Abstract
Background
Current research fails to capture the temporal dynamics of chronic disease in favor of cross-sectional snapshots of symptoms and outcomes.
Objective
To estimate the effects of comprehensive psychosocial support on trajectories of spouse caregivers’ well-being related to the nursing home placement transition.
Method
Data from the New York University Caregiver Intervention, a randomized controlled trial of a comprehensive support program for spouse caregivers of persons with Alzheimer’s disease, were utilized. A convenience sample of 406 spouse caregivers of community-dwelling persons with Alzheimer’s disease was enrolled over a 9.5-year time period in an Alzheimer’s disease research center in New York City. Outcome measures, including the Zarit Burden Inventory and Geriatric Depression Scale, were used to assess differential effects of nursing home placement and the Intervention on spouse caregivers. In-person interviews of spouse caregivers took place every 4 months during the first year of participation and every 6 months thereafter for up to 16 years; 385 caregivers provided sufficient follow-up data for all analyses.
Results
Longitudinal models found that wives were more likely than husbands to indicate reductions in burden in the months following placement in an institution. Wives also reported greater decreases in depressive symptoms after placement in an institution when compared to husbands.
Discussion
The inclusion of transitions and health trajectories in a randomized controlled trial offers an intriguing picture of how comprehensive psychosocial interventions can help families navigate the challenges of chronic disease care. The results also demonstrate how advances in nursing science can facilitate future research in the modeling of trajectories and transitions in the dementia care context.
Keywords: family caregiving, institutionalization, nursing home admission
Existing conceptual models (Henly, Kallas, Klatt, & Swenson, 2003; Verbrugge & Jette, 1994; Wagner, Austin, & Von Korff, 1996) emphasize the need to consider the temporal nature of illness, symptom occurrence, and symptom management when studying the progression of disability. Too often, however, current research fails to capture the temporal dynamics of chronic disease in favor of cross-sectional snapshots of symptoms and outcomes. The purpose of this research study was to examine the effects of a “change in lives, health, relationships, or environments” (Meleis, Sawyer, Im, Hilfinger Messias, & Schumacher, 2000; p. 13) in people with Alzheimer’s disease (AD). Specifically, the objective of this study was to estimate the effects of comprehensive psychosocial support and nursing home admission (NHA) for a person with AD on trajectories of husband and wife caregivers’ well-being, using contemporary longitudinal methods. This secondary analysis provides an empirical exemplar when studying psychosocial interventions and important transitions in a chronic disease context.
Theoretical Perspectives of Health Transitions
Nursing science has become proactive in studying health transitions. In part, this stems from nurses’ clinical roles in managing health transitions (e.g., from health to sickness; from hospital to home) for persons with complicated, chronic health conditions (Harrison, 2004). There exist numerous initiatives in nursing science that have helped disabled individuals and families navigate key health transitions. A health transition that has received considerable attention is the move from hospital to home. This transition has been studied in nursing research dating from the early 20th century (Burns, 1921), and nursing interventions for complex healthcare transitions have been examined recently (e.g., Naylor et al., 2004).
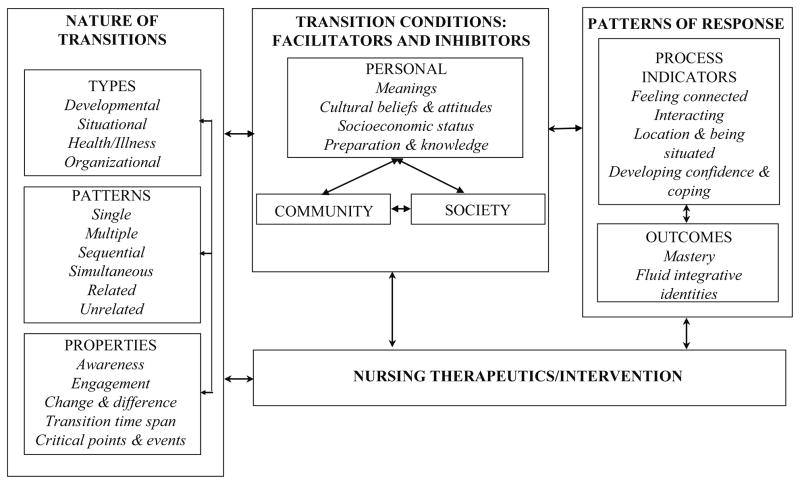
Meleis et al., in particular, have spent the past several decades refining a comprehensive conceptual model of health transitions (Chick & Meleis, 1986; Meleis et al., 2000; Schumacher & Meleis, 1994; Figure 1). In developing this conceptual model (or middle-range theory) Meleis et al. established a detailed framework to ascertain the type, pattern, and property of a given transition (or transitions), what factors could facilitate or inhibit individuals’ or families’ experience of the transition event (e.g., preparation, cultural attitudes, socioeconomic status), and how individuals or families may respond to such transitions via process (coping strategies, social engagement) and outcomes. The middle-range theory that Meleis et al. have developed is based largely on qualitative research. This model includes a number of concepts relevant to empirical measurement and quantitative analysis, particularly when attempting to define types, patterns, and properties of given transition events. The Meleis model serves as a framework to interpret the results of the present study on trajectories and transitions in dementia caregiving.
Figure 1.
The Meleis Health Transition Model.
From Meleis, A.I., Sawyer, L.M., Im, E-O., Hilfinger Messias, D.K., & Schumacher, K. (2000). Experiencing transitions: An emerging middle-range theory. Advances in Nursing Science, 23, 12–28. (Figure 1)
Transitions in Alzheimer’s Disease Caregiving
Due to longstanding trends of accelerated hospital discharge and increased prevalence of chronic illness, families are at the core of long-term care provisioning in the United States (Stephens & Franks, 2009). As a chronic illness like Alzheimer’s disease progresses over time, a number of critical events can occur that can influence the family care context significantly. These include diagnosis, disease stage transitions, increasing need for formal care at home, placement in an institution, and bereavement (Montgomery & Kosloski, 2000). Numerous studies have been focused on identifiable predictors of placement in an institution and how to delay or prevent this transition (Gaugler, Duval, Anderson, & Kane, 2007; Mittelman, Haley, Clay, & Roth, 2006). However, comparatively few researchers have examined whether NHA influences family caregivers, and what kinds of interventions can mitigate persistent stress or depression before and after nursing home entry of a disabled relative.
