Abstract
Children and adolescents with acute lymphoblastic leukemia (A.L.L.) receive treatment that relies on daily self- or parent/caregiver-administered oral chemotherapy for approximately two years. Despite the fact that pediatric A.L.L. is uniformly fatal without adequate treatment, non-adherence to oral chemotherapy has been observed in up to one-third of patients. Little is known about the reasons for non-adherence in these patients. This study employed Straussian grounded theory methodology to develop and validate a model to explain the process of adherence to oral chemotherapy in children and adolescents with A.L.L. Thirty-eight semi-structured interviews (with 17 patients and 21 parents/caregivers) and four focused group discussions were conducted. Three stages were identified in the process of adherence: (1) Recognizing the Threat, (2) Taking Control, and (3) Managing for the Duration. Doing Our Part was identified as the core theme explaining the process of adherence, and involves the parent (or patient) taking responsibility for assuring that medications are taken as prescribed. Understanding the association between taking oral chemotherapy and control/cure of leukemia (Making the Connection) appeared to mediate adherence behaviors.
Keywords: pediatric acute lymphoblastic leukemia, oral chemotherapy, adherence, grounded theory
Acute lymphoblastic leukemia (A.L.L.), a malignant disorder of lymphoid hematopoiesis, is the most common malignancy of childhood, and accounts for nearly 25% of all cancer diagnosed in children less than 15 years of age (Horner et al., 2009). Prior to the advent of modern therapy for leukemia in the latter half of the twentieth century, childhood A.L.L. had a rapidly fatal course and most children succumbed to the disease within a matter of months (Simone, 2006). Fortunately, progress in therapy for children and adolescents with A.L.L. has resulted in dramatic improvements in survival over the past four decades, such that overall 5-year survival with contemporary therapy now exceeds 85% (Jemal et al., 2009). However, even with contemporary therapy, approximately 1 in 5 children with A.L.L. will experience relapse of their disease (Nguyen et al., 2008). Once relapse has occurred, the probability of long-term survival is significantly diminished; thus, relapsed A.L.L. is a significant contributor to cancer-related death in children (Nguyen et al., 2008).
Therapy for pediatric A.L.L. requires a prolonged “maintenance” phase that relies primarily on self- or parent/caregiver-administered oral antimetabolite chemotherapy (i.e., 6-mercaptopurine) that must be taken at home on a daily basis for approximately two years (Gale & Butturini, 1991). Numerous studies have demonstrated a relationship between lower systemic exposure to these oral chemotherapy agents during the maintenance phase of therapy and increased risk of relapse in childhood A.L.L. (Dibenedetto et al., 1994; Koren et al., 1990; Lilleyman & Lennard, 1994; Schmiegelow et al., 1995). One potential reason for lower systemic exposure to these oral chemotherapy agents is non-adherence to prescribed therapy (Davies, Lennard, & Lilleyman, 1993; Davies & Lilleyman, 1995; Pritchard, Butow, Stevens, & Duley, 2006). Salvage therapy for relapsed A.L.L. is considerably more toxic and significantly less likely to be curative than front-line therapy. Thus, avoidance of modifiable factors that could contribute to the increased risk of relapse (such as poor adherence to oral chemotherapy) is likely to be beneficial for these young people.
The terms “adherence” and “compliance” are often used interchangeably in the biomedical literature. The classic definition of compliance, attributed to Sackett (1979), is “the extent to which a person’s behavior…coincides with the clinical prescription” (p. 1). In more recent literature, “adherence” has emerged as the preferable term, and is more commonly associated with shared decision-making between patient and healthcare provider regarding the treatment regimen (Rapoff, 2006). Adherence has been defined as “an active, intentional, and responsible process of care, in which the individual works to maintain his or her health, in close collaboration with healthcare personnel” (Kyngas, Duffy, & Kroll, 2000, p. 5). Adherence to medical therapy is a complex health behavior. Numerous factors have been shown to adversely influence adherence, including increased complexity of the medication regimen (McDonald, Garg, & Haynes, 2002), longer duration of therapy (Haynes, McDonald, & Garg, 2002), unpleasant medication side effects (Partridge, Avorn, Wang, & Winer, 2002), and impaired cognitive functioning (Logan, Zelikovsky, Labay, & Spergel, 2003). Additional factors that influence adherence include health beliefs (Elliott, Morgan, Day, Mollerup, & Wang, 2001), family structure and dynamics (Fiese & Everhart, 2006; Gayer & Ganong, 2006; Leonard, Garwick, & Adwan, 2005), socioeconomic status (Blais, Beauchesne, & Levesque, 2006), cultural beliefs and practices (Rose & Garwick, 2003; Sidelinger et al., 2005), and communication with and trust in healthcare providers (Dimatteo, 2004).
In the context of oral chemotherapy prescribed for treatment of pediatric A.L.L., lack of adherence may fall on a continuum that ranges from not taking any of the prescribed medication (Lilleyman & Lennard, 1996) to frequent or occasional missed doses, to failure to heed associated instructions, resulting in incorrect dosing, incorrect timing, or interference with absorption due to ingestion of food and dairy products (Schmidt & Dalhoff, 2002). Any of these non-adherent behaviors has the potential to contribute to suboptimal drug levels. Despite the fact that pediatric A.L.L. is uniformly fatal without adequate treatment, non-adherence to oral antimetabolite chemotherapy has been observed in up to one-third of patients with A.L.L. across the pediatric age range (Davies et al., 1993; Lau, Matsui, Greenberg, & Koren, 1998; Lennard, Welch, & Lilleyman, 1995; MacDougall, Wilson, Cohn, Shuenyane, & McElligott, 1989). Given the crucial role of oral chemotherapy in A.L.L. treatment, the potential consequences of non-adherence to prescribed therapy may include an increased risk of leukemia relapse and death (Davies et al., 1993; Dibenedetto et al., 1994; Koren et al., 1990; Lilleyman & Lennard, 1996). Additionally, studies of large cohorts of children and adolescents with A.L.L. have shown that 5-year survival rates for Hispanics are significantly lower than that for Caucasians. (Bhatia et al., 2002; Kadan-Lottick, Ness, Bhatia, & Gurney, 2003; Pollock et al., 2000). Factors such as cultural beliefs and practices, and communication and trust may be of even greater importance among Hispanics, due to socioeconomic barriers that may limit healthcare access, and linguistic and contextual barriers that may preclude effective communication between patients/parents and their healthcare providers (Institute of Medicine, 2002; Patino, Sanchez, Eidson, & Delamater, 2005; Sobo, 2004; Tumiel-Berhalter & Zayas, 2006).
Because little research has been conducted regarding the process of adherence to oral chemotherapy in children and adolescents with A.L.L., and since Hispanics have been identified as a subgroup that is potentially vulnerable to adverse health-related outcomes (Institute of Medicine, 2002), this study aimed to address these gaps in a cohort of Hispanic and Caucasian youth with A.L.L., in order to describe the process of adherence and thus inform future studies focusing on interventions to improve adherence in this population.
Methods
Design
This study employed a qualitative, grounded theory design. Grounded theory methodology is used to identify key explanatory constructs of the phenomenon under study and the relationships between those constructs (Carpenter, 2003). For this analysis, the research team utilized Straussian grounded theory methodology (Corbin & Strauss, 2008; Strauss, 1987; Strauss & Corbin, 1990, 1998), which places emphasis on interpretivism (asking questions about data), through a highly structured process of data analysis and coding. Straussian grounded theory is strongly identified with symbolic interactionism (Mead & Strauss, 1977), a philosophy arising from the use of shared symbols (including words, roles, gestures, and rituals) to construct realities that are seen as the basic social processes occurring in everyday life experiences (Gillespie, 2005). Straussian grounded theory therefore offers an excellent methodological fit with this study exploring adherence to oral chemotherapy in children and adolescents with leukemia, a process that involves significant interactions between the young patients, their parents, and healthcare providers.
Sample and Setting
The sample consisted of patients with a diagnosis of A.L.L. who received treatment at a comprehensive cancer center in the southwestern United States and met the following inclusion criteria: (1) Diagnosis of A.L.L. within the past 10 years at age 21 or younger; (2) Hispanic or Caucasian; (3) Received oral antimetabolite chemotherapy for at least one year during the maintenance phase of therapy; (4) Had completed leukemia therapy at time of study participation; and (5) English or Spanish-speaking. Patients age 12 and older and their parent/caregiver who was most involved in the maintenance phase of therapy were invited to participate in a semi-structured interview. Permission to invite the parent/caregiver was obtained from patients age 18 and older. Children under age 12 at the time of study enrollment were not interviewed but were represented in the interview by their parent/caregiver. Purposive sampling techniques (Strauss & Corbin, 1998) were used to select participants with characteristics that were relevant to targeted thematic areas requiring further exploration. Sampling continued until data saturation was achieved.
Procedures and Measures
The study protocol was approved by Institutional Review Boards at each of the three institutions with which the researchers were affiliated. Informed consent was obtained from each adult participant (≥age 18 years), and assent with parental consent was obtained from participants who were minors (12–17 years). Participants were informed that the purpose of the study was to understand the factors that may be helpful or that may make it more difficult for young people to take their oral chemotherapy regularly during A.L.L. treatment.
Three tools were used to support data collection: (1) an Interview Guide, consisting of 15 questions developed by the investigators based on literature review and expert opinion, designed to explore the factors and processes important to understanding adherence to oral chemotherapy during the maintenance phase of pediatric A.L.L. treatment; (2) a demographic tool administered prior to the interview, used to assess standard sociodemographic variables including age, gender, race, ethnicity, birthplace, parental birthplace, education, employment, household income, number of persons in household, medical insurance status, marital/relationship status, primary language, and preferred language for spoken/written healthcare encounters; and (3) a 12-item acculturation tool (Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987), with previously established reliability and validity (Calvillo & Flaskerud, 1993; Latham & Calvillo, 2007), administered to Hispanic participants and used to measure 3 important dimensions of acculturation: language use (5 items), media factor (3 items), and ethnic social relations factor (4 items).
