Abstract
This study examined the long-term outcomes of women who were pregnant or parenting at admission to women-only (WO; n=500) versus mixed-gender (MG; a matched sample of 500) substance abuse treatment programs. Administrative records on arrests, incarcerations, mental health services utilization, and drug treatment participation were collected, covering 3 years pre-admission and 8 years post-admission. Women treated in WO programs had lower levels of arrest, mental health services utilization rates, and drug treatment participation during the first year after drug treatment. No differences were found between the two groups in the long-term trajectories except that WO program participants had lower incarceration rates during the third year after treatment. The study findings suggest a positive short-term impact of WO versus MG programs with regard to arrest and mental health service utilization. Limited long-term gain is shown in the reductions in post-treatment incarceration. The study findings suggest the added value of specialized WO programs and begin to address the gap in knowledge regarding long-term outcomes for substance-abusing women.
Keywords: Long-term outcomes, drug dependent mothers, women-only program, mixed-gender programs
Introduction
Abuse of alcohol and illicit drugs can cause serious psychological and physical health problems for mothers and their children. Nationally about 5% of pregnant women use an illicit drug during pregnancy (Substance Abuse and Mental Health Services Administration, 2009), a figure that is believed to be an underestimation due to the stigma associated with substance abuse during pregnancy, and the accompanying legal, ethical, and economic issues (Huestis & Choo, 2002). Additionally, pregnant women who have recently used illicit substances may delay seeking prenatal care, further compromising the health of their children (Staton et al., 2003; Wagner et al., 1998). A mothers' ongoing substance abuse, and the chaotic home environment it creates, can have detrimental effects on children's psychological growth and development as well. The long-term effects of maternal drug use on children's overall well-being remain relatively unknown, but what is clear is that without intervention the children of substance-abusing mothers are at high-risk to continue intergenerational patterns of substance abuse, criminal behaviors, and neglectful parenting (Dunn et al., 2002; Greene, Haney, & Hurtado, 2000).
In recent years, increased numbers of women-only (WO) substance abuse programs have offered special services to address the unique problems and service needs among substance-abusing mothers, including child care and parenting services. Several studies assessing these types of programs have reported positive effects for women participating in WO programs compared to those in mixed gender (MG) programs (e.g., greater treatment retention or completion, reductions in substance abuse, and criminal activities), but these studies are restricted to short-term observations during or shortly after treatment (Grella, Joshi, & Hser, 2000; Prendergast, Messina, & Hall, under review). Few studies have examined longitudinal outcomes of women served in WO programs. A better understanding of the long-term outcomes among mothers and their children associated with WO and MG programs can help to improve existing services and interventions to prevent or ameliorate the adverse consequences associated with substance abuse among pregnant and parenting women. The purpose of the present study is to investigate long-term outcomes over a period of 8 years for mothers treated in WO versus MG treatment programs.
Unique Treatment Needs of Women
Substance-abusing pregnant and parenting women face many life challenges and have tremendous needs for medical issues, mental health, and other social support services. Many studies have shown that compared with substance-abusing men, women are more likely to have coexisting psychiatric problems, lower self-esteem, and extensive histories of traumatic life events, including sexual and physical abuse (Hser et al., 2003; Messina, Burdon, & Prendergast, 2003; Messina et al., 2000; Messina & Grella, 2006). Most substance-abusing women have limited education, are unemployed, and rely on public assistance and/or illegal activities as their primary source of income. Drug use by these women is often initiated by their male partners (Hser et al., 1987; Messina, Burdon, Hagopian, & Prendergast, 2006; Owen, 1998), and the women frequently continue to use drugs to cope with abusive relationships and other life stressors (Covington & Surrey, 1997; Messina et al., 2003; Owen, 1998).
Specialized Treatment for Women
In response to an increased awareness of the unique issues and service needs of substance-abusing women, especially those who are pregnant or parenting, specialized programs or services for women increased during the late 1980s and early 1990s. Although the standard of care for women in the community remains equivalent to that found in the MG treatment environment (Grella et al., 1999; Grella et al., 2000), WO programs are more likely than MG programs to offer special services such as childcare and prenatal and postpartum care for pregnant women, assistance with housing, transportation, job training, practical skills training, and on-site childcare services (Ashley et al., 2003; Brady & Ashley, 2005; Grella et al., 1999). Women-only programs also tend to employ only women in counseling positions, creating a gender-specific environment. By contrast, MG programs usually employ both men and women in counseling positions and combine men and women together in treatment.
Gaps in Knowledge
The literature assessing post-treatment outcomes for women in WO programs is limited in both number and design. A meta-analysis of four studies conduced by Orwin et al. (2001) is the first formal quantitative synthesis of the outcome studies on women's treatment contrasting women in WO versus MG treatment programs. The authors reported significantly reduced psychiatric problems for the treatment participants in the WO programs. Other post-treatment outcomes such as reduced criminal behaviors and improved attitudes/beliefs were in a positive direction but had small effect sizes. The authors suggest that findings should be interpreted with caution due to the limited number of studies available and/or eligible for the meta-analysis. A more recent study contrasting outcomes of WO and MG treatment programs showed that WO participants reported less drug use and criminal activity at the one year follow up, but no differences were found in official arrest or employment rates (Prendergast et al., under review). Although participants in each type of program received treatment for similar lengths of time, the additional services provided in the WO programs may have implied greater treatment intensity. Two additional studies further showed that women treated in WO programs were more likely to be engaged in continuity of care after the initial treatment episode (Claus et al., 2007; Messina, Grella, Cartier, & Torres, 2010).
