Abstract
The nonsteroidal antiinflammatory drug (NSAID) sulindac and the ornithine decarboxylase (ODC) antagonist difluoromethylornithine (DFMO), individually and together, are effective inhibitors of colon carcinogenesis. However, chronic use of sulindac is associated with significant side effects. We evaluated the chemopreventive efficacy of phospho-sulindac (P-S, OXT-328), an apparently safe derivative of sulindac, together with DFMO, in HT-29 human colon cancer xenografts. Nude mice were divided into 4 groups: group 1 received vehicle (corn oil); group 2 received P-S (100 mg/kg/d) by oral gavage; group 3 received DFMO (2% in drinking water); and group 4 received P-S (100 mg/kg/d) by gavage plus DFMO (2% in drinking water) (P-S/DFMO). Eighteen days after implantation, compared to controls, tumor volume was inhibited 65.9% by P-S, 52.9% by DFMO and 70.9% by P-S/DFMO (p<0.01 for all). P-S/DFMO reduced cell proliferation 27.1% and increased apoptosis 38.9% compared to controls (p<0.05 for both). Compared to controls, P-S reduced the levels of thioredoxin-1 (Trx-1) and thioredoxin reductase (TrxR), whereas DFMO reduced polyamine content (putrescine and spermidine) and TrxR levels. Importantly, P-S/DFMO decreased putrescine and spermidine levels and the expression of Trx-1, TrxR, and cyclooxygenase (COX)-2. Of these molecular targets, TrxR most consistently correlated with tumor growth. Study results show that P-S/DFMO is an efficacious drug combination for colon cancer prevention, and also demonstrate the safety of P-S, which may overcome the limiting side effects of conventional sulindac. P-S/DFMO has an intricate mechanism of action extending beyond polyamines and including the thioredoxin system, an emerging regulator of chemoprevention. P-S/DFMO merits further evaluation.
Keywords: Phospho-sulindac, DFMO, colon cancer prevention, polyamines, thioredoxin, thioredoxin reductase
INTRODUCTION
The last decade has witnessed increasing emphasis on cancer chemoprevention. Using pharmacological agents or natural substances, chemoprevention aims to lower the risk of developing new cancers or the recurrence of already treated cancers. Colon cancer is the third most prevalent cancer and the second leading cause of death in the U.S (1). The molecular pathogenesis of colon cancer is one of the best understood amongst human cancers, including clearly defined precancerous stages. Given the poor performance of currently available treatment options for advanced colon cancer, efforts to develop effective prevention strategies are important and urgent.
A major development in colon cancer chemoprevention emerged from the work by Meyskens et al., who reported on a phase 2 clinical trial showing that the combination of difluoromethylornithine (DFMO) and sulindac versus placebo reduced the recurrence of all adenomas by 69% and of advanced adenomas by 92% (2). This study is the culmination of more than two decades of work on the role of polyamines in cancer by several groups. Polyamines are polycationic aliphatic amines, including putrescine, spermidine, and spermine, and are indispensable for cell survival through their role in cell proliferation. Their level is increased when proliferation is induced by growth factors, carcinogens or oncogenes (3). Not surprisingly, polyamine biosynthesis is tightly regulated, with ornithine decarboxylase (ODC) being the pivotal enzyme. DFMO inhibits ODC, which catalyzes the rate-limiting step in polyamine synthesis, whereas sulindac stimulates polyamine acetylation and export; combining the two results in a profound reduction of polyamine levels in the colon, leading to suppressed growth of cancer cells (4; 5; 6; 7).
Like all NSAIDs, sulindac has significant toxicity, especially when used long-term. Its main side effects are gastrointestinal (20% of patients), central nervous system (10%), skin rash and pruritus (5%); and elevations of hepatic enzymes in plasma, which are often transient. To diminish sulindac's toxicity and enhance its efficacy, we synthesized phospho-sulindac (P-S; OXT-328; Fig. 1), which consists of sulindac chemically modified at the −COOH group, which is considered responsible for most of its gastrointestinal toxicity (8). We have recently reported that P-S is much safer than sulindac (9; 10) and that it displays greater efficacy against intestinal cancer in Apc/Min mice than sulindac (10).
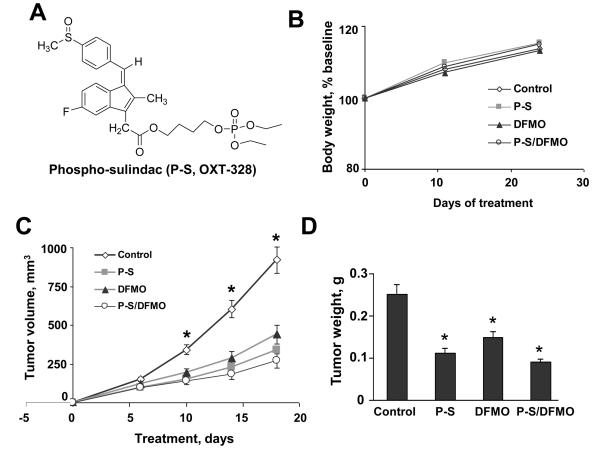
Figure 1. P-S alone and in combination with DFMO inhibits colon cancer growth in a xenograft model.