Nursing home admission usually reduces the daily load of caregiving activities, but can cause new stress. For example, families may witness poor quality care, injuries to their relatives, or loss of personal possessions. They may also feel compelled to spend large amounts of time at the nursing home, regardless of the inconvenience. As a result, prospective longitudinal research suggests that certain dimensions of stress and negative mental health may remain stable or worsen following NHA (Matsuda, Hasebe, Ikehara, Futatsuya, & Akahane, 1997; Rudd, Viney, & Preston, 1999; Schulz et al., 2004; Winslow & Carter, 1999). Although negative outcomes may occur for caregivers after NHA, particularly for those who had difficulty managing care demands and other stressors prior to placement in an institution, only one intervention study to date reported on the sustained benefits of treatment prior to and following placement in an institution (Gaugler, Roth, Haley, & Mittelman, 2008).
Pearlin’s stress process model (Pearlin, Mullan, Semple, & Skaff, 1990) has provided the New York University Caregiver Intervention (NYUCI) with a conceptual framework to study dementia caregiving over time and across key transitions such as NHA and bereavement (Gaugler et al., 2008; Haley et al., 2008). The stress process model is guided by the concept of proliferation, or the spread of stress, strain, and conflict from the actual provision of care to other life domains (e.g., family). As caregiving stress proliferates, global outcomes such as psychological well-being (e.g., depressive symptoms) are likely to be affected.
The stress process model first identifies primary stressors: those challenges or problems that are embedded in the caregiving situation and that are a direct result of the illness or disability of the person with AD. Primary objective stressors refer to the functional and health status of the person with AD, such as type and severity of dementia and behavioral problems. Caregivers’ emotional reactions to these demands are primary subjective stressors and represent the degree to which caregivers perceive care demands as exhausting, confining, or distressing (e.g., burden; Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995; Pearlin et al., 1990; Zarit, 1990). The results of these stressors are embodied in outcomes. In the context of the current analysis, outcomes refer to indices of negative mental health (global indicators of psychological well-being, such as depressive symptoms). The stress process model also includes resources that may stem the proliferation of stress during NHA. These resources include support provided to the family caregiver by other relatives and feelings of emotional connectedness with members of the social network (Aneshensel et al., 1995). The proliferation of stress has relevance to the placement-in-an-institution context (Whitlatch, Schur, Noelker, Ejaz, & Looman, 2001). The exacerbation of dementia severity and the potential inability of the nursing home staff to address these issues adequately may result in greater emotional distress for families, who may raise concerns about appropriateness of care to nursing home staff or advocate more vigorously to the staff to ensure proper care is delivered to their relative.
Meta-analyses suggest that gender differences in key caregiving outcomes are moderate to small, with wives or daughters more likely to indicate difficulties with behavior problems, emotional distress, depressive symptoms, and health impairment when compared to male caregivers (Pinquart & Sorensen, 2006). However, few researchers have examined gender differences across the placement event. While in a recent large-scale analysis of dementia caregiver adaptation to NHA, it was found that women were more likely to report decreases in depressive symptoms up to a year after placement in an institution (Gaugler, Mittelman, Hepburn, & Newcomer, 2009), in smaller-scale studies mixed results were reported in whether men or women experience greater emotional or psychological distress after NHA (Gaugler, Zarit, & Pearlin, 1999; Rudd et al., 1999; Schulz et al., 2004). There are also few studies focused on whether gender moderates response to caregiver intervention, in either community or institutional settings.
The New York University Caregiver Intervention
The New York University Aging and Dementia Research Center (NYU-ADRC) has been conducting a pioneering randomized trial of a psychosocial intervention for spouse caregivers of people with AD since 1987 that has demonstrated efficacy in reducing caregiver depressive symptoms, improving appraisal of behavior problems in persons with AD, and delaying NHA for the person with AD (Mittelman, Roth, Coon, & Haley, 2004; Mittelman, Roth, Haley, & Zarit, 2004; Mittelman et al., 2006). Because of its randomized controlled design and prospective data collection before and after NHA or bereavement of the person with AD, the NYUCI is uniquely positioned to answer research questions pertaining to key transitions in dementia caregiving. For example, it has been demonstrated that the NYUCI treatment had significant effects in reducing spousal caregivers’ depressive symptoms and burden after NHA (Gaugler et al., 2008). This secondary analysis adds to prior work by estimating the effects of the NYUCI on trajectories of spouse caregivers’ well-being by examining gender differences in well-being after NH placement and as a result of the NYUCI.
An influential hypothesis of early work on stress process models (Lazarus & Folkman, 1984) is that social support may ameliorate primary subjective stress, or, caregivers’ appraisal of primary objective stress (Goode, Haley, Roth, & Ford, 1998; Haley, Levine, Brown, & Bartolucci, 1987). A main clinical focus of the NYUCI was to build caregivers’ social support via individual and family counseling sessions. A chronic dementing illness such as AD can have devastating effects on the structure and functioning of the family. There is a deconstruction of the role of the ill family member, and other family members have to renegotiate their roles, even though the person with AD is still alive. The attachment of family members to the caregiver and the person with AD motivates their initial involvement in the NYUCI. The family counseling sessions provide problem solving and communication techniques for the family. In addition, the primary caregiver learns to ask for and accept help (also facilitated during additional individual counseling), and family members learn how to offer help so that it is likely to be accepted. Thus, a clinical objective of the NYUCI via improving family support for the primary caregiver is to develop increased mutuality and intimacy, potentially leading to improvements in primary subjective stress and outcomes on the part of dementia caregivers.
Research Questions
Based on findings generated from the NYUCI and prior research on the ramifications of NHA for family caregivers, analyses were conducted on data derived from the NYUCI to answer the following questions:
Do husbands and wives who care for a person with AD and receive the NYUCI exhibit different patterns of reducing burden before and after NHA when compared to spouses in the usual care conditions?
Do husbands and wives who care for a person with AD and receive the NYUCI exhibit different patterns of reducing depressive symptoms before and after NHA when compared to spouses in the usual care conditions?