Potential participants were identified through the cancer registry and from the patient roster maintained by the Department of Pediatrics at the cancer center. Once eligible patients were identified and permission to contact them was obtained from their primary oncologist, an introductory letter was mailed to the potential participants (age 18 or older) or to their parent/guardian (age less than 18). If no response was obtained within one week, a follow-up phone call was made by a study research assistant. Patients scheduled for clinic visits during the recruitment phase were approached in person by a research assistant at the time of their clinic visit and invited to participate. Once the patient and/or parent/caregiver agreed to participate, an interview was scheduled at the cancer center or at the patient’s home, as per preference of the participant. Semi-structured interviews were conducted according to the Interview Guide in the participant’s preferred language (English or Spanish) by one of the researchers or by a bilingual research assistant who participated in training sessions prior to the first interview.
Parents/caregivers and patients were interviewed separately. Interviews with parents/caregivers were a median of 51 minutes in duration, whereas interviews with patients, particularly with the younger participants, tended to be briefer, with a median duration of 33 minutes. The demographic tool and acculturation tool (Hispanic participants only) were completed at the time of the interview, averaging 10–15 minutes for completion. Each interview participant received $25 in compensation for their time.
Following completion and analysis of all interviews and generation of the preliminary theoretical model, participants were invited to return for focused group discussions. Four discussion sessions were conducted (for patients, parents of children under age 12, parents of adolescents/young adults, and Spanish-speaking parents) for the purpose of verifying and refining the preliminary theory, confirming the identified conceptual categories, and assuring data saturation. Scripts were developed for each of the focused group discussions by the research team. Each session was facilitated by two research team members (investigators and/or research assistants); facilitators participated in training sessions with the research team prior to conducting these focused group discussions. Card sorting, a qualitative research technique in which cards with key words are ordered by participants from most to least important (Jahrami, Marnoch, & Gray, 2009; Neufeld et al., 2004), was employed during each session to facilitate confirmation of previously identified categories. Group discussion sessions were a median of 114.5 minutes in duration. Each discussion session participant received an additional $25 in compensation for their time.
Data Management
Interviews and focused group discussions were digitally recorded and transcribed verbatim using Start Stop Universal Software Version 9.8 (HTH Engineering, Dunedin, FL). All names were removed from the transcripts and each name was replaced with a code. The coded list was kept in a locked file accessible only to designated members of the research team responsible for code assignment. Spanish interview and discussion group recordings were translated and transcribed into English by one bilingual research assistant, and a second bilingual research assistant then verified the translated version while listening to the Spanish recording. Atlas.ti software Version 5.2 (Berlin, Germany) was used as a data management, storage, retrieval, and data merging tool to assist with the management of field notes and memos, and to facilitate coding after the research team completed the initial assignment of codes.
Trustworthiness of Qualitative Data
Because the process of research in grounded theory is concurrent and iterative, with data collected and analyzed on an ongoing basis, researchers must be continuously cognizant (i.e., reflexive) that theory is emerging directly from the data and not from outside sources. Reflexivity involves self-awareness of how the researchers’ particular backgrounds and identities impact the research process, and involves open acknowledgment of the influence of any prior knowledge or experience on their perspective (McGhee, Marland, & Atkinson, 2007). Trustworthiness of the data was therefore addressed by close adherence to methodological considerations by the research team. Transcripts were initially reviewed independently by each member of the research team, and then presented at a monthly research team meeting for discussion, comparison with previously collected data, and finalization of analysis and coding. One member of the research team was assigned as primary analyst for each interview and was responsible for leading the discussion and summarizing the analysis for that interview. A three-member judge panel, consisting of two experts in qualitative research methodology and one expert in pediatric oncology nursing, was consulted to independently verify the coding schema (Beck, 1993); more than 90% agreement was achieved. Additionally, auditability and confirmability were achieved through careful organization of all data, including digital audio recordings, transcripts, field notes, memos, and coding lists, and by compiling an audit trail of decisions made by the research team during the data collection and analysis process (Lincoln & Guba, 1985).
Data Analysis
Quantitative Measures
SPSS Version 16.0 (SPSS, Inc., Chicago, IL) was used to calculate means, medians, and ranges for demographic and acculturation data.
Qualitative Analysis – Grounded Theory
The qualitative analysis was conducted according to Straussian grounded theory methodology (see Box) and included the use of analytic tools such as constant comparison, structured questioning, and searching for negative cases (Corbin & Strauss, 2008; Strauss & Corbin, 1990). Data collection and analysis occurred concurrently in an iterative process, and the interview guide was modified by the research team as the study progressed in order to capture relevant concepts as they emerged. The Caucasian cohort in this study was used as the referent group, and comparison between data collected from Hispanic and Caucasian participants was undertaken throughout the process of data analysis. The initial coding process involved open coding, in which the data were broken open or “fractured,” resulting in a large number of codes that were later collapsed into more abstract conceptual categories. This process involved structured questioning of the data, such as asking “What is this piece of data an example of?” (Strauss & Corbin, 1990, p. 62). This was followed by axial coding, which involved interconnecting of the initial codes identified in the open coding process (i.e., “crosscutting” the data) (Corbin & Strauss, 2008; Strauss & Corbin, 1990). The final stage of coding was selective coding, in which the core category, was identified. The objective of this final coding process was to identify a central theme that integrated the previously identified categories and was grounded in the data but was at a higher level of abstraction, constituting the substantive theory explaining the process under study (Punch, 2005).
Box. Coding Process in Straussian Grounded Theory.
Level 1: Open coding
Describes “what is happening” in the data
Data are broken open or “fractured”
Data compared for similarities and differences
Large number of codes
Categories generated
Properties and dimensions of categories identified
Level II: Axial coding
Interconnection of initial codes “putting data back together in new ways”
-
Categories systematically developed and their relationships solidified
Coding occurs around the axis of each category
Linkage occurs at the level of properties and dimensions of the categories
-
Paradigm model used identify linkages between categories by focusing on
Conditions
Contextual factors
Actions/interactional strategies
Intervening/mediating factors
Consequences
Level III: Selective coding (Development of substantive theory)
Core category (centerpiece of theory) identified
Integration of previously identified categories at a higher level of abstraction
-
Techniques useful in identifying core category include
Reviewing memos
Writing a story that connects categories that relate to and explain the core category
Developing diagrams
Questions asked of the data during the analysis process
What is the basic problem with which these participants must deal?
What helps these participants to resolve the basic problem?
What accounts for most of the variation or difference between how they go about resolving the basic problem?
What constrains or facilitates the process?
Findings
Participant Characteristics
The final sample consisted of 22 patients with A.L.L. (12 Hispanic, 10 Caucasian). A total of 38 interviews were conducted with 17 patients (16 in English, 1 in Spanish) and 21 parents/caregivers (15 in English, 6 in Spanish). There were no refusals among eligible patients or parents/caregivers approached for interview participation. Five patients younger than age 12 at the time of study entry were not interviewed in accordance with the study design; one young adult declined permission to contact a parent, and thus one parent/caregiver interview was not conducted. Although group discussion invitations were extended to all patients and parent/caregivers who were interviewed, participation was limited to those available during the scheduled sessions. Of the 38 participants, 14 returned to participate in the focused group discussions (4 Spanish-speaking parents, 4 parents of children younger than age 12 years, 2 parents/caregivers of adolescents/young adults, and 4 adolescent patients).
Median age of patients at diagnosis was 11 years (range 2 – 18 years); median age at study participation was 16 years (range 6 – 28 years). Eighteen mothers, two fathers, and one grandmother participated in interviews regarding these patients. Median age of these parents/caregivers at time of study participation was 45 years (range 34–60 years). Mean acculturation score of Hispanic participants was 39.5 (range 14–56); total possible range of scores was between 12 and 60, with 12 representing the lowest level of acculturation and 60 representing the highest level of acculturation. Participant characteristics and acculturation data are presented in the Table.
Table 1.
Participant Characteristics
| Characteristic | Entire Cohort (N=22) | Hispanic (n=12) | Caucasian (n=10) |
|---|---|---|---|
| Sex (n, %) | |||
| Female | 9/22 (41) | 5/12 (42) | 4/10 (40) |
| Male | 13/22 (59) | 7/12 (58) | 6/10 (60) |
|
| |||
| Age (in years) at diagnosis - median (range) | 11 (2–18) | 12 (3–18) | 10 (2–18) |
|
| |||
| Age (in years) at study entry - median (range) | 16 (6–28) | 15.5 (6–23) | 16 (6–28) |
|
| |||
| Time off treatment (years) - median (range) | 3 (0.2–6.7) | 1.5 (0.2–6.3) | 3 (0.7–6.7) |
|
| |||
| Parent/caregiver relationship to patient (n, %) | |||
| Mother | 18/22 (82) | 11/12 (92) | 7/10 (70) |
| Father | 2/22 (9) | 1 /12 (8) | 1/10 (10) |
| Grandmother | 1/22 (4.5) | 0 (0) | 1/10 (10) |
| Did not participate | 1/22 (4.5) | 0 (0) | 1/10 (10) |
|
| |||
| Parent/caregiver age at study entry – median (range) | 45 (34–60) | 43 (34–58) | 46 (37–60) |
|
| |||
| Parent/caregiver educational level - median | Some college | High school diploma/GED | 2 years college (Associate degree) |
|
| |||
| Parent/caregiver preferred language (n, %) | |||
| English | 14/22 (64) | 6/12 (50) | 8/10 (80) |
| Spanish | 6/22 (27) | 6/12 (50) | 0 (0) |
| Other | 1/22 (4.5) | 0 (0) | 1/10 (10) |
| Did not participate | 1/22 (4.5) | 0 (0) | 1/10 (10) |
|
| |||
| Type of household (n, %) | |||
| Single parent | 9/22 (41) | 8/12 (67) | 1/10 (10) |
| Two parent | 13/22 (59) | 4/12 (33) | 9/10 (90) |
|
| |||
| Number of household members - median (range) | 4 (2–7) | 4 (3–7) | 4.5 (2–7) |
|
| |||
| Annual household income - median | $20-50K | <$20K | $75–100K |
|
| |||
| Acculturation score† (Hispanics only) | |||
| Patients – mean (range) | N/A | 44.7 (30–52) | N/A |
| Parents/caregivers – mean (range) | 35.6 (14–56) | ||
Lowest possible acculturation score = 12; highest possible acculturation score = 60 (Calvillo & Flaskerud, 1993; Latham & Calvillo, 2007). Note: Acculturation data were obtained from Hispanic interview participants only; data were not obtained on 2 Hispanic patients who were younger than 12 years of age at the time of study enrollment and thus did not participate in interviews.
