good discriminant validity. More recently, Albert et al. (2010) conducted an exploratory factor analysis (EFA), utilizing an adult sample, on the FAS and found evidence for three distinct subscales (i.e., Modification, Distress and Consequences, and Participation) though these subscales demonstrated variable internal consistency ranging from 0.67 (i.e., Participation) to 0.76 (i.e., Modification). The authors noted a small, positive correlation with symptom severity (i.e., YBOCS total score) and significantly higher FAS scores among relatives (i.e., those completing the measure) with a current Axis I disorder and those presenting with a comorbid mood disorder. These data provide preliminary empirical support for use of a clinician-administered version of the FAS among the families of adults with OCD. However, limitations to this scale’s development hinder its use among the families of children with OCD.
Studies examining accommodation in children with OCD have utilized a modified, 13-item parent-report version of the scale (i.e., FAS-PR) rather than a semi-structured interview. The items constituting this adapted parent-report version are markedly different, both in content and structure, from those of the original FAS. No data exist to elucidate whether parental accommodation during childhood is a unitary or multidimensional construct. That is, are facets of accommodation germane to adults (i.e., Modification, Distress and Consequences, and Participation; Albert et al. 2010) also applicable to children? Peris et al. (2008b) are the only researchers to examine potential facets to accommodation in any manner among children. The authors constructed three subscales (Total Involvement [nine items; e.g., “Have you modified your family routine because of the patient’s symptoms”], Consequences [three items; e.g., “Has the patient become distressed/anxious when you have not provided assistance?”], and Distress [one item]) from FAS-PR items. While possibly demonstrating face validity, these subscales were developed utilizing clinical judgment rather than empirical evidence. Previous child OCD studies have utilized only a total score from the FAS-PR constructed by summing all scale items. Collectively, these limitations suggest substantial room for improvement in the assessment of parental accommodation.
Albeit limited by the methodological shortcomings noted above, available research suggests a positive association between accommodation and symptom severity (i.e., Child-YBOCS), internalizing symptoms (e.g., anxiety), impact of the disorder (i.e., Child Obsessive-Compulsive Impact Scale [COIS]), and parental symptoms of psychopathology (Peris et al. 2008b; Storch et al. 2007) among children with OCD. Interestingly, Merlo et al. (2009) recently found that changes in parental accommodation (assessed via the 13-item FAS-PR) predicted treatment response to cognitive-behavior therapy (CBT) among children. Given these preliminary findings and the potential treatment implications, it seems prudent for researchers to explore whether the FAS-PR provides a reliable and valid assessment of accommodation among the parents of children with OCD.
To date, all studies examining accommodation in childhood OCD have used utilized the same measure, the FAS-PR (Mariaskin et al. 2007; Merlo et al. 2009; Peris et al. 2008b; Storch et al. 2007). Unfortunately, the factor structure, reliability, and validity of the FAS-PR have yet to be examined. As such, available empirical evidence regarding the role of accommodation among children with OCD should be examined with some degree of caution. Given the potential treatment implications, it is important that the field more aptly characterizes parental accommodation. Previous studies have lacked the sample size necessary to adequately examine this scale’s factor structure. As a result, the primary objective of the current study is to examine the factor structure of the FAS-PR utilizing EFA and to subsequently examine the scale’s reliability (i.e., internal consistency) and construct validity (i.e., convergent, discriminant). In an exploratory analysis, we also intend to examine whether parental accommodation is related to child age or gender.
Methods
Participants
Participants were recruited as part of the Pediatric OCD Treatment Study (POTS), to examine the efficacy of CBT alone, pharmacotherapy alone (i.e., sertraline), and combined therapy, as compared to placebo for the treatment of youths (7–17 years of age) with OCD (POTS 2004). The background and rationale for the POTS have been described elsewhere (Franklin et al. 2003). Three sites participated in this study: Duke University, the University of Pennsylvania (Penn), and, under a subcontract to Penn, Brown University. Informed consent was obtained from all participants.
To mirror a sample more representative of a treatment-seeking population, inclusion criteria were kept to a minimum (Franklin et al. 2003; POTS 2004). Briefly, inclusion into the larger study required: meeting diagnostic criteria for OCD as obtained jointly on the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al. 1997) and the Anxiety Disorder Interview Schedule for Children (ADIS-C; Silverman and Albano 1996); a CY-BOCS score of 16 or higher; NIMH Global Severity Score greater than 7 (Goodman and Price 1992); IQ greater than 80; and being free of antiobsessional medication prior to the start of the study. Additionally, families participating in the current study were required to have completed the FAS-PR at baseline with less than 15% missing data (i.e., omitting one or fewer items).
