Abstract
Objective To describe baseline characteristics of participants in a pediatric obesity intervention tailored specifically to rural families delivered via telemedicine. Methods Randomized-control trial comparing a family-based behavioral intervention to a usual care condition. Participants Fifty-eight first through fifth graders and their parents from the rural Midwest. Measures Demographic, body mass index (BMI), Actigraph activity monitor information, 24-h dietary recalls, Child Behavior Checklist, Behavioral Pediatrics Feeding Assessment Scale. Results Child mean BMI was in the 94th percentile for weight. Average daily dietary intake exceeded 2,000 kcal and children consumed over eight servings of high-calorie, low-nutrient-dense foods. Children are engaged in approximately 65 min of moderate, 12 min of vigorous and over 300 min of sedentary physical activity daily. Conclusions Baseline data suggest children in rural areas may engage in adequate physical activity but eat many daily servings of energy-dense foods. Rural families may benefit from a comprehensive, rurally tailored obesity-related health behavior intervention.
Keywords: accelerometer, baseline, obesity, rural, telemedicine
Nearly one-third of the children between 2 and 19 years of age in the US are overweight or obese (Ogden, Carroll, & Curtin, 2010). Childhood obesity is linked to an increased risk of mortality (Neovius, Sundström, & Rasmussen, 2009) and other medical comorbidities such as cardiovascular disease (Freedman et al., 2008; Baker, Olsen, & Sørensen 2007), musculoskeletal problems (Taylor et al., 2006; Krul, van der Wouden, Schellecis, van Suijlekom-Smit, & Koes, 2009), and impaired glucose tolerance (Sinha et al., 2002). Children who are obese have lower self-esteem, more negative self-perceptions of physical competence (Braet, Mervielde, & Vandereycken, 1997), and more behavioral and emotional difficulties than children who are not obese (Braet, Mervielde, & Vandereycken, 1997).
Children in rural areas are more likely to be overweight and obese than children who live in urban areas (Joens-Matre et al., 2008). For instance, between 4% (Montgomery-Reagan et al., 2009) and 25% (Lutfiyya, Lipsky, Wisdom-Behounek, & Inpanbutr-Martinkus, 2007) more rural children are obese compared to their city-dwelling peers. In addition, higher prevalence rates in rural areas are not explained by demographic factors such as ethnicity, gender, or grade level (Davis, Flickinger, et al., 2005). More data are needed to determine the reasons rural children are at higher risk for obesity, but different dietary and activity patterns likely contribute. For example, high numbers of overweight children have been found in predominantly rural states, and lower physical activity is hypothesized to be a contributing factor (Davis, Boles, et al., 2008). Residents in suburban areas are nearly twice as likely to meet physical activity requirements as rural residents (Cherry, Huggins, & Gilmore, 2007), and rural children are less likely than their suburban and urban counterparts to engage in adequate amounts of daily physical activity (Lutfiyya, Lipsky, Wisdom-Behounek, & Inpanbutr-Martinkus, 2007).
Interventions targeting obesity in rural children exist, but none have utilized telemedicine (interactive televideo) technology. Gombosi and colleagues (Gombosi, Olasin, & Bittle, 2007) instituted a comprehensive primary prevention program in rural Pennsylvania, which intervened at the school, family, community, industry, and restaurant levels. The prevention program, however, showed little impact on obesity rates over a 5-year period. Dennison and colleagues (Dennison, Yin, Kibbe, Burns, & Trowbridge, 2008) also developed a direct-contact intervention, which trained health care workers to manage overweight adolescents in rural primary care settings. Findings demonstrated the feasibility of training health care workers to appropriately and comprehensively assess adolescents for obesity risk factors. Janicke and colleagues (Janicke et al., 2008) facilitated Project STORY, a randomized clinical trial comparing parent-only and family-based interventions. Findings from Project STORY suggested potential feasibility and efficacy of rural pediatric obesity interventions, but did not explore the technological possibilities offered by telemedicine.
One of the greatest benefits of using telemedicine technology in rural settings is that it allows for specialized professionals in urban settings to provide interventions to all corners of the state. There have been some randomized controlled trials using telemedicine to treat obesity in adults (Goulis et al., 2004; Frisch et al., 2009), and in both studies the intervention groups were fairly compliant and, relative to comparison groups, saw greater improvements in cardiovascular risk factors and weight loss. However, to date there are no telemedicine interventions (TM) specifically targeting rural pediatric obesity. The objective of this article is to report on the methodology and baseline characteristics of a randomized controlled trial comparing telemedicine to usual care (UC) for the treatment of pediatric obesity in rural children.
