Abstract
Objective Children and adolescents living in rural communities may be at particular risk for psychiatric problems, yet factors associated with mental health service use in these populations are not clear. This study examined the role of father warmth in offspring psychological treatment utilization in community sample of rural families (n = 298). Methods Observer ratings of paternal warmth were examined as a predictor of adolescent treatment seeking and as a moderator of the longitudinal association between adolescent depressive symptoms and treatment seeking. Results Paternal warmth was a marginally significant predictor of adolescent mental health service use. The association between adolescent depressive symptoms and treatment seeking varied as a function of paternal behavior; adolescents were more likely to seek needed help in the context of a warm, supportive father. Conclusions These findings suggest that fathers can play an important role in the intrafamilial processes through which rural adolescents recognize and seek help for their psychological problems.
Keywords: adolescents, at risk youth, depression, family functioning
Introduction
Often beginning in adolescence, depressive disorders are associated with a range of long-term psychosocial impairments and psychopathology (for review, see Hankin, 2006). Both clinical and subclinical levels of depressive symptoms have been linked to substance abuse, anxiety disorders, academic problems, cigarette smoking, high-risk sexual behavior, physical health problems, impaired social relationships, and suicide (Fergusson, Horwood, Ridder, & Beautrais, 2005; Field, Diego, & Sanders, 2001; Lewinsohn, Soloman, Seeley, & Zeiss, 2000). Moreover, of those who experience an initial episode of depression, up to 85% are expected to suffer from relapse or recurrence (American Psychiatric Association, 2000). Despite these risks, only a fraction of adolescents who meet criteria for disorders seek help or receive adequate treatment (e.g., Haines, McMunn, Nazroo, & Kelly, 2002; Saunders, Resnick, Hoberman, & Blum, 1994).
Rural adolescents may be at particular risk for mental health problems. Estimates using national samples indicate that adolescent depression prevalence rates are around 14% (e.g., Kessler & Walters, 1998), while in rural populations, estimates have been as high as 41% (Hauenstein & Boyd, 1994). Other research has consistently associated socioeconomic disadvantage with high psychiatric morbidity (Kessler et al., 2003; Lorant et al., 2003) and unmet need for mental health treatment (Flisher et al., 1997). These associations are not unique to rural populations, but they are particularly relevant considering that rural families, on average, have fewer resources and less access to mental health professionals than their urban counterparts (Goldsmith, Wagenfeld, Manderscheid, & Stiles, 1997). Considering that effective treatments for psychiatric problems are available (see DeRubeis, Siegle, & Hollon, 2008; Hollon, Thase, & Markowitz, 2002), the understanding of factors associated with mental health service use in rural populations has important clinical and policy implications.
Evidence suggests that fathers may be particularly underrepresented in pediatric psychology research and treatment (Phares, Lopez, Fields, Kamboukos, & Duhig, 2005). Despite this, a growing body of work has suggested that fathers play important roles in children’s functioning. For example, several recent cross-sectional studies have associated adversity in the father–offspring relationship with increased risk for adolescent depression (e.g., Plunkett, Henry, Robinson, Behnke, & Falcon, 2007; Sheeber, Davis, Leve, Hops, & Tildesley, 2007). Using a large, nationally representative sample, Zimmerman (2005) found that the presence of a father decreased the likelihood of children receiving needed treatment for internalizing and externalizing problems. The use of cross-sectional data limited causal inference, but this finding raises interesting questions about how or in which contexts fathers influence offspring mental health treatment utilization. One possibility is that positive aspects the father–adolescent relationship may serve to promote healthy treatment-seeking behavior. This would be consistent with a wealth of data from clinical and community samples that have demonstrated an inverse association between adolescent maladjustment and warm, supportive parenting (Sheeber et al., 2007). One of the processes underlying this association may involve intrafamilial social support when a family member experiences emotional problems that require professional treatment.