Reported outcomes are often restricted to completion or retention rates and are sometimes inconsistent. For example, while some studies indicate that women in WO programs were more likely to complete treatment than those in MG programs (Grella, 1999; Dahlgren & Willander, 1989), other studies found women in specialized women's programs were less likely to complete treatment than women in regular programs (Harrison & Asche, 2001) or there was no difference in completion rates between the two (Kaskutas et al., 2005). Nevertheless, similar to the broader treatment literature for other populations showing that treatment success is associated with time in treatment, studies of pregnant substance abusers have also reported that greater treatment retention is related to healthier pregnancies and improved neonatal outcomes (Greenfield et al., 2004; Howell et al., 1999; Kissin et al. 2004).
In sum, empirical assessment of the effectiveness of WO programs compared to traditional programs or MG programs is growing but limited (Greenfield et al., 2007). Some studies have begun to show the positive short-term impact of services that are designed to meet the needs of substance-abusing women. Long-term outcomes and the factors that sustain successful recovery are relatively unstudied for this population. It is vitally important to gain insight from empirical evidence to determine the critical factors associated with the desistence of substance use and the types of settings, services and approaches that are optimal to enhance long-term outcomes.
California Treatment Outcome Project (CalTOP) and the Present Study
The present study applies propensity score matching methods (see Method section) to select women treated in WO versus MG substance abuse treatment programs and compares their long-term outcomes over an 8 year period. Given that the literature has shown some mixed results regarding outcomes associated with different types of programs, and that most existing studies are limited by short-term observations, the current study findings can add vital information to the overall knowledge base regarding the long-term effects of treatment for pregnant and parenting women. The sample and data are drawn from those originally collected in the California Treatment Outcome Project (CalTOP). CalTOP programs included 32 MG programs, 8 WO programs, and 3 men-only facilities
Compared to the MG programs, the WO programs in CalTOP were significantly more likely to offer child care and child development services, mothering groups, and HIV testing (Hser & Niv, 2006). Of the intake sample of 6,255 women, 189 women in the WO programs and 871 women in the MG programs had completed the 3-month and 9-month assessments. We compared their service needs at intake, service utilization at 3-month follow-up, and outcomes at the 9-month follow-up interview (Niv & Hser, 2007). In contrast to women in the MG programs, women in the WO programs were more likely to be white, less educated, physically abused in the 30 days prior to intake, and in residential programs. Women in the WO programs also had greater problem severity in a number of domains including alcohol, drug, family, medical, and psychiatric. They utilized more treatment services (drug, alcohol, employment, medical, psychiatric, parenting & HIV services), and had better drug and legal/arrest outcomes at the 9-month follow-up (Niv & Hser, 2007).
Building on our prior work, the purpose of the present study is to investigate the long-term outcomes of mothers (women who were pregnant or parenting) admitted to WO versus MG substance abuse treatment programs. Specifically, we examine a matched sample of 1,000 mothers treated for substance abuse between 2000 and 2002 in WO versus MG programs and compare their long-term outcomes via their administrative records. Our hypotheses are as follows. Compared to women in MG programs, mothers treated in WO programs will demonstrate less subsequent involvement with the criminal justice system (less arrest and incarceration), less mental health services utilization, and less subsequent drug treatment participation.
Methods
As part of CalTOP, conducted in multiple counties of California, approximately 4,500 pregnant or parenting women (i.e., women having dependent children or children under age 18) from 8 WO programs and 32 MG programs were assessed at admission between 2000 and 2002. Administrative records of these mothers were updated in 2009 on arrests, incarcerations, mental health services utilization, and drug treatment participation. The State of California and UCLA Institutional Review Boards reviewed and approved all study procedures.
Sample
To assess differences in outcomes between the WO vs. MG programs, we used propensity matching procedures to select an equivalent 500 women from each type of program. Post-treatment outcomes were assessed over 8 years. Table 1 provides characteristics at treatment intake by the two groups for the overall samples as well as the subgroups selected by propensity matching. The two groups without matching were significantly different in many aspects (mostly consistent with those reported in literature), and these differences were no longer significant within the matched groups.
Table 1.