Methods
Rural schools were recruited for participation via flyers mailed out several times a year to all rural elementary schools in the state of Kansas, list serves for professional groups such as school nurses or telemedicine professionals, professional talks at local pediatric health-related conferences (i.e., Kansas Coordinated School Health), and word of mouth. Criteria for school participation included having rural designation (in a town or county with a population <20,000) and telemedicine capabilities (common in rural districts for distance learning). Interested schools were required to send in a letter from their principal or superintendent indicating their willingness to participate, and name a designated school representative who would be the liaison for the project. These representatives then received training in Human Subjects Research, Conflict of Interest, and HIPAA, as well as training on study-specific procedures. School representatives were most often school nurses, but also included a gym teacher, a principal, and a computer teacher.
The study was designed to target third–fifth grade children, but schools were allowed to invite any grades they felt were pertinent, sometimes including children as young as Kindergarten. Recruitment letters were sent home with children by school personnel to determine which families were interested in participation, and interested families signed consent forms and completed baseline measures. Inclusion criteria were living in rural Kansas and attending elementary school, being overweight/obese for age/gender, and parent ability to speak English. Exclusion criteria included having a developmental disability that would prevent the child from participating in the group format, or being immobile which would prevent them from increasing exercise. Parents and children who chose to participate gave informed consent and assented, respectively. Children who met these criteria and whose parents completed baseline measures were enrolled in the study and randomly assigned (via a random numbers table) to the TM or UC group.
TM
Children and families randomized to the intervention group participate in 8-weekly psychoeducational groups over telemedicine led by trained PhD level psychologists. Telemedicine is a technology similar to other interactive televideo modalities (i.e., Skype©) except that it is point-to-point such that data are transferred directly from one site to another and do not move through an off-site server, thus increasing patient confidentiality. From a provider perspective, telemedicine is very similar to face-to-face in that the provider can see and speak with the patient in real time.
Prior to the current study, a preexisting pediatric obesity intervention treatment manual (Healthy Hawks, available from Ann Davis at adavis6@kumc.edu) was tailored to better meet the needs of rural families. As described elsewhere (Davis, James, Curtis, Felts, & Daley, 2008) 21 rural parents of overweight or obese third through fifth grade elementary school children participated in focus groups designed to learn about the specific barriers they face regarding their child’s weight status. The results indicated that many of the barriers faced by rural parents were similar to those faced by urban parents, with the exception that rural parents also cited lack of weight loss resources in their community, lack of exercise facilities, and lack of low-calorie options in grocery stores. They also reported a need for more information on self-esteem and dressing for larger body sizes. Thus, the preexisting manual was adapted to specifically cover these additional topics as well as the existing topics based upon behavior modification, activity and sedentary activity and the stop-light-diet by Epstein & Squires (1988).
After the introduction and review of weekly goals and progress, children participated as a group in an age-appropriate lesson with the school representative on site using a standardized treatment manual, while parents separately but simultaneously met as a group with the psychologist over telemedicine using a similar, standardized treatment manual. Parents and children covered the same topics, and were reunited at the end of the meeting for goal setting. After 8-weekly sessions were completed, groups meet monthly for additional 6 months. Sessions during the summer break occurred individually over the phone. All group meetings lasted approximately 1 hr.
Control Group
Children and families randomized to the control group agreed to meet with their primary care physician to discuss a standardized list of topics. If they did not have a primary care physician, we agreed to provide one for them, but this was not necessary throughout the study. Prior to the visit, research staff sent a list of topics to both the family and the physician’s office requesting that the physician discuss the topics with the family during the visit, sign the form, and return it to the research staff in a postage-paid envelope. Topics that were covered included the causes of obesity and the relationship between diet, exercise, and body mass index (BMI); the importance of eating a balanced diet; current exercise recommendations for children; and current sedentary behavior recommendations for children.
Measures
Demographic Form
At baseline, the target child’s birth date, gender, grade level, and ethnicity were gathered. Information pertaining to maternal and paternal age, height and weight, marital status, education, occupation, and income level were also collected, as was information pertaining to siblings of the target child (e.g., age, height, weight, grade level, health concerns).