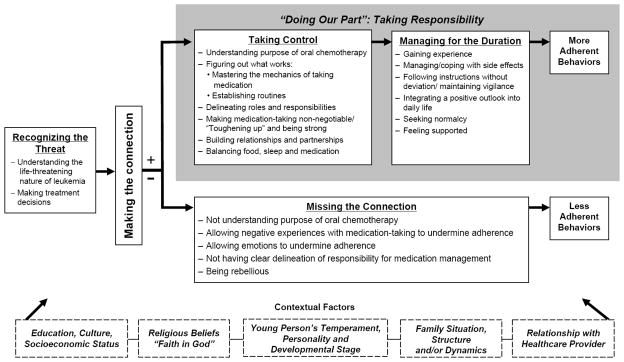
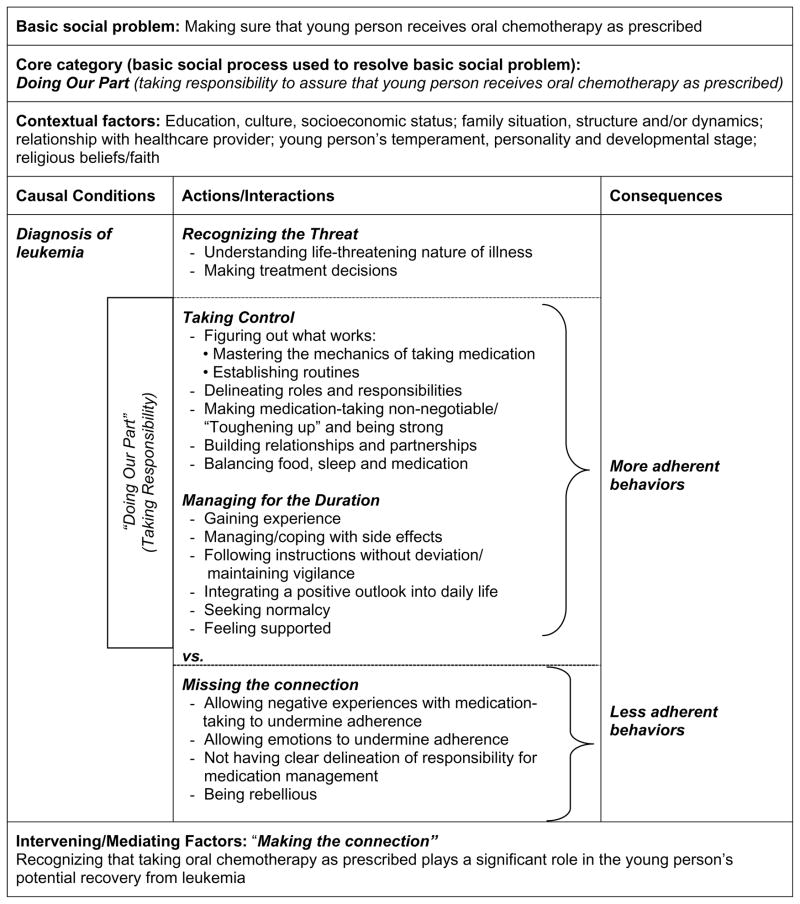
Theoretical Model - Overview
In developing the theoretical model (Figure 1), the focus was placed on understanding the process of being adherent or non-adherent to oral chemotherapy during treatment for childhood A.L.L. The relationships between categories, conditions, contextual and intervening/mediating factors, actions/ interactions, and consequences identified through the analysis are explained by the paradigm model (Figure 2). Further details regarding the identified constructs, including relevant examples from the data, are provided in the text.
Figure 1.
Theoretical Model: A Grounded Theory of the Process of Adherence to Oral Chemotherapy in Children with Acute Lymphoblastic Leukemia
Figure 2.
Paradigm Model
Phase I: Recognizing the Threat
The initial step in the process of adherence began with recognition that a serious health problem threatened the young person’s life. The process of Recognizing the Threat included both understanding the life-threatening nature of the illness and making treatment decisions.
Understanding the Life-Threatening Nature of the Illness
The onset of leukemia symptoms ranged from generalized fatigue and pallor that sometimes lingered for weeks, to sudden and severe illness requiring immediate hospitalization. Some participants described that they had suspected something was seriously wrong and insisted on additional testing even before the doctor had suggested it, while others lacked awareness of the potentially serious nature of the symptoms and described that they received the unexpected and shocking news of the leukemia diagnosis after what they had perceived as an innocuous medical visit for a routine illness. However, upon hearing the diagnosis of leukemia, the participants universally described recognition that the illness was life-threatening:
When [the doctor] told us that my son had leukemia, we thought that there wasn’t a cure and that he was telling us that my son was no longer going to be with us.
Mother of 7 yr old Hispanic male diagnosed at age 3
And she said, “You know, it’s a type of cancer, honey.” And I was like “What?” I was like “Are you kidding me?” And it was like – the whole way home…I couldn’t think about anything else. Got home, sat on the couch, and I was like “Man, I’m fifteen and I’m gonna [expletive] die. Like cancer – that’s a death sentence – right?”
22 yr old Caucasian male diagnosed at age 15
Making Treatment Decisions
News of the leukemia diagnosis was followed by information regarding the patient’s prognosis and treatment options. Many participants described their surprise and relief in learning that leukemia was potentially curable. After taking in the news of the diagnosis and learning that potentially curable therapy was available, patients or their parents/caregivers relied on the pediatric oncologist to make decisions regarding the specifics of the treatment that they should receive. During this phase, participants described themselves as not having the knowledge or experience to know what was medically required, and expressed the need to trust the healthcare team to make treatment decisions on their behalf. One mother noted:
They would tell us what they had to do, and I would tell them that they had to do what they thought - and not us - because we don’t know.
Mother of 7 yr old Hispanic male diagnosed at age 3
Acknowledgment on the part of the patient or parent that they did not possess sufficient knowledge to make reasoned decisions regarding the treatment - and that they needed to defer those decisions to expertise of the medical team - set the stage for the next phase, in which some participants recognized that they themselves had considerable expertise in regard to other aspects of their care.
Intervening/Mediating Factor: Making the Connection
Making the Connection describes recognition of the association between taking oral chemotherapy and control/cure of the leukemia. Many of the study participants indicated that they recognized this association shortly following the leukemia diagnosis, and that this understanding formed the basis for their subsequent actions.
I knew that if I wanted to get better – that I had to take these [pills]…there was no way around it. I mean, even if you felt fine, I took them. And if you felt sick, you knew you had to take them.
19 yr old Caucasian male diagnosed at age 12
I would just take it. Even if it did have a [side] effect, I would just have to deal with it. ‘Cuz I would say, “It’s either having this [side] effect or having an effect that will cost me my life.”
14 yr old Hispanic female diagnosed at age 10
Making the Connection appeared to mediate or explain adherence behaviors in this study. Those participants who recognized that taking oral chemotherapy as prescribed was necessary for control/cure of leukemia (“Making the Connection”) described more adherent behaviors, while those who failed to demonstrate this understanding (“Missing the Connection”) described less adherent behaviors. Participants who Made the Connection also recognized that they had a significant role to play in the recovery process, and that there were certain components of the treatment, including oral medications, over which they could exercise control. These participants described development of strategies to enhance adherence-related behaviors. These strategies were categorized into two phases, Taking Control and Managing for the Duration.
Phase II: Taking Control
The process of Taking Control was evident in those participants who Made the Connection, and consisted of figuring out what works, delineating roles and responsibilities, building relationships and partnerships, balancing food, sleep, and medication, and making medication-taking non-negotiable/toughening up/being strong.
Figuring Out What Works
Mastering the mechanics of taking medication
Some children, particularly those with no prior experiences or previous negative experiences with pill-swallowing, had significant problems with medication-taking beginning from the first day of treatment. Initially, parents of younger children relied on their child’s nurses to problem-solve medication administration, but many discovered that the standard approaches taken (e.g., crushing the medication and mixing it with flavored syrup or small amounts of food, or attempts to teach pill swallowing) were not effective and that the children resisted taking the medications. Common problems cited by the parents included poor palatability of certain medications, poor appetite related to the illness, and choking on or spitting out pills. Some parents expressed fears that their child might not be consuming the entire dose of medication, as well as concern in regard to the level of distress (for child and parent) associated with getting the full dose of medication into the child. Many parents were quick to intervene and develop their own solutions to the medication administration problems that their child encountered, as this mother described:
So can you imagine trying to give a 3-year-old a big pill? And they [the nurses] crushed it up and put it in Jell-O, and they would put in pudding, and they’d put it in apple juice, and they’d - and they were so nice - but she wasn’t taking that. I mean, she’d take some of it, she’d take a couple of bites…And so I got really scared that she wasn’t getting the full dose. So at one point I just sat her up in bed and opened up her mouth and stuck the pill down in the back of her throat, gave her a glass of water and said “just take it!” And - and she did.
Mother of 9 yr old Caucasian female diagnosed at age 3
For others, the process of mastering the mechanics of taking medication occurred over weeks to months and in some cases required the parent to request help from the medical team (e.g., consultation with a child psychologist for pill-swallowing training, and in one case, surgical placement of a gastrostomy tube to ensure administration of the full dose of medication in a child with severe behavioral aversion to oral medication). One patient describes how a nurse helped him to overcome difficulties with pill-swallowing several months after his diagnosis:
It took me forever to swallow pills, because either I waited till it dissolved in my mouth – which I knew I couldn’t do – you had to chew – and eventually I threw up. And I was just like “There’s gotta be a better way to do this!”…And then the nurse…she told me when you lean your head back…take the water bottle - your lips around it - and you swallow and it goes down right away…so it’s easier to take. And I did, and I was like “Holy cow! This is a piece of cake – this is a lot easier!”