The present study seeks to contribute to the literature by examining interpersonal processes between the father and adolescent which may influence adolescent mental health treatment seeking. Prospective data from a large, nonclinical sample of rural families were used to address the two main study objectives. First, observer ratings of paternal warmth exhibited toward their adolescent offspring were examined as predictors of subsequent adolescent treatment seeking. We expected that father warmth would be positively associated with adolescent treatment seeking (H1). Second, father warmth was evaluated as a moderator of the association between adolescent depressive symptoms and mental health service utilization. We hypothesized that the longitudinal association between depressive symptoms and treatment seeking would be stronger in the context of higher levels of paternal warmth (H2).
Method
Participants and Procedures
Participants from this study took part in the Iowa Youth and Families Project (Conger & Conger, 2002; Conger & Elder, 1994), an ongoing longitudinal investigation originally focused on family relationships and individual development during the extreme downturn of the Midwest rural agriculture economy during the 1980s. This economic decline marked a period of financial crisis for many rural families, as thousands of small businesses and family owned and operated farms were forced to close (Lasley, 1994). The sample for current analyses consists of 298 adolescents (164 female, 134 male) from two-parent intact families living in the rural Midwest. Participants were from predominately middle- and lower-middle class families who resided on farms (34%), in nonfarm rural areas (12%), or in small towns (54%).
Families were originally recruited from seventh-grade classes in 34 public and private schools across 8 rural counties in central Iowa. Within these counties, names and addresses of seventh-grade students and their parents were obtained from all schools in communities of 6,500 or less. All eligible families were contacted via telephone and mail, and asked to participate. Of the eligible families, 78% agreed to participate in the first wave of data collection. Participants were compensated with approximately $10 per each hour spent in the study.
Due to the ethnic composition of the area, all families were European-American. The first wave of data in the present study was collected from a sample of adolescents in the 12th grade (mean age = 17.4 years). Of the original families, approximately 95% of the sample remained in the study one year later at Time 2. No significant differences in parents’ age, family income, or parents’ level of education were found between participants remaining in the study compared to those who dropped out.
During the first year of the present study, families were visited twice by trained interviewers; each visit lasted approximately 2 hr. For the first visit, family members individually completed questionnaires concerning family life, school, finances, and mental health. During the second visit, which occurred within 2 weeks of the first, parents and adolescents were videotaped while engaged in a 30-min family discussion task. In this task, family members sat at a table together and were given cards instructing them to discuss general questions about family life, such as how the family interacted, parental expectations of the children, and the children’s relationship with each parent. Videotapes were coded using the Iowa Family Interaction Rating Scale (Melby & Conger, 2001), which was designed to measure the nature of behavioral exchanges between family members. Observers received 2 months of training and had to pass extensive written and viewing tests before coding videotapes. For approximately 25% of the videotaped tasks, a second observer was randomly assigned to code family interactions in order to estimate interobserver reliability. Details regarding the paternal warmth variable are provided in the following section on study measures.
Measures
Mental Health Services Utilization
Adolescent mental health treatment utilization was categorized as hospitalization or outpatient treatment for symptoms of a mental disorder from a mental health professional including psychologists, psychiatrists, or social workers. On a 4-point scale ranging from 1 (never) to 4 (often), adolescents reported on the frequency of treatment seeking during the 12 months preceding the interview. This measure of mental health service use has been used in previous research on the prevalence and comorbidity of psychiatric disorders among young adults (e.g., Rueter, Holm, Burzette, Kim, & Conger, 2007).
Psychological Symptoms
Adolescents’ psychological symptoms were assessed at Time 1 using the depression, anxiety, and hostility subscales of the Symptom Checklist 90-Revised (SCL-90-R; Derogatis, 1983), which has demonstrated reliability and validity in many studies of adolescents and adults (e.g., Essau, 2004). Composite scores were created separately for each subscale; higher scores indicated higher levels of symptoms. In our sample, internal consistencies for all three subscales were satisfactory (depression α = .86; anxiety α = .89; hostility α = .92). Adolescents’ raw score means for the depression subscale (.64) were slightly lower than the score of .80 reported for the normative sample in the SCL-90-R manual (Derogatis, 1983).