BMI z-score
Height and weight were assessed by school nurses via a Harpenden Holtain stadiometer, Model 603 (Holtain, Crymych, UK) and a portable SECA digital scale (SECA, Hamburg, Germany). Height and weight were always taken in triplicate and used to calculate BMI z-scores for children based on the Center for Disease Control’s growth charts (CDC, 2010a).
Twenty-Four Hour Diet Recall
The Twenty-four hour diet recall (24 hr FR) is a standardized three-pass method, developed by the US Department of Agriculture for use in national dietary surveillance. This measure has been shown to be a valid and reliable representation of a child’s overall diet (Crawford, Obarzanek, Morrison, & Sabry, 1994). Dietary recall data were gathered by master’s- and PhD-level researchers trained in diet, recall data gathering by a master’s-level registered dietician. All data were analyzed by master’s-level registered dieticians. Daily intake of calories, percent fat from calories, fruit and vegetable servings, and sweetened beverages were assessed. Red foods were also assessed. Epstein & Squires (1988) defined red foods as having 12 or more grams of sugar or 7 or more grams of fat, and are a target of the stop-light-diet, the primary educational curriculum regarding dietary changes for the current intervention.
Activity Monitors
The ActiGraph (Actigraph LLC, Pensacola, FL) is a small, light weight device worn on an adjustable belt over the nondominant hip that measures physical activity duration and intensity. The ActiGraph has been shown to provide valid assessments of physical activity for adults and children during daily living activities (Sirard, Melanson, & Freedson, 2000). Participants were asked to wear the activity monitor for at least 10 hr a day for a minimum of 4 days during a 1-week period. We assessed activity counts per minute, minutes spent in moderate and vigorous physical activity, and number of bouts of moderate and physical activity (for specific cut-offs, see Troiano et al., 2008).
Child Behavior Checklist
The child behavior checklist (CBCL) is a standardized measure that assesses parental report of child competencies and behavioral or emotional problems. Total scores for internalizing behaviors, externalizing behaviors, and total problem behavior ratings were assessed (Achenbach, 1991).
Behavioral Pediatrics Feeding Assessment Scale
The Behavioral Pediatrics Feeding Assessment Scale (BPFAS) is composed of 35 items: 25 describe the child’s feeding behavior and 10 describe parent’s feelings about or strategies for dealing with eating problems (Babbit et al., 1994). Parents are also asked to rate on a scale from 1 to 5 for how much they agree or disagree with each statement (a frequency score, possible scores range from 35 to 175), as well as whether or not each of the 35 items is a problem (a problem score, possible scores range from 0 to 35). Thus, the measure results in a child frequency score, a child problem score, a parent frequency score, and a parent problem score. Higher scores are suggestive of more problematic feeding behaviors. Previous research has shown the BPFAS to be a valid and reliable representation of a child’s and parent’s mealtime behavior (Crist et al., 1994).
Results
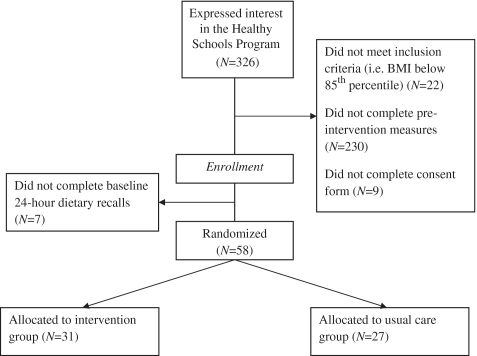
Figure 1 depicts the CONSORT Diagram for the current study. Three hundred and twenty-six families initially expressed interest in the project. However, 230 did not complete baseline measures, 9 did not properly complete the consent form, 7 did not complete the diet recall and 22 were not overweight or obese, resulting in a final sample of 58 child and parent dyads. Of these, 31 were randomly assigned to the TM group and 27 were randomly assigned to the UC group (N = 58); there were no significant between-group differences at baseline. Children ranged in age from 5 to 11 years (M = 8.55, SD = 1.74). Fifty-two children were White (89.7%), three were Native American (5.2%), and three (5.2%) did not indicate their ethnicity. Approximately one-third (31%) of the children were eligible for free or reduced-priced lunch.
Figure 1.
CONSORT Table.