Method
For additional discussion on the effects of the NYUCI during and after NHA, see Gaugler et al. (2008). For detail about how the NYUCI met CONSORT (Consolidated Standards of Reporting Trials; http://www.consort-statement.org/) criteria, see Mittelman et al. (2006).
Procedure
Participants in the NYUCI included 406 spouses of persons with a clinical diagnosis of AD. Participants were recruited through the NYU-ADRC and community referral sources. All participants had spouses with an AD diagnosis. All spouses were living with the person with AD and were residing at home at the time of study enrollment. Following completion of a comprehensive, in-person baseline assessment, caregivers were assigned randomly to the NYUCI condition (n = 203) or the usual care control condition (n = 203). The assessment battery was re-administered every 4 months during the first year of participation and on a biannual basis in subsequent years; all follow-up assessments were conducted in person or over the telephone. Following the NHA, caregiver assessments continued at the regularly scheduled follow-up intervals unless the caregiver refused or was lost to follow-up. Two annual follow-ups were conducted after the death of the person with AD.
Sample
Participants were followed for up to 15.9 years. Twelve percent of the participants (n = 48) had at least 10 years of follow-up data. Twenty-one caregivers were lost to follow-up; thus, the longitudinal sample available for analysis of NHA included 385 caregivers. During the course of the study 210 persons with AD were placed in an institution. Analysis of attrition bias did not indicate significant differences between cases lost to follow-up and those who remained in the longitudinal analysis (Gaugler et al., 2008). Among the 210 care recipients who were placed in an institution, 9 were placed in a nursing home between baseline and the first postbaseline assessment and were not included in the present analysis. The median time to NHA for the NYUCI intervention and usual care groups were 4.8 and 3.3 years after baseline, respectively (Mittelman et al., 2006). For all 406 participants in the NYUCI, the mean follow-up period was 5.9 years and the median was 5.4 years. The analyses are based on 3,818 postbaseline assessments. Baseline descriptive data for the analytic sample are presented in Table 1.
Table 1.
Baseline Descriptive Characteristics: Analytic Sample
| Variable | Treatment (n = 191) | Usual Care (n = 194) |
|---|---|---|
| Female caregiver, n (%) | 103 (53.9) | 126 (65.0) |
| Age of caregiver, mean (±SD) | 71.55 (8.7) | 71.03 (9.5) |
| Age of person with Alzheimer’s disease, mean (±SD) | 73.67 (8.2) | 74.60 (8.2) |
| Global Deterioration Scale = 4, n (%) | 71 (37.2) | 63 (32.5) |
| Global Deterioration Scale = 5, n (%) | 85 (44.5) | 73 (37.6) |
| Global Deterioration Scale > 6, n (%) | 35 (18.3) | 58 (29.9) |
| Caregiver Geriatric Depression Scale, mean (±SD), range = 0–30 | 8.97 (5.7) | 10.33 (7.1) |
| Caregiver Modified Zarit Burden Scale, mean (±SD), range = 0–60 | 25.55 (9.5) | 26.87 (10.9) |
Notes. Sample is the subset of 385 caregivers who provided sufficient follow-up data for the analyses. Sufficient follow-up data consisted of any postbaseline data obtained when care recipients were living and residing in either the community or in an institutional setting.
From Gaugler, J. E., Roth, D. L., Haley, W. E., & Mittelman, M. S. (2008). Can counseling and support reduce Alzheimer’s caregivers’ burden and depressive symptoms during the transition to institutionalization? Results from the NYU Caregiver Intervention study. Journal of the American Geriatrics Society, 56, 421–428. (Table 1). Used with permission.
The New York University Caregiver Intervention
The NYUCI consisted of three components: individual and family counseling, support group participation, and ad hoc counseling. During the 4 months following the baseline assessment, spouse caregivers participated in six individual and family sessions with the study counselor (two with only the spouse caregiver and four with the spouse caregiver and at least one other family member; the person with AD did not participate in these sessions). The content of these sessions was individualized to address the unmet needs of each caregiver. These sessions generally included information, skills related to the management of behavioral problems, and strategies to bolster communication among involved and noninvolved family members. Caregivers agreed at baseline that they would participate in a weekly support group (under the auspices of the Alzheimer’s Association) after the 4-month follow-up. The third component, provided throughout the duration of the NYUCI, was ad hoc or ongoing counseling--caregivers and participating family members were free to contact the study counselors via telephone to address any issues, crises, or other significant changes that occurred. The NYUCI was delivered by counselors with advanced degrees in social work, psychology, counseling, or gerontology. Caregivers in the usual care group did not receive the formal counseling sessions, but were free to utilize supportive services in the community and could contact study counselors for information or referral purposes.
Key Measures
Burden
Caregivers’ burden was measured with a subset of questions from the Zarit Burden Interview (ZBI). The ZBI is one of the most widely used instruments to assess caregiving burden (Zarit, Reever, & Bach-Peterson, 1980). The shortened ZBI includes 15 questions to measure areas of potential stress (e.g., perceived time pressure, emotional distress, financial strain, guilt, overall burden) that could arise both before and following NHA for spouse caregivers.
Depressive symptoms
The Geriatric Depression Scale (Yesavage, Rink, Rose, & Aday, 1983) was administered at baseline and each follow-up interval to measure spouse caregivers’ mood and psychological well-being. The 30-item version has been validated widely (Brink et al., 1982). Pertinent to the present study, both the ZBI and Geriatric Depression Scale have demonstrated significant variance and utility in prior longitudinal analyses (e.g., growth curve modeling; Gaugler et al., 2009).
Nursing home admission
Dates of NHA were derived from follow-up interviews, NYU-ADRC records, or ad hoc telephone contacts with spouse caregivers or other family members.
Global Deterioration Scale
The severity of dementia was determined using the Global Deterioration Scale (Reisberg, Ferris, de Leon, & Crook, 1982), a semistructured rating of the person with AD’s functioning by the counselor based on each caregiver interview (administered every 4 months in the first year of participation and every 6 months thereafter). The Global Deterioration Scale has demonstrated extensive reliability and validity as a method to stage dementia severity (Reisberg, Ferris, & Sclan, 1993).