Father Warmth
Ratings of paternal warmth by independent observers during the videotaped interaction task were used to measure fathers’ level of expressed interest, care, concern, support, encouragement, and responsiveness towards their adolescent offspring. This measure emphasized fathers’ nonverbal communication (e.g., physical gestures, eye contact), emotional expression (e.g., smiling, laughing), supportiveness (e.g., offering encouragement or praise), and responsiveness (e.g., asking follow-up questions to show interest) directed towards their adolescent offspring. Using a scale from 1 (the behavior is not at all characteristic) to 9 (the behavior is highly characteristic), higher scores indicated higher levels of warmth, affection, and support. The interobserver reliability coefficient for this measure was .82.
Results
Bivariate correlations and descriptive statistics are presented in Table 1. Consistent with previous research on gender differences in the prevalence of internalizing problems (see Nolen-Hoeksema & Hilt, 2009), being male was negatively associated with depressive and anxiety symptoms. There was a significant negative association between adolescent gender and mental health service utilization indicating less treatment seeking among boys. Depressive, anxiety, and hostility symptoms were all significantly and positively intercorrelated, a finding consistent with the epidemiology of depression, which has shown that depressive disorders often co-occur with other psychiatric problems (for review, see Boland & Keller, 2009). Adolescent depressive symptoms at Time 1 were positively associated with mental health treatment seeking at Time 2. Correlational analyses also provided preliminary support for the study hypotheses, indicating a significant positive association between paternal warmth and subsequent adolescent treatment seeking.
Table I.
Descriptive Statistics and Correlations
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. Gender (1 = male) | – | – | ||||||
| 2. Per-capita family income/1,000 | 12.81 (11.44) | −.04 | – | |||||
| 3. SCL-90-R depression | 0.64 (0.65) | −.24*** | .00 | – | ||||
| 4. SCL-90-R anxiety | 0.40 (0.52) | −.15** | −.05 | .74*** | – | |||
| 5. SCL-90-R hostility | 0.54 (0.60) | .01 | .03 | .64*** | .64*** | – | ||
| 6. Father warmth | 6.13 (1.99) | −.02 | .09 | −.10 | −.17** | −.21*** | – | |
| 7. Time 2 mental health service utilization | 1.10 (0.46) | −.12* | −.01 | .12* | .07 | .05 | .10* | – |
Note. n = 298.
*p < .05, **p < .01, ***p < .001.
Ordinary least squares multiple regression analyses were conducted using PASW 18 statistical software (Allen & Bennett, 2010). Regression parameter estimates are presented in Table 2. Adolescent gender was coded as 0 for female and 1 for male. All continuous independent variables were grand mean centered and adolescent gender and per capita family income were included as covariates due to their potential to influence the outcome measure. Family demographic measures including parental age and education were also included as statistical controls; these covariates did not produce significant effects and, for the sake of brevity, are excluded from reported analyses.
Table II.
Ordinary Least Squares Regression Coefficients Predicting Time 2 Treatment Utilization from Gender, Family Income, Psychological Symptoms, and Paternal Warmth
| Independent variables | β | SE | b |
|---|---|---|---|
| Gender (1 = male) | −0.088 | 0.054 | −0.078 |
| Per-capita family income | −0.032 | 0.000 | 0.000 |
| SCL-90-R depression | 0.024 | 0.065 | 0.016 |
| SCL-90-R anxiety | 0.033 | 0.083 | 0.030 |
| SCL-90-R hostility | 0.056 | 0.060 | 0.041 |
| Paternal warmth | 0.113† | 0.014 | 0.026 |
| Depression by paternal warmth | 0.179* | 0.062 | 0.063 |
| Constant | 1.134 | ||
| R2 | .083** |
Note. n = 298.
F(11, 286) = 2.37, p < .01.
†p < .10; *p < .05; ** p < .01.