A- Chemical structure of phospho-sulindac (P-S; OXT-328). B-D- HT-29 cells (2 × 106) were injected subcutaneously into the right and left flank of nude mice. Drug administration was started one week prior to tumor injection. Animals were gavaged with 100 mg/kg P-S once a day for 18 days. DFMO 2% (w/v) was dissolved in water. B- Body weight progression over the course of the study for vehicle control (◇), P-S (■), DFMO (▲) and P-S/DFMO (○) treated mice. No significant differences in body weight were observed among the various groups. C- Tumor volume growth over time for vehicle control (◇), P-S (■), DFMO (▲) and P-S/DFMO (○) treated mice. *Significantly different from all the other groups (p<0.01, one way ANOVA test). #Significantly different compared to P-S/DFMO group (p<0.05, one way ANOVA test). D- Tumor mass of the dissected tumors. Mean tumor size in mice treated with P-S, DFMO and the combination of the two was smaller than that of vehicle. All values: mean±SEM, *p<0.05.
Our recent work has documented that, to a large extent, the anticancer effect of P-S and other similarly modified compounds is mediated through the thioredoxin system (11). Central to redox homeostasis in the cell, the thioredoxin system consists of Trx, whose main isoform is Trx-1; TrxR, which converts Trx to its (active) reduced state; and nicotinamide adenine dinucleotide phosphate (NADPH) (12; 13). Several signaling cascades relevant to cancer interact with or are dependent upon the thioredoxin system (14; 15).
Here, we evaluated the chemopreventive efficacy of P-S/DFMO in nude mice xenografted with HT-29 human colon cancer cells. Our results show that this combination inhibited the growth of HT-29 xenografts by over 70% through a significant cytokinetic effect likely mediated by changes in tumor polyamine levels and key signaling molecules, including members of the Trx system and COX-2. We conclude that P-S/DFMO has merit as a chemopreventive strategy against colon cancer and should be further evaluated.
MATERIALS AND METHODS
Reagents
P-S (OXT-328) was provided by Medicon Pharmaceuticals, Inc, Stony Brook, NY. DFMO was a gift from the National Cancer Institute (Bethesda, MD). Antibodies: Ki-67 antibody (Santa Cruz Biotechnology, Santa Cruz, CA), COX-2 antibody (Cayman Chemicals, Ann Arbor, MI), Trx-1 antibody (Abcam, Cambridge, MA) and phospho-NF-κB p65 (Ser276) antibody (Cell Signaling Technology, Beverly, MA), and TrxR (Sigma, St Louis, MO).
Animal study
Animals were kept under conditions of constant temperature (23±2 °C) and humidity (55±15%) with a 12 h light/dark cycle (lights on at 07:00 a.m.), and had free access to food (Purina Pico Mouse 5053) and water. Female NCr nude mice (5-6 weeks old) were purchased from Taconic, Hudson, NY. Animals were inoculated subcutaneously on their right and left flanks, each with 2.0×106 HT-29 colon cancer cells, which express COX-2 (16) in a volume of 100 μl in PBS. We followed a chemoprevention protocol: One week prior to cell implantation, 4 groups of animals (n=6/group) started receiving one of the following treatments: group 1 received vehicle (corn oil); group 2 received 100 mg/kg/d P-S by oral gavage; group 3 received 2% (w/v) DFMO in drinking water; and group 4 received 100 mg/kg/d P-S by gavage plus 2% (w/v) DFMO in drinking water. The dose of P-S was chosen based on published reports (17; 10). Tumors were measured twice a week with a digital microcaliper, and tumor volume was calculated as [length × width × (length + width/2) × 0.56]. Eighteen days after cell implantation, animals were sacrificed and their tumors were removed and weighed. Portions of each tumor were either preserved in formalin for analysis by immunohistochemistry or snap-frozen in liquid nitrogen for determination of polyamine levels. The animal study was approved by our Institutional Animal Care and Use Committee.
Determination of polyamines by HPLC
Xenograft tissues were homogenized in PBS containing 0.1 mM EDTA and 1 mM 1, 4-dithiothreitol. After sonication and centrifugation for 10 min at 12,000 rpm, samples were deproteinized using 10% (v/v) perchloric acid, and the acid-soluble polyamines, analyzed by reverse phase, ion-paired HPLC as described (18), were normalized to protein content. HPLC was performed with a Waters Alliance system, using a Thermo Hypersil BDSC18 column (150×4.6 mm, particle size 3 μm). Mobile phase A: 0.02 M 1-heptanesulphonic acid (pH=3.4); CH3CN;CH3OH = 5:3:3. Mobile phase B: CH3CN;CH3OH = 3:2. Authentic polyamines were used as standards.
Immunohistochemistry
Immunohistochemical staining for Ki-67, COX-2, Trx-1, TrxR, and phospho-NF-κB (activated form of NF-κB) was performed on the samples as previously described (19).
Determination of apoptosis
Apoptosis was determined immunohistochemically by the terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate-biotin nick end-labeling (TUNEL) assay (20) The in formalin-fixed tissues using the In Situ Cell Death Detection Kit, POD (Roche) per manufacturer's instructions. Positive control: treatment of samples with DNAse I.