Children’s baseline BMI percentiles for weight ranged from 85 to >99% (M = 94.17%, SD = 4.27) with BMI z-scores ranging from 1.05 to 2.78 (M = 1.76, SD = 0.48; see Table I). Dietary recall data indicated children consumed between 1,066 and 3,784 kcal per day (M = 2,049.92, SD = 541.07), and between 24% and 51% (M = 35.28, SD = 4.8%) of calories were from fat. They ate between 0 and 7 fruit servings (M = 1.61, SD = 1.48) and 0.5–5 vegetable servings (M = 2.23, SD = 1.09) per day. Children consumed zero to nearly five sugar-sweetened beverages (M = 0.97, SD = 1.01) and zero to over four servings of “junk food” (M = 1.18, SD = 0.96) per day. They consumed between 4 and 13 daily servings (M = 7.48, SD = 1.96) of high-fat and high-sugar “red” foods.
Table I.
Sample Characteristics and Baseline Values for Outcome Measures
| Category | Measure | Baseline valuea |
|---|---|---|
| Body mass index | BMI percentile for weight | 94.17 ± 4.27 |
| BMI z-score | 1.76 ± 0.48 | |
| Dietary intake/dayb | kcal | 2049.92 ± 541.07 |
| Percent of kilocalory from fat | 35.28 ± 4.8 | |
| Fruit servings | 1.61 ± 1.48 | |
| Vegetable servings | 2.23 ± 1.09 | |
| Junk food servings | 1.18 ± 0.96 | |
| Sweetened drinks | 0.97 ± 1.01 | |
| “Red” foods | 7.48 ± 1.96 | |
| Physical activity/day | Sedentary (min) | 304.56 ± 94.93 |
| Light PA (min) | 337.38 ± 80.64 | |
| Moderate PA (min) | 64.74 ± 34.35 | |
| Vigorous PA (min) | 12.17 ± 10.36 | |
| Behavior | CBCL internalizing | 52.24 ± 10.04 |
| CBCL externalizing | 52.43 ± 8.43 | |
| CBCL total problems score | 52.65 ± 9.47 | |
| BPFAS frequency, child score | 39.32 ± 8.2 | |
| BPFAS frequency, adult score | 14.85 ± 3.94 | |
| BPFAS problem, child score | 2.55 ± 2.9 | |
| BPFAS problem, adult score | 0.83 ± 1.28 |
aAll values presented as means plus/minus standard deviations.
bRed foods refer to food items with more than 7 g of fat or 12 g of sugar per serving.
PA = physical activity, CBCL = Child Behavior Checklist, BPFAS = Behavioral Pediatrics Feeding Assessment Scale.
At baseline, children engaged in between 15 and 141 min (M = 64.74, SD = 34.35) of moderate physical activity and 0.5–38 min (M = 12.17, SD = 10.36) of vigorous physical activity per day. They were sedentary for 107–561 daytime min (M = 304.56, SD = 94.93), and engaged in light physical activity, which included any sort of movement, for 156–494 min (M = 337.38, SD = 80.64) per day. Children’s baseline CBCL internalizing scores ranged from 33 to 74 (M = 52.24, SD = 10.045) and externalizing scores ranged from 40 to 73 (M = 52.43, SD = 8.743). Total scores ranged from 32 to 72 (M = 52.65, SD = 9.47). Children’s baseline BPFAS frequency scores ranged from 25 to 55 (M = 39.32, SD = 8.2) while parent frequency scores ranged from 10 to 24 (M = 14.85, SD = 3.94). Parents reported that between 0 and 9 of their child’s feeding behaviors were problematic (M = 2.55, SD = 2.9) and reported between 0 and 6 (M = 0.83, SD = 1.28) parent problems with feeding their children.
Discussion
Children living in rural areas are at particular risk of being obese (Joens-Matre et al., 2008). The objective of the current study was to describe the design and baseline characteristics of a randomized-controlled trial designed to treat pediatric obesity in rural children. Results indicate child mean baseline BMI percentile for weight was 94% with a mean BMI z of 1.76, which is slightly lower than previous studies, which showed baseline mean BMI z between 2.015 and 2.25 (Dennison, Yin, Kibbe, Burns, & Trowbridge, 2008; Janicke et al., 2008).
Dietary Consumption
Children’s calorie and fat intake were at the upper end or in excess of the nutrition recommendations for children (American Heart Association, 2010) and they consumed several servings of high-calorie, high-sugar foods daily. Rural children have been shown to receive up to one-third of the daily energy intake from low-nutrient-dense (i.e., high fat and high sugar) foods and beverages (Stroehla, Malcoe, & Velie, 2005), suggesting dietary intake of the present sample is on par with that of other rural children.