19 yr old Caucasian male diagnosed at age 12
Establishing routines
Participants also described strategies that they developed to assure that the medication was taken regularly as prescribed, including use of pill boxes to organize medications, integrating medication administration into daily routines, and using reminder systems, such as calendars. These strategies differed depending on patient and family characteristics. For example, some participants described strict reliance on the use of a reminder system, while others described relying on inherent mechanisms in order to remember:
They gave you that calendar … I always looked at it. Even though I thought I knew what I was going to give her, I would always look at it just to be sure that I wasn’t giving her something different, yes.
Mother of 14 yr old Hispanic female diagnosed at age 10
For us, we never had a calendar. It was just the last thing we did in the evening….It’s just like - I can wake up without an alarm. I don’t know, you know - it’s just too big to miss. Too big.
Mother of 6 yr old Caucasian male diagnosed at age 2
Delineating Roles and Responsibilities
Role delineation varied depending on contextual factors, including family structure and climate, parent/caregiver preferences, and the patient’s developmental stage. For some families with younger children, medication administration was the sole responsibility of one parent, while for other families there was shared responsibility between the parents:
He [child’s father] would begin work at 6AM and I would give her the medicine before I went to work. And then in the afternoon he would come home at 3PM, and he would take care of her. And in the evening he would also give her the medicine. But yes, both of us would tend to her, but she took all of her medicine.
Mother of 11 yr old Hispanic female diagnosed at age 4
At times, parents of younger children described delegation of responsibility to other adults, such as when the child was at a sleepover event or participating in a school-related trip. This was done with exceptional scrutiny, with parents delegating responsibility only to those adults whom they deemed were sufficiently responsible to carry out their instructions exactly. Even when the parent delegated medication administration, they described maintaining primary responsibility by checking in with the designated adult by telephone to be sure that the child was receiving the medication as prescribed:
And I didn’t take [my son] to every birthday or every occasion because…some of the parents they didn’t want to take responsibility. And if he’s gonna be at overnight sleep party - you know, they [friend’s parent] call me, they tell me how [my son] is doing, are they doing the right thing? And I remind them…“Please tell [my son] he has to take this medication and this medication.”
Father of 14 yr old Caucasian male diagnosed at age 7
There was a couple times when I let my mother administer the medicine to her, but very few times. I remember one time we had to go out to dinner or some birthday or something and I was like, “Now don’t forget,” and I’d say, “She has to have her pill at this time.” And I’d call her, ”Did you give her the pill?”
Mother of 9 yr old Caucasian female diagnosed at age 3
Older children and teens and their parents/caregivers often described working together as a team to assure that the medication was taken as prescribed:
She [my mother] reminded me to take my pills. But she would prep them for me, or she would tell me to prep them, but one or the other of us would make sure that I got my pills.
18 yr old Caucasian female diagnosed at age 11
It was teamwork. She couldn’t have did it without me, and I couldn’t have did it without her. It worked.
Mother of 19 yr old Hispanic female diagnosed at age 12
Patient: My mom she would wake me up and she would tell me, “Did you take it?” Yeah…everyday…”Did you take them?”
Interviewer: If your mom was not reminding you, how do you think you would have done? Patient: Real, real, real bad (laughs).
22 yr old Hispanic male diagnosed at age 17
Additionally, some teens indicated that while they would normally find close parental supervision distasteful, they welcomed parental involvement and oversight when it came to assuring that they were taking their oral chemotherapy as prescribed:
I know it’s for the best for me – for my health – and she [my mother] wanted the best as well, so it didn’t really bother me at all. When it comes to my health – I let my mom butt into my health business or life – so to speak.
19 yr old Hispanic male diagnosed at age 13
Building Relationships and Partnerships
Participants described developing alliances with their healthcare providers, family members, friends, and community members, in order to ease the burden of care that they were experiencing. While they recognized that they needed to shoulder the primary responsibility for care, they also welcomed help from others, and found that by forging partnerships and alliances, they were able to better meet their own and/or their child’s needs. Several parents described other family members or friends taking over primary responsibility for the care of the child’s siblings for varying periods of time so that they could focus their attention solely on the care of the ill child. They also described relationships with their child’s healthcare providers in which they began to see themselves as partners in their child’s care – approaching the healthcare providers with their ideas for problem-solving and seeking confirmation from the healthcare provider that it was safe for them to implement a new idea:
[My son’s doctor] knows…I did some little research. I sat down, I put my time on it. It’s amazing what we parents can do… “This is my research from the Internet. Doctor - you want to go look at it? What do you think about it?” And it was one-on-one with the doctor before we do anything.
Father of 14 yr old Caucasian male diagnosed at age 7
Balancing Food, Sleep, and Medication
Some oral chemotherapy agents used in the treatment of childhood A.L.L., particularly 6-mercaptopurine and methotrexate, require restrictions regarding timing of food and dairy products (Schmidt & Dalhoff, 2002; Sofianou-Katsoulis, Khakoo, & Kaczmarski, 2006). These restrictions were particularly problematic for parents of young children, who were required to withhold food and dairy products from their children for one to two hours before and after each dose.
But his big thing was he loves milk at night. That’s a very big part of his routine. So to have him have the pill late enough in the evening where he hadn’t eaten an hour before- but then he couldn’t have milk after - was very- We did it, but that (sigh)- that was exhausting.
Mother of 6 yr old Caucasian male diagnosed at age 2
In addition, parents sometimes had to wake their children in order to give evening doses when the child fell asleep too soon after eating, and teens sometimes struggled to stay awake in order to maintain the required restrictions on food and dietary intake.
Sometimes we had to get him out of bed, because he may have fallen asleep. But it wasn’t an option to just keep him asleep. We had to get him up to take the pills.
Mother of 16 yr old Caucasian male diagnosed at age 9
Making Medication Taking Non-Negotiable / “Toughening up” and Being Strong
Many parents described the need to take a hard-line stance with their children and make it clear that medication-taking was non-negotiable. Even though the parents indicated that it was painful to them personally to be strict with their children, particularly in light of the seriousness of the child’s illness, they made it clear that their intentions were to benefit the child:
And I was a bit tough with her in the sense that I would tell her, “You can do it, and if you want to get better you have to do this” …and so it hurt me to be tough with her, strict….and she would get mad at me and I would feel awful, but it was for her own good, even though it hurt me to tell her she had to do it.
Mother of 14 yr old Hispanic female diagnosed at age 10
So myself, I just had to turn off the emotion. Because I knew that in order for this kid to live – he has to take them [the chemotherapy pills]. So it’s like I just kind of became the general, and you use that authoritative voice with him, he’d just take it.
Mother of 19 yr old Caucasian male diagnosed at age 12
This philosophy of communicating the importance of “toughening up” to the child was sometimes evident from early on in the illness, as one mother described in an episode that occurred during her daughter’s initial hospitalization just after diagnosis of her leukemia:
And I said, “But you’ve got a long haul ahead of you, and this little [intravenous] tube that’s bugging you is really very minor compared to what we’re – so you’re gonna have to toughen up a little bit and you’re gonna have to figure out - we have to figure out a way to make it work.” And we never had an issue after that, she never complained about taking any pills.
Mother of 16 yr old Caucasian female diagnosed at age 11
Eventually, patients and families resolved medication-related issues in a way that worked best for them and their particular situation. Throughout the process of Taking Control, patients and parents came to realize that they were able to use their problem-solving skills to make a unique contribution toward enhancing their chances of achieving cure.
Phase III: Managing for the Duration
Once patients/parents determined how to manage the day-to-day aspects of the treatment, they moved into the final phase, during which they were challenged with finding ways to consistently maintain adherence to prescribed medications over the entire duration of treatment. This process involved gaining experience, managing/coping with side effects, following instructions without deviation/maintaining vigilance, integrating a positive outlook into daily life, seeking normalcy, and feeling supported.
Gaining Experience
Participants explained that with experience and in conjunction with information provided by the healthcare provider, they mastered the specifics of the medication schedule and learned to anticipate and manage common side effects. They expressed that by knowing what to expect, they were able to feel some control over an otherwise difficult situation. One father explained:
Instructions from the doctor, that makes it a lot easier…[the doctor] would explain to me - this medication is gonna help him for this, or you know, the Predisone, I remember him saying, you know, he’s gonna have - a lot of appetite.
Father of 14 yr old Caucasian male diagnosed at age 7
I remember getting to know what effect each one had, and like preparing myself a little bit. Like “Okay, I’m gonna have this and that now,” so I’d like eat more before I’d take that one, or just little things like that.
16 yr old Caucasian female diagnosed at age 11
Managing/Coping with Side Effects
By receiving anticipatory counseling regarding potential side effects, participants explained that their anxiety was decreased when expected side effects occurred, and that they felt better prepared to manage them.
[The doctor] told me that is one of the consequences of the medicine, makes him nervous, angry, bitter, in a bad mood. He would hit us, he would get very upset, and he is not like that. I would understand that it was due to the medicine.
Mother of 7 yr old Hispanic male diagnosed at age 3
Following Instructions Without Deviation/ Maintaining Vigilance
Instructions from the healthcare team were often viewed as something that needed to be followed meticulously. Many parents, particularly parents of young children, emphasized that deviating from instructions was not tolerable for them, because it made them feel that they weren’t providing their child with the best possible chance for recovery. One mother explained:
To me it was so important to follow the rules. Because then in my mind I felt like I was doing what I was told to do. Like if anything went wrong, I would say, “Well at least I didn’t go ‘Oh here is a glass of milk and a 6MP on a full stomach’” (laughs). I just thought if I could do anything to make her odds better, I would.
Mother of 9 yr old Caucasian female diagnosed at age 3
Maintaining high levels of vigilance during the 2 to 3 years of leukemia treatment to assure that medications were taken as prescribed was a strategy reported by both parents and patients. Vigilance included actions such as checking and double-checking calendars or medication containers to be certain that all scheduled doses were administered:
I went by that calendar like it was – just to me it was just like God’s word – you know, there is no way I’m deviating from this. I checked it and double checked it and triple checked it and made sure it was absolutely accurate everyday.
Mother of 9 yr old Caucasian female diagnosed at age 3
Some parents reported checking with others and even awakening others from sleep to verify that medication doses had been taken:
I would sometimes wake up in the middle of the night and I would [say], “Oh we didn’t give her the medicine.” And I would wake him [child’s father] up and ask him, “Did you give our daughter the medicine?” “Yes, yes we did give it to her.” “What time did we give it to her? Tell me what time we gave it to her.” “We gave it to her.” “But are you sure?” “Yes,” and I would get up and sometimes I would not be sure of what he would tell me. And I would get up and count the pills in the bottle and I would realize that we did give it to her.