Scoring
At least 10 fields per sample (at magnification × 200) were scored independently by one investigator blinded to the identity of the samples. Cells with a blue nucleus were considered unlabeled, while those with a brown nucleus were considered labeled. We calculated the percentage of proliferating and apoptotic cells by dividing the number of labeled cells by the number of cells in each field and multiplying by 100.
Statistical Analyses
Data were summarized using descriptive statistics and graphical displays. Tumor volumes were compared among the treatment groups using repeated-measures ANOVA. In these models, treatment was included as a between-subjects factor, while time was entered as a within-subjects factor. The interaction between group and time was interpreted using appropriate post-hoc tests and graphical displays. In the above model, baseline was excluded due to zero variance among all groups. Potential associations between parameters of interest (e.g., COX-2, Trx-1, tumor volume) were assessed using correlation analysis. Given the limited sample size, Spearman correlations were used. All tests were considered significant at the α<0.05 threshold and were analyzed using SAS, version 9.1.
RESULTS
The effect of P-S, DFMO and P-S/DFMO on the growth of HT-29 human colon cancer xenografts
We assessed whether P-S, DFMO or P-S/DFMO inhibit the growth of HT-29 human colon cancer xenografts in athymic nude mice. P-S and DFMO given alone significantly inhibited the growth of the HT-29 tumors. When compared to controls, the inhibitory effect of the drugs became statistically significant starting 6 days after cell implantation for the P-S and P-S/DFMO groups and 10 days after cell implantation for the DFMO treatment group. As shown in Fig 1C-D, 18 days after cells were implanted, the tumor volume of each study group was as follows: control = 953±148 mm3 (mean±SEM for this and all subsequent values), P-S = 324±60 mm3; DFMO = 448±72 mm3; and P-S/DFMO = 277±39 mm3. This indicates a reduction in tumor volume of 65.9%, 52.9% and 70.9% by P-S, DFMO and P-S/DFMO, respectively (p<0.01 for all). While P-S and DFMO inhibited tumor growth significantly compared to control, P-S/DFMO was more efficacious than either one alone, but the increased efficacy of the combination only trended toward statistical significance.
P-S, DFMO or P-S/DFMO produced no apparent adverse effects in mice during 25 days of administration. Throughout the study, the body weight of mice receiving P-S, DFMO, or P-S/DFMO was comparable to that of the control group (Fig. 1B). For example, on the day before sacrifice, the body weight of the four groups of mice was as follows: control = 23.6±2.6 g; P-S = 23.5±1.6 g; DFMO = 23.1±1.7 g; P-S/DFMO = 23.4±3.0 g.
The cytokinetic effect of P-S, DFMO and P-S/DFMO in human colon cancer xenografts
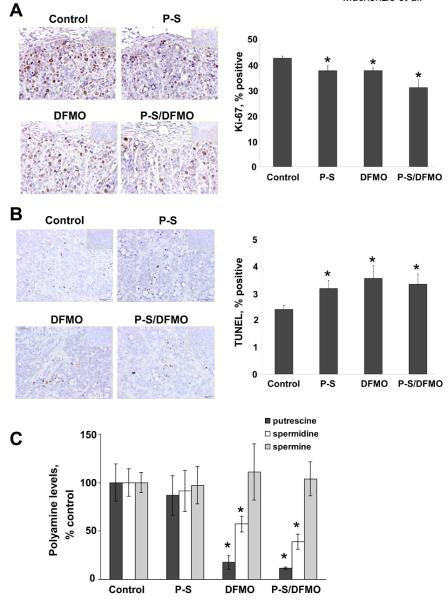
To elucidate the mechanism underlying the effect of P-S, DFMO and P-S/DFMO on tumor growth, we determined their effects on cell proliferation and apoptosis. Proliferation of the tumors treated with P-S/DFMO was reduced by 27.1% compared to controls; the percent of proliferating cells was 42.5±0.87 in controls vs. 31.0±3.09 in the combination-treated mice (p<0.01). P-S and DFMO alone decreased cell proliferation modestly but significantly compared to control mice (12% each, p<0.05; Fig. 2A). P-S, DFMO and P-S/DFMO also induced apoptosis; the apoptosis index was increased from 2.39±0.15 in controls to: 3.16±0.30 in the P-S group; 3.54±0.47 in the DFMO group; and 3.32±0.37 in the P-S/DFMO group (32.2%, 48.0% and 38.9%, respectively; p<0.05 for all). Of note, the induction of apoptosis by P-S/DFMO did not differ significantly from that by P-S or DFMO (Fig. 2B).
Figure 2. P-S/DFMO decreases proliferation, induces cell death by apoptosis, and reduces polyamine levels in human colon xenografts in mice.
Changes in proliferation and apoptosis indices in response to P-S, DFMO, or combination of both. Percentage of proliferation (A) and apoptotic cells (B) of xenograft tumors were determined as described in Materials and Methods. Left: Images of tissue sections from xenograft tumors treated with either vehicle (control), P-S, DFMO, or both and stained for Ki-67 expression (proliferation marker) or by the TUNEL method (apoptosis) as described in Materials and Methods. Negative controls are shown as insets at the top right corner of each image. Right: The number of Ki-67 and TUNEL-positive cells were counted and expressed as percentage of the total number of cells per field. *Significantly different from control group (p<0.05, one-way ANOVA test; IHC staining, ×20). C. P-S/DFMO reduces the level of polyamines in human colon xenografts in mice. Polyamine levels were measured by HPLC as described in Materials and Methods. Polyamine content in the tissue samples isolated from tumors treated with P-S, DFMO or both. Data are expressed as percentage of control. Values are shown as mean±SEM of 5 independent tumors. *Significantly different from control group (p<0.05, one way ANOVA test).