In total, 96 youths met inclusion criteria for the current study. The sample was 51% girls (n=49), predominantly Caucasian (93.8%, n=90), and ranged in age from 7 to 17 years old (M=11.6, SD=2.7). Per data obtained via administration of the ADIS-C, GAD (36.5%, n=35), specific phobia (29.2%, n=28), ADHD (i.e., combined, inattentive, or hyperactive type; 20.8%, n=20), tic disorder (17.7%; n=17), separation anxiety disorder (SAD; 15.6% %, n=15), and oppositional defiant disorder (ODD; 8.3%, n=8) were among the most common comorbid diagnoses.
Demographic information was also obtained from parents completing baseline measures. Fifty percent (n= 49) of parents were mothers. Fathers ranged in age from 32 to 60 (M=43.6 years, SD=6.3), while mothers ranged in age from 29 to 52 (M=40.5 years, SD=5.5). Mothers and fathers each reported a modal highest degree completed of “college degree.” The modal number of siblings in the home was two. The median primary (n=90) and secondary incomes (n=14) among families was $60,000–$69,000.
Procedure
Entrance into the larger study POTS (2004) took an average of 2–3 weeks and proceeded through 4 entry gates: (1) telephone screening, (2) review of youth- and parent-report measures, (3) consent and assessment of all inclusion and exclusion criteria and (4) baseline assessment and randomization to treatment condition. CY-BOCS data was obtained jointly from both the child and at least one parent. During the baseline assessment, all remaining measures were completed by either the child or parent individually. Depending upon the severity of the child’s OCD-related symptoms, the duration of this assessment ranged from 60 to 90 min.
Instruments
Child Measures of Psychopathology
Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; Scahill et al. 1997)
The CY-BOCS is a 10-item clinician-administered instrument assessing OCD obsessions (scores ranging from 0 to 20), compulsions (scores ranging from 0 to 20), and total (scores ranging from 0 to 40) symptom severity in youths. Higher total and subscale scores indicate greater or more severe obsessions and/or compulsions. Past research suggests that the CY-BOCS is both a reliable and valid instrument for the assessment of symptom severity amongst youths with OCD (Scahill et al. 1997).
Multidimensional Anxiety Scale for Children (MASC; March 1998)
The MASC is a 39-item self-report scale assessing anxiety that yields an overall and four subscale scores. MASC items are rated on a 4-point Likert scale with scores ranging from 0 (never true about me) to 3 (often true about me). For the purposes of the current study, only the MASC total T-score was utilized. Higher T-scores indicate increasing symptoms of anxiety. Research has demonstrated good internal consistency for the overall MASC score and acceptable test-retest reliability (3 months; March 1998). In addition, the MASC has demonstrated adequate convergent and divergent validity (March 1998; Wood et al. 2002).
Child OCD Impact Scale-Child Report (COIS-C)
The COIS-C is a child self-report on the impact that OCD symptoms have on a child’s psychosocial functioning. The COIS-C covers functioning in home, school, and social domains. COIS-C items are rated on a 4-point Likert scale with scores ranging from 0 (not at all) to 3 (very much). The COIS-C global T-score was used for this study. The scale has excellent internal consistency and preliminary evidence suggests the measure has adequate concurrent validity (Piacentini et al. 2003).
Piers-Harris Children’s Self-Concept Scale (Piers-Harris; Piers and Harris 1969)
The Piers-Harris is an 80-item child-report scale assessing a variety of domains relating to self-concept (i.e., intellectual and school status, physical appearance and attributes, popularity). In turn, the scale yields a total score, as well as several subscale scores. For the purposes of this study, the Piers-Harris total T-score was used. Importantly, higher T-scores represent greater/healthier self-concept. Available empirical evidence suggests that the scale demonstrates excellent internal consistency and good concurrent validity (Simola and Holden 1992).
Child and Adolescent Trauma Survey (CATS; March et al. 1997)
The CATS is a 12-item self-report scale designed to assess symptoms resulting from stressful and traumatic events (based upon a symptom checklist provided to the child) that children may experience. The scale yields a total, as well as several subscale scores. For the purposes of this study, the CATS total score was used. Higher scores indicate increasing symptoms of trauma or stress. The scale has demonstrated excellent internal consistency (J. S. March et al. 1997) and has been used frequently in research as a screening tool and outcome measure for traumatic life events in children (March et al. 1998; Suliman et al. 2005).
