Abstract
Objective To test structural models of parental involvement in type 1 diabetes and to examine associations of parental involvement with adherence and metabolic control. Methods Two hundred and fifty-two young adolescents (10–14 years) completed reports of adherence and parents’ involvement: acceptance, independence encouragement, communication, general and diabetes-specific monitoring, frequency of help, and intrusive support. HbA1c values came from medical records. Results A model of relationship quality, behavioral involvement, and monitoring as three separate yet interrelated factors best fit the data. Higher reports of mothers’ and fathers’ monitoring and fathers’ relationship quality uniquely related to better adherence, whereas higher reports of fathers’ behavioral involvement uniquely related to poorer adherence. Higher reports of paternal monitoring were related to lower HbA1c. Conclusions Adolescent perceptions of components of parental involvement are interrelated, yet separate constructs for both mothers and fathers. Parental monitoring was an important predictor of management of type 1 diabetes during adolescence.
Keywords: adherence, fathers, involvement, monitoring, mothers, parenting, young adolescents
Parental behaviors are of interest to researchers across multiple fields and disciplines. In Pediatric Psychology, parenting is critical as families deal with complex disease management (e.g., Ellis et al., 2007; Ellis, Templin, Naar-King, & Frey, 2008; Palmer et al., 2004; Seiffge-Krenke, 2002; Wiebe et al., 2005). Researchers have conceptualized parental behaviors in a variety of ways, including acceptance, monitoring, behavioral involvement, responsibility for disease management, and support, with most of the work measuring parental involvement via single assessment indicators (Anderson, Auslander, Jung, & Miller, 1990; Holmbeck, 2002; Laffel et al., 2003). Although the field has amassed an impressive number of family assessment measures (Alderfer et al., 2008), questions remain as to whether parental behaviors are all part of one unified construct or whether they reflect distinct components of involvement. Also, researchers have focused heavily on maternal involvement (c.f., Seiffge-Krenke, 2002; Wysocki & Gavin, 2006) despite the fact that the broader Developmental Psychology literature acknowledges the important role fathers play (Bumpus, Crouter, & McHale, 2006). In this study, we examined the structure that underlies adolescents’ perspectives of mothers’ and fathers’ involvement and its connections to diabetes management.
The successful management of type 1 diabetes has been linked to an array of positive parenting characteristics. For instance, better adherence and metabolic control in diabetes management have been associated with children having a warm, accepting and supportive parent as well as a parent who is behaviorally involved in the daily management of diabetes (Anderson, Ho, Bracket, Finkelstein, & Laffel, 1997; Ellis et al., 2007; Wiebe et al., 2005). Recent work also suggests that parental monitoring—parents’ regular contact with and supervision of adolescents’ daily activities—is important for diabetes management (Berg et al., 2008; Ellis et al., 2007; Ellis, Templin, Naar-King, & Frey, 2008). An important question is whether measures of parental involvement are indicators of a global construct of “good” parental behaviors, measure separate but related constructs, or are indicators of distinct constructs of parents’ involvement in diabetes management.
Many behaviors have been combined under the heading of positive parental involvement within Developmental, Educational, and Pediatric Psychology (Day, Lewis, O’Brien, & Lamb, 2005; Fan & Chen, 2001; Palmer et al., 2004). For instance, in Developmental Psychology, Dishion and McMahon (1998) suggest the existence of multiple aspects of parenting, including relationship quality (trust, security), monitoring and behavior management (e.g., limit setting), all of which are interrelated, though separate, dimensions of the parent–child relationship. Implicit within the diabetes literature is the notion that there may be two components of parental involvement, one focused on the emotional and supportive quality of the relationship and the other on more instrumental aspects of involvement, including monitoring and behavioral involvement (Berg et al., 2008; Ellis et al., 2007; Wysocki et al., 2006). Recent pediatric work also distinguishes between monitoring and behavioral involvement; parents, for instance, may demonstrate low daily behavioral involvement (e.g., not be responsible for blood glucose checks), but may closely monitor their adolescents’ blood glucose levels (Ellis et al., 2007).
There has been limited research examining fathers’ involvement in diabetes management, though recently, investigators have compared maternal and paternal involvement (Berg et al., 2008; Wysocki & Gavin, 2006). Some propose a multidimensional conceptualization of father behaviors (Day, Lewis, O’Brien, & Lamb, 2005) and emphasize differences from maternal behaviors (e.g., dads demonstrate more instrumental task performance: Collins & Russell, 1991), but others suggest that paternal behaviors—in the context of disease management—are more similar to maternal behaviors (Hawkins & Palkovitz, 1999).