DFMO and P-S/DFMO reduce the level of putrescine and spermidine in human colon cancer xenografts
Increased polyamine levels, a common finding in colorectal cancers, have long been associated with colon carcinogenesis in both preclinical models and in humans (3). Thus, the levels of polyamines in tumor xenografts treated with P-S, DFMO or P-S/DFMO were evaluated by HPLC. As shown in Fig. 2C, only DFMO and P-S/DFMO significantly reduced putrescine and spermidine levels. Compared to controls, DFMO alone and P-S/DFMO decreased the levels of putrescine in tumor xenografts by 82.2% and 88.1% respectively (p<0.01 for both), and spermidine levels by 42.8% and 60.9% (p<0.03, for both), respectively. Spermine levels remained unchanged among the various groups.
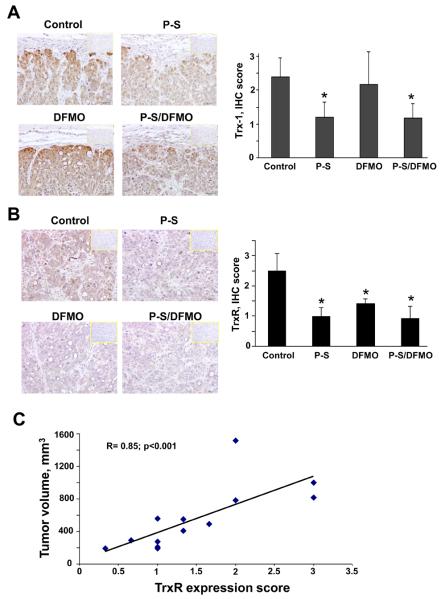
P-S, DFMO and P-S/DFMO decrease expression of Trx-1 and TrxR in human colon cancer xenografts
We have previously shown that the thioredoxin system could mediate redox-induced cell death in response to various anticancer agents, including P-S (21). TrxR is overexpressed in many cancers and together with Trx-1 is also associated with drug resistance (14). Using immunohistochemistry, we determined the levels of Trx-1 and TrxR in tumor xenografts treated with P-S, DFMO or P-S/DFMO.
Compared with controls, P-S/DFMO decreased the expression levels of Trx-1 in tumor xenografts by 50% (p<0.01). P-S alone also decreased Trx-1 levels by 50% (p<0.02), whereas DFMO had no such effect when compared to control (Fig. 3A). We also analyzed in detail the different expression patterns of Trx-1 by scoring the intensity of the Trx-1 positive staining for each individual sample. We observed that control samples predominantly had index scores of 2+ and 3+. In contrast, P-S or P-S/DFMO decreased Trx-1 expression to an intensity score of mainly 1+, whereas DFMO alone generated an intermediate response. These results indicate that P-S/DFMO, and in particular P-S, inhibit Trx-1 expression in HT-29 tumor xenografts. Compared to controls, P-S and DFMO, each alone, decreased TrxR levels in tumor xenografts by 60% and 40%, respectively (p<0.01). P-S/DFMO decreased TrxR levels by 63% (p<0.01; Fig. 3B).
Figure 3. P-S/DFMO decreases Trx-1 and TrxR expression levels in tumor xenografts in mice.
Tumor tissue sections were immunohistochemically stained with Trx-1 and TrxR. A. Representative images of Trx-1 for the various groups. The consecutive section was stained with isotype IgG as negative staining control. The number of Trx-1 positive cells was scored and ranked according to its intensity of each field. Trx-1 was expressed as IHC rank number of cells in the field. *Significantly different from control group (p<0.02, one-way ANOVA test; IHC staining, ×20). B. Tumor tissue sections were immunohistochemically stained with TrxR. Representative images of TrxR for the various groups. The consecutive section was stained with isotype IgG as negative staining control. The number of TrxR-positive cells was scored and ranked according to intensity of each field. TrxR was expressed as IHC rank number of cells in the field. *Significantly different from control group (p<0.01, one way ANOVA test; IHC staining, ×20). C. The association between tumor volume in HT-29 xenografts and TrxR expression score of all the study groups; R=0.85, p<0.01.