Mother of 11 yr old Hispanic female diagnosed at age 4
Several parents who expressed strong beliefs that instructions had to be followed exactly and who described vigilant behaviors also reported that their child never missed a dose of medication; these parents perceived the magnitude of missing a dose to be so great that they could not imagine allowing this to happen:
Interviewer: You don’t remember ever forgetting any [doses of medication]?
Mother: No, not at all. No, it - Never. I couldn’t even comprehend it.
Mother of 16 yr old Caucasian female diagnosed at age 8
It’s such an important thing. How do you – it’s kinda like not remembering to put clothes on that day – I mean, how do you not remember?
Mother of 16 yr old Caucasian female diagnosed at age 11
Integrating a Positive Outlook into Daily Life
Many participants reported that maintaining a positive attitude and discovering the “silver lining” in an otherwise negative experience of serious illness motivated them to manage the day-to-day responsibilities involved in the ongoing care requirements over the prolonged treatment period.
When they come [to the clinic] and it’s their birthday they get a gift from the nurses.…we’ve [patient and family members] all gone on the “Make A Wish” Disney cruise and the picnic - the pediatric picnic. And there’s you know - this horrible thing happened - and we usually tell the kids the silver lining is all these neat things that we wouldn’t have been doing…
Mother of 6 yr old Hispanic male diagnosed at age 3
Those diagnosed in adolescence particularly emphasized the importance of maintaining a positive outlook throughout treatment.
I always thought positive. My mom asked me “So you sick?” and I’m like “No, I’m not sick, it’s just a little minor set back thing in my health. It’s nothing big, I guess.” Knowing the fact that it was kinda something big, but I didn’t want to admit to it. I wasn’t in denial or anything – I just didn’t want to think like that. I was always positive, positive, positive.
19 yr old Hispanic male diagnosed at age 13
Think about your dreams, think about your future…if you have a dream, then you will survive. And if you have faith in yourself, you are not a person who will give up easily.
28 yr old Caucasian male diagnosed at age 18
Seeking Normalcy
Participants described the importance of getting back to normal activities once the initial symptoms had resolved and the treatment was underway. Being allowed to remain connected with or participate in school activities and sports, even if modifications had to be made, was described as an important component of making the treatment more tolerable, and giving the patient something to look forward to:
He wanted to play ball, that’s basically what a 9-year-old wanted to do…so we’d drive to the places and sit in the car and …we watched his team play.
Mother of 16 yr old Caucasian male diagnosed at age 9
In fact one time we went straight from the hospital to the school because she had a survey to fill out, and she’d get all these kids to fill them out at lunch while they were available. I mean literally getting out right from a spinal or something…And then another time there was this little concert choir…well she had a spinal that day and she had a headache…but she braved through and “I’m going, I’m going!”…And she was determined to be as normal as possible.
Mother of 16 yr old Caucasian female diagnosed at age 11
Feeling Supported
Support systems continued to play an important role throughout the lengthy treatment period. Parents described receiving concrete support from the healthcare team, family, neighbors, schools, and community and religious organizations. Several teens emphasized the importance of friendship, particularly having one close friend who understood what they were going through and supported them throughout their illness:
One of my personal friends was always there for me, and he also played soccer on the same team. So he kinda helped me out too, you know, “Kinda be careful,” and stuff…I mean we are best friends but he knew – and he was aware of everything. So he’d kinda like also take care of me, I guess, so to speak.
19 yr old Hispanic male diagnosed at age 13
I think it’s very important – like knowing that your friends are there for you. Not only your family – but people that are not even related to you are there for you.
14 yr old Hispanic female diagnosed at age 10
Core Category: Doing Our Part
The theoretic construct Doing Our Part (Taking Responsibility) was identified as the central theme that integrates the previously identified categories (i.e., Recognizing the Threat, Making the Connection, Taking Control, and Managing for the Duration) and explains the process of adherence to oral chemotherapy among young individuals with A.L.L. in this study. Although participants recognized that the healthcare team possessed the knowledge and skills needed to determine the treatment plan and to carry out many aspects of that plan, those participants who described more adherent behaviors also acknowledged the importance of taking personal responsibility for assuring that oral chemotherapy was delivered as prescribed, and that by taking on this responsibility (i.e., Doing Our Part), the patient/family was playing a key role in the recovery process. One mother explained:
Understand that she had to take all of her medications…that you couldn’t forget to give it to her if you wanted her to be okay. Because that was the most important, too, that we did our part in that. If we had not worried about her, who was? She wasn’t, because she was young, so she didn’t know whether to take medicine or not.
Mother of 11 yr old Hispanic female diagnosed at age 4
A key dimension (mediator) of the core variable was recognition that taking oral chemotherapy as prescribed played a significant role in the young person’s potential recovery from leukemia (Making the Connection); this intervening condition served as a motivator for Doing Our Part. The consequences of taking on the responsibility for Doing Our Part were sometimes striking, as some participants (particularly parents of young children) clearly indicated that every medication dose was taken on schedule as prescribed, in accordance with the associated dietary and dose-timing restrictions, and that they were able to maintain this level of adherence over the 2- to 3-year course of leukemia treatment:
I could swear to you on anything that she didn’t miss one dose of medicine. Never. It was my whole life.
Mother of 9 yr old Caucasian female diagnosed at age 3
She took all of her medicine. For us there was not a single day where you could say, “Oh, we forgot today.”
Mother of 11 yr old Hispanic female diagnosed at age 4
Parents who maintained this remarkable level of adherence explained that an additional positive outcome was the realization that they would not harbor feelings of guilt or have regrets should their child develop a leukemia recurrence, since they believed that they had done everything they could to assure that their child had the best possible chance for cure.
But I was very insistent that he not miss. I know [the doctor] told me that some parents have missed, and she told me that they felt guilty. And I can’t even imagine someone - I wouldn’t want it to be my fault for it coming back. And I always felt that way. So I have to do it. I need to do whatever I’m supposed to do.
Mother of 16 yr old Caucasian male diagnosed at age 9
Missing the Connection
Missing the Connection describes a theoretic construct in which study participants failed to recognize that taking oral chemotherapy was necessary for control/cure of the leukemia:
[I had] more pills than I can name or remember…I didn’t remember what any of them were for.
23 yr old Hispanic male diagnosed at age 18
Participants who Missed the Connection described behaviors less consistent with adherence. Although all participants acknowledged that they took their oral chemotherapy at least some of the time, participants who Missed the Connection described situations in which they allowed negative experiences to keep them from taking their oral chemotherapy as prescribed.
Medication side effects were commonly described by most study participants; however, those who Missed the Connection described situations in which they allowed side effects to keep them from taking their oral chemotherapy as prescribed:
I started doing that [not taking the pills] ‘cuz I kept getting sick and stuff…I would get like invited to places to go with people and stuff, and I would have to always cancel ‘cuz I would get sick. And I was getting mad. So, I mean – sometimes I wouldn’t take ‘em [the oral chemotherapy pills].
21 yr old Hispanic male diagnosed at age 17
I didn’t have difficulty remembering to take the pills, but I pretended I forgot, ‘cuz I didn’t want to take them…It’s just that sometimes I knew – I know of the consequences, I know of the reaction, I know of the things that happen after I took the medication. And doing this on a regular basis, sometimes you just don’t want to take it…sometimes you just want to avoid taking the medications.
28 yr old Caucasian male diagnosed at age 18
Additionally, participants who Missed the Connection described experiencing negative emotions that undermined their medication adherence:
I started getting aggravated with all the pills after about 4 or 5 months. It would anger me severely…I was just so irritated…Sometimes I’d all-out refuse [to take my pills], ‘cuz I was just so annoyed, and just all-out pissed with the situation.
23 yr old Hispanic male diagnosed at age 18
These participants were also unable to describe clear delineation of responsibility for medication management between parent and patient:
He [my son] said, “I can do it on my own, you don’t have to be here.” I go, “I got to make sure you are taking them, because it comes up in your tests…because if the doctor or nurse say anything, that’s on you – not on me – because I’ve been telling you.”
Mother of 21 yr old Hispanic male diagnosed at age 17
Instances of rebellion or acting out behavior were also described during which patients actively discarded prescribed doses of oral chemotherapy:
But since I didn’t like them [the pills], sometimes I would take them, or if not, I would throw them away.
15yr old Hispanic female diagnosed at age 12
Sometimes she wouldn’t take the medicine or she’d lie to me…One time I do remember I found [the pills] in the trash and it upset me very much.
Mother of 15yr old Hispanic female diagnosed at age 12
He was so annoyed – so then the nurses would come by and tell him, “At this time you have to take this” – and so he would just throw it [the pill] in the garbage.
Mother of 23 yr old Hispanic male diagnosed at age 18
Contextual Factors
Several contextual factors appeared to influence the process of adherence in this study, including socioeconomic status, family structure and climate, relationships with healthcare providers, the child’s temperament and developmental stage, and religious beliefs/ faith in God. Of note, this study failed to identify adherence-related cultural differences between the Hispanic and Caucasian participants. This occurred despite the fact that the interview guide was modified to more specifically elicit culturally-based practices when no cultural differences were identified during the interim data analyses, and the group discussion scripts were specifically designed to elicit data regarding the role of culture in adherence.
Socioeconomic Status, Family Structure and Climate
Most participants in this study reported positive home environments, in which they received needed support and in which their basic needs for food, shelter, and safety were met; however, some participants reported significant financial challenges:
I remembered the financial hardships that we had…the gas and all that to come [to the clinic], the round trips, we would come and go. Yes, that was a lot – a lot of problems.
Mother of 7 yr old Hispanic male diagnosed at age 3
In contrast, some participants emphasized their gratefulness for not having financial stressors during the time of their child’s illness:
And thank goodness – I think of those other moms that, what if they’re a single mom and their child is stricken with cancer? And they have to be – what do they do? I don’t know. I thanked God everyday for that. That I was fortunate enough to have the time and money or energy or whatever to be here, and not have to worry about how I’m going to make my house payment.