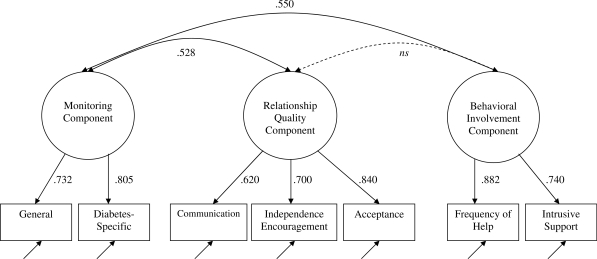
In the current study, we had two overarching goals. First, we compared three structural models, conceptualizing parental involvement as (1) a single global factor; (2) two separate but interrelated constructs—relationship quality and behavioral involvement; and (3) a three-factor model consisting of relationship quality, behavioral involvement, and monitoring (see Figure 1). We tested these models separately for adolescents’ perceptions of mothers’ and fathers’ involvement, predicting that the three-factor model was the most likely to be supported. Second, we examined the relationship of these factors to adolescents’ adherence and blood glucose control. We expected that each identified factor would be associated with better adherence and metabolic control.
Figure 1.
Results of the confirmatory factor analysis (CFA) conducted to identify the factor structure of maternal involvement. Significant correlations and standardized path coefficients (p < .05) are presented in the figure
Materials and Methods
Participants
Participants included 252 young adolescents (M age = 12.49 years, range: 10–14 years, SD = 1.53, 53.6% females) diagnosed with type 1 diabetes mellitus recruited from a university/private partnership (76%) and a community-based private practice (24%). For each adolescent, one mother and one father were eligible to participate (74% of fathers participated), with most being the biological parent (mothers = 96.8%, fathers = 74.6%). Eligibility criteria included that adolescents had diabetes more than 1 year (M = 4.13 years, SD = 3, range: 1–12 years), were able to read and write either English or Spanish (3 individuals completed a Spanish version of the materials), and resided with the participating mother. Families were largely Caucasian (94%) and middle class with most (73%) reporting household incomes averaging $50,000 or more annually; 51% of mothers and 58% of fathers reported education levels of 2 years of college or beyond and had an average Hollingshead Index (1975) of 5, indicating a medium business, minor professional, technical status. Of the qualifying individuals approached, 66% agreed to participate in the study, the first wave of a 3-year longitudinal study (the most common reasons for refusal included distance of commute 18%, too busy 21%, not interested 30%, uncomfortable with being studied 14%, and too much of a time commitment 5%). Comparisons of eligible adolescents who participated versus those who did not indicated that participants versus non-participants were older (12.5 vs. 11.6, t(367) = 6.2, p < .01) but did not differ on gender, pump status, HbA1c or time since diagnosis (ps > .20). Approximately half (50.8%) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI: M = 4.14 insulin injections, SD = 1.81, range: 0–10; 5.53 blood glucose checks daily; SD = 1.70, range: 1–11).
Measures
Measures of Relationship Quality
Acceptance
The acceptance subscale of the Mother–Father–Peer Scale (MFP; Epstein, 1983) consisted of five items where adolescents rated on a 1 (strongly disagree) to 5 (strongly agree) scale on how much the parent communicated love and acceptance. An average score was obtained (reports on mothers: α = .73, M = 4.39, SD = 0.65; reports on fathers: α = .83, M = 4.24, SD = 0.81). In adolescents, the MFP correlates with parental attachment (Bernier, Larose, & Whipple, 2005).
Independence Encouragement
This subscale from the MFP (Epstein, 1983) consisted of seven items where adolescents rated on a 1 (strongly disagree) to 5 (strongly agree) scale whether parents promoted and encouraged independence. An average score was obtained (reports on mothers α = .79, M = 4.05, SD = 0.62; reports on fathers: α = .87, M = 3.99, SD = 0.77).
Communication
This subscale from the Inventory of Parent and Peer Attachment, which has demonstrated adequate validity and reliability (Armsden & Greenberg, 1987), consisted of five items on a 1 (almost never or never true) to 5 (almost always or always true) scale assessing adolescents’ communication with parents. Average scores were computed (reports on mothers: α = .64, M = 4.00, SD = 0.66; reports on fathers: α = .69, M = 3.82, SD = 0.75).