Client Demographics, Family Relationships, and Substance Use Treatment History at Drug Treatment Admission
| Total Sample (n=4,448) | Matched Sample (n=1,000) | |||
|---|---|---|---|---|
| Mixed-gender Programs (n=3.688) |
Women-only Programs (n=760) |
Mixed-gender Programs (n=500) |
Women-only Programs (n=500) |
|
|
Demographic and background characteristics |
||||
| Age, mean (SD) | 33.1 (7.6) | 32.4 (7.5) ** | 30.5 (7.3) | 31.9 (7.3) ** |
| Pregnant at intake, % | 7.43 | 17.50 ** | 45.20 | 73.40 ** |
| Race/Ethnicity, % | ** | |||
| White | 54.4 | 60.5 | 57.23 | 56.91 |
| African American | 16.5 | 15.7 | 13.05 | 18.84 |
| Hispanic | 23.3 | 16.8 | 22.49 | 17.84 |
| Other | 5.8 | 7.0 | 7.23 | 6.41 |
| ≥ High school , % | 58.89 | 57.63 | 53.40 | 54.80 |
| Never married, % | 39.5 | 41.0 | 48.40 | 44.40 |
| Employed, % | 23.2 | 18.6 ** | 13.40 | 15.40 |
| On public assistance, % | 37.0 | 39.1 | 36.20 | 41.40 |
| Family relationships, % | ||||
| Number of children living with women in prior 30 days |
** | |||
| None | 1.00 | 2.89 | 7.20 | 4.40 |
| 0 | 51.71 | 54.21 | 52.60 | 51.20 |
| 1-3 | 43.03 | 39.08 | 36.20 | 39.20 |
| 4+ | 4.26 | 3.82 | 4.00 | 5.20 |
| Children living with someone else by court order |
33.79 | 31.71 | 30.20 | 29.40 |
| Parental rights were terminated | 15.3 | 10.39 ** | 13.20 | 9.80 |
| Substance use treatment history | ||||
| Primary drug problem, % | ** | |||
| Methamphetamine | 41.66 | 39.47 | 43.80 | 36.60 |
| Heroin | 12.70 | 18.95 | 21.60 | 22.20 |
| Alcohol | 21.22 | 21.97 | 16.60 | 20.00 |
| Cocaine | 12.02 | 9.08 | 9.20 | 10.20 |
| Marijuana | 9.93 | 9.34 | 7.80 | 10.20 |
| Other drugs | 2.47 | 1.18 | 1.00 | 0.80 |
| Number of prior alcohol treatments (SD) | 0.75 (2.54) | 1.13 (2.78) ** | 0.79 (2.62) | 1.16 (3.11) |
| Number of prior drug treatments (SD) | 1.69 (3.21) | 2.35 (4.09) ** | 2.01 (3.22) | 2.56 (4.41) |
p<0.05
P<0.01
Propensity Score Matching Methods
In the absence of an experimental study design, propensity score adjustment is a popular statistical technique for reducing the impact of selection bias in estimation of causal effects using observational data (D'Agostino, 1998; Feng et al., 2006; Rosenbaum & Rubin, 1983; Rubin, 1997; Rubin & Thomas, 1996; Ye & Kaskutas, 2008). The propensity score is a subject's probability of receiving a specific service conditional on observed covariates for this analysis. Matched pairs were constructed using the nearest available Mahalanobis metric matching within calipers defined by the propensity score.
Specifically, we considered WO programs as the “case” group and MG programs as “control” group: (1) Propensity score was computed based on 47 variables at intake (31 variables are presented in the Table 1). (2) Women in both groups were first stratified by treatment modality at intake and psychiatric severity at intake. (3) Treatment modalities were residential, outpatient and methadone maintenance. (4) Psychiatric severity was indicated by the Addiction Severity Index (ASI) psychiatric score and separated using a median split as HIGH and LOW categories. (5) All women in each group were divided into six sub-strata. (6) Matched pairs were searched only among subjects that belonged to the same stratum. (7) The matching procedure was divided into 3 steps and was started with pregnant women first. Step 1: Given each pre-stratified stratum, a matched subject from the MG programs was found for each pregnant woman in WO programs. Step 2: Of the remaining unmatched subjects, a matched subject from WO programs was found for each pregnant woman in a MG program, given each pre-stratified stratum. Step 3. Of the remaining unmatched subjects, a matched subject was found from MG programs for a subject in a WO program, given each pre-stratified stratum.
Measures
The present study include data collected at intake using the ASI, as well as administrative records on criminal justice involvement, mental health services utilization, and drug treatment participation over 11 years of observations (3 years prior to the CalTOP entry and 8 years afterwards).
Addiction Severity Index (ASI; McLellan et al., 1992)
The ASI is a structured interview that assesses problem severity in seven areas: alcohol use, drug use, employment, family and social relationships, legal, medical status, and mental health. A composite score was computed for each of the scales to indicate severity in that area; the range of scores is 0 to 1 with higher scores indicating greater problem severity.
Arrests and Incarcerations
Patients' involvement in the criminal justice system (e.g. arrests, incarcerations) was obtained from the Automated Criminal History System of the California Department of Justice (DOJ).
Drug treatment
Information on alcohol and drug treatment received from public providers, as well as from methadone treatment providers that are licensed by the state, was obtained from the California Alcohol and Drug Data System (CADDS) from the state Department of Alcohol and Drug Programs. CADDS tracks all admission and discharge episodes and provides data on: dates of admission and discharge; types of drugs used; treatment type, duration, and discharge status; and other information.
Mental health
Information regarding mental health services and diagnoses was obtained from the California Department of Mental Health (DMH). DMH maintains the Client and Service Information (CSI), a database with services and psychiatric diagnoses for clients treated in mental health facilities that received DMH funds.
Analysis
For the total and the matched samples respectively, women were compared between the two treatment types by using ANOVA on continuous measures and Chi-square tests on categorical measures. Analyses were first conducted to examine demographic characteristics, ASI severity scores and parenting status at intake. Trajectories of arrests, incarcerations, and mental health and drug treatment services utilization across 11-year period were depicted for women in WO and MG programs. Utilizing the matched sample and using SAS PROC MIXED, growth curve modeling was conducted to examine 8-year trajectories after CalTOP enrollment for the WO versus MG programs. Differences on intercepts and slopes of trajectories between the two programs were tested using F-statistic. Because growth curve models are not sensitive to point differences, supplemental tests were conducted to identify differences in specific time points. The significance level for all statistical tests was set at p < 0.05.