Mother of 9 yr old Caucasian female diagnosed at age 3
And thank God at the time…we didn’t have any big financial burdens, so I just think that wherever the parent is allowed to be mentally - I’m sure has a huge impact. If you’re completely stressed about paying the bills…so thankfully we didn’t have that.
Mother of 6 yr old Caucasian male diagnosed at age 2
Additionally, some participants from single-parent family structures reported situations in which they were unable to provide home supervision of medication administration due to employment responsibilities.
Interviewer: You wouldn’t see her taking her pills because you were working?
Mother: Yes. …she would always take them at night because I was there, but she would have to take them [alone] in the morning period.
Interviewer: So there was nobody else at home that gave them to her?
Mother: No, because I was alone with my three kids.
Mother of 15 yr old Hispanic female diagnosed at age 12
In contrast, several parents/caregivers from higher income, dual-partner families described how one parent was freed from other family responsibilities in order to focus their efforts on caring for their ill child and assure strict regimen adherence. One mother explained:
The other two [siblings] had their father’s undivided attention. “Your job is to take care of these two, the meals, the food, you worry about that – I’m down here dealing with what I need to with [the sick child].”
Mother of 19 yr old Caucasian male diagnosed at age 12
Relationships with Healthcare Providers
Most participants reported generally positive relationships with their healthcare providers:
I was really honest with them [my doctor and nurses] and they were really honest with me, so it was really like a open communication - just really open dialogue between us - which was always, I think, what made it so successful.
22 yr old Caucasian male diagnosed at age 15
However, some parents of adolescents who were exhibiting non-adherent behaviors attempted to enlist the assistance of their healthcare provider, who would then outline the potential consequences of non-adherence to the adolescent. This approach appeared to result in a somewhat adversarial relationship between patient and healthcare provider:
And so when we would come here [to the clinic] I’d say to the doctor, “This girl does not understand, she doesn’t take her pills.” So the doctor would threaten her, well not threaten her, but would tell her that if she didn’t listen to me she would be right back here - if she wanted to be admitted back to the hospital. And she didn’t like that very much.
Mother of 15 yr old Hispanic female diagnosed at age 12
Yeah, they [doctors and nurses] kept telling me they were going to put me back in the hospital if I didn’t take them [the pills].
23 yr old Hispanic male diagnosed at age 18
Patient’s Temperament and Developmental Stage
Differences in temperament and developmental stage also played a role in how participants managed medication administration over the 2 to 3 years of treatment. Some patients were described by their parents as easy-going and compliant with treatment throughout, while the strong-willed behavior of others presented significant challenges to adherence.
Ever since he was small…he hasn’t been a bratty kid, he was always compliant…he wouldn’t throw those tantrums. So he was very compliant with a lot of things that he would do.
Father of 15 yr old Hispanic male diagnosed at age 6
So he had a certain anger, a certain boredom – so he didn’t want to take it [the medicine].
Mother of 23 yr old Hispanic male diagnosed at age 18
Age at diagnosis also appeared to play a role in medication management. While parents of younger children indicated that medication administration was always under their direct supervision, responsibility for the adolescent’s medication administration was often reported to be either shared with the parent, or lacking clear delineation, allowing for the possibility of non-adherence in these older youth.
For me it was kind of like showing my mom I could do it by myself, I wanted to be independent.
16 yr old Caucasian female diagnosed at age 11
Religious Beliefs/Faith in God
Many participants emphasized the important role of religious beliefs and faith in God in helping them to adhere to the prolonged treatment:
That was very important for us – God and the medicine. Because like God says, “Help me, and I’ll help you.” Because look aside from everything, I believe in God and everything, but you are not going to ask only. Because if I asked but didn’t give her the medicine, what was going to happen? There was not going to be a good path. But those two things - asking God and giving her the medicine - that was what helped.
Mother of 11 yr old Hispanic female diagnosed at age 4
So for me faith is very important. It’s hugely important. Because when there is faith there is hope and everything, and that helped me to keep going, it’s God’s proof and I never stopped thanking Him.
Mother of 7 yr old Hispanic male diagnosed at age 3
Discussion
To our knowledge, this is the first study to examine the process of adherence to oral chemotherapy in young people with A.L.L. Our findings suggest that understanding the association between taking oral chemotherapy and control/cure of leukemia (Making the Connection) plays an important role in the adherence behaviors of young people with A.L.L. Participants in this study who recognized that taking oral chemotherapy was an important part of the potentially curative therapy for A.L.L. described a process in which they took steps to assure that they were as adherent as possible (Taking Control), and that the adherent behaviors were maintained throughout treatment (Managing for the Duration). Several adolescent patients in our study lacked recognition of the significant role that oral chemotherapy played in control/cure of their leukemia (Missing the Connection); these patients described behaviors less consistent with adherence despite the fact that they clearly articulated the life-threatening nature of their illness.
Several studies of pediatric chronic illness have demonstrated an association between lack of regimen-related knowledge and poorer adherence (Martin et al., 2007; Nicholson, Mellins, Dolezal, Brackis-Cott, & Abrams, 2006). In one study examining the information needs of parents of children with A.L.L., only two-thirds of the parents understood the purpose of their child’s maintenance chemotherapy, suggesting the need for improved health education targeted to those families lacking this understanding (Christiansen, Taylor, & Duggan, 2008). Beliefs regarding the efficacy of prescribed treatments are closely linked with knowledge and understanding of treatment regimens (Becker, 1974). Participants in this study who acknowledged the important role of oral chemotherapy in leukemia treatment also strongly endorsed beliefs regarding efficacy of the treatment. This finding is consistent with studies of other pediatric chronic illnesses that have shown positive associations between beliefs regarding the necessity of the prescribed treatment, the severity of health consequences if the treatment is not taken as prescribed, and adherence (Conn, Halterman, Lynch, & Cabana, 2007; Elliott et al., 2001).
A critical component of the efforts of participants who described more adherent behaviors in this study was the process of taking responsibility for assuring that the medication was taken exactly as prescribed (Doing Our Part). This finding is consistent with studies that have shown that an internally-focused locus of control (i.e., patient/family believing that they have some power to control the illness) is associated with higher levels of adherence than an externally-focused locus of control (i.e., belief that only the healthcare provider has power to control the illness) (Rapoff, 1999; Salabarria-Pena et al., 2001). Additionally, higher levels of patient/caregiver self-efficacy (an individual’s belief in their own capability to perform the required actions needed to achieve adherence) (Bandura, 1997) have been associated with improved outcomes in childhood chronic illness (Nicholson et al., 2006; Salabarria-Pena et al., 2001).
In our study, participants who described more adherent behaviors were also able to clearly delineate who was responsible for medication administration, and responses of these patient – parent/caregiver pairs were concordant in this regard; however, patients describing less adherent behaviors lacked concordance with their parent/caregivers in their attributions of responsibility for medication-taking. This is consistent with results of other studies that have shown that clear delineation of responsibility for medication administration, and concordance between adolescents and their parents/caregivers regarding this responsibility, are important components of adherence in pediatric cancer (Tebbi, Richards, Cummings, Zevon, & Mallon, 1988) and HIV infection (Martin et al., 2007).
Although this was a qualitative study and therefore not designed to quantitatively assess sociodemographic differences between groups, it is notable that those participants who described less adherent behaviors were all within the adolescent age range at the time of their diagnosis. The older age of the less adherent participants in this study is consistent with findings of several studies of adherence in pediatric chronic illness, including A.L.L., in which older age (particularly adolescence) is associated with poorer adherence (Lancaster, Lennard, & Lilleyman, 1997; Orrell-Valente, Jarlsberg, Hill, & Cabana, 2008; Williams et al., 2006). The less adherent participants also each described instances of volitional non-adherence, a behavior that involves an active decision not to adhere to a prescribed treatment (Rapoff, 2006); the volitional nature of these non-adherent behaviors was corroborated by the parents/caregivers of the less adherent participants. These participants justified their decisions not to adhere with explanations regarding their anger toward the illness, and/or interference of the treatment with their attempts to live a normal adolescent life. This is consistent with literature that describes acting out and rebellious/risk-taking behaviors as defensive coping mechanisms commonly employed by adolescents in an attempt to preserve autonomy and normalcy (Nevins, 2002; Smith & Shuchman, 2005; Wolff, Strecker, Vester, Latta, & Ehrich, 1998). Since many adolescents lack an awareness of the future consequences of their actions, and those who previously attained this awareness may regress developmentally in response to the stressors of their illness, this age group is highly vulnerable to non-adherent behaviors (Malbasa, Kodish, & Santacroce, 2007; Nevins, 2002).
While differences in culturally-based practices influencing adherence were not identified between the Hispanic and Caucasian cohorts in this study, our findings suggest that sociodemographic differences between the groups may play a role. For example, more Hispanic participants were from single-parent families, were non-English speaking, and had lower levels of education and household income than Caucasian participants (Table), and participants who described behaviors less consistent with adherence were also from low income, single-parent families. It is possible that socioeconomic constraints may play a role in gaining access to or understanding of information regarding the importance of oral chemotherapy in the childhood leukemia treatment (Making the Connection) and may adversely influence the consistent availability of a caregiver in the home to supervise medication administration (Doing Our Part). Additionally, language barriers may make the development of a positive relationship with the healthcare provider (Building Relationships and Partnerships) more difficult. However, it is important to note that this study was not designed or powered to detect differences in socioeconomic indicators between the Hispanic and Caucasian cohorts, and thus these findings would need to be confirmed in a study adequately powered to determine if these differences are significant. The impact of sociodemographic and family factors on adherence have been studied in other chronic childhood illnesses (Marhefka, Tepper, Brown, & Farley, 2006; Mellins, Brackis-Cott, Dolezal, & Abrams, 2004; Modi, Morita, & Glauser, 2008). Higher income levels have been associated with higher levels of adherence in pediatric HIV (Marhefka et al., 2006), chronic pediatric renal disease (Brownbridge & Fielding, 1994), epilepsy (Modi et al., 2008), and asthma (Blais et al., 2006), whereas poverty has been associated with unstable living environments, in which caregiver concern for long-term goals such as a child’s adherence to a prolonged treatment regimen may be overridden by concern for more immediate needs, such as providing food and shelter, and maintaining a safe environment for the family (Marhefka et al., 2006; Wolff et al., 1998).