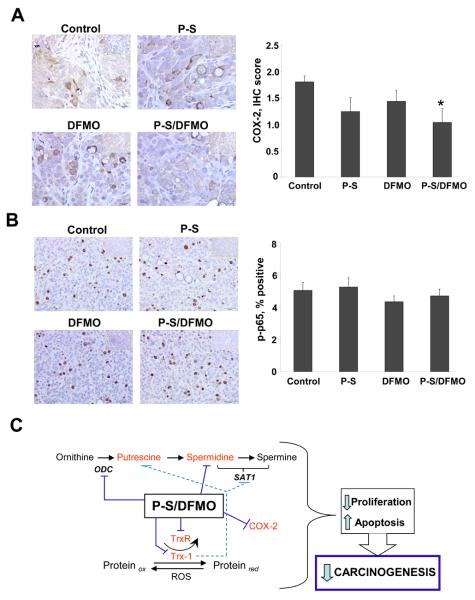
P-S/DFMO decreases the expression of COX-2 but not the activation of NF-κB in human colon cancer xenografts
Both COX-2 and NF-κB are redox-sensitive signaling molecules. There is extensive evidence that the progression of precancerous lesions is associated with the upregulation of COX-2 (22). In addition, NF-κB activation is frequently observed in colon cancer and is associated with resistance to chemotherapy (23). Thus, we investigated the expression of COX-2 and the activation of NF-κB in tumor xenografts from the four study groups. The latter was measured by determining Ser276 phosphorylation of the p65 subunit of NF-κB.
As shown in Fig. 4A, compared to controls, P-S/DFMO decreased the expression of COX-2 in tumor xenografts by 42.8% (p<0.03). P-S and DFMO, each alone, had a small but statistically not significant (p<0.07) effect on COX-2 levels (31% and 20% reduction, respectively). No significant differences in the degree of NF-κB activation between study groups were observed (Fig. 4B).
Figure 4. Effect of P-S and DFMO on COX-2 and NF-κB in human colon xenografts.
A- P-S/DFMO decreases COX-2 expression levels in tumor xenografts in mice. Tumor tissue sections were immunohistochemically stained with COX-2. Representative images of COX-2 for the various groups. The consecutive section was stained with isotype IgG as negative staining control. The number and intensity of COX-2 positive cells were scored and ranked according to intensity of each field. COX-2 was expressed as IHC rank number of cells in the field. *Significantly different from control group (p<0.03, one-way ANOVA test; IHC staining, ×20). B- P-S/DFMO does not inhibit NF-κB activation in tumor xenografts in mice. Tumor tissue sections were immunohistochemically stained with phospho-NF-κB p65 (Ser276) antibody. Representative images of phospho-p65 for the various groups. The number of phospho-p65 positive cells were counted and expressed as percentage of the total number of cells in the field. (IHC staining, ×20). C. Scheme illustrating the molecular effectors affected by P-S/DFMO combination (highlighted in red), that lead to an increase in apoptosis and decrease in cell proliferation, finally culminating with a decrease carcinogenesis.
Association between signaling events and xenograft growth in response to P-S, DFMO and P-S/DFMO
Our work revealed key molecular effectors of P-S, DFMO and P-S/DFMO. Table 1 summarizes their percent change in each treatment group compared to control, highlighting the principal differences between the two drugs and their combination. DFMO mainly decreased putrescine and spermidine levels, as expected; it also suppressed TrxR levels. P-S only affected the thioredoxin system, suppressing the expression of Trx-1 and TrxR. The combination of the two agents showed the same effects plus suppressed COX-2 expression and a more pronounced inhibition of tumor growth.
Table 1.
The effect of P-S, DFMO or P-S/DFMO on molecular targets in colon cancer: xenografts
| P-S | DFMO | P-S/DFMO | |
|---|---|---|---|
| Polyamines | |||
| putrescine | ↓ 13%, n.s. | ↓ 82%, p<0.01 | ↓ 88%, p<0.01 |
| spermidine | ↓ 8%, n.s. | ↓ 43%, p<0.03 | ↓ 61%, p<0.03 |
| spermine | ↓ 3%, n.s. | ↑ 10%, n.s. | ↑ 4%, n.s. |
| COX-2 | ↓ 31%, n.s. | ↓ 20%, n.s. | ↓ 42%, p<0.03 |
| NF-κB | ↑ 4%, n.s. | ↓ 14%, n.s. | ↓ 6%, n.s. |
| Trx-1 | ↓ 50%, p<0.02 | ↓ 8%, n.s. | ↓ 50%, p<0.01 |
| TrxR | ↓ 60%, p<0.01 | ↓ 40%, p<0.01 | ↓ 63%, p<0.01 |
| Tumor inhibition | 65.9%, p<0.01 | 52.9%, p<0.01 | 70.9%, p<0.01 |
All comparisons are to the control group, n.s.: not significant.
To evaluate the contribution of each molecular target to the antitumor effect, we performed correlation analyses (Table 2 and Supplemental figure 1). TrxR was the molecular target that best correlated with tumor volume data (Fig. 3C). Tumor volume values plotted against the respective TrxR levels showed a statistically significant positive association between them (R=0.850, p<0.001). This was also true, albeit to a lesser extent, for Trx-1 (R=0.499, p<0.03) and COX-2 levels (R=0.582, p<0.01). As expected, putrescine levels were positively associated with spermidine levels (R=0.836, p<0.001); both were associated with the cell proliferation marker Ki-67 (R=0.551, p<0.02 for putrescine; R=0.588, p<0.001 for spermidine), reflecting the known positive association between polyamines and cell proliferation.
Table 2.