Analysis
The effects of the intervention and NHA on the 15-item ZBI and the 30-item Geriatric Depression Scale were estimated and tested using random effects regression growth curve analyses. A multilevel change model was used that estimated longitudinal trajectories for individual participants at one level, with the slopes of these person-specific longitudinal trajectories as the effects of between-subjects predictors at a higher-order second level (Singer & Willett, 2003). Since the main purpose of these analyses was to examine rates of change in burden and depressive symptoms across the NH transition, the main outcomes of interest were linear rates of change, with fixed effects or interaction terms added to further examine: (a) rates of change in burden or depressive symptoms in the years prior to NHA (i.e., years after baseline); (b) change in burden or depressive symptoms immediately after NHA (i.e., type of assessment); (c) change in burden or depressive symptoms in the years after NHA (years after NHA); and (d) the moderating effects of gender or treatment on these outcome trajectories. Intercepts (or baseline assessments) of burden and depressive symptoms were included as key covariates to provide additional statistical control. The years after baseline effect was centered by subtracting 1; this indicates the time until the 1-year postbaseline point. Centering allowed for a scaling of the models so that main effect tests for the time-invariant predictors (e.g., treatment group, gender) were comparisons between the groups 1-year postbaseline (see Gaugler et al., 2008, p. 424).
All analyses were conducted using restricted maximum likelihood estimation as provided by SAS PROC MIXED (Littell, Milliken, Stroup, & Wolfinger, 1996). An initial descriptive model was used to take a random selection of eight spouses, to plot individual trajectories of burden and depressive symptoms against NHA and examine variance and initial patterns of change visually. Subsequent primary analytic models included four time-invariant variables: caregiver gender, treatment group, placement group, and the baseline (pretreatment) value on the outcome being examined. As noted above, the models included two predictors for time to NHA, respectively: one to measure time elapsed between the date of the baseline assessment and NHA (years after baseline) and one for the amount of time elapsed since NHA (years after NHA). Time was measured in days but scaled in years for subsequent models. A time-varying indicator for placement in an institution (type of assessment) was included also in the NHA model as a predictor. This time-varying indicator provided a test of whether NHA led to an abrupt change in the level of the outcome (burden [ZBI] or depressive symptoms [GDS]) immediately after placement in an institution. A series of interaction effects were included also in the primary analytic models to test whether the change in caregiver burden or depressive symptoms following NHA was moderated by gender as well as treatment vs. control group assignment. Estimates from models without interaction effects were used to quantity main effects as indicated by the tests of statistical significance.
Results
Sample Characteristics
Baseline characteristics of the analytic sample are displayed in Table 1. As noted in prior NYUCI publications (Mittelman et al., 2006; Mittleman, Roth, Coon, et al., 2004; Mittleman, Roth, Haley, et al., 2004) there was a gender imbalance at baseline, with more women in the usual care condition (65.0%) than the NYUCI treatment (53.9%). Baseline Geriatric Depression Scale scores also varied between the treatment and usual care control conditions (due to the gender imbalance at baseline). For these reasons, baseline depressive symptom scores were included in all subsequent depressive symptoms trajectory models, and, to make the analytic strategy comparable, baseline burden was included in all burden trajectory models. Another potential covariate (Global Deterioration Scale scores, used to measure dementia severity) was found to be correlated with baseline values of the outcomes. By including baseline burden and depressive symptom scores as covariates in the longitudinal models, statistical control was approximated for this and other potential covariates that were not included explicitly in the analytic models (see Gaugler et al., 2008).
Individual Trajectories
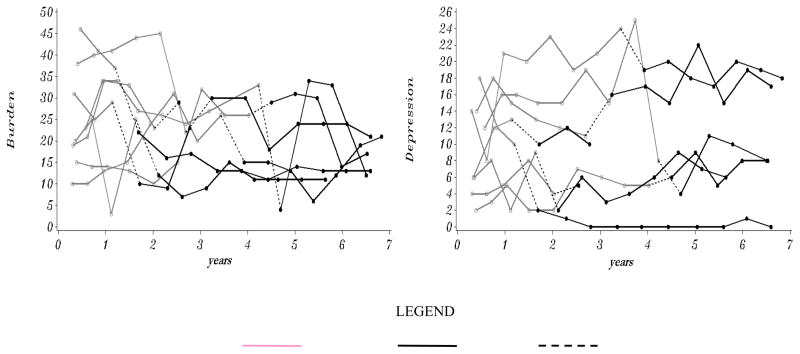
On average, there were 10.9 data points per caregiver, with a minimum of 1 and a maximum of 32. Random samples (n = 8) of intraindividual trajectories in the placement sample are shown in Figure 2. The gray segments of each trajectory denote at-home care periods, while black segments demonstrate postplacement reports. Dashed lines represent the time elapsed between the interviews administered immediately prior to NHA and the first postplacement interview. Considerable variability in terms of initial status, rate of change during the course of NYUCI, and the timing of NHA for each individual are shown. For example, in Figure 2 it appears that 5 cases exhibited increases in depressive symptoms during preplacement (the gray-shaded trajectories) and 3 cases exhibited decreases during preplacement assessment periods. Increases or decreases in burden or depressive symptoms after placement in an institution (the black-shaded trajectories) also appeared to be variable across the randomly selected cases.
Figure 2.
Random select of individual trajectories in New York University Caregiver
Gender, Intervention, and Nursing Home Admission Analysis
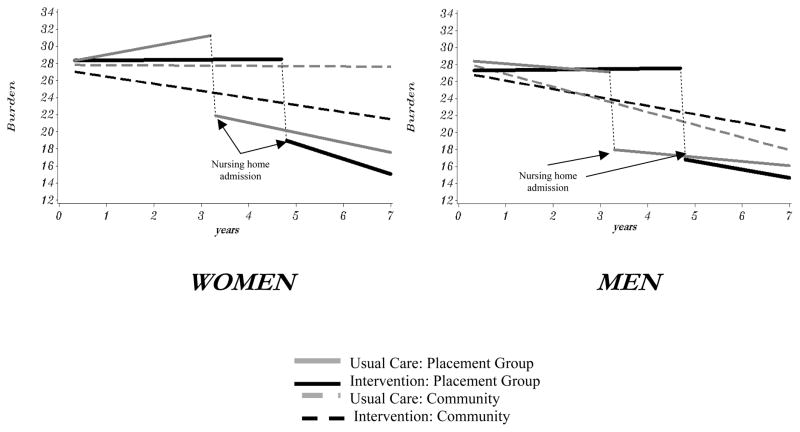
Model-predicted trajectories of the modified burden or ZBI score for intervention and usual care participants are illustrated in Figure 3 for women and men to provide visual interpretation of the various interaction terms tested in the multilevel models. Solid lines indicate predicted values for caregivers where placements were observed, and dashed lines indicate predicted values for caregivers where no placements occurred. The NHA transition points were the median times to placement established in prior NYUCI evaluations (Mittelman et al., 2006).