Results
Sample Characteristics
Consistent with prior findings, analysis of client characteristics at treatment admission showed differences between women treated in the WO settings versus MG settings for the total sample (see Tables 1 & 2). Women in the WO programs generally demonstrated greater problem severity in many key life domains at intake. However, with a few exceptions, these differences were eliminated for the matched sample. The characteristics of the matched sample are as follows. At intake, the women were at their early 30s and more than 40% had never been married. By study design, these women were either pregnant or had children, but almost a third had children living with someone else by court order, and about 10% had their parental rights terminated. Methamphetamine was the leading primary drug (40%), followed by heroin, alcohol, cocaine, and marijuana. On average, the women had at least 2 prior drug treatments, and some had a history of alcohol treatment. Only about 13-15% of women were employed and almost 40% were receiving public assistance. Consistent with previous literature, many of the women reported psychiatric problems with 30-40% reporting serious depression or anxiety. More than 10% were taking psychiatric medications.
Table 2.
Client ASI Scores, Criminal Justice Involvement, and Psychiatric Characteristics at Drug Treatment Admission
| Total Sample (n=4,448) | Matched Sample (n=1,000) | |||
|---|---|---|---|---|
| Mixed-gender Programs (n=3.688) |
Women-only Programs (n=760) |
Mixed-gender Programs (n=500) |
Women-only Programs (n=500) |
|
| ASI scores, mean (SD) | ||||
| Alcohol | 0.15 (0.24) | 0.19 (0.25) ** | 0.14 (0.24) | 0.17 (0.25) |
| Drug | 0.12 (0.12) | 0.16 (0.12) ** | 0.15 (0.13) | 0.16 (0.12) |
| Employment | 0.73 (0.29) | 0.77 (0.27) ** | 0.80 (0.25) | 0.79 (0.26) |
| Family | 0.21 (0.24) | 0.25 (0.25) ** | 0.22 (0.23) | 0.22 (0.24) |
| Legal | 0.15 (0.20) | 0.20 (0.21) ** | 0.19 (0.22) | 0.19 (0.20) |
| Medical | 0.20 (0.31) | 0.25 (0.33) ** | 0.22 (0.32) | 0.23 (0.32) |
| Psychiatric | 0.24 (0.25) | 0.30 (0.24) ** | 0.24 (0.24) | 0.26 (0.24) |
| Criminality/ legal system involvement, % | ||||
| Ever arrested | 77.1 | 82.8 ** | 79.80 | 83.40 |
| Crime involved in the past 30 days | 56.6 | 59.5 | 57.80 | 59.40 |
| Psychiatric symptoms, % | ||||
| Psychiatric medications – in the past 30 days | 17.3 | 21.2 * | 13.80 | 15.20 |
| Psychiatric symptoms – in the past 30 days | ||||
| Serious depression | 38.0 | 42.2 * | 36.20 | 37.80 |
| Serious anxiety | 42.6 | 52.1 ** | 45.20 | 44.60 |
| Hallucinations | 6.1 | 5.5 | 3.80 | 5.20 |
| Trouble understanding, concentrating, or remembering | 30.2 | 41.7 ** | 33.60 | 37.00 |
| Trouble controlling violent behavior | 12.0 | 13.6 | 12.40 | 12.20 |
| Serious thoughts of suicide | 7.6 | 9.6 | 7.00 | 8.20 |
| Attempted suicide | 2.0 | 2.0 | 2.20 | 2.20 |
| Ever in Inpatient psychiatric treatment | 23.9 | 25.1 | 19.20 | 22.00 |
| Ever in Outpatient psychiatric treatment | 36.1 | 46.8 ** | 32.80 | 41.00 ** |
p<0.05
P<0.01
Criminal Justice System Involvement
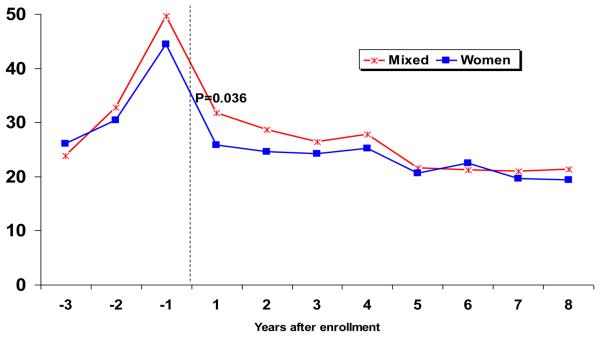
More than 80% of women reported an arrest history and more than 40% had an arrest record during the year prior to CalTOP entry. Women in both WO and MG programs showed significant reductions in arrest after treatment with significantly fewer mothers in WO than MG programs being arrested during the first year after treatment. Differences between the two groups became smaller and diminished as time passed (see Figure 1). Mixed modeling results confirmed that arrest trajectories significantly decreased across years (p<0.01). Arrest rate was significantly different by program type at the first year post-entry (Intercept, p=0.04), but the slope was not different between programs.
Figure 1.