Limitations
These findings must be considered in the context of several methodological limitations. Since this study used a retrospective design in which participants who had completed treatment were requested to recall their experiences during leukemia therapy, the potential for recall bias exists. Additional research involving patients currently receiving therapy is therefore needed to confirm the wider applicability of these findings. Given the qualitative nature of the study design, its purposive sampling technique, its relatively small sample size, and the fact that all participants had survived through completion of their leukemia therapy, the study results may not be generalizable to the larger population of childhood A.L.L. patients. Additionally, the cohort was older at diagnosis (median age, 11 years) than the typical A.L.L. population (typical age peak, 2 to 5 years of age), and the findings are limited to the experiences of Hispanic and Caucasian patients who were treated at a single institution. Nevertheless, despite these limitations, this is the first study to describe the process of adherence to oral chemotherapy in children and adolescents with A.L.L.
Conclusion/Implications for Future Research
This study employed Straussian grounded theory methodology to develop a model explaining the process of adherence to oral chemotherapy in a cohort of Hispanic and Caucasian youth with A.L.L. Three stages were identified in the process of adherence (Recognizing the Threat, Taking Control, and Managing Duration). Doing Our Part, the construct of taking responsibility for assuring that medications are taken as prescribed, was identified as the central theme in the adherence process, and Making the Connection (understanding the association between taking oral chemotherapy and control/cure of leukemia) appeared to mediate adherence behaviors among study participants. Although the study did not identify differences in culturally-based practices influencing adherence among Hispanic and Caucasian participants, our findings suggest that differences in contextual factors (e.g., lower socioeconomic status, single-parent family structure) may play a role in adherence. These differences in contextual factors may result in more limited access to or understanding of information regarding the importance of oral chemotherapy in childhood leukemia treatment (Making the Connection) and may adversely influence the consistent availability of a caregiver in the home to supervise medication administration (Doing Our Part). Additional research is needed to further explore the role of contextual factors in adherence, and to confirm or modify the theoretical model describing the process of adherence to oral chemotherapy in children and teens with A.L.L.
Acknowledgments
Funded in part by the National Cancer Institute/ CSULA-City of Hope Cancer Collaborative Pilot Project Research Program – 5P20CA118775 (Kane) & 5P20CA118783 (Momand)
References
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Beck CT. Qualitative research: the evaluation of its credibility, fittingness, and auditability. Western Journal of Nursing Research. 1993;15(2):263–266. doi: 10.1177/019394599301500212. [DOI] [PubMed] [Google Scholar]
- Becker M. The Health Belief Model and personal health behavior. In: Becker M, editor. Health education monographs. San Francisco: Society for Public Health Education; 1974. pp. 324–473. [Google Scholar]
- Bhatia S, Sather HN, Heerema NA, Trigg ME, Gaynon PS, Robison LL. Racial and ethnic differences in survival of children with acute lymphoblastic leukemia. Blood. 2002;100(6):1957–1964. doi: 10.1182/blood-2002-02-0395. [DOI] [PubMed] [Google Scholar]
- Blais L, Beauchesne MF, Levesque S. Socioeconomic status and medication prescription patterns in pediatric asthma in Canada. Journal of Adolescent Health. 2006;38(5):607, e609–616. doi: 10.1016/j.jadohealth.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Brownbridge G, Fielding DM. Psychosocial adjustment and adherence to dialysis treatment regimes. Pediatric Nephrology. 1994;8(6):744–749. doi: 10.1007/BF00869109. [DOI] [PubMed] [Google Scholar]
- Calvillo ER, Flaskerud JH. Evaluation of the pain response by Mexican American and Anglo American women and their nurses. Journal of Advanced Nursing. 1993;18(3):451–459. doi: 10.1046/j.1365-2648.1993.18030451.x. [DOI] [PubMed] [Google Scholar]
- Carpenter DR. Grounded theory as method. In: Speziale H, Carpenter DR, editors. Qualitative Research in Nursing. 3. Philadelphia: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- Christiansen N, Taylor KM, Duggan C. Oral chemotherapy in paediatric oncology in the UK: problems, perceptions and information needs of parents. Pharmacy World & Science. 2008;30(5):550–555. doi: 10.1007/s11096-008-9208-5. [DOI] [PubMed] [Google Scholar]
- Conn KM, Halterman JS, Lynch K, Cabana MD. The impact of parents’ medication beliefs on asthma management. Pediatrics. 2007;120(3):e521–526. doi: 10.1542/peds.2006-3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbin J, Strauss AL. Basics of qualitative research: Techniques and procedures for developing grounded theory. 3. Thousand Oaks, CA: Sage Publications, Inc; 2008. [Google Scholar]
- Davies HA, Lennard L, Lilleyman JS. Variable mercaptopurine metabolism in children with leukaemia: a problem of non-compliance? BMJ: British Medical Journal. 1993;306(6887):1239–1240. doi: 10.1136/bmj.306.6887.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies HA, Lilleyman JS. Compliance with oral chemotherapy in childhood lymphoblastic leukaemia. Cancer Treatment Reviews. 1995;21(2):93–103. doi: 10.1016/0305-7372(95)90022-5. [DOI] [PubMed] [Google Scholar]
- Dibenedetto SP, Guardabasso V, Ragusa R, Di Cataldo A, Miraglia V, D’Amico S, et al. 6-Mercaptopurine cumulative dose: a critical factor of maintenance therapy in average risk childhood acute lymphoblastic leukemia. Pediatric Hematology and Oncology. 1994;11(3):251–258. doi: 10.3109/08880019409141668. [DOI] [PubMed] [Google Scholar]
- Dimatteo MR. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Education and Counseling. 2004;55(3):339–344. doi: 10.1016/j.pec.2003.04.003. [DOI] [PubMed] [Google Scholar]
- Elliott V, Morgan S, Day S, Mollerup LS, Wang W. Parental health beliefs and compliance with prophylactic penicillin administration in children with sickle cell disease. Journal of Pediatric Hematology/Oncology. 2001;23(2):112–116. doi: 10.1097/00043426-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Everhart RS. Medical adherence and childhood chronic illness: family daily management skills and emotional climate as emerging contributors. Current Opinion in Pediatrics. 2006;18(5):551–557. doi: 10.1097/01.mop.0000245357.68207.9b. [DOI] [PubMed] [Google Scholar]
- Gale RP, Butturini A. Maintenance chemotherapy and cure of childhood acute lymphoblastic leukaemia. Lancet. 1991;338(8778):1315–1318. doi: 10.1016/0140-6736(91)92604-z. [DOI] [PubMed] [Google Scholar]
- Gayer D, Ganong L. Family structure and mothers’ caregiving of children with cystic fibrosis. Journal of Family Nursing. 2006;12(4):390–412. doi: 10.1177/1074840706294510. [DOI] [PubMed] [Google Scholar]
- Gillespie A. G. H. Mead: Theorist of the social act. Journal for the Theory of Social Behavior. 2005;35(1):19–39. [Google Scholar]
- Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA - Journal of the American Medical Association. 2002;288(22):2880–2883. doi: 10.1001/jama.288.22.2880. [DOI] [PubMed] [Google Scholar]
- Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, et al., editors. SEER cancer statistics review, 1975–2006, based on November 2008 SEER data submission. Bethesda, MD: National Cancer Institute; 2009. [Google Scholar]
- Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Jahrami H, Marnoch G, Gray AM. Use of card sort methodology in the testing of a clinical leadership competencies model. Health Services Management Research. 2009;22(4):176–183. doi: 10.1258/hsmr.2009.009007. [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA: A Cancer Journal for Clinicians. 2009;59(4):225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- Kadan-Lottick NS, Ness KK, Bhatia S, Gurney JG. Survival variability by race and ethnicity in childhood acute lymphoblastic leukemia. JAMA – Journal of the American Medical Association. 2003;290(15):2008–2014. doi: 10.1001/jama.290.15.2008. [DOI] [PubMed] [Google Scholar]
- Koren G, Ferrazini G, Sulh H, Langevin AM, Kapelushnik J, Klein J, et al. Systemic exposure to mercaptopurine as a prognostic factor in acute lymphocytic leukemia in children. The New England Journal of Medicine. 1990;323(1):17–21. doi: 10.1056/NEJM199007053230104. [DOI] [PubMed] [Google Scholar]
- Kyngas H, Duffy ME, Kroll T. Conceptual analysis of compliance. Journal of Clinical Nursing. 2000;9(1):5–12. doi: 10.1046/j.1365-2702.2000.00309.x. [DOI] [PubMed] [Google Scholar]
- Lancaster D, Lennard L, Lilleyman JS. Profile of non-compliance in lymphoblastic leukaemia. Archives of Disease in Childhood. 1997;76(4):365–366. doi: 10.1136/adc.76.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham CL, Calvillo E. A health protection model for Hispanic adults with Type 2 diabetes. Journal of Clinical Nursing. 2007;16(7B):186–196. doi: 10.1111/j.1365-2702.2007.01879.x. [DOI] [PubMed] [Google Scholar]