Parent Measures of Psychopathology/Behavior
Family Accommodation Scale-Parent Report (FAS-PR)
The FAS-PR is a 13-item parent-report measure designed to assess accommodation of a child’s OCD-related behaviors over the previous month. In an effort to assess multiple dimensions to accommodations (rather than one in isolation), items are anchored with respect to either frequency or magnitude utilizing a 5-pt Likert scale ranging from 0 (Never) to 4 (Daily) with higher scores indicating greater parental accommodation. To ensure that Total and subscale scores were not adversely influenced by a parent’s omission of an item when completing the scale (n=4, 4.2%) mean: item, subscale, and total scores are presented throughout and are utilized for analysis of convergent and discriminant validity.
Brief Symptom Inventory (BSI) (Derogatis and Melisaratos 1983)
The BSI is an adult self-report measure of psychological symptoms. The measure yields global severity scores indicating the total number of symptoms and severity of the distress, as well as nine primary symptom subscales. Participants rate items utilizing a 5-pt Likert scale ranging from 0 (not at all) to 4 (extremely). For the purposes of the current study, the T-score of the Global Symptom Index was used. Higher T-score represent increasing symptoms of psychopathology. The BSI has demonstrated good reliability (i.e., test-retest reliability and internal consistency) and convergent validity (Derogatis and Melisaratos 1983).
Results
Exploratory Factor Analysis (EFA)
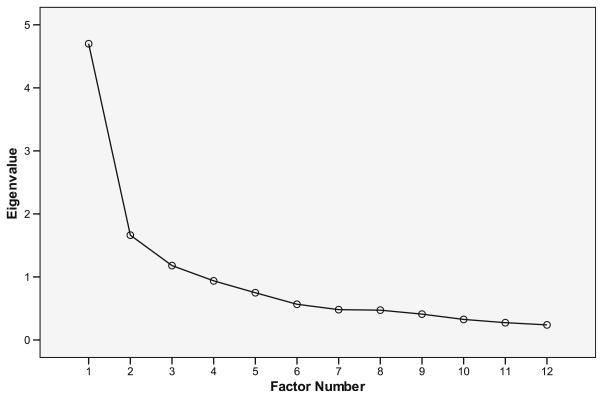
To examine the factor analytic structure of the FAS-PR, an EFA was performed. An EFA was chosen versus a confirmatory factor analysis because (1) the current study represents the first attempt to formally examine this scale’s factor structure, (2) limited research exists to suggest a specified number of factors, and (3) of sample size considerations. An EFA with promax rotation was conducted to allow potential factors to correlate with each other. Prior to generating factor solutions, factor retention criteria were determined by conducting parallel analysis (Hayton et al. 2004). Random data sets with identical dimensions (subjects, variables, range of response) were generated to determine the critical values for eigenvalues of identified factors (95th percentile from 1,000 iterations). Utilizing the 13-item FAS-PR, an initial two-factor solution was identified from the criteria above. However, item 10 (i.e., “Does helping the patients in these ways cause you distress?”) was found not to load on either of the retained factors and was subsequently dropped from further investigation. The procedure described above was repeated for the 12-item FAS-PR. The parallel analysis for a hypothetical 12-item questionnaire with identical dimensions of our sample identified that eigenvalues for the first 3 factors must exceed 1.812, 1.578, and 1.422, respectively.
Evidence from the factor analysis of FAS-PR scores (as shown via Scree plot, Fig. 1) suggests that only two factors met minimum eigenvalue criteria as evidenced by results from the parallel analysis mentioned previously. As a result, a two-factor solution was identified accounting for 53% of the variance. Table 1 describes retained items and factor loadings for respective factors. Factor one includes 6 items labeled Avoidance of Triggers (FAS-AT). Items from the FAS-AT describe parental modifications to their daily routine (i.e., “Have you modified your work schedule because of the patients needs?” “Have you modified your family routine because of the patient’s symptoms?”) or avoidance of situations or stimuli that may elicit anxiety (i.e., “Have you avoided doing things, going places, or being with people because of the patient’s OCD?”, “How often do you assist the patient in avoiding things that might make him/her more anxious?”). Factor two also includes 6 items and was labeled Involvement in Compulsions (FAS-IC). Items from the FAS-IC describe the parent’s direct role in the child’s OCD-related rituals (i.e., “How often do you participate in behaviors related to patient’s compulsions?” “How often do you provide items for patient’s compulsions?”), as well as the child’s response to removal of parental involvement in rituals (i.e., “Has the patient become distressed/anxious when you have not provided assistance?” “Has the patient spent more time completing rituals when you have not provided assistance?”).