Percent of Arrest over Time
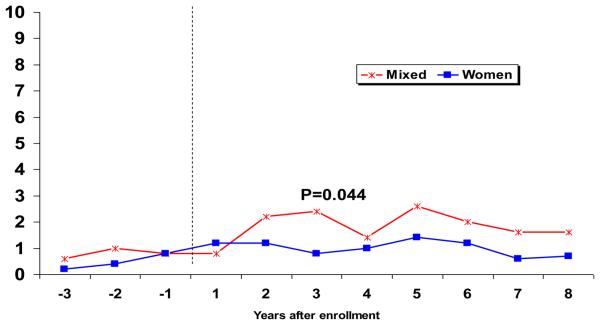
The trajectories of incarceration however, demonstrated slightly different patterns between the two groups (see Figure 2). The rate of incarceration remained stably low among mothers in WO programs, but incarceration increased for mothers in MG programs approximately 2 years after CalTOP treatment and was significantly higher than mothers in WO programs during the third year post-treatment.
Figure 2.
Percent of Incarceration over Time
Mental Health Services
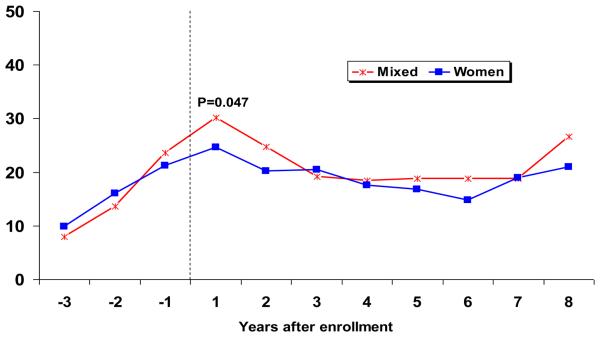
For mothers in both WO and MG programs, mental health services utilization actually increased during the first year post-CalTOP, but reduced or leveled off subsequently (p < .01) (Figure 3). Differences between the two groups were only significant for the first year, with more mothers in MG programs (30%) accessing mental health services than mothers in WO programs (25%).
Figure 3.
Percent of Using Mental Health Services over Time
Drug Abuse Treatment Involvement
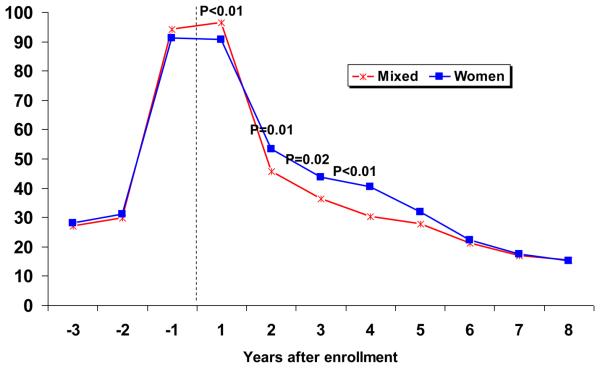
Treatment trajectories significantly decreased across years (p<0.01). While mothers in MG programs continued in treatment during the first year post-CalTOP at a significantly higher level than mothers in WO programs, the pattern was reversed during the subsequent years, until about 5 years post intake and beyond (see Figure 4).
Figure 4.
Percent Using Drug Treatment Services over Time
Discussion
The present study on the long-term outcomes of women treated in WO versus MG programs is, to our knowledge, the first of this kind reported in the substance abuse treatment literature. Our findings suggest that short and some limited long-term outcomes after treatment may be improved for mothers treated in WO versus MG drug treatment programs, even after propensity score adjustments. In the matched sample, women treated in WO treatment programs had lower mental health services utilization rates and arrest rates during the first year after treatment. While ongoing drug treatment utilization was also lower among women treated in the WO programs during the first year post-CalTOP, it was higher in subsequent three years compared with those in the MG programs. No differences were found between the two groups in the long-term trajectories of incarceration except that WO program participants had lower incarceration rates during the third year after treatment.
Previous literature has found that programs that provide child care and/or provide services for children have been shown to improve mothers' retention in treatment and short-term post-treatment outcomes, as well as contributing to the development of inter-organizational linkages between prenatal care providers, child protection systems, and other mental health and social services systems (Clark, 2001; Howell & Chasnoff, 1999; Howell et al., 1999; Hughes et al., 1995; Messina & Chand, 2009). Consistent with this literature, our study demonstrated the short-term positive impact of WO programs with regard to reductions in mental health service utilization and recorded criminal activity (relative to MG programs). It is possible that participants in the WO programs received less mental health services because they had improved post-treatment psychological well-being as a result of program services which better addressed their mental health needs. Moreover, improved psychological functioning may have resulted in a reduction in offending and subsequent arrest, as there is a very strong association between mental health and criminal behaviors among women. However, it is also possible that women participating in the WO programs were more likely to be involved with multiple systems, such as child protective services, resulting in reductions in criminal activity from fear of loss of custody of their children.
Our findings of drug treatment utilization over time are somewhat different from those studies which found that specialized WO programs increased participation in post-treatment aftercare and for a longer period of time than those in standard treatment programs (Claus et al., 2007; Messina et al., 2010). In our study, women in the WO programs demonstrated a lower level of treatment participation during the first year after treatment admission, but their treatment participating became higher in the subsequent years. Interpretation of the drug treatment participation is complex. For example, data may reflect a traditional “ramp” effect, that is, because these women were recruited from treatment facilities, their treatment utilization appears to increase at the time of the index episode and then, in comparison, decrease markedly thereafter. Also, as we do not know if treatment participation is due to relapse or a means to avoid relapse and to meet their other needs. Many these women are engaged with multiple agencies (as pregnant and parenting women) which created an increased awareness of the need for continued care. It is possible that the WO participants become more engaged in care/or return to care over the long-term when services which meet their specific needs were originally provided. Thus providing appropriate treatment services for pregnant and parenting women entering treatment programs may be more effective for promoting long-term recovery and overall wellbeing. Continued involvement in treatment of these WO participants could account for some of the positive findings revealed in the present study. However, the outcome trajectories for WO and MG participants converged in the long-run. Nevertheless, longer-term patterns of outcomes are more complicated to interpret, as non-treatment factors occurring over time may influence the trajectory of outcomes (e.g., relationships with family and children, employment, or marriage).