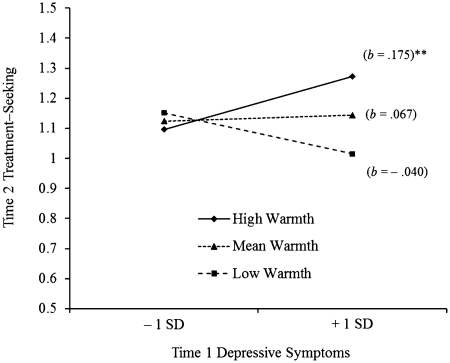
Controlling for adolescent psychological symptoms, paternal warmth was a marginally significant predictor of subsequent adolescent help seeking (p = .059), providing partial support for H1. The statistical interaction between adolescent depressive symptoms and father warmth indicated that the association between adolescent depressive symptoms and treatment seeking varied as a function of father warmth. As suggested by Holmbeck (2002), post hoc probing of the interaction effect was conducted in which simple regression equations were generated at each level of paternal warmth (see Figure 1). Consistent with H2, significance tests demonstrated that only the slope for high-warmth fathers was significantly different from zero, the direction indicating a stronger association between depressive symptoms and treatment seeking among adolescents when paternal warmth was high. Together, the independent measures in this model accounted for roughly 8.3% of the variance in adolescent mental health treatment utilization.
Figure 1.
Adolescent treatment seeking as a function of depressive symptoms and paternal warmth. Note. SD = standard deviation, b = unstandardized regression coefficient. **p < .01.
Discussion
Nearly a third of the children and adolescents in the United States live in rural areas (Petti & Leviton, 1986). Recent estimates indicate significant risk for depression in these individuals (Rueter et al., 2007), who often live in areas with shortages of mental health professionals, limited transportation, and a lack of service outreach (Spoth, 1997). Despite this, there has been relatively little systematic study of factors related to treatment seeking in rural communities (Jesse, Dolbier, & Blanchard, 2008). In particular, little is known about how the family context or environment may influence whether adolescents find help for their psychological problems. This report extends previous work by examining the role of father–offspring interactions in relation to rural adolescent mental health treatment utilization. Father warmth was a marginally significant predictor of adolescent treatment seeking 1 year later, after controlling for gender and family demographic measures. Moreover, paternal warmth moderated the longitudinal association between offspring depressive symptoms and subsequent treatment seeking such that adolescents were more likely to seek needed help in the context of a warm, supportive father. This interaction effect remained significant after including adolescent anxiety and hostility symptoms as covariates.
In the current study, we focused on fathers, who continue to be dramatically under-represented in research on children’s development (Phares et al., 2005). As noted earlier, previous work using a national sample indicated that the presence of the father was linked to fewer concurrent adolescent attempts to seek treatment (Zimmerman, 2005). Zimmerman suggested that, compared to mothers, fathers may be more opposed to the idea of mental health treatment. Indeed, research has consistently associated traditional notions of masculinity with the tendency for many men to hide, overlook, or under-report symptoms of depression (e.g., Brownhill, Wilhelm, Barclay, & Schmied, 2005). Findings from the present study suggest that it may not only be the presence of the father that influences adolescent treatment seeking, but also, the nature of the father–adolescent relationship. This is consistent with previous work indicating that in families experiencing depression, resilience in offspring is associated with the availability of a support system for the child (Luthar & Zigler, 1991).
Data presented here also indicated that the association between offspring depressive symptoms and mental health service use was a function of the paternal warmth; only at high levels of warmth did adolescent depressive symptoms predict treatment utilization. It may be that fathers’ warmth contributed to a context of open communication which influenced adolescents’ willingness to disclose more about her or his emotional state, which, in turn, provided fathers the opportunity to assist their children in finding professional help. Indeed, previous research indicates that processes of emotional self-disclosure may function as a means by which adolescents gain social input or provisions that address underlying concerns (Buhrmester & Prager, 1995). Likewise, warmth and support from a father may contribute to adolescent self-esteem and to the feeling that they are worthwhile and deserving of help for their psychological distress, a process consistent with recent work on fathers’ family involvement suggesting that children have better social and behavioral outcomes when fathers are available and involved in the daily activities and care of their children (see Pleck, 2007).