Fig. 1.
Scree Plot of 12-item FAS-PR principal axis factor analysis
Table 1.
Factor Loadings for 12-Item FAS-PR
| Factor loadings
|
||
|---|---|---|
| I | II | |
| Factor I-Avoidance of OCD Triggers | ||
| 1. Have you modified your family routine because of the patient’s symptoms? | 0.83 | −0.01 |
| 2. Have you avoided doing things, going, places, or being with people because of the patient’s OCD? | 0.76 | 0.04 |
| 3. Have you modified your leisure activities because of the patient’s needs? | 0.75 | −0.01 |
| 4. Have you modified your work schedule because of the patient’s needs? | 0.64 | −0.02 |
| 5. Have you had to do some things for the family that are usually the patient’s responsibility? | 0.55 | −0.09 |
| 6. How often did you assist the patient in avoiding things that might make him/her more anxious? | 0.32 | 0.19 |
| Factor II-Involvement in Compulsions | ||
| 7. Has the patient become distressed/anxious when you have not provided assistance? | −0.09 | 0.91 |
| 8. How often did you participate in behaviors related to patient’s compulsions? | −0.04 | 0.71 |
| 9. Has the patient become angry/abusive when you have not provided assistance? | 0.05 | 0.65 |
| 10. How often did you reassure the patient? | −0.12 | 0.57 |
| 11. Has the patient spent more time completing rituals when you have not provided assistance? | 0.08 | 0.55 |
| 12. How often did you provide items for patient’s compulsions? | 0.27 | 0.36 |
Factor loadings less than 0.30 are not reported
FAS-PR Family Accommodation Scale-Parent Report
Internal Consistency
Internal consistency was examined utilizing the total sample. Internal consistency coefficients (Cronbach’s alphas) were obtained for scores from the FAS-AT and FAS-IC subscales, as well as FAS-PR total scale. Results indicated that both the Avoidance of Triggers and Involvement in Compulsions subscales demonstrated good internal consistency (α=0.80), while the internal consistency of the FAS-PR total scale was excellent (α=0.90). Deletion of items (i.e., those demonstrating lower factor loadings) did not result in significant increases in internal consistency. The relationship between the FAS-AT and -IC subscales were in the large range (r= 0.51), suggesting separate, yet related constructs. These results yielded a 12-item version of the FAS-PR consisting of a total score and two related, 6-items subscales (Avoidance of Triggers & Involvement in Compulsions) with scores ranging from 12 to 60 and 6 to 30, respectively. Higher scores indicate greater levels of parental accommodation.
Means and Standard Deviations & Age and Gender Differences
The average score on the FAS-PR was 31.0 (SD=9.5), while the average score on the FAS-AT and FAS-IC subscales were 13.4 (SD=5.1) and 17.8 (SD=5.8), respectively. We also conducted Pearson product moment correlations to examine whether parental accommodation demonstrated a significant relationship to child age. Results revealed no statistically significant relationship between child age and FAS-PR Total Score (r= −0.12, p=0.27) or FAS-AT (r=−0.04, p=0.70) and FAS-IC (r=−0.16, p= 0.13) subscale scores. In addition, we conducted three separate independent samples t-tests to examine whether parental accommodation differed based upon child gender. No statistically significant differences were found on FAS-PR Total Score (p=0.12) or FAS-AT (p=0.11) and FAS-IC (p=0.21) subscale scores.
Convergent Validity
Convergent validity was examined utilizing the total sample. Pearson product moment correlations were conducted to examine the strength of the relationship between the FAS-PR and its two subscales and criterion measures of convergent validity (CY-BOCS total, CY-BOCS obsessions and compulsions, MASC, COIS-C, and BSI scores). Results from these analyses are presented in Table 2.
Table 2.