Measures of Behavioral Involvement
Intrusive Support
This scale, which demonstrated adequate validity and reliability (α = .86, r = .69; Pomerantz & Eaton, 2001), was modified to include four items adolescents rated on a 1 (never) to 4 (all of the time) scale on how often they received unasked-for-assistance with diabetes from parents. An average score was computed (reports on mothers: α = .83, M = 2.50, SD = 0.80; reports on fathers: α = .87, M = 1.87, SD = 0.81).
Frequency of Help
One item each for mother and father assessed how frequently they provided assistance with diabetes tasks. The response choices were 0 days (never) = 1 to daily = 5. For reports on mothers: M = 4.57, SD = 0.89 and for reports on fathers: M = 3.47, SD = 1.50.
Measures of Monitoring
General Monitoring
Adolescents completed a scale of general parental monitoring, which shows excellent reliability and external validity (Barber, 1996; Brown, Mounts, Lamborn, & Steinberg, 1993), predicting an array of positive behaviors. This measure consisted of five items where adolescents rated on a 1 (doesn’t know) to 5 (knows everything) scale on parents’ knowledge of their daily activities. An average score was computed (reports on mothers: α = .80, M = 4.26, SD = 0.62; reports on fathers: α = .85, M = 3.52, SD = 0.96).
Diabetes Monitoring
Five items captured adolescents’ perceptions of their parents’ knowledge of diabetes care behaviors adapted from the general monitoring scale. Response choices were 1 (doesn’t know) to 5 (knows everything). An average score was computed (reports on mothers: α = .90, M = 4.10, SD = 0.79; reports on fathers: α = .91, M = 3.04, SD = 1.06).
Adherence
Sixteen items from the Self-Care Inventory (La Greca, Follansbee, & Skyler, 1990) were used to assess adolescents’ adherence to their recommended diabetes management regimens. Total scores on this scale have good validity (α = .88; La Greca, Swales, Kemp, & Madigan, 1988) and correlate well with more time-intensive interview methods measuring adherence (La Greca et al., 1995). This scale was adapted to reflect current standards of diabetes care by a certified diabetes educator. Items were updated and two items were added to reflect the current focus on carbohydrate counting and adjusting insulin rather than following a specific food plan (e.g., “How well have you followed recommendations for counting carbohydrates?”). Response choices were 1 (never) to 5 (always, without fail). All items were used to compute an average score and the scale had good internal consistency (α = .85; M = 3.94, SD = 0.58).
Metabolic Control
Adolescents’ metabolic control was indexed by glycosolated hemoglobin (HbA1c) using the Bayer DCA2000 and values were drawn from medical records at recruitment. HbA1c represents the average blood glucose over the prior 2–3 months, with higher levels indicating poorer metabolic control. The average HbA1c level was 8.16 (range = 4.9–13.9, SD = 1.58). This average was above the 7% level (representing 170 mg/dl mean plasma glucose over the preceding 2–3 months) considered good control (American Diabetes Association, 2007).
Procedure
The study was approved by the Institutional Review Board, with parents providing informed consent and adolescents written assent. During recruitment at their diabetes clinic appointments, participants received questionnaires to be completed independently prior to coming to their laboratory appointments where they completed additional questionnaires; medical records were accessed for blood glucose. The measures reported here are a subset of those included in the larger study (e.g., Berg et al., 2008; Palmer et al., 2009).
Statistical Analysis
All analyses were conducted as Structural Equation Models in EQS version 6.1 (Bentler, 2005). Adolescents’ reports of mothers’ and fathers’ involvement were analyzed separately as we were interested in the factor structure for each as opposed to a couple-effect that would be produced if run together. We first tested the factor structure of parental involvement by examining three different models, each of which were extrapolated from the parental involvement literature. We then expanded the best fitting model to examine how the resultant factors predicted adolescents’ adherence and metabolic control. The initial confirmatory factor models were evaluated using commonly accepted goodness of fit indices that are believed to function acceptably for this sample size (Hu & Bentler, 1998; Marsh, Balla, & MacDonald, 1988). In the final model, our interest was only in the relations between the factors to adherence and metabolic control. We therefore report the appropriate path coefficients and their Wald tests.