Families in rural areas are likely to experience multiple barriers to psychological treatment. As noted previously, limited transportation, cost of care and lack of health insurance, and a scarcity of experienced mental health professionals are all commonly cited obstacles to treatment for individuals from rural communities (e.g., Fox, Blank, Rovnyak, & Barnett, 2001). The stigma associated with psychiatric disorders may be another particularly salient obstacle to mental health treatment in rural communities. Compared to their urban counterparts, rural residents are more likely to have conservative views on mental health and to make negative attributions about people who seek psychological treatment (Rost, Smith, & Taylor, 1993). Furthermore, the lack of anonymity characteristic of many close-knit rural communities may increase the likelihood of being labeled for seeking help (Berry & Davis, 1978). Together, these findings suggest that rurality may play a role in how families respond when children experience depression or depressive symptoms. An important direction for future work will be to examine how access to mental health care and attitudes toward psychological treatment may influence the association between parent–offspring relationships and adolescent treatment seeking in high-risk populations.
There were several important limitations to this study that should be considered in future research. Perhaps most importantly, a substantial proportion of the variance in adolescent depressive symptoms remains unexplained by these independent variables and covariates. Given the complex transactional and interpersonal nature of depression in families (Kaslow, Deering, & Racusin, 1994), it is likely that adolescent treatment utilization is influenced by an array of additive and interactive factors including individual characteristics of adolescents and parents and multiple family relationships. Subsequent prospective studies will benefit from more comprehensive models of family functioning and mental health treatment utilization. For example, it will be important to consider how maternal and sibling characteristics may influence the association between adolescent psychological problems and treatment seeking. Additionally, the effects of adversity in family relationships on offspring mental health service use warrant further investigation.
Given the relatively low levels of symptoms reported from this rural community sample of adolescents, the results may not generalize to clinical populations. However, it is important to note that the majority of research to date on adolescent depression has relied on clinical samples which may not be representative of the general population of adolescents (Costello, Foley, & Angold, 2006). Other limitations include the European-American nature of the sample and the fact that the current data were collected in the 1980s. Replication of these results with more diverse and recent samples, including single parent, same sex, urban, and minority families is needed. Future work will also benefit from the utilization of a more rigorous and reliable measure of mental health help seeking, such as information from medical records.
In summary, we found evidence that in rural families, fathers’ behavior can promote offspring mental health treatment seeking. Future research will help shed light on the mechanisms underlying this process, as well as on other intrafamilial moderators of the association between adolescent psychological symptoms and treatment utilization. Ultimately, the understanding of the role of family functioning in adolescent mental health service use may have valuable applied implications, considering the efficacy of data driven, family-level interventions in families experiencing depression (e.g., Garber et al., 2009). Despite the myriad of barriers to treatment, many rural adolescents experiencing clinical depression or depressive symptoms are able to obtain effective professional mental health treatment (Rost, Zhang, Fortney, Smith, & Smith, 1998), and we hope these results assist other youth to obtain services when needed. Consistent with Zimmerman (2005), findings from the present study indicate that it may be particularly important to help fathers recognize their children’s psychological problems. In addition, the current analyses suggest and that in rural communities, both families and mental health providers should pay attention to the father–adolescent relationship which may serve as a facilitator of or barrier to (i.e., a moderator) adolescent mental health treatment seeking and utilization.
Funding
This research is currently supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health (HD064687, HD051746, and MH051361). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Support for earlier years of the study also came from multiple sources, including the National Institute of Mental Health (MH00567, MH19734, MH43270, MH59355, MH62989, and MH48165); the National Institute on Drug Abuse (DA05347); the National Institute of Child Health and Human Development (HD027724, HD047573); the Bureau of Maternal and Child Health (MCJ-109572); and the MacArthur Foundation Research Network on Successful Adolescent Development Among Youth in High-Risk Settings.
Conflict of interest: None declared.