Children consumed approximately three daily servings of produce, considerably less than the recommended 5–9 daily servings yet on par with the average daily consumption among American children (Lorson, Melgar-Quinonez, & Taylor, 2009). In addition, at baseline it appears that calorie intake from sweetened beverages is similar to that of other rural children (Stroehla, Malcoe, & Velie, 2005).
The present findings suggest that rural children who are obese are eating too many energy-dense foods with little nutritional value. These findings are supported by prior research comparing dietary intake in rural and urban children, which demonstrated that rural children tended to eat more junk food or “red” foods than their urban counterparts (Davis, James, et al., 2008). Had the sample been an urban population, these findings might be attributed to the dearth of supermarkets and fresh produce in cities, especially low-income areas. Supermarkets tend to be even further away in rural areas than urban (Michimi & Wimberly, 2010). However, while proximity to supermarkets has been shown to be predictive of obesity among urban residents, it shows no effect on obesity among rural residents (Ford & Dzewaltowski, 2010; Michimi & Wimberly, 2010).
Rural children who are obese have been shown to have dietary intakes and habits that are similar to their urban and suburban counterparts (Cherry, Huggins, & Gilmore, 2007). However, some research has suggested that rural families may in fact consume fewer fruits and vegetables than urban and suburban families (Champagne, Bogle, & Karge, 2002). In addition, despite the lack of disparity in obesity risk factors (i.e., cholesterol, physical activity) between urban and rural children, rural children may be over 50% more likely to develop obesity (McMurray, Harrell, Bangdiwala, & Deng, 1999). More comprehensive data are needed to better understand rural obese children’s dietary intake and its role in obesity and related risk factors.
Physical Activity
Children engaged in approximately 65 min of moderate physical activity per day, which met Center for Disease Control and Prevention (CDC, 2010b) guideline of 60 min. However, the wide range of time children spent engaging in moderate physical activity (15–141 min) suggests that a notable proportion of rural children—approximately half the sample—were not sufficiently active. The relatively low amount of vigorous physical activity could be accounted for by the difficulty associated with exercise among children who are obese: intense exercise feels more painful or difficult for those who are obese than for those who are not obese (Sothern, 2001). It is possible that if vigorous or other activity had also been measured using a heart rate monitor, it would have shown that children spent more time than it appears in a heart rate zone comparable to vigorous exercise. If activity monitors were used that also measure heart rate, such a device would likely provide a more comprehensive measure of physical exertion. Lutfiyya and colleagues (2007) found that rural children were more likely than urban children to be inactive. There have been mixed findings suggesting that rural children are equally or more active than urban children, but rural children are consistently more likely to be obese (Joens-Martre et al., 2008; MacMurray, Harrell, Bangdiwala, & Deng, 1999). Therefore, it is unclear what role physical activity plays in rural childhood obesity but it appears that, despite an adequate amount of mean physical activity, energy intake and expenditure are out of balance.
The relatively high physical activity found in the present sample may have been influenced by measurement increasing socially desirable behavior. Although parents and children were not instructed to change their dietary or physical activity habits until after baseline measurement, it is possible that families were more motivated to be active when they knew it would be measured by researchers. Replication and continued follow-up may provide a complete picture of rural obese children’s physical activity patterns.
Behavior
According to CBCL scores, participating children appeared to be functioning reasonably well. Scores were slightly lower (better) compared to prior behavioral research with children who are obese and seeking clinical treatment (Braet, Mervielde, & Vandereycken, 1997). However, prior research with children who are obese and were recruited from the community (Braet, Mervielde, & Vandereycken, 1997) showed that total problems, internalizing and externalizing scores were nearly identical to the present sample’s scores.
Child and parent frequency of feeding behaviors and strategies, respectively, and rating of associated problems were very similar to the normative sample (see Crist et al., 1994). Positive mealtime experiences and parental encouragement of healthy feeding behaviors play an important role in helping children to regulate caloric intake and maintain a healthy weight (Birch & Fisher, 1998; Johnson & Birch, 1994). It bodes well for this rural sample that low baseline feeding scale ratings suggest families are experiencing few behavioral issues or “battles” during mealtimes. However, it is also possible that parents’ own feeding behaviors are problematic and perception of their children’s feeding is similarly skewed. It will be interesting to assess parent ratings of children’s feeding behaviors after the intervention to see whether there has been any change in perceptions or ratings; for instance, there could be an improvement in children’s actual feeding behavior but parents’ perceptions and ratings may change and therefore lead to more accurate or appropriate judgments.