Pearson product-moment correlations between family accommodation scale-pr and indicators of construct validity
| Family accommodation scale- parent report
|
|||
|---|---|---|---|
| FAS-AT | FAS-IC | FAS-Total | |
| Convergent validity | |||
| Symptoms/functioning (IE) | |||
| CYBOCS total | 0.26** | 0.30** | 0.32*** |
| Obsessions | 0.16 | 0.24* | 0.24* |
| Compulsions | 0.33*** | 0.31** | 0.36*** |
| Symptoms/functioning (patient) | |||
| MASC-total T-Score | 0.27** | 0.10 | 0.20 |
| COIS-child total score | 0.34*** | 0.22* | 0.32** |
| Parent psychopathology (parent) | |||
| BSI-global T-score | 0.39*** | 0.18 | 0.32** |
| Discriminant validity | |||
| CATS total (child-report) | 0.22 | 0.07 | 0.17 |
| Piers-Harris total T-score (child-report) | −0.07 | −0.11 | −0.11 |
FAS-AT Family Accommodation Scale- Avoidance of Triggers
FAS-IC Family Accommodation Scale- Involvement in Compulsions
=<.05,
=<.01,
=<.001
FAS-PR Total Scale
Pearson product moment correlations revealed a small to medium, positive correlation between the FAS-PR total scale and CY-BOCS obsession score (r= 0.24, p≤0.001). In addition, Pearson correlations revealed a medium correlation between the FAS-PR total scale and CY-BOCS total (r=0.32, p≤0.001) and compulsion scores (r=0.36, p≤0.001) and BSI total T-scores (r=0.32, p≤0.05) and COIS-C total scores (r=0.32, p≤0.01). Collectively, these findings suggest that the FAS-PR total scale demonstrates good convergent validity.
FAS-AT Subscale
Pearson product moment correlations revealed a small to medium, positive correlation between the FAS-AT subscale and CY-BOCS total score (r=0.26, p≤0.01) and MASC total T-scores (r=0.27, p≤0.01). In addition, Pearson correlations revealed a medium relationship between the FAS-AT subscale and CY-BOCS compulsion score (r=0.33, p≤0.001) and a medium to large correlation with BSI total T-scores (r=0.39, p≤0.001). No additional statistically significant relationships were evident. These findings suggest that the FAS-AT subscale demonstrates good convergent validity.
FAS-IC Subscale
Pearson product moment correlations revealed a small to medium positive correlation between the FAS-IC subscale and CY-BOCS obsession score (r=0.24, p≤0.05) and COIS-C total score (r=0.22, p≤0.05). In addition, Pearson correlations revealed a medium correlation between the FAS-IC subscale and CY-BOCS total (r=0.30, p≤0.01) and compulsion scores (r=0.31, p≤0.01). No additional statistically significant relationships were evident. Take together these findings suggest that the FAS-IC subscale demonstrates adequate convergent validity.
Discriminant Validity
In an attempt to examine whether the FAS-PR and its two subscales demonstrate discriminant validity, Pearson correlations were conducted to examine the relationship between these scales’ scores and Piers-Harris and CATS total scores. Results demonstrated no statistically significant relationship between the FAS-PR, FAS-AT, or FAS-IC and CATS total scores (r=0.17, 0.22, and 0.07, respectively; p>0.05 for each) or Piers-Harris total t-scores (r=−0.11, 0.07, and −0.11, respectively; p>0.05 for each) suggesting adequate discriminant validity for this measure.
Discussion
This is the first study to formally examine the psychometric properties of the FAS-PR. Collectively, findings from this study suggest that a 12-item FAS-PR demonstrates a factor structure consisting of two separate, yet related subscales (Avoidance of Triggers, Involvement in Compulsions), and demonstrates good internal consistency and construct validity. Of note, both the FAS-PR total score and, in particular, its subscales differ from what has been published in prior OCD research (see discussion below; Merlo et al. 2009; Peris et al. 2008a, b; Storch et al. 2007). We found no relationship between accommodation and child age or child gender. These findings are discussed further below.