Correlation of various molecular effectors with tumor volume and with each other
| TrxR | Trx-1 | Ki-67 | COX-2 | Putrescine | Spermidine | Spermine | NF-κB | |
|---|---|---|---|---|---|---|---|---|
| Tumor volume | 0.85,p<0.001 | 0.50, p<0.03 | 0.54, p<0.02 | 0.59, p<0.01 | n.s. | n.s. | n.s. | n.s. |
| TrxR | 0.66, p<0.01 | 0.72, p<0.01 | 0.63, p<0.02 | n.s. | n.s. | n.s. | n.s. | |
| Trx-1 | n.s. | 0.48, p<0.04 | n.s. | n.s. | n.s. | n.s. | ||
| Ki-67 | n.s. | 0.55, p<0.02 | 0.59, p<0.01 | n.s. | n.s. | |||
| COX-2 | n.s. | n.s. | n.s. | n.s. | ||||
| Putrescine | 0.84, p<0.001 | n.s. | n.s. | |||||
| Spermidine | n.s. | n.s. | ||||||
| Spermine | n.s. |
For each column, the first number represents the R value, n.s.: not significant.
DISCUSSION
This study demonstrates that the combination of P-S and DFMO significantly prevents human colon cancer in a xenograft model. This effect is associated with reduced levels of a) polyamines, key regulators of cell proliferation; b) Trx-1 and TrxR, the two protein members of the thioredoxin system; and c) COX-2, a protein considered important in colon tumorigenesis and a target of chemopreventive agents. These molecular effects likely culminate in substantial inhibition of proliferation and induction of apoptosis, the net effect of which was the 70.9% reduction in xenograft growth by P-S/DFMO (Fig. 4D).
Agent safety is critical to chemoprevention, which by definition entails long-term (decades) of agent administration to often healthy individuals at risk of cancer. Neither DFMO nor P-S, even when combined, showed signs of toxicity, particularly gastrointestinal toxicity, a major limitation of conventional sulindac. Indeed, safety concerns have prompted efforts to devise chemopreventive protocols using the lowest possible dose of sulindac that maintains adequate efficacy, including the co-administration of a gastroprotective drug (24). Our results are consistent with previous work indicating the preclinical efficacy of P-S (9; 10). For example, though 100% of mice receiving P-S (100 mg/kg/d) for 3 wks were alive and healthy, treatment with sulindac at an equimolar dose (66 mg/kg/d) resulted in 80% mortality (10).
The chemopreventive efficacy of P-S/DFMO was stronger than that of either compound alone, and even though these effects only trended toward statistical significance, such lack of significance is probably due to lack of power. Nonetheless, we deem this finding as highly relevant. Thus, although this enhanced efficacy did not represent true pharmacological synergy, it is consistent with the notion that these compounds modulate the polyamine biosynthetic pathway synergistically. The growth inhibitory effect by P-S, DFMO and P-S/DFMO was associated with significantly decreased cell proliferation and increased apoptosis. Of the two, the effect on apoptosis was somewhat more pronounced. The end result of these two effects was significant suppression of xenograft growth.
The cytokinetic effect of the test compounds reflects the summation of changes in several cell signaling pathways. Analysis of cell signaling in response to P-S, DFMO, and P-S/DFMO revealed that at least three important pathways are modulated significantly by these two agents: polyamines, the thioredoxin system, and the eicosanoid pathway. Perhaps surprisingly, NF-κB does not seem to be part of this chemopreventive effect.
A strong relationship between polyamines and cancer is known to exist. However, our results make it clear that the relationship between each of the three polyamines and tumor growth inhibition is complex. None of them individually is significantly associated with tumor volume, though putrescine and spermidine are associated with cell proliferation, in keeping with their well-known role in cell renewal (3; 25). Putrescine and spermidine (the immediate metabolic product of putrescine) are associated with each other, whereas spermine, whose levels did not change in any of the study groups, seems to be differentially regulated by P-S and/or DFMO.
The most consistent and statistically strongest association with tumor volume concerned the thioredoxin system, most notably TrxR and, to a lesser degree, Trx-1. These two proteins are pivotal in regulating redox chemistry in the cell. Trx-1 reduces client proteins oxidized by reactive oxygen species under conditions of oxidative stress, itself undergoing oxidation during this process. TrxR reverses this, returning Trx-1 to its active (reduced) status. Under our experimental conditions, the apparently dominant effect was the significant suppression of TrxR and Trx-1 by P-S/DFMO, presumably precipitating a state of massive oxidative stress that leads to the death of HT-29 cells. We have previously proposed such a mechanism of chemopreventive action for P-S and other chemopreventive agents (26; 11). Adding complexity, there is a possible direct interaction between the thioredoxin system and polyamines. In MCF-7 human breast cancer cells, transfected Trx-1 decreased the expression and enzyme activity of spermidine/spermine N1-acetyltransferase and also lowered putrescine levels without changing those of spermine or spermidine (27). Of interest, an inverse relationship (reduction of thioredoxin caused by polyamine depletion) has been reported in a different system (28).
COX-2 levels were significantly suppressed by P-S/DFMO, but not by either one alone. The difference in the degree of suppression, especially by P-S compared to P-S/DFMO, was not great (31% vs. 42%); in the case of P-S, however, its effect on COX-2 expression did not reach statistical significance. The relationship between the eicosanoid cascade and cancer prevention by P-S/DFMO is unclear. Contrary to expectations, Meyskens et al. noted no change in PGE2 levels in the colonic mucosa of patients treated with sulindac/DFMO (29). COX-2-independent effects in cancer prevention by NSAIDs have long been considered (30). Nevertheless, the suppressed levels of COX-2 and the presumed accompanying suppression of PGE2 levels may have contributed to their chemopreventive effect.