Strengths and Limitations
A primary strength of the present study is its novel use of telemedicine to reach rural children and families who are obese. When used with adults who are obese, telemedicine has been found to be an effective avenue for weight loss and reduction of cardiovascular risk factors (Frisch et al., 2009; Goulis et al., 2004). Rural children and families are at risk for obesity and lack access to health care resources, and interventions that use technology to simulate in vivo treatment are likely to be an important component of behavioral medicine interventions in the coming years.
A second strength of the study is its use of objective assessment measures, namely accelerometers and multiple 24-hr dietary recalls. These tools are sometimes more burdensome for participants (i.e., wearing the monitor for 10 hr on multiple days, making multiple telephone appointments with research staff to complete dietary recalls) but they also provide superior data in terms of specificity and accuracy. Another strength of the study is the focus on rural children and families who are more likely to be obese, and may also lack sufficient health services.
Limitations of the present study include the fact that only baseline information can be presented at this time. Administration of the study’s independent variable (i.e., the 8-month intervention) has yet to be completed. However, the present study offers a novel intervention and methodology to treat rural pediatric obesity. Comprehensive explanation of the methodology and theory that informed present methodology is important for a nascent intervention. Evaluation of baseline data may provide greater understanding of factors concomitant with pediatric obesity in rural areas, as well as allow for replication of the intervention in other rural areas.
A second limitation is that only a small proportion of eligible families chose to participate in the intervention. This seemed to be for two main reasons. First, some families did not feel that their child were overweight/obese or unhealthy, and did not feel they needed to change. When school representatives sent home recruitment letters with the children, these families would often either speak to the school representative and state this or write this on the recruitment form and return it to the school representative. However, most of the families who did not participate signed up as having interest, but once they found out about the many measures and weekly hour long meetings, declined to participate due to the high burden for participation. It is helpful to compare the present study to previous telemedicine obesity interventions. The Goulis (2004) intervention was conducted in participants’ homes while the Frisch (2009) study held weekly meetings but also had dietary counseling sessions over the phone between group meetings. It is possible that the use of in-home technology reduced participant burden, or that between-meeting individual telephone sessions maintained engagement and motivation better than holding group meetings alone. However, the initial patient pool in Frisch (2009) was 298 and 206 chose to participate, while in Goulis (2004) the initial patient pool was 700 and 122 opted to participate. Thus, while the present study showed a high decline rate among the initial subject pool, it may be typical when compared to other TM for obesity.
Perhaps an intervention with lower participant burden would help to meet the needs of these non-participating families. More information is needed to determine how to reduce participant burden during TM for obesity while maintaining a sufficient level of contact and engagement among participants.
Future Directions
The different roles of physical activity and dietary intake on rural childhood obesity should be further examined. The present study as well as Davis and colleagues (Davis, Boles et al. 2008), Janicke (2008), and Dennison (2008) showed excessive calorie and/or junk food consumption. The present study suggests wide ranges in physical activity and sedentary behavior. However, more research using objective assessment tools such as accelerometers or multiple 24-hr dietary recalls may provide information necessary to delineate predictive relationships and factors that prevent rural children from attaining a healthy weight.
In addition, it is likely that increasingly more interventions will be delivered through telemedicine and similar technologies. Completion and replication of the present study will help to clarify whether telemedicine is an effective method for working with rural families and children who are obese and which factors must be modified in order to reach the most participants, prevent attrition and maintain healthy habits in the long term.
Conclusions
Due to a confluence of environmental and behavioral factors, rural children are at higher risk for developing obesity. Researchers and mental health professionals who target pediatric obesity in rural communities will play important roles in alleviating the physical, emotional, and economic consequences of this public health issue. The use of telemedicine could be one mode of intervention to increase rural access to research studies, mental health professionals, and other treatment options.
Funding
National Institute of Diabetes and Digestive and Kidney Diseases (K23 DK068221).
Conflicts of interest: None declared.
References
- Achenbach T M. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. 1991. University of Vermont, Department of Psychiatry, Burlington (VT) [Google Scholar]
- American Heart Association. Dietary Recommendations for Children. 2010. Retrieved from: http://www.americanheart.org/presenter.jhtml?identifier=3033999.