In comparison to prior research utilizing a 13-item measure of accommodation, the current study suggests that a 12-item version is most appropriate. This study also suggests that the FAS-PR consists of two separate, yet related subscales that we refer to as Avoidance of Triggers and Involvement in Compulsions. Of note, these empirically derived subscales are disparate from the clinically derived subscales developed by Peris et al. (2008b). In fact, only three of the nine items included in the authors’ Total Involvement subscale (i.e., “How often did you participate in behaviors related to patient’s compulsions?” “How often did you reassure the patient?” and “How often did you provide items for patient’s compulsions?”) would be retained in the current study’s Involvement in Compulsions subscale (FAS-IC). The three remaining items of the FAS-IC were relegated to a separate “Consequences” subscale in the Peris et al. study. To date, no study published in the child OCD literature has used a 12-item version of the FAS-PR or empirically derived subscales (Mariaskin et al. 2007; Merlo et al. 2009; Peris et al. 2008b; Storch et al. 2007). We recognize that removal of only one item from the FAS-PR may have a limited impact on the results of prior research. However, the ascertainment of two distinct yet related subscales provides clinical researchers with important empirical evidence moving forward in the examination of the role that these facets to parental accommodation may play in the etiology, maintenance, and treatment of childhood OCD. This may be particularly true given results relating to the convergent validity of the Avoidance of Triggers (FAS-AT) and FAS-IC subscales.
Interestingly, although the FAS-PR as a whole demonstrated good convergent validity with criterion measures, the FAS-AT and FAS-IC subscales appeared to demonstrate different patterns. For example, the FAS-AT demonstrated a consistently stronger relationship to global indicators of patient and parent psychopathology, while the FAS-IC demonstrated a stronger relationship to a clinician-administered measure of symptom severity (i.e., CY-BOCS). These findings suggest that these respective subscales may be differentially influenced by patient and parent characteristics. That is, scores on the FAS-IC may be more influenced by severity of a child’s OCD symptoms, while scores on the FAS-AT may be more influenced by global patient (i.e., symptoms of anxiety, impact of the disorder) or parent characteristics (i.e., parental psychopathology). If this is indeed the case, it will be important for future research to examine specific patient- and parent-level predictors of increased accommodation. In turn, given recent evidence suggesting that change in parental accommodation is predictive of response to CBT (Merlo et al. 2009), it will be important to examine whether these disparate facets to accommodation differentially impact treatment outcome. This line of research may inform further advancement of more efficacious therapeutic interventions for children with OCD and their families.
In addition to the psychometric analyses described above, we also found that neither child age nor gender demonstrate a differential impact on parental accommodation. Findings with regards to child age are perhaps most interesting. Steinberg and Silk (2002) note that the relationship between a child and parent becomes less close as the child matures. Interestingly, no age-related differences in parenting practices have been noted among the families of children with OCD (Barrett et al. 2002; Peris et al. 2008b; Storch et al. 2007), and results from the current study support these prior findings. One potential explanation for these apparently contradictory results is that while topography of behavior may differ across time, the function of this behavior may remain unchanged. That is, the parent of a 7-year-old with a fear of contamination may wash the child’s toys, or other personal items to eliminate perceived dirt or germs, while the parent of a 17-year-old may provide his/her child with money necessary to purchase products that the adolescent will use to eliminate perceived dirt or germs. Both examples suggest differing topography of behavior. However, the function (i.e., decrease parent and/or child anxiety) of this behavior may be identical. Alternatively, it is possible that parenting practices among the families of children with OCD are inherently different from those of “normal” children. These parenting practices may be poor at age 7 and equally poor at age 17. Clearly, further empirical investigation is necessary to test these hypotheses.
Limitations to the current study should be noted. First, due to sample size considerations we were unable to conduct a confirmatory factor analysis. Second, factor loading for two items from the FAS-PR were noticeably lower than other items. We decided to retain these items, however, because the items were conceptually similar to their respective subscales, and removal of either item did not result in a significant increase in internal consistency. Third, construct validation against a well-established family assessment measure was not possible due to the exclusion of such an instrument from the original POTS study (2004). In a related vein, although not reaching statistical significance, the strength of relationship between CATS scores (i.e., discriminant validity) and accommodation were comparable (though weaker) to those of the MASC (i.e., convergent validity). It is possible that both measures (the MASC and CATS) assessed aspects of negative affect and, in turn, demonstrated similar relationships to parental accommodation. Corroborating evidence, however, obtained from other criterion measures of construct validity (i.e., CY-BOCS total and subscales, BSI, COIS-C, and Piers-Harris) suggest that this is likely not a significant limitation. These limitations highlight the importance of further study investigating the FAS-PR’s factor structure (i.e., confirmatory factor analysis), reliability (i.e., temporal stability), and validity. Lastly, given the high rate of comorbid anxiety and externalizing disorders among the current sample (e.g. GAD, 36%), it is unclear to what extent findings from the current study are similar or dissimilar from children presenting without comorbid diagnoses. The present sample size did not allow for such analyses. However, the rates of comorbidity in the present sample mirror that of previous clinical research (Geller 2006). The clinical and research utility of the FAS-PR would be significantly weakened if the measure were validated among a sample of children presenting with no comorbid diagnoses as this represents a minority of children presenting with symptoms of OCD.