The lack of any significant effect on NF-κB by our test compounds is rather surprising, especially since NF-κB is redox-sensitive and modulated by the thioredoxin system (21). Multiple lines of evidence indicate that NF-κB is an important mediator of carcinogenesis; depending on biological context, it modulates proliferation and apoptosis (31). Anticancer drugs, including P-S, inhibit NF-κB activation as part of their pharmacological activity (11; 31). This finding underscores the complexity of cell signaling pathways and suggests that the final outcome represents the balance of many competing processes.
In conclusion, our study demonstrates that P-S combined with DFMO is a promising drug combination for colon cancer prevention. P-S/DFMO has an intricate mechanism of action that extends beyond polyamines, involving emerging regulators of chemoprevention such as the thioredoxin system. The (preclinical) safety of P-S may enable it to overcome safety concerns regarding the clinically successful combination of conventional sulindac with DFMO. Given P-S's efficacy and apparent safety as well as its effective combination with DFMO, P-S deserves further evaluation for its role in colon cancer prevention.
Supplementary Material
Acknowledgments
Financial Support
Grant support: NIH grants R01-CA139453, R01CA13945402 and 1N01CN43302WA22
LIST OF ABBREVIATIONS
- COX
cyclooxygenase
- DAB
3,3′-diaminobenzidine
- DFMO
difluoromethylornithine
- dUTP
2′-deoxyuridine, 5′-triphosphate
- NSAID
non-steroidal antiinflammatory drug
- NF-κB
nuclear factor κB
- ODC
ornithine decarboxylase
- PG
prostaglandin
- P-S
phospho-sulindac
- Trx-1
thioredoxin-1
- TrxR
thioredoxin reductase
Footnotes
Competing interests
The authors have nothing to disclose except for BR, who has an equity position in Medicon, Inc.
REFERENCES
- 1.American Cancer Society Statistics for 2009. 2009 [Google Scholar]
- 2.Meyskens FL, Jr., McLaren CE, Pelot D, et al. Difluoromethylornithine plus sulindac for the prevention of sporadic colorectal adenomas: a randomized placebo-controlled, double-blind trial. Cancer Prev Res (Phila Pa) 2008;1:32–38. doi: 10.1158/1940-6207.CAPR-08-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerner EW, Meyskens FL., Jr. Polyamines and cancer: old molecules, new understanding. Nat Rev Cancer. 2004;4:781–792. doi: 10.1038/nrc1454. [DOI] [PubMed] [Google Scholar]
- 4.Qu N, Ignatenko NA, Yamauchi P, et al. Inhibition of human ornithine decarboxylase activity by enantiomers of difluoromethylornithine. Biochem J. 2003;375:465–470. doi: 10.1042/BJ20030382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basuroy UK, Gerner EW. Emerging concepts in targeting the polyamine metabolic pathway in epithelial cancer chemoprevention and chemotherapy. J Biochem (Tokyo) 2006;139:27–33. doi: 10.1093/jb/mvj022. [DOI] [PubMed] [Google Scholar]
- 6.Gerner EW. Impact of dietary amino acids and polyamines on intestinal carcinogenesis and chemoprevention in mouse models. Biochem Soc Trans. 2007;35:322–325. doi: 10.1042/BST0350322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerner EW, Meyskens FL, Jr., Goldschmid S, et al. Rationale for, and design of, a clinical trial targeting polyamine metabolism for colon cancer chemoprevention. Amino Acids. 2007;33:189–195. doi: 10.1007/s00726-007-0515-2. [DOI] [PubMed] [Google Scholar]
- 8.Piazza GA, Keeton AB, Tinsley HN, et al. A novel sulindac derivative that does not inhibit cyclooxygenases but potently inhibits colon tumor cell growth and induces apoptosis with antitumor activity. Cancer Prev Res (Phila Pa) 2009;2:572–580. doi: 10.1158/1940-6207.CAPR-09-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang L, Mackenzie G, Ouyang N, et al. The novel phospho-non-steroidal anti-inflammatory drugs, OXT-328, MDC-22 and MDC-917, inhibit adjuvant-induced arthritis in rats. Br J Pharmacol. 2010 doi: 10.1111/j.1476-5381.2010.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mackenzie GG, Sun Y, Huang L, et al. Phospho-Sulindac (OXT-328), a Novel Sulindac Derivative, Is Safe and Effective in Colon Cancer Prevention in Mice. Gastroenterology. 2010;139:1320–1332. doi: 10.1053/j.gastro.2010.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun Y, Rigas B. The Thioredoxin System Mediates Redox-Induced Cell Death in Human Colon Cancer Cells: Implications for the Mechanism of Action of Anticancer Agents. Cancer Res. 2008;68:8269–8277. doi: 10.1158/0008-5472.CAN-08-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koharyova M, Kolarova M. Oxidative stress and thioredoxin system. Gen Physiol Biophys. 2008;27:71–84. [PubMed] [Google Scholar]