- Babbit R L, Hoch T A, Coe D A, Cataldo M F, Kelly K J, Stackhouse C, Perman J A. Behavioral assessment and treatment of pediatric feeding disorders. Journal of Developmental and Behavioral Pediatrics. 1994;15:278–291. [PubMed] [Google Scholar]
- Baker J L, Olsen L W, Sørensen T I. Childhood body mass index and the risk of coronary heart disease in adulthood. New England Journal of Medicine. 2007;357:2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch L L, Fisher J O. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- Braet C, Mervielde I, Vandereycken W. Psychological aspects of childhood obesity: A controlled study in a clinical and nonclinical sample. Journal of Pediatric Psychology. 1997;22:59–71. doi: 10.1093/jpepsy/22.1.59. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control. Overweight and obesity: Defining childhood overweight and obesity. 2010a. Retrieved from http://www.cdc.gov/obesity/childhood/defining.html.
- Center for Disease Control. Physical activity for everyone: How much physical activity do children need? 2010b. Retrieved from http://www.cdc.gov/physicalactivity/everyone/guidelines/ children.html.
- Champagne C M, Bogle M L, Karge W H III. Using national dietary data to measure dietary changes. Public Health and Nutrition. 2002;5:985–989. doi: 10.1079/PHN2002375. [DOI] [PubMed] [Google Scholar]
- Cherry DC, Huggins B, Gilmore K. Children’s health in the rural environment. Pediatric Clinics of North America. 2007;54:121–133. doi: 10.1016/j.pcl.2006.11.008. [DOI] [PubMed] [Google Scholar]
- Crawford P B, Obarzanek E, Morrison J, Sabry Z E. Comparative advantage of 3-day food records over 24-hour recall and 5-day food frequency validated by observation of 9- and 10-year-old girls. Journal of the American Dietetic Association. 1994;94:626–630. doi: 10.1016/0002-8223(94)90158-9. [DOI] [PubMed] [Google Scholar]
- Crist W, McDonnell P, Beck M, Gillespie C T, Barrett P, Matthews J. Behavior at mealtimes and the young child with cystic fibrosis. Journal of Developmental and Behavioral Pediatrics. 1994;15:157–161. [Google Scholar]
- Davis A M, Boles R E, James R L, Sullivan D K, Donnelly J E, Swirczynski D L, Goetz L. Health behaviors and weight status among urban and rural children. Rural and Remote Health. 2008;8:1–11. [PMC free article] [PubMed] [Google Scholar]
- Davis A M, James R L, Curtis M, Felts S, Daley C M. Pediatric obesity attitudes, services, and information among rural parents: A qualitative study. Obesity. 2008;16:2133–2140. doi: 10.1038/oby.2008.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C L, Flickinger B, Moore D, Bassali R, Domel Baxter S, Yin Z. Prevalence of cardiovascular risk factors in schoolchildren in a rural Georgia community. American Journal of Medical Science. 2005;330:53–9. doi: 10.1097/00000441-200508000-00001. [DOI] [PubMed] [Google Scholar]
- Dennison D A, Yin Z, Kibbe D, Burns S, Trowbridge F. Training health care professional to manage overweight adolescents: Experience in rural Georgia communities. The Journal of Rural Health. 2008;24:55–59. doi: 10.1111/j.1748-0361.2008.00137.x. [DOI] [PubMed] [Google Scholar]
- Epstein L H, Squires S. The Stoplight Diet for Children: An Eight-week Program for Parents and Children. Boston, MA: Little, Brown; 1988. [Google Scholar]
- Ford P B, Dzewaltowski D A. Limited supermarket availability is not associated with obesity risk among participants in the Kansas WIC program. Obesity. 2010;18:1944–1951. doi: 10.1038/oby.2009.487. [DOI] [PubMed] [Google Scholar]
- Freedman D S, Patel D A, Srinivasan S R, Chen W, Tang R, Bond MG, Berenson GS. The contribution of childhood obesity to adult carotid intima-media thickness: The Bogalusa Heart Study. International Journal of Obesity. 2008;35:749–756. doi: 10.1038/sj.ijo.0803798. [DOI] [PubMed] [Google Scholar]
- Frisch S, Zittermann A, Berthold H K, Götting C, Kuhn J, Kleesiek K, Stehle P, Körtke H. A randomized controlled trial on the efficacy of carbohydrate-reduced or fat-reduced diets in patients attending a telemedically guided weight loss program. Cardiovascular Diabetology. 2009;8:1–10. doi: 10.1186/1475-2840-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gombosi R L, Olasin R M, Bittle J L. Tioga County Fit for Life: A primary obesity prevention project. Clinical Pediatrics. 2007;46:592–601. doi: 10.1177/0009922807299315. [DOI] [PubMed] [Google Scholar]