Despite the limitations noted above, the current study provides an important addition to the assessment of and empirical evidence regarding parental accommodation in child OCD. In addition to areas for further research highlighted previously, researchers may wish to examine possible differential levels of accommodation among children presenting with comorbid anxiety and/or externalizing disorders. Replication of previous research in the area of parental accommodation of childhood OCD may also be warranted. Research of this nature will help to advance our understanding of not only factors that impact accommodation and the effect accommodation may have on treatment outcome, but also the development or more efficacious and effective interventions for children afflicted with this debilitating disorder.
Contributor Information
Christopher A. Flessner, Email: cflessner@lifespan.org, Rhode Island Hospital, Child and Adolescent Psychiatry, Bradley Hasbro Children’s Research Center, 1 Hoppin St., Suite 204, Coro West, Providence, RI 02903, USA, Warren Alpert School of Medicine at Brown University, Providence, RI, USA
Jeffrey Sapyta, Duke University Medical Center, Durham, NC, USA.
Abbe Garcia, Rhode Island Hospital, Child and Adolescent Psychiatry, Bradley Hasbro Children’s Research Center, 1 Hoppin St., Suite 204, Coro West, Providence, RI 02903, USA, Warren Alpert School of Medicine at Brown University, Providence, RI, USA.
Jennifer B. Freeman, Rhode Island Hospital, Child and Adolescent Psychiatry, Bradley Hasbro Children’s Research Center, 1 Hoppin St., Suite 204, Coro West, Providence, RI 02903, USA, Warren Alpert School of Medicine at Brown University, Providence, RI, USA
Martin E. Franklin, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
Edna Foa, University of Pennsylvania School of Medicine, Philadelphia, PA, USA.
John March, Duke University Medical Center, Durham, NC, USA.
References
- Adams G, Waas G, March J, Smith M. Obsessive-compulsive disorder in children and adolescents: the role of the school psychologist in identification, assessment, and treatment. School Psychology Quarterly. 1994;9:274–294. [Google Scholar]
- Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D. Family accomodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical, and family characteristics. Psychiatry Res. 2010 doi: 10.1016/j.psychres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Amir N, Freshman M, Foa E. Family distress and involvement in relatives of obsessive-compulsive disorder patients. Journal of Anxiety Disorders. 2000;14(3):209–217. doi: 10.1016/s0887-6185(99)00032-8. [DOI] [PubMed] [Google Scholar]
- Barrett P, Shortt A, Healy L. Do parent and child behaviours differentiate families whose children have obsessive-compulsive disorder from other clinic and non-clinic families? Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43(5):597–607. doi: 10.1111/1469-7610.00049. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Lweis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, et al. Family accommodation in obsessive-compulsive disorder. The American Journal of Psychiatry. 1995;152:441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Mazure C, Kasl SV, Skolnick J, Fisk D, Vegso SJ, et al. Family accommodation of obsessive-compulsive symptoms. The Journal of Nervous and Mental Disease. 1999;187(10):636–642. doi: 10.1097/00005053-199910000-00008. [DOI] [PubMed] [Google Scholar]
- Cooper M. Obsessive-compulsive disorder: effects on family members. The American Journal of Orthopsychiatry. 1996;66(2):296–304. doi: 10.1037/h0080180. [DOI] [PubMed] [Google Scholar]
- Derogatis L, Melisaratos N. The brief symptom inventory: an introductory report. Psychological Medicine. 1983;13(3):595–605. [PubMed] [Google Scholar]
- Franklin M, Foa E, March JS. The pediatric obsessive-compulsive disorder treatment study: rationale, design, and methods. Journal of Child and Adolescent Psychopharmacology. 2003;13(Supplement 1):39–51. doi: 10.1089/104454603322126331. [DOI] [PubMed] [Google Scholar]
- Geller DA. Obsessive-compulsive and spectrum disorders in children and adolescents. The Psychiatric Clinics of North America. 2006;29(2):353–370. doi: 10.1016/j.psc.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH. Assessment of severity and change in obsessive compulsive disorder. Pediatric Clinics of North America. 1992;15(4):861–869. [PubMed] [Google Scholar]
- Hayton J, Allen D, Scarpello V. Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organizational Research Methods. 2004;7:191–205. [Google Scholar]