Figure 3.
Effects of the New York University Caregiver Intervention and nursing home admission on burden trajectories: Women and men
The interpretation of the reported main effects in Tables 2 and 3 by themselves is not useful conceptually. Specifically, the main effects in Tables 2 and 3 indicate the amount of change in the outcome for hypothetical participants who have a value of 0 on all other predictors. In addition, the interpretation of interaction terms (particularly in models with 3-way interaction terms) requires substantial arithmetic to obtain gender and group specific estimates for participants in the treatment or usual care control groups. For these reasons, prototypical (model-based) trajectories were plotted for burden and depressive symptoms; this is the most straightforward method to describe and interpret significant main effects and interaction terms simultaneously as recommended by methodologists (Singer & Willett, 2003).
Table 2.
Effects of Nursing Home Admission, New York University Caregiver Intervention, and Gender on Burden
| Effect | Estimate | SE | t | df | p |
|---|---|---|---|---|---|
| Intercept | 26.87 | 0.88 | 30.54 | 379 | <.0001 |
| Burden at baseline (mean centered) | 0.57 | 0.03 | 16.90 | 3064 | <.0001 |
| Treatment Group (Intervention = 1, Usual Care = 0) | −0.77 | 1.04 | −0.74 | 3069 | .46 |
| Caregiver gender (Female = 1, Male = 0) | 0.93 | 1.01 | 0.92 | 3064 | .36 |
| Placement Group (Yes = 1, No = 0) | 1.22 | 0.67 | 1.83 | 3064 | .07 |
| Years after baseline (centered at 1 year) | −1.49 | 0.30 | −5.05 | 355 | .0004 |
| Years after NHA | −0.14 | 0.40 | −0.36 | 3064 | .72 |
| Type of Assessment (NHA = 1, Community = 0) | −9.14 | 0.86 | −10.67 | 3064 | <.0001 |
| Baseline burden by Years after baseline | −0.10 | 0.01 | −9.68 | 3064 | <.0001 |
| Gender by Years after baseline | 1.47 | 0.37 | 3.98 | 3064 | <.0001 |
| Placement Group by Years after baseline | 1.06 | 0.24 | 4.38 | 3064 | <.0001 |
| Treatment group by Caregiver gender | −0.58 | 1.35 | −0.43 | 3064 | .67 |
| Treatment Group by Years after NHA | −0.92 | 0.49 | −1.86 | 3064 | .06 |
| Treatment Group by Years after baseline | −0.50 | 0.35 | 1.42 | 3064 | .16 |
| Treatment Group by Type of Assessment | −1.62 | 1.08 | −1.50 | 3064 | .13 |
| Caregiver gender by Years after NHA | −2.05 | 0.56 | −3.65 | 3064 | .0003 |
| Caregiver gender by Type of assessment | −0.39 | 1.09 | −0.35 | 3064 | .72 |
| Treatment group by Caregiver gender by Years after baseline | −1.30 | 0.49 | −2.65 | 3064 | .008 |
| Treatment group by Caregiver gender by Type of assessment | 1.54 | 1.46 | 1.05 | 3064 | .29 |
| Treatment group by Caregiver gender by Years after NHA | 1.12 | 0.74 | 1.52 | 3064 | .13 |
Notes. NHA = nursing home admission; Estimate represents the amount of change in the outcome variable that is predicted for a one unit change in that predictor variable.
Table 3.
Effects of Nursing Home Admission, New York University Caregiver Intervention and Gender on Symptoms of Depression
| Effect | Estimate | SE | t | df | p |
|---|---|---|---|---|---|
| Intercept | 10.15 | 0.57 | 17.95 | 379 | <.0001 |
| Depression at baseline (mean centered) | 0.69 | 0.03 | 20.30 | 3065 | <.0001 |
| Treatment Group (Intervention = 1, Usual Care = 0) | −1.71 | 0.67 | −2.54 | 3065 | .01 |
| Caregiver gender (Female = 1, Male = 0) | 0.03 | 0.65 | 0.05 | 3065 | .96 |
| Placement Group (Yes = 1, No = 0) | 0.36 | 0.43 | 0.83 | 3065 | .41 |
| Years after baseline (centered at 1 year) | −0.38 | 0.19 | −1.99 | 354 | .05 |
| Years after NHA | −0.27 | 0.25 | −1.10 | 3065 | .27 |
| Type of Assessment (NHA = 1, Community = 0) | −0.83 | 0.53 | −1.54 | 3065 | .12 |
| Baseline depression by Years after baseline | −0.06 | 0.01 | −5.52 | 3065 | <.0001 |
| Gender by Years after baseline | 0.38 | 0.24 | 1.60 | 3065 | .11 |
| Placement Group by Years after baseline | 0.15 | 0.16 | 0.95 | 3065 | .34 |
| Treatment group by Caregiver gender | 0.64 | 0.88 | 0.73 | 3065 | .47 |
| Treatment Group by Years after NHA | 0.37 | 0.31 | 1.18 | 3065 | .24 |
| Treatment Group by Years after baseline | 0.20 | 0.23 | 0.90 | 3065 | .37 |
| Treatment Group by Type of Assessment | −0.18 | 0.68 | −0.26 | 3065 | .79 |
| Caregiver gender by Years after NHA | −0.37 | 0.35 | −1.03 | 3065 | .30 |
| Caregiver gender by Type of assessment | −1.44 | 0.68 | −2.12 | 3065 | .03 |
| Treatment group by Caregiver gender by Years after baseline | −0.58 | 0.31 | −1.86 | 3065 | .06 |
| Treatment group by Caregiver gender by Type of assessment | 0.47 | 0.91 | 0.51 | 3065 | .61 |
| Treatment group by Caregiver gender by Years after NHA | 0.43 | 0.46 | 0.94 | 3065 | .35 |
Notes. NHA = nursing home admission; Estimate represents the amount of change in the outcome variable that is predicted for a one unit change in that predictor variable.