Several strengths of the study design which enhance the validity and reliability of our findings should be noted. First, our study included a large and diverse sample of pregnant and parenting substance-abusing mothers, more so than that found in the previous literature. Second, the inclusion of multiple treatment sites and a diversity of treatment settings increases the generalizability of our findings, as many existing studies of substance-using women rely on observation of a single site and a single intervention with a demographically similar sample. Third, the propensity score design for matched comparison groups is an innovative design in lieu of random assignment. Fourth, examination of the long-term outcomes of substance abuse treatment is relatively unstudied. Finally, focusing on the understudied and underserved population of substance-abusing women can add to the knowledge gap regarding appropriate services for this population. Substance abuse treatment can be a significant turning point in the life course, promoting family unification and long-term recovery, but understanding the specific needs and responses for women is of utmost importance to have lasting effects.
Limitations
We acknowledge several study limitations. The present study is not a randomized experimental study. For ethical and practical reasons, random assignment of participants to either a WO or MG treatment program was not possible (i.e., it would be unethical to randomize pregnant and parenting mothers to a treatment program that does not provide for their specific needs if it is otherwise available. Also, it is very difficult to implement a randomized study design in large statewide field evaluations). Applying propensity matching procedures using a large number of pre-treatment measures (47), the baseline group differences were largely eliminated but a few remained (e.g., ages of 30.5 vs. 31.9; pregnant status of 45% versus 73%; and prior outpatient psychiatric treatment 33% versus 41%). These differences may have influenced the long-term trajectories examined in the study. Also, although a propensity score approach allows the evaluation of causal effects via multivariate analyses, it can also exclude study participants due to incomplete or inexact matching. In addition, sensitivity analyses revealed significant differences in patient characteristics between the total and matched samples. It may be that the population of women at MG agencies does not sufficiently overlap the population of women at WO agencies to generalize more broadly.
To our knowledge there are no standardized programming requirements for WO programs in California but it is possible that as a condition of funding, WO programs may have had to observe specific standards and requirements may vary by contract. The study did not collect data on programming requirements for WO programs. Possible structural differences between program types and their impact on treatment outcomes remains an important area for future research.
The study utilized administrative data, a data source that is subject to over- or under-reporting of behaviors (McCarty et al., 1998; Saunders & Heflinger, 2004). For example, measures of arrest and drug treatment/mental health services utilization that relied on administrative data did not capture events that may have occurred outside of California. Also omitted from analysis were any events they may have occurred but did not come to the attention of the institution from which data was acquired (e.g., utilization of health services in non-publicly funded settings; crimes for which there was no arrest). Nevertheless, we have applied similar procedures in prior work (Hser & Evans, 2008), and consistent with other literature on the uses of administrative data for research purposes (e.g., Evans et al., 2010; McCarty et al., 1998), we have found that administrative data contribute valuable information, particularly in the investigation of service system interactions and outcomes among substance abusers as they unfold and influence each other over the long term (Evans et al., 2010).
Conclusion
To date, WO programs represent a small proportion of available programs within the overall substance abuse treatment system. Yet these specialized programs serve an important function in providing services to women who present with more severe problems and may not seek treatment in traditional MG programs, such as pregnant and/or parenting women. The present study oversampled pregnant women because they face additional medical, psychological, legal, and family problems associated with their substance abuse. Despite study limitations, our findings provide evidence of the positive short-term impact of these programs in arrest and mental health utilization, and limited long-term gain was observed in the incarceration outcomes. Taken together the findings indicate some positive impacts of WO programs for this population of women. Future studies should examine other outcomes, particularly the program effects on these mothers' children development and well-being.
Female substance abusers often come in contact with multiple service systems including substance abuse treatment, criminal justice, mental health, welfare, and primary health care. A full examination of addiction and recovery of women acknowledges the effects of both individual-level factors and treatment and criminal justice processes themselves. Treatment philosophies and availability of services also change over time (i.e., proportion of women in treatment, modalities, services related to pregnancy, parenting, domestic violence), as well as relevant social policies. Such time-sensitive policies must also be taken into account when assessing the impact of treatment interventions (Grella & Greenwell, 2004). In order to best address the needs of substance-abusing pregnant or parenting women and to curtail the intergenerational cycle of abuse and addiction, future studies should continue to address these critical issues in-depth and over time.