References
- Allen P J, Bennett K. PASW statistics by SPSS: Version 18.0. South Melbourne: Cengage Learning; 2010. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. revised 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Berry B, Davis A E. Community mental health ideology. American Journal of Orthopsychiatry. 1978;48(4):673–679. doi: 10.1111/j.1939-0025.1978.tb02572.x. [DOI] [PubMed] [Google Scholar]
- Boland R J, Keller M B. Course and outcome of depression. In: Gotlib I H, Hammen C L, editors. Handbook of depression. New York: Guilford Press; 2009. pp. 2023–2043. [Google Scholar]
- Brownhill S, Wilhelm K, Barclay L, Schmied V. “Big build”: Hidden depression in men. Australian and New Zealand Journal of Psychiatry. 2005;39:921–931. doi: 10.1080/j.1440-1614.2005.01665.x. [DOI] [PubMed] [Google Scholar]
- Buhrmester D, Prager K. Patterns and functions of self–disclosure during childhood and adolescence. In: Rotenberg K J, editor. Disclosure processes in children and adolescents. New York, NY, US: Cambridge University Press; 1995. pp. 1910–1956. [Google Scholar]
- Costello E J, Foley D L, Angold A. 10–year research update review: The epidemiology of child and adolescent psychiatric disorders II: Developmental epidemiology. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Conger R D, Conger K J. Resilience in Midwestern families: Selected findings from the first decade of a prospective, longitudinal study. Journal of Marriage and Family. 2002;64:361–373. [Google Scholar]
- Conger, R. D., & Elder, G. H. Jr. (Eds.). (1994). Families in troubled times: Adapting to change in rural America. Hawthorne, NY: Aldine de Gruyter.
- Derogatis L. SCL–90–R administration, scoring, and procedures Manual II. Townsen, MD: Clinical Psychometric Research; 1983. [Google Scholar]
- DeRubeis R J, Siegle G J, Hollon S D. Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience. 2008;9(10):788–796. doi: 10.1038/nrn2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau C A. The association between family factors and depressive disorders in adolescents. Journal of Youth and Adolescence. 2004;33:365–372. [Google Scholar]
- Fergusson D M, Horwood L J, Ridder E M, Beautrais A L. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Sanders C E. Adolescent depression and risk factors. Adolescence. 2001;36:491–498. [PubMed] [Google Scholar]
- Flisher A J, Kramer R A, Grosser R C, Alegria M, Bird H R, Bourdon K H, Goodman S H, Greenwald S, Horwitz S M, Moore R E, Narrow W E, Hoven C W. Correlates of unmet need for mental health services by children and adolescents. Psychological Medicine. 1997;27:1145–1154. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Fox J C, Blank M, Rovnyak V G, Barnett R Y. Barriers to help seeking for mental disorders in a rural impoverished population. Community Mental Health Journal. 2001;37:421–436. doi: 10.1023/a:1017580013197. [DOI] [PubMed] [Google Scholar]
- Garber J, Clarke G N, Weersing V R, Beardslee W R, Brent D A, Gladstone T R G, DeBar L L, Lynch F L, D’Angelo E, Hollon S D, Shamseddeen W, Iyengar S. Prevention of depression in at–risk adolescents: A randomized controlled trial. JAMA. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith H F, Wagenfeld M O, Manderscheid R W, Stiles D. Specialty mental health services in metropolitan and nonmetropolitan areas: 1983 and 1990. Administration and Policy in Mental Health and Mental Health Services Research. 1997;24(6):475–488. doi: 10.1007/BF02042826. [DOI] [PubMed] [Google Scholar]
- Haines M M, McMunn A, Nazroo J Y, Kelly Y J. Social and demographic predictors of parental consultation for child psychological difficulties. Journal of Public Health. 2002;24(4):276–284. doi: 10.1093/pubmed/24.4.276. [DOI] [PubMed] [Google Scholar]
- Hankin B L. Adolescent depression: Description, causes, and interventions. Epilepsy & Behavior. 2006;8:102–114. doi: 10.1016/j.yebeh.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Hauenstein E J, Boyd M E. Depressive symptoms in young women of the Piedmont: Prevalence in rural women. Women & Health. 1994;21(2):105–123. doi: 10.1300/j013v21n02_07. [DOI] [PubMed] [Google Scholar]