Parameter estimates for fixed effects of burden and gender on the level-2 growth parameters are presented in Table 2. Post-NHA measurements of the modified ZBI that occurred in the interval immediately after placement in an institution were 9.20 units lower on average than the measurements obtained immediately prior to NHA (as noted above, empirical main effects were calculated in a model that did not include interaction terms to derive an interpretable result). Figure 3 was relied on to interpret interaction terms. Caregivers who placed their husbands or wives with AD in an institution were more likely to indicate increases in burden in the years leading up to NHA when compared to caregivers who did not place their husbands or wives in an institution. Women who placed spouses with AD in an institution exhibited the greatest increases in burden during the years prior to NHA. The trajectories in Figure 3 indicate that women in the usual care control group who placed their husbands or wives with AD exhibited an increase in burden of close to 2 points prior to NHA, while men who did not place their wives in an institution reported an average decrease in burden of approximately .5 to 1 point on the ZBI per year during the same period. These results are supported by three of the significant interactions reported in Table 2. Immediately after NHA, a drop in burden occurred for both women and men (Figure 3), but the two-way interaction suggested that women were more likely to report decreases in burden in the years after NHA when compared to men. Interpretation of the trajectories in Figure 3 shows that women in the control and treatment groups exhibited decreases of approximately 1 to 2 points per year on the ZBI, respectively, whereas for men, decreases in burden appeared less substantial.
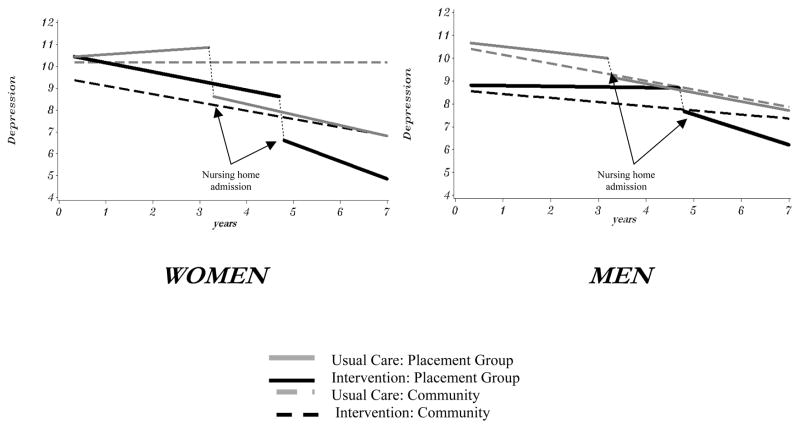
As with burden, depressive symptoms were plotted to examine the significant interaction terms. The main effect for years after baseline indicates that caregivers in the treatment group exhibited a decline of .17 points in depressive symptoms per year prior to NHA (as noted in an unconditional growth curve model that did not include the interaction terms, to facilitate interpretation). The trajectories in Figures 4 also show differences in gender and NHA. Specifically, women appeared to exhibit a greater decrease in depressive symptoms immediately after NHA (approximately 2 or more points) when compared to men who placed in an institution (approximately 1 point or less). This trend is suggested in one significant interaction term: Type of assessment by Caregiver gender.
Figure 4.
Effects of the New York University Caregiver Intervention and nursing home admission on depressive symptom trajectories: Women and men
Discussion
Spouse caregivers exhibited considerable reductions in burden (approximately 9 points on the ZBI, or nearly a standard deviation) following NHA. These results are in contrast to prior research that suggests caregiver stress remains stable or even increases after placement (Matsuda et al., 1997; Rudd et al., 1999; Schulz et al., 2004; Winslow & Carter, 1999). One important difference between the current study and many previous studies in this area is the type of analyses used. The multilevel longitudinal models with multiple time-invariant and time-varying predictors and interaction effects provided sensitive tests of specific changes in burden both before and after the NHA transition. This approach has advantages over more traditional analytic approaches (e.g., repeated measures analyses of variance with only a few independent variables; Raudenbush & Bryk, 2002; Singer & Willet, 2003). The NHA transition itself may offer considerable emotional benefit to spouses who have provided many years of community care.
A surprising nonfinding was the lack of effect of NHA on depressive symptoms immediately after placement. This appears to contradict a previous analysis of NHA and the NYUCI (Gaugler et al., 2008). However, the lack of significance in this instance may be due to statistical artifacts. For example, a gender difference was observed in depressive symptoms at NHA, and it is possible that the inclusion of multiple 2- and 3-way gender interaction effects in the current analyses obscured the main effect of NHA on depressive symptoms found in the earlier study (Gaugler et al., 2008).
These results add to previous findings by demonstrating how husbands and wives experienced NHA differently during the multiyear study period. In particular, wives appeared more likely to report decreases in burden in the years after NHA than husbands, and women exhibited greater decreases in depressive symptoms immediately after NHA when compared to male AD caregivers. The placement transition may result in particular benefits for wives. For husbands, reductions in burden are less consequential following the NH transition; moreover, men experienced a less significant decrease in depressive symptoms after NHA when compared to women who placed their husbands with AD in an institution (Gaugler et al., 1999, 2009).
Wives tend to provide more direct, hands-on assistance with activities of daily living or behavior management to persons with AD in the community, and once these responsibilities are relinquished, wives may feel greater reductions in emotional distress or depressive symptoms. Men appear more likely to rely on other family members to help them provide at-home care even when assuming primary informal (i.e., unpaid) care responsibilities (Mittelman, 2003); thus, the potential effects of NHA are less pronounced.