Acknowledgement
This study is funded by the National Institute on Drug Abuse Grant No. R01DA021183. Dr. Hser is also supported by P30DA016383 and K05DA017648.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: A review. American Journal of Drug and Alcohol Abuse. 2003;29(1):19–53. doi: 10.1081/ada-120018838. [DOI] [PubMed] [Google Scholar]
- Brady TM, Ashley OS, editors. Women in substance abuse treatment: Results from the Alcohol and Drug Services Study (ADSS) Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2005. (DHHS Publication No. SMA 04-3968, Analytic Series A-26) [Google Scholar]
- Clark HW. Residential substance abuse treatment for pregnant and postpartum women and their children: Treatment and policy implications. Child Welfare. 2001;80(2):179–198. [PubMed] [Google Scholar]
- Claus RE, Orwin RG, Kissin W, Krupski A, Campbell K, Stark K. Does gender-specific substance abuse treatment for women promote continuity of care? Journal of Substance Abuse Treatment. 2007;32:27–39. doi: 10.1016/j.jsat.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Covington SS, Surrey JL. The relational model of women's psychological development: Implications for substance abuse. In: Wilsnack RW, Wilsnack SC, editors. Gender and alcohol: Individual and social perspectives. Rutgers Center of Alcohol Studies; Piscataway, NJ, US: 1997. pp. 335–351. [Google Scholar]
- D'Agostino R. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Dahlgren L, Willander A. Are special treatment facilities for female alcoholics needed? A controlled 2-year follow-up study from a specialized female unit (EWA) versus a mixed male/female treatment facility. Alcoholism Clinical & Experimental Research. 1989;13:499–504. doi: 10.1111/j.1530-0277.1989.tb00366.x. [DOI] [PubMed] [Google Scholar]
- Dunn M, Tarter R, Mezzich A, Vanyukov M, Kirisci L, Kirillova G. Origins and consequences of child neglect in substance abuse families. Clinical Psychology Review. 2002;22:1063–1090. doi: 10.1016/s0272-7358(02)00132-0. [DOI] [PubMed] [Google Scholar]
- Evans E, Grella C, Murphy D, Hser YI. Using administrative data for longitudinal substance abuse research. Journal of Behavioral Health Services & Research. 2010;37:252–271. doi: 10.1007/s11414-008-9125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng W, Jun Y, Xu R. A Method/Macro Based on Propensity Score and Mahalanobis Distance to Reduce Bias in Treatment Comparison in Observational Study. SAS Technical Report. 2006:1–11. paper PR05. [Google Scholar]
- Greene S, Haney C, Hurtado A. Cycles of pain: Risk factors in the lives of incarcerated mothers and their children. Prison Journal. 2000;80(1):3–23. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, et al. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield L, Burgdorf K, Chen X, Porowski A, Roberts T, Herrell J. Effectiveness of long-term residential substance abuse treatment for women: Findings from three national studies. American Journal of Drug and Alcohol Abuse. 2004;30(3):537–550. doi: 10.1081/ada-200032290. [DOI] [PubMed] [Google Scholar]
- Grella CE. Women in residential drug treatment: Differences by program type and pregnancy. Journal of Health Care for the Poor and Underserved. 1999;10(2):216–229. doi: 10.1353/hpu.2010.0174. [DOI] [PubMed] [Google Scholar]
- Grella CE, Greenwell L. Substance abuse treatment for women: Changes in settings where women received treatment and types of services provided, 1987-1998. Journal of Behavioral Health Services & Research. 2004;31(4):367–383. doi: 10.1007/BF02287690. [DOI] [PubMed] [Google Scholar]
- Grella CE, Joshi V, Hser YI. Program variation in treatment outcomes among women in residential drug treatment. Evaluation Review. 2000;24(4):364–383. doi: 10.1177/0193841X0002400402. [DOI] [PubMed] [Google Scholar]
- Grella CE, Polinsky ML, Hser YI, Perry SM. Characteristics of women-only and mixed-gender drug abuse treatment programs. Journal of Substance Abuse Treatment. 1999;17(1-2):37–44. doi: 10.1016/s0740-5472(98)00045-2. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Asche SE. Adolescent treatment for substance use disorders: Outcomes and outcome predictors. Journal of Child & Adolescent Substance Abuse. 2001;11(2):1–18. [Google Scholar]
- Howell EM, Chasnoff IJ. Perinatal substance abuse treatment. Findings from focus groups with clients and providers. Journal of Substance Abuse Treatment. 1999;17(1-2):139–148. doi: 10.1016/s0740-5472(98)00069-5. [DOI] [PubMed] [Google Scholar]
- Howell EM, Heiser N, Harrington M. A review of recent findings on substance abuse treatment for pregnant women. Journal of Substance Abuse Treatment. 1999;16(3):195–219. doi: 10.1016/s0740-5472(98)00032-4. [DOI] [PubMed] [Google Scholar]
- Hser YI, Anglin MD, McGlothlin W. Sex differences in addict careers. 1. Initiation of use. American Journal of Drug and Alcohol Abuse. 1987;13(1-2):33–57. doi: 10.3109/00952998709001499. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E. Cross-system data linkage for treatment outcome evaluation: Lessons learned from the California Treatment Outcome Project. Evaluation and Program Planning. 2008;31:125–135. doi: 10.1016/j.evalprogplan.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Huang D, Teruya C, Anglin MD. Gender comparisons of drug abuse treatment outcomes and predictors. Drug and Alcohol Dependence. 2003;72(3):255–264. doi: 10.1016/j.drugalcdep.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Hser YI, Niv N. Pregnant women in women-only and mixed-gender substance abuse treatment programs: A comparison of client characteristics and program services. Journal of Behavioral Health Services & Research. 2006;33(4):431–442. doi: 10.1007/s11414-006-9019-1. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Choo RE. Drug abuse's smallest victims: In utero drug exposure. Forensic Science International. 2002;128(1-2):20–30. doi: 10.1016/s0379-0738(02)00160-3. [DOI] [PubMed] [Google Scholar]