- 13.Arner ES. Focus on mammalian thioredoxin reductases--important selenoproteins with versatile functions. Biochim Biophys Acta. 2009;1790:495–526. doi: 10.1016/j.bbagen.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Mukherjee A, Martin SG. The thioredoxin system: a key target in tumour and endothelial cells. Br J Radiol. 2008;81:S57–68. doi: 10.1259/bjr/34180435. Spec No 1: [DOI] [PubMed] [Google Scholar]
- 15.Tonissen KF, Di Trapani G. Thioredoxin system inhibitors as mediators of apoptosis for cancer therapy. Mol Nutr Food Res. 2009;53:87–103. doi: 10.1002/mnfr.200700492. [DOI] [PubMed] [Google Scholar]
- 16.Williams JL, Nath N, Chen J, et al. Growth inhibition of human colon cancer cells by nitric oxide (NO)-donating aspirin is associated with cyclooxygenase-2 induction and beta-catenin/T-cell factor signaling, nuclear factor-kappaB, and NO synthase 2 inhibition: implications for chemoprevention. Cancer Res. 2003;63:7613–7618. [PubMed] [Google Scholar]
- 17.Wahlfors T, Hakkarainen T, Janne J, et al. In vivo enhancement of herpes simplex virus thymidine kinase/ganciclovir cancer gene therapy with polyamine biosynthesis inhibition. Int J Cancer. 2006;118:2907–2910. doi: 10.1002/ijc.21722. [DOI] [PubMed] [Google Scholar]
- 18.Aboul-Enein HY, al-Duraibi IA. Separation of several free polyamines and their acetylated derivatives by ion-pair reversed-phase high performance liquid chromatography. Biomed Chromatogr. 1998;12:291–293. doi: 10.1002/(SICI)1099-0801(199809/10)12:5<291::AID-BMC749>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 19.Ouyang N, Williams JL, Rigas B. NO-donating aspirin isomers downregulate peroxisome proliferator-activated receptor (PPAR){delta} expression in APCmin/+ mice proportionally to their tumor inhibitory effect: Implications for the role of PPAR{delta} in carcinogenesis. Carcinogenesis. 2006;27:232–239. doi: 10.1093/carcin/bgi221. [DOI] [PubMed] [Google Scholar]
- 20.Rigas B, Kozoni V. The novel phenylester anticancer compounds: Study of a derivative of aspirin (phoshoaspirin) Int J Oncol. 2008;32:97–100. [PubMed] [Google Scholar]
- 21.Sun Y, Rigas B. The thioredoxin system mediates redox-induced cell death in human colon cancer cells: implications for the mechanism of action of anticancer agents. Cancer Res. 2008;68:8269–8277. doi: 10.1158/0008-5472.CAN-08-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guruswamy S, Rao CV. Multi-Target Approaches in Colon Cancer Chemoprevention Based on Systems Biology of Tumor Cell-Signaling. Gene Regul Syst Bio. 2008;2:163–176. doi: 10.4137/grsb.s486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grivennikov SI, Karin M. Dangerous liaisons: STAT3 and NF-kappaB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 21:11–19. doi: 10.1016/j.cytogfr.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hayashi T, Ishiwatari H, Ihara H, et al. Suppressive effect of sulindac on branch duct-intraductal papillary mucinous neoplasms. J Gastroenterol. 2009;44:964–975. doi: 10.1007/s00535-009-0089-8. [DOI] [PubMed] [Google Scholar]
- 25.Gerner EW, Ignatenko NA, Lance P, et al. A comprehensive strategy to combat colon cancer targeting the adenomatous polyposis coli tumor suppressor gene. Ann N Y Acad Sci. 2005;1059:97–105. doi: 10.1196/annals.1339.033. [DOI] [PubMed] [Google Scholar]
- 26.Rigas B, Sun Y. Induction of oxidative stress as a mechanism of action of chemopreventive agents against cancer. Br J Cancer. 2008;98:1157–1160. doi: 10.1038/sj.bjc.6604225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Husbeck B, Stringer DE, Gerner EW, et al. Increased thioredoxin-1 inhibits SSAT expression in MCF-7 human breast cancer cells. Biochem Biophys Res Commun. 2003;306:469–475. doi: 10.1016/s0006-291x(03)00993-8. [DOI] [PubMed] [Google Scholar]
- 28.Moon MS, Kim JS, Kim TL, et al. Polyamine depletion partially reduces the radiation-induced cell death via cell cycle delay mediated by thioredoxin. Cell Biol Toxicol. 2006;22:137–147. doi: 10.1007/s10565-006-0042-z. [DOI] [PubMed] [Google Scholar]
- 29.Thompson PA, Wertheim BC, Zell JA, et al. Levels of rectal mucosal polyamines and prostaglandin E2 predict ability of DFMO and sulindac to prevent colorectal adenoma. Gastroenterology. 2010;139:797–805. doi: 10.1053/j.gastro.2010.06.005. 805 e791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shiff SJ, Rigas B. The role of cyclooxygenase inhibition in the antineoplastic effects of nonsteroidal antiinflammatory drugs (NSAIDs) [comment] J Exp Med. 1999;190:445–450. doi: 10.1084/jem.190.4.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sakamoto K, Maeda S. Targeting NF-kappaB for colorectal cancer. Expert Opin Ther Targets. 2010;14:593–601. doi: 10.1517/14728221003769903. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.