- Hollon S D, Thase M E, Markowitz J C. Treatment and Prevention of Depression. Psychological Science in the Public Interest. 2002;3(2):39–77. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- Holmbeck G N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. Special Issue on Methodology and Design. 2002;27(1):87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Jesse D E, Dolbier C L, Blanchard A. Barriers to seeking help and treatment suggestions for prenatal depressive symptoms: Focus groups with rural low–income women. Issues in Mental Health Nursing. 2008;29(1):3–19. doi: 10.1080/01612840701748664. [DOI] [PubMed] [Google Scholar]
- Kaslow N J, Deering C G, Racusin G R. Depressed children and their families. Clinical Psychology Review. 1994;14:39–59. [Google Scholar]
- Kessler R C, Berglund P, Demler O, Jin R, Koretz D, Merikangas K R, Rush A J, Walters E E, Wang P S. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS–R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler R C, Walters E E. Epidemiology of DSM–III–R major depression and minor depression among adolescents and young adults in the national comorbidity survey. Depression and Anxiety. 1998;7(1):3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Lasley P. Rural economic and social trends. In: Conger R D, Elder G H Jr., editors. Families in troubled times. Hawthorne, NY: Aldine de Gruyter; 1994. pp. 57–78. [Google Scholar]
- Lewinsohn P M, Solomon A, Seeley J R, Zeiss A. Clinical implications and “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109:345–351. [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Luthar S S, Zigler E. Vulnerability and competence: A review of research on resilience in childhood. American Journal of Orthopsychiatry. 1991;61:6–22. doi: 10.1037/h0079218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melby J N, Conger R D. The Iowa Family Interaction Rating Scales: Instrument summary. In: Kerig P, Lindahl K, editors. Family observational coding systems: Resources for systematic research. Mahwah, NJ: Erlbaum; 2001. pp. 33–58. [Google Scholar]
- Nolen-Hoeksema S, Hilt L M. Gender differences in depression. In: Gotlib I H, Hammen C L, editors. Handbook of depression. New York: Guilford Press; 2009. pp. 2386–2404. [Google Scholar]
- Petti T A, Leviton L C. Re-thinking rural mental health services for children and adolescents. Journal of Public Health Policy. 1986;7:58–77. [PubMed] [Google Scholar]
- Phares V, Fields S, Kamboukos D, Lopez E. Still looking for poppa. American Psychologist. 2005;60:735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- Pleck J H. Why could father involvement benefit children? Theoretical perspectives. Applied Developmental Science. 2007;11(4):196–202. [Google Scholar]
- Plunkett S W, Henry C S, Robinson L C, Behnke A, Falcon P C. Adolescent perceptions of parental behaviors, adolescent self-esteem, and adolescent depressed mood. Journal of Child and Family Studies. 2007;16:760–772. [Google Scholar]
- Rost K, Smith G R, Taylor J L. Rural–urban differences in stigma and the use of care for depressive disorders. The Journal of Rural Health. 1993;9(1):57–62. doi: 10.1111/j.1748-0361.1993.tb00495.x. [DOI] [PubMed] [Google Scholar]
- Rost K, Zhang M, Fortney J, Smith J, Smith G R J. Rural–urban differences in depression treatment and suicidality. Medical Care. 1998;36(7):1098–1107. doi: 10.1097/00005650-199807000-00015. [DOI] [PubMed] [Google Scholar]
- Rueter M, Holm K, Burzette R, Kim K, Conger R. Mental health of rural young adults: Prevalence of psychiatric disorders, comorbidity, and service utilization. Community Mental Health Journal. 2007;43(3):229–249. doi: 10.1007/s10597-007-9082-y. [DOI] [PubMed] [Google Scholar]
- Saunders S M, Resnick M D, Hoberman H M, Blum R W. Formal help-seeking behavior of adolescents identifying themselves as having mental health problems. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(5):718–728. doi: 10.1097/00004583-199406000-00013. [DOI] [PubMed] [Google Scholar]
- Sheeber L B, Davis B, Leve C, Hops H, Tildesley E. Adolescents’ relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R. Challenges in defining and developing the field of rural mental disorder preventive intervention research. American Journal of Community Psychology. 1997;25(4):425–448. doi: 10.1023/a:1024603504781. [DOI] [PubMed] [Google Scholar]
- Zimmerman F J. Social and economic determinants of disparities in professional help-seeking for child mental health problems: Evidence from a national sample. Health Services Research. 2005;40:1514–1533. doi: 10.1111/j.1475-6773.2005.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]