- Hughes PH, Coletti SD, Neri RL, Urmann CF. Retaining cocaine-abusing women in a therapeutic community: The effect of a child live-in program. American Journal of Public Health. 1995;85(8, Pt 1):1149–1152. doi: 10.2105/ajph.85.8_pt_1.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Zhang L, French MT, Witbrodt J. Women's programs versus mixed-gender day treatment: Results from a randomized study. Addiction. 2005;100(1):60–69. doi: 10.1111/j.1360-0443.2005.00914.x. [DOI] [PubMed] [Google Scholar]
- Kissin WB, Svikis DS, Moylan P, Haug NA, Stitzer ML. Identifying pregnant women at risk for early attrition from substance abuse treatment. Journal of Substance Abuse Treatment. 2004;27(1):31–38. doi: 10.1016/j.jsat.2004.03.007. [DOI] [PubMed] [Google Scholar]
- McCarty D, McGuire TG, Harwood HJ, Field T. Using state information systems for drug abuse services research. American Behavioral Scientist. 1998;41:1090–106. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Messina N, Burdon W, Hagopian G, Prendergast M. Predictors of prison TC treatment outcomes: A comparison of men and women participants. American Journal of Drug and Alcohol Abuse. 2006;32(1):7–28. doi: 10.1080/00952990500328463. [DOI] [PubMed] [Google Scholar]
- Messina N, Burdon W, Prendergast M. Assessing the needs of women in institutional therapeutic communities. Journal of Offender Rehabilitation. 2003;37(2):89–106. [Google Scholar]
- Messina N, Burdon W, Prendergast M. Prison-based treatment for drug-dependent women offenders: Treatment versus no treatment. Journal of Psychoactive Drugs. 2006;3:333–343. doi: 10.1080/02791072.2006.10400597. [DOI] [PubMed] [Google Scholar]
- Messina N, Chand N. Exemplary programs for women offenders with co-occurring disorders: Key recommendations for implementation and replication. 2009. White paper prepared for the Co-Occurring Joint Action Council (COJAC), the Department of Alcohol and Drug Programs (ADP), and Department of Mental Health (DMH). Retrieved from http://www.aodpolicy.org/COD.htm. [Google Scholar]
- Messina N, Grella C. Childhood trauma and women's health: A California prison population. American Journal of Public Health. 2006;96(10):1842–1848. doi: 10.2105/AJPH.2005.082016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Grella C, Cartier J, Torres S. A randomized experimental study of gender responsive substance abuse treatment for women in prison. Journal of Substance Abuse Treatment. 2010;38(2):97–107. doi: 10.1016/j.jsat.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Wish E, Nemes S. Predictors of treatment outcomes in men and women admitted to a therapeutic community. The American Journal of Drug and Alcohol Abuse. 2000;26(2):207–228. doi: 10.1081/ada-100100601. PMID: 10852357. [DOI] [PubMed] [Google Scholar]
- Niv N, Hser YI. Women-only and mixed-gender drug abuse treatment programs: Service needs, utilization and outcomes. Drug and Alcohol Dependence. 2007;16(87):194–201. doi: 10.1016/j.drugalcdep.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Orwin R, Francisco L, Bernichon T. Effectiveness of women's substance abuse treatment programs: A meta-analysis. National Evaluation Data Services. Center for Substance Abuse Treatment; 2001. [Google Scholar]
- Owen B. “In the mix”: Struggle and survival in a women's prison. State University Press of New York; Albany: 1998. [Google Scholar]
- Prendergast M, Messina N, Hall N. The relative effectiveness of women-only vs. mixed-gender substance abuse treatment. doi: 10.1016/j.jsat.2010.12.001. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in the observational studies for causal effects. Biometricka. 1983;70:41–55. [Google Scholar]
- Rubin DB. Estimating causal effects from large data sets using propensity scores. Annals of Internal Medicine. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Rubin DB, Thomas N. Matching using estimated propensity scores: Relating theory to practice. Biometrics. 1996;52:249–264. [PubMed] [Google Scholar]
- Saunders RC, Heflinger CA. Integrating data from multiple public sources: Opportunities and challenges for evaluators. Evaluation: International Journal of Theory, Research, and Practice. 2004;10:349–65. [Google Scholar]
- Staton M, Leukefeld C, Webster JM. Substance use, health, and mental health: Problems and service utilization among incarcerated women. International Journal of Offender Therapy and Comparative Criminology. 2003;47(2):224–239. doi: 10.1177/0306624X03251120. [DOI] [PubMed] [Google Scholar]
- Wagner CL, Katikaneni LD, Cox TH, Ryan RM. The impact of prenatal drug exposure on the neonate. Obstetrics & Gynecology Clinics of North America. 1998;25(1):169–194. doi: 10.1016/s0889-8545(05)70364-8. [DOI] [PubMed] [Google Scholar]
- Ye Y, Kaskutas LA. Using propensity scores to adjust for bias when assessing the effectiveness of alcoholics anonymous in observational studies. Drug and Alcohol Dependence. 2008;104:56–64. doi: 10.1016/j.drugalcdep.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]