- Lau RC, Matsui D, Greenberg M, Koren G. Electronic measurement of compliance with mercaptopurine in pediatric patients with acute lymphoblastic leukemia. Medical and Pediatric Oncology. 1998;30(2):85–90. doi: 10.1002/(sici)1096-911x(199802)30:2<85::aid-mpo3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Lennard L, Welch J, Lilleyman JS. Intracellular metabolites of mercaptopurine in children with lymphoblastic leukaemia: a possible indicator of non-compliance? British Journal of Cancer. 1995;72(4):1004–1006. doi: 10.1038/bjc.1995.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard BJ, Garwick A, Adwan JZ. Adolescents’ perceptions of parental roles and involvement in diabetes management. Journal of Pediatric Nursing. 2005;20(6):405–414. doi: 10.1016/j.pedn.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Lilleyman JS, Lennard L. Mercaptopurine metabolism and risk of relapse in childhood lymphoblastic leukaemia. Lancet. 1994;343(8907):1188–1190. doi: 10.1016/s0140-6736(94)92400-7. [DOI] [PubMed] [Google Scholar]
- Lilleyman JS, Lennard L. Non-compliance with oral chemotherapy in childhood leukaemia. BMJ: British Medical Journal. 1996;313(7067):1219–1220. doi: 10.1136/bmj.313.7067.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln YS, Guba E. Naturalistic inquiry. Newbury Park, CA: Sage Publications, Inc; 1985. [Google Scholar]
- Logan D, Zelikovsky N, Labay L, Spergel J. The Illness Management Survey: identifying adolescents’ perceptions of barriers to adherence. Journal of Pediatric Psychology. 2003;28(6):383–392. doi: 10.1093/jpepsy/jsg028. [DOI] [PubMed] [Google Scholar]
- MacDougall LG, Wilson TD, Cohn R, Shuenyane EN, McElligott SE. Compliance with chemotherapy in childhood leukaemia in Africa. South African Medical Journal. 1989;75(10):481–484. [PubMed] [Google Scholar]
- Malbasa T, Kodish E, Santacroce SJ. Adolescent adherence to oral therapy for leukemia: a focus group study. Journal of Pediatric Oncology Nursing. 2007;24(3):139–151. doi: 10.1177/1043454206298695. [DOI] [PubMed] [Google Scholar]
- Marhefka SL, Tepper VJ, Brown JL, Farley JJ. Caregiver psychosocial characteristics and children’s adherence to antiretroviral therapy. AIDS Patient Care and STDS. 2006;20(6):429–437. doi: 10.1089/apc.2006.20.429. [DOI] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BO, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- Martin S, Elliott-DeSorbo DK, Wolters PL, Toledo-Tamula MA, Roby G, Zeichner S, et al. Patient, caregiver and regimen characteristics associated with adherence to highly active antiretroviral therapy among HIV-infected children and adolescents. The Pediatric Infectious Disease Journal. 2007;26(1):61–67. doi: 10.1097/01.inf.0000250625.80340.48. [DOI] [PubMed] [Google Scholar]
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA - Journal of the American Medical Association. 2002;288(22):2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- McGhee G, Marland GR, Atkinson J. Grounded theory research: literature reviewing and reflexivity. Journal of Advanced Nursing. 2007;60(3):334–342. doi: 10.1111/j.1365-2648.2007.04436.x. [DOI] [PubMed] [Google Scholar]
- Mead GH, Strauss AL. George Herbert Mead on social psychology. Chicago: The University of Chicago Press; 1977. [Google Scholar]
- Mellins CA, Brackis-Cott E, Dolezal C, Abrams EJ. The role of psychosocial and family factors in adherence to antiretroviral treatment in human immunodeficiency virus-infected children. Pediatric Infectious Disease Journal. 2004;23(11):1035–1041. doi: 10.1097/01.inf.0000143646.15240.ac. [DOI] [PubMed] [Google Scholar]
- Modi AC, Morita DA, Glauser TA. One-month adherence in children with new-onset epilepsy: white-coat compliance does not occur. Pediatrics. 2008;121(4):e961–966. doi: 10.1542/peds.2007-1690. [DOI] [PubMed] [Google Scholar]
- Neufeld A, Harrison MJ, Rempel GR, Larocque S, Dublin S, Stewart M, et al. Practical issues in using a card sort in a study of non-support and family caregiving. Qualitative Health Research. 2004;14(10):1418–1428. doi: 10.1177/1049732304271228. [DOI] [PubMed] [Google Scholar]
- Nevins TE. Non-compliance and its management in teenagers. Pediatric Transplant. 2002;6(6):475–479. doi: 10.1034/j.1399-3046.149.ptr1s077.1.x. [DOI] [PubMed] [Google Scholar]
- Nguyen K, Devidas M, Cheng SC, La M, Raetz EA, Carroll WL, et al. Factors influencing survival after relapse from acute lymphoblastic leukemia: a Children’s Oncology Group study. Leukemia. 2008;22(12):2142–2150. doi: 10.1038/leu.2008.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson O, Mellins C, Dolezal C, Brackis-Cott E, Abrams EJ. HIV treatment-related knowledge and self-efficacy among caregivers of HIV-infected children. Patient Education and Counseling. 2006;61(3):405–410. doi: 10.1016/j.pec.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Orrell-Valente JK, Jarlsberg LG, Hill LG, Cabana MD. At what age do children start taking daily asthma medicines on their own? Pediatrics. 2008;122(6):e1186–1192. doi: 10.1542/peds.2008-0292. [DOI] [PubMed] [Google Scholar]
- Partridge AH, Avorn J, Wang PS, Winer EP. Adherence to therapy with oral antineoplastic agents. Journal of the National Cancer Institute. 2002;94(9):652–661. doi: 10.1093/jnci/94.9.652. [DOI] [PubMed] [Google Scholar]
- Patino AM, Sanchez J, Eidson M, Delamater AM. Health beliefs and regimen adherence in minority adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2005;30(6):503–512. doi: 10.1093/jpepsy/jsi075. [DOI] [PubMed] [Google Scholar]
- Pollock BH, DeBaun MR, Camitta BM, Shuster JJ, Ravindranath Y, Pullen DJ, et al. Racial differences in the survival of childhood B-precursor acute lymphoblastic leukemia: a Pediatric Oncology Group Study. Journal of Clinical Oncology. 2000;18(4):813–823. doi: 10.1200/JCO.2000.18.4.813. [DOI] [PubMed] [Google Scholar]
- Pritchard MT, Butow PN, Stevens MM, Duley JA. Understanding medication adherence in pediatric acute lymphoblastic leukemia: a review. Journal of Pediatric Hematology/Oncology. 2006;28(12):816–823. doi: 10.1097/01.mph.0000243666.79303.45. [DOI] [PubMed] [Google Scholar]
- Punch KF. Introduction to social research. 2. Thousand Oaks, CA: Sage Publications, Inc; 2005. [Google Scholar]
- Rapoff MA. Adherence to pediatric medical regimens. New York: Kluwer Academic/Plenum Publishers; 1999. [Google Scholar]
- Rapoff MA. Management of adherence and chronic rheumatic disease in children and adolescents. Best Practice & Research: Clinical Rheumatology. 2006;20(2):301–314. doi: 10.1016/j.berh.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Rose D, Garwick A. Urban American Indian family caregivers’ perceptions of barriers to management of childhood asthma. Journal of Pediatric Nursing. 2003;18(1):2–11. doi: 10.1053/jpdn.2003.2. [DOI] [PubMed] [Google Scholar]
- Sackett DL. Introduction. In: Sackett DL, Haynes RB, editors. Compliance with therapeutic regimens. Baltimore: The Johns Hopkins University Press; 1979. pp. 1–6. [Google Scholar]
- Salabarria-Pena Y, Trout PT, Gill JK, Morisky DE, Muralles AA, Ebin VJ. Effects of acculturation and psychosocial factors in Latino adolescents’ TB-related behaviors. Ethnicity and Disease. 2001;11(4):661–675. [PubMed] [Google Scholar]
- Schmidt LE, Dalhoff K. Food-drug interactions. Drugs. 2002;62(10):1481–1502. doi: 10.2165/00003495-200262100-00005. [DOI] [PubMed] [Google Scholar]
- Schmiegelow K, Schroder H, Gustafsson G, Kristinsson J, Glomstein A, Salmi T, et al. Risk of relapse in childhood acute lymphoblastic leukemia is related to RBC methotrexate and mercaptopurine metabolites during maintenance chemotherapy. Nordic Society for Pediatric Hematology and Oncology. Journal of Clinical Oncology. 1995;13(2):345–351. doi: 10.1200/JCO.1995.13.2.345. [DOI] [PubMed] [Google Scholar]
- Sidelinger DE, Meyer D, Blaschke GS, Hametz P, Batista M, Salguero R, et al. Communities as teachers: learning to deliver culturally effective care in pediatrics. Pediatrics. 2005;115(4 Suppl):1160–1164. doi: 10.1542/peds.2004-2825L. [DOI] [PubMed] [Google Scholar]
- Simone JV. History of the treatment of childhood ALL: a paradigm for cancer cure. Best Practice & Research: Clinical Haematology. 2006;19(2):353–359. doi: 10.1016/j.beha.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Smith BA, Shuchman M. Problem of nonadherence in chronically ill adolescents: strategies for assessment and intervention. Current Opinion in Pediatrics. 2005;17(5):613–618. doi: 10.1097/01.mop.0000176443.26872.6e. [DOI] [PubMed] [Google Scholar]
- Sobo EJ. Good communication in pediatric cancer care: a culturally-informed research agenda. Journal of Pediatric Oncology Nursing. 2004;21(3):150–154. doi: 10.1177/1043454204264408. [DOI] [PubMed] [Google Scholar]
- Sofianou-Katsoulis A, Khakoo G, Kaczmarski R. Reduction in bioavailability of 6-mercaptopurine on simultaneous administration with cow’s milk. Pediatric Hematology and Oncology. 2006;23(6):485–487. doi: 10.1080/08880010600796095. [DOI] [PubMed] [Google Scholar]
- Strauss AL. Qualitative analysis for social scientists. Cambridge: Cambridge University Press; 1987. [Google Scholar]
- Strauss AL, Corbin J. Basics of qualitative research: Grounded theory procedures and techniques. Thousand Oaks, CA: Sage Publications, Inc; 1990. [Google Scholar]
- Strauss AL, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Thousand Oaks, CA: Sage Publications, Inc; 1998. [Google Scholar]
- Tebbi CK, Richards ME, Cummings KM, Zevon MA, Mallon JC. The role of parent-adolescent concordance in compliance with cancer chemotherapy. Adolescence. 1988;23(91):599–611. [PubMed] [Google Scholar]
- Tumiel-Berhalter L, Zayas LE. Lay experiences and concerns with asthma in an urban Hispanic community. Journal of the National Medical Association. 2006;98(6):875–880. [PMC free article] [PubMed] [Google Scholar]
- Williams PL, Storm D, Montepiedra G, Nichols S, Kammerer B, Sirois PA, et al. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics. 2006;118(6):e1745–1757. doi: 10.1542/peds.2006-0493. [DOI] [PubMed] [Google Scholar]
- Wolff G, Strecker K, Vester U, Latta K, Ehrich JH. Non-compliance following renal transplantation in children and adolescents. Pediatric Nephrology. 1998;12(9):703–708. doi: 10.1007/s004670050531. [DOI] [PubMed] [Google Scholar]