- Leonard HL, Lenane M, Swedo SE. Obsessive-compulsive disorder. Child and Adolescent Psychiatric Clinics of North America. 1993;2(4):655–665. doi: 10.1016/j.chc.2005.06.002. [DOI] [PubMed] [Google Scholar]
- March J. Cognitive-behavioral psychotherapy for children and adolescents with ocd: a review and recommendations for treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(1):7–18. doi: 10.1097/00004583-199501000-00008. [DOI] [PubMed] [Google Scholar]
- March JS. Multidimensional anxiety scale for children. North Tonawanda: Multi-health systems; 1998. [Google Scholar]
- March JS, Amaya-Jackson L, Terry R, Costanzo P. Posttraumatic symptomatology in children and adolescents after an industrial fire. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(8):1080–1088. doi: 10.1097/00004583-199708000-00015. [DOI] [PubMed] [Google Scholar]
- March JS, Amaya-Jackson L, Murray MC, Schulte A. Cognitive-behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(6):585–593. doi: 10.1097/00004583-199806000-00008. [DOI] [PubMed] [Google Scholar]
- Mariaskin M, Curry JF, March J, Franklin M, Foa E, Team P-IR. Family accommodation and emotion socialization in childhood obsessive-compulsive disorder. Association for Behavioral and Cognitive Therapies; Philadelphia, PA: 2007. [Google Scholar]
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2009;77(2):355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pediatric OCD Treatment Study Team [POTS] Cognitive-behavior therapy, sertraline, and their combination with children and adolescents with Obsessive-Compulsive Disorder: the pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004;292(16):1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- Peris TS, Benazon N, Langley A, Roblek T, Piacentini J. Parental attitudes, beliefs, and responses to childhood obsessive compulsive disorder: the parental attitudes and behaviors scale. Child & Family Behavior Therapy. 2008a;30(3):199–214. [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of Accommodation of Pediatric Obsessive-Compulsive Disorder: Parent, Child, and Family Characteristics. J Am Acad Child Adolesc Psychiatry. 2008b doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Bergman RL, Keller M, McCracken J. Functional impairment in children and adolescents with obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13(Supplement 1):S61–S69. doi: 10.1089/104454603322126359. [DOI] [PubMed] [Google Scholar]
- Piers EV, Harris DB. The Piers-Harris children’s self-concept scale. Los Angeles: Western Psychological Services; 1969. [Google Scholar]
- Scahill L, Riddle MA, McSwiggan-Hardin M, Ort SI, King RA, Goodman WK, et al. Children’s Yale-Brown obsessive-compulsive scale: reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety disorders interview schedule for DSM-IV. San Antonio: The Psychological Corporation; 1996. [Google Scholar]
- Simola SK, Holden RR. Equivalence of computerized and standard administration of the Piers-Harris children’s self-concept scale. Journal of Personality Assessment. 1992;58(2):287–294. doi: 10.1207/s15327752jpa5802_8. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Silk JS. Parenting adolescents. In: Bornstein MH, editor. Handbook of parenting: Children and parenting. 1. Vol. 2. Mahwah: Taylor & Francis; 2002. pp. 103–133. [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, et al. Family accommodation in peditric obsessive-compulsive disorder. Journal of Clinical Child and Adolescent Psychology. 2007;36(2):207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Suliman S, Kaminer D, Seedat S, Stein D. Assessing post-traumatic stress disorder in South African adolescents: using the child and adolescent trauma survey (CATS) as a screening tool. Annals of General Psychiatry. 2005;4(1):2. doi: 10.1186/1744-859X-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toro J, Cervera M, Osejo E, Salamero M. Obsessive-compulsive disorder in childhood and adolescence: a clinical study. Journal of Child Psychology and Psychiatry. 1992;33(6):1025–1037. doi: 10.1111/j.1469-7610.1992.tb00923.x. [DOI] [PubMed] [Google Scholar]
- Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, et al. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(2):128–129. doi: 10.1097/00004583-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Waters T, Barrett P. The role of the family in childhood obsessive-compulsive disorder. Clinical Child and Family Psychology Review. 2000;3(3):173–184. doi: 10.1023/a:1009551325629. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the anxiety disorders interview schedule for DSM-IV: child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Zohar AH. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 1999;8(3):445–461. [PubMed] [Google Scholar]