- Goulis D G, Giaglis G D, Boren S A, Lekka I, Bontis E, Balas E A, Maglaveras N, Avramides A. Effectiveness of home-centered care through telemedicine applications for overweight and obese patients: A randomized controlled trial. International Journal of Obesity Related Metabolic Disorders. 2004;28:1391–1398. doi: 10.1038/sj.ijo.0802773. [DOI] [PubMed] [Google Scholar]
- Janicke D M, Sallinen B J, Perri M G, Lutes L D, Huerta M, Silverstein J H, Brumback B. Comparison of parent-only vs. family-based interventions for overweight children in underserved rural settings: Outcomes from Project STORY. Archives of Pediatric and Adolescent Medicine. 2008;162:1119–1125. doi: 10.1001/archpedi.162.12.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joens-Marte R R, Welk G J, Calabro M A, Russell D W, Nicklay E, Hensley L D. Rural-urban differences in physical activity, physical fitness, and overweight prevalence of children. The Journal of Rural Health. 2008;24:49–54. doi: 10.1111/j.1748-0361.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- Johnson S L, Birch L L. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- Krul M, van der Wouden J C, Schellecis F G, van Suijlekom-Smit L W, Koes B W. Musculoskeletal problems in overweight and obese children. Annals of Family Medicine. 2009;7:352–356. doi: 10.1370/afm.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorson B A, Melgar-Quinonez H R, Taylor C A. Correlates of fruit and vegetable intakes in US children. Journal of the American Dietetic Association. 2009;109:474–478. doi: 10.1016/j.jada.2008.11.022. [DOI] [PubMed] [Google Scholar]
- Lutfiyya M N, Lipsky M S, Wisdom-Behounek J, Inpanbutr-Martinkus M. Is rural residency a risk factor for overweight and obesity in U.S. children? Obesity. 2007;15:2348–2356. doi: 10.1038/oby.2007.278. [DOI] [PubMed] [Google Scholar]
- McMurray R G, Harrell J S, Bangdiwala S I, Deng S. Cardiovascular disease risk factors and obesity of rural and urban elementary school children. Journal of Rural Health. 1999;15:265–274. doi: 10.1111/j.1748-0361.1999.tb00760.x. [DOI] [PubMed] [Google Scholar]
- Michimi A, Wimberly M C. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health Geographics. 2010;9:1–14. doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery-Reagan K, Lianco J A, Heh V, Rettos J, Huston R S. Prevalence and correlates of high body mass index in rural Appalachian children ages 6–11 years. Rural Remote Health. 2009;9:1234–1244. [PubMed] [Google Scholar]
- Neovius M, Sundström J, Rasmussen F. Combined effects of overweight and smoking in late adolescence on subsequent mortality: Nationwide cohort study. British Medical Journal. 2009;338:1–8. doi: 10.1136/bmj.b496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C L, Carroll M D, Curtin L E. Prevalence of high body mass index in US children and adolescents, 2007-2008. Journal of the American Medical Association. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Sinha R, Fisch G, Teague B, Tamborlane W V, Banyas B, Allen K, Sovoye M, Rieger V, Taksali S, Barbetta G, Sherwin R S, Caprio S. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. New England Journal of Medicine. 2002;346:802–810. doi: 10.1056/NEJMoa012578. [DOI] [PubMed] [Google Scholar]
- Sirard J R, Melanson E L, Li L, Freedson P S. Field evaluation of the Computer Science and Applications, Inc., physical activity monitor. Medicine & Science in Sports & Exercise. 2000;32:695–700. doi: 10.1097/00005768-200003000-00022. [DOI] [PubMed] [Google Scholar]
- Sothern M S. Exercise as a modality in the treatment of childhood obesity. Pediatric Clinics of North America. 2001;48:995–1015. doi: 10.1016/s0031-3955(05)70353-9. [DOI] [PubMed] [Google Scholar]
- Stroehla B C, Malcoe L H, Velie E M. Dietary sources of nutrition among rural Native American and White children. Journal of the American Dietetics Association. 2005;105:1908–1916. doi: 10.1016/j.jada.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Taylor E D, Theim K R, Mirch M C, Ghorbani S, Tanofsky-Kraff M, Adler-Wailes D C, Brady S, Reynolds J C, Calis K A, Yanovski J A. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117:2167–2174. doi: 10.1542/peds.2005-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano R P, Berrigan D, Dodd K W, Mâsse L C, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]