Another important finding was that the NYUCI appeared particularly effective in reducing emotional distress (burden) for women in the years leading up to NHA (i.e., women in the usual care condition who placed their husbands in an institution reported significant increases in burden in the years prior to NHA). Perhaps the NYUCI enabled female caregivers to better access support from other family members, or the ongoing availability and flexibility of the NYUCI through support groups and ad hoc consultation may have helped women to better withstand the demands of informal dementia caregiving at home. Wives’ emotional investment in their role, via their more intensive hands-on care, may result in more difficult challenges pertaining to dementia care (Pinquart & Sorensen, 2006), and the comprehensive psychosocial approach of the NYUCI appeared well-suited to help wives obtain needed support from family members and to navigate the complicated, dynamic aspects of at-home family caregiving.
The study of the NYUCI had an unusually long follow-up period and number of assessments for many participants before and after the nursing home transition. The advanced statistical method and unique longitudinal data source allowed for modeling the potential effects of NHA on key outcome trajectories for caregivers who did or did not receive psychosocial intervention. Interpreting these results through a rigorous analytic lens suggests important directions and improvements for research on health transitions in dementia caregiving. This analysis of NYUCI data and NHA was secondary; the NYUCI was not designed to model the effects of psychosocial treatment and key transitions simultaneously. For these reasons, the available data did not describe the nature of the NH transition itself per more complex conceptualizations of health transitions.
A consideration of the Meleis model in the context of NHA demonstrates how incorporating a detailed health transition model a priori could have enhanced the description of potential responses to NHA. It could be argued that NHA is a health or illness type of transition, and information about other previous transitions, such as whether the observed NHA was the first time residential care was used, would have provided more information on the background of the transition to placement in an institution. Considerations of NHA implicit in the Meleis model, such as measuring caregivers’ engagement in the placement-in-an-institution event (e.g., frequency of meeting with staff, continuation of family care for the older person after placement in the NH, caregivers’ perceptions of engagement during the admission process) and the length of time between the decision to admit the relative in the NH and when the transition was completed would have helped to more fully describe the impact of placement in an institution. Consideration of these concepts could lead to a study that would amplify understanding of the process of NHA and result in a more complete empirical analysis of how placement in an institution and the receipt of comprehensive psychosocial support affect caregiver distress for wives and husbands.
There are several additional limitations. There was a lack of ethnic/racial diversity in the sample, and the study was limited to New York City. In addition, little data are available on how the NYUCI may have influenced variables related to end-of-life care or service utilization in the months prior to NHA or the death of the person with AD. More detail on the process of the NYUCI and usual care service use during the NH transition would have been illuminating; usual care participants were utilizing a considerable number of services (e.g., support groups; Mittelman, 2003). The efficacy of the NYUCI for other types of dementia caregivers (e.g., adult children) remains unknown. Another potential limitation is the baseline variation in disease severity among persons with AD in the NYUCI. As noted in earlier secondary analyses of the NYUCI (Gaugler et al., 2008, p. 424), Global Deterioration Scale scores were correlated with baseline values of burden or depressive symptoms. For these reasons, the baseline values of burden or depressive symptoms were included as covariates, and thus it was possible to achieve statistical control while avoiding the inclusion of additional parameters in the complex analytical models (which would threaten statistical power).
Dementia caregiving is in many ways a career, and a key aspect of this conceptualization is recognition of the various transitions that may occur for family caregivers during the course of dementia (Montgomery & Kosloski, 2000). The analyses of the NYUCI in this study, using complex modeling approaches, illustrate how comprehensive psychosocial support and the NH transition influence husband and wife caregivers’ well-being in the years leading up to and following NHA. The analytical and methodological approach demonstrated in this study has potential application beyond the NH transition in dementia caregiving. Numerous transitions exist across various types of chronic diseases (e.g., diagnosis, hospitalization, discharge to community, death), and clinical intervention strategies may help disabled persons and family caregivers successfully adjust to such transitions. The multilevel analytical approach of outcome trajectories prior to and following key transitions as utilized in this study has great potential to evaluate the effects of clinical intervention strategies throughout the course of chronic illness.
The analytic advantages of utilizing complex longitudinal models demonstrate how these techniques can demonstrate the long-term effects of psychosocial interventions before and after key health transitions. However, assessment of the nature, condition, and process of key transitions often is not considered in quantitative studies of family caregiving as specified in nursing science models (e.g., the Meleis model). In this regard, the novel findings of the NYUCI and how gender operated across NHA represent an exemplar for the empirical study of key transitions in dementia caregiving, and demonstrate the need to incorporate rigorous assessment of key events a priori to model health transitions effectively during the course of informal long-term care in chronic illness.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01 MH 42216) and National Institute on Aging (R01 AG14634). Additional funding was provided through the New York University Alzheimer’s Disease Center (Grant P30-AG08051). Dr. Haley was supported by Florida AD Research Center Grant P50-AG025711.
Contributor Information
Joseph Gaugler, McKnight Presidential Fellow, School of Nursing, Center on Aging, University of Minnesota, Minneapolis, Minnesota.
David L. Roth, Department of Biostatistics, University of Alabama-Birmingham, Birmingham, Alabama.
William E. Haley, School of Aging Studies, College of Behavioral and Community Sciences, University of South Florida, Tampa, Florida.
Mary S. Mittelman, Department of Psychiatry and Director, Psychosocial Research and Support Program Center of Excellence on Aging New York University Langone School of Medicine New York, New York.
References
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- Brink TL, Yesavage JA, Owen L, Heersema PH, Adey M, Rose TL. Screening tests for geriatric depression. Clinical Gerontologist. 1982;1:37–44. [Google Scholar]
- Burns MS. Hospital convalescents in their homes. Modern Hospital. 1921;16:525–526. [Google Scholar]
- Chick N, Meleis AL. Transitions: A nursing concern. In: Chinn PL, editor. Nursing research methodology: Issues and implantation. Gaithersburg, MD: Aspen; 1986. pp. 237–257. [Google Scholar]
- Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: A meta-analysis. BMC Geriatrics. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Mittelman MS, Hepburn K, Newcomer R. Predictors of change in caregiver burden and depressive symptoms following nursing home admission. Psychology and Aging. 2009;24:385–396. doi: 10.1037/a0016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Roth DL, Haley WE, Mittelman MS. Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzheimer’s disease during the transition to institutionalization? Results from the New York University Caregiver Intervention study. Journal of the American Geriatrics Society. 2008;56:421–428. doi: 10.1111/j.1532-5415.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Zarit SH, Pearlin LI. Caregiving and institutionalization: Perceptions of family conflict and socioemotional support. International Journal of Aging & Human Development. 1999;49:1–25. doi: 10.2190/91A8-XCE1-3NGX-X2M7. [DOI] [PubMed] [Google Scholar]
- Goode KT, Haley WE, Roth DL, Ford GR. Predicting longitudinal changes in caregiver physical and mental health: A stress process model. Health Psychology. 1998;17:190–198. doi: 10.1037//0278-6133.17.2.190. [DOI] [PubMed] [Google Scholar]
- Haley WE, Bergman EJ, Roth DL, McVie T, Gaugler JE, Mittelman MS. Long-term effects of bereavement and caregiver intervention on dementia caregiver depressive symptoms. The Gerontologist. 2008;48:732–740. doi: 10.1093/geront/48.6.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley WE, Levine EG, Brown SL, Bartolucci AA. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychology and Aging. 1987;2:323–330. doi: 10.1037//0882-7974.2.4.323. [DOI] [PubMed] [Google Scholar]
- Harrison MB. Transitions, continuity, and nursing practice. The Canadian Journal of Nursing Research. 2004;36:3–6. [PubMed] [Google Scholar]
- Henly SJ, Kallas KD, Klatt CM, Swenson KK. The notion of time in symptom experiences. Nursing Research. 2003;52:410–417. doi: 10.1097/00006199-200311000-00009. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman J. Stress, appraisal and coping. New York, NY: Springer Publishing; 1984. [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger R. SAS System for mixed models. Cary, NC: SAS Institute; 1996. [Google Scholar]
- Matsuda O, Hasebe N, Ikehara K, Futatsuya M, Akahane N. Longitudinal study of the mental health of caregivers caring for elderly patients with dementia: Effect of institutional placement on mental health. Psychiatry and Clinical Neurosciences. 1997;51:289–293. doi: 10.1111/j.1440-1819.1997.tb03200.x. [DOI] [PubMed] [Google Scholar]
- Meleis AI, Sawyer LM, Im EO, Hilfinger Messias DK, Schumacher K. Experiencing transitions: An emerging middle-range theory. ANS: Advances in Nursing Science. 2000;23:12–28. doi: 10.1097/00012272-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Mittelman MS. Community caregiving. Alzheimer’s Care Quarterly. 2003;4:273–285. [Google Scholar]
- Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer’s disease. Neurology. 2006;67:1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- Mittelman MS, Roth DL, Coon DW, Haley WE. Sustained benefit of supportive intervention for depressive symptoms in caregivers of patients with Alzheimer’s disease. The American Journal of Psychiatry. 2004;161:850–856. doi: 10.1176/appi.ajp.161.5.850. [DOI] [PubMed] [Google Scholar]
- Mittelman MS, Roth DL, Haley WE, Zarit SH. Effects of a caregiver intervention on negative caregiver appraisals of behavior problems in patients with Alzheimer’s disease: Results of a randomized trial. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2004;59:27–34. doi: 10.1093/geronb/59.1.p27. [DOI] [PubMed] [Google Scholar]
- Montgomery RJV, Kosloski KD. Family caregiving: Change, continuity, and diversity. In: Lawton MP, Rubenstein RL, editors. Interventions in dementia care: Toward improving quality of life. New York, NY: Springer; 2000. pp. 143–171. [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist. 1990;30:583–594. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2006;61:33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Newbury Park, CA: Sage; 2002. [Google Scholar]
- Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. The American Journal of Psychiatry. 1982;139:1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- Reisberg B, Ferris SH, Sclan SG. Empirical evaluation of the Global Deterioration Scale for staging Alzheimer’s disease. The American Journal of Psychiatry. 1993;150:680–682. doi: 10.1176/ajp.150.4.aj1504680. [DOI] [PubMed] [Google Scholar]
- Rudd MG, Viney LL, Preston CA. The grief experienced by spousal caregivers of dementia patients: The role of place of care of patient and gender of caregiver. International Journal of Aging & Human Development. 1999;48:217–240. doi: 10.2190/MGMP-31RQ-9N8M-2AR3. [DOI] [PubMed] [Google Scholar]
- Schulz R, Belle SH, Czaja SJ, McGinnis KA, Stevens A, Zhang S. Long-term care placement of dementia patients and caregiver health and well-being. JAMA. 2004;292:961–967. doi: 10.1001/jama.292.8.961. [DOI] [PubMed] [Google Scholar]
- Schumacher KL, Meleis AI. Transitions: A central concept in nursing. Image--the Journal of Nursing Scholarship. 1994;26:119–127. doi: 10.1111/j.1547-5069.1994.tb00929.x. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Stephens MAP, Franks MM. All in the family: Providing care to chronically ill and disabled older adults. In: Qualls SH, Zarit SH, editors. Aging families and caregiving. Hoboken, NJ: John Wiley & Sons, Inc; 2009. pp. 61–84. [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. The Milbank Quarterly. 1996;74:511–544. [PubMed] [Google Scholar]
- Whitlatch CJ, Schur D, Noelker LS, Ejaz FK, Looman WJ. The stress process of family caregiving in institutional settings. The Gerontologist. 2001;41:462–473. doi: 10.1093/geront/41.4.462. [DOI] [PubMed] [Google Scholar]
- Winslow BW, Carter P. Patterns of burden in wives who care for husbands with dementia. The Nursing Clinics of North America. 1999;34:275–287. [PubMed] [Google Scholar]
- Yesavage JT, Rink T, Rose T, Aday M. Geriatric depression rating scale: Comparison with self-report and psychiatric rating scales. In: Crook T, Ferris S, Bartus R, editors. Assessment in geriatric psychopharmacology. New Canaan, CT: Mark Powley and Associates; 1983. pp. 153–167. [Google Scholar]
- Zarit SH. Interventions with frail elders and their families: Are they effective and why? In: Stephens MAP, Crowther JH, Hobfoll SE, Tennenbaum DL, editors. Stress and coping in later life families. New York, NY: Hemisphere Publishing Co; 1990. pp. 241–265. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]