A mean-replacement strategy was used when less than 20% of the items for a particular measure were missing (M % per participant = .2, number of values replaced across all scales = 16). In all analyses, we utilized the Satorra–Bentler adjustment for non-normality. Due to the degree of non-normality for mothers (standard skewness = −13.56, standard kurtosis = 11.54) and fathers (standard skewness = 2.44, standard kurtosis = −4.30), the variables for frequency of help (FOH) were treated as ordinal variables. All other variables were untransformed and screened for the presence of multivariate outliers using SPSS version 16. We identified one case as a potential outlier, where the adolescent’s mother was uniquely not the primary caregiver (the Grandmother was). When we reran the analyses excluding this case, the analysis of adherence predicting HbA1c lost significance at an alpha level of .05. However, the overall pattern of the results of this analysis did not change, and retained significance at an alpha level of .06. As the precedent has been set in our previous studies to include this case in all analyses (e.g., Berg et al., 2009; Palmer et al., 2009), and there is no strong rationale for deviating from this prior precedent in this study, we chose to report analyses with the case included. All analyses, therefore, were conducted with the full sample available for each set of variables.
Results
Structure of Maternal Involvement
To identify the structure of maternal involvement, we conducted three confirmatory factor analyses (CFA). We began with a one-factor model, with each maternal involvement measure serving as an indicator of a global Maternal Involvement factor. Results indicated that this model was not a good fit to the data: Satorra-Bentler χ2 (14) = 142.45, p < .001; CFI = .68; IFI = .68; RMSEA = .20. Next, we tested a two-factor model, which distinguished between maternal Relationship Quality (communication, acceptance, and independence encouragement) and Behavioral Involvement (FOH, intrusive support, general monitoring, and diabetes-specific monitoring). Decisions regarding which items would serve as indicators of the latent factors were based on previous theoretical and empirical work. The two maternal involvement factors were allowed to covary. Results indicated that the two-factor model was also not a good fit to the data: Satorra-Bentler χ2 (13) = 58.77, p < .001; CFI = .89; IFI = .89; RMSEA = .12.
The final model (see Figure 1) was a three-factor model of maternal involvement consisting of a Relationship Quality Factor (communication, acceptance, and independence encouragement), a Behavioral Involvement Factor (FOH and intrusive support), and a Monitoring Factor (general monitoring and diabetes-specific monitoring). The model included covariances among the maternal involvement factors. The three-factor model was a good fit: Satorra-Bentler χ2 (11) = 11.65, p = .39; CFI = 1.0; IFI = 1.0; RMSEA = .02, and was a better fit than either the one-factor model (Satorra-Bentler scaled χ2 difference (3) = 1572.90, p < .001) or the two-factor model (Satorra-Bentler scaled χ2 difference (2) = 82.96, p < .001).
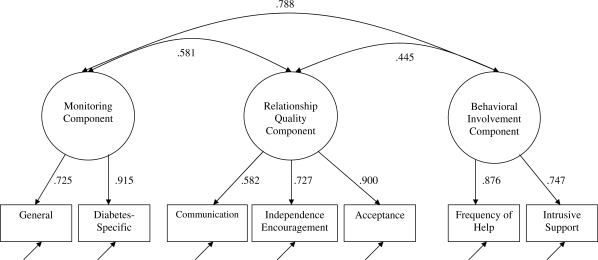
Structure of Paternal Involvement
Paralleling the analyses conducted for mothers’ involvement, we began with a CFA examining a one-factor model of paternal involvement. This one-factor model was not a good fit to the data: Satorra-Bentler χ2 (14) = 171.20, p < .001; CFI = .88; IFI = .85; RMSEA = .22. The two-factor model of paternal involvement, which included a Relationship Quality and Behavioral Involvement Factor, with the same variables loading on these factors as for the mothers’ model, was also not a good fit to the data: Satorra-Bentler χ2 (13) = 92.39, p < .001; CFI = .92; IFI = .92; RMSEA = .16. Finally, we examined the same three-factor model (see Figure 2) that was tested for mothers. The three-factor model of paternal involvement was an adequate fit to the data: Satorra-Bentler χ2 (11) = 57.79, p < .001; CFI = .95; IFI = .95; RMSEA = .14. Similar to results found for mothers, the three-factor model of paternal involvement was the best-fitting of the three models tested, significantly better than either the one-factor (Satorra-Bentler scaled χ2 difference (3) = 98.90, p < .001) or two-factor model (Satorra-Bentler scaled χ2 difference (2) = 31.49, p < .001).
Figure 2.
Results of the confirmatory factor analysis (CFA) conducted to identify the factor structure of paternal involvement. Significant correlations and standardized path coefficients (p < .05) are presented in the figure
Link of Parental Involvement to Diabetes Outcomes
Maternal Models
In the first set of structural models, we examined the associations between the three components of maternal involvement (relationship quality, monitoring, and behavioral involvement) and adolescents’ adherence. First, we examined each factor’s individual effect on adherence (fixing the other factors’ paths to adherence to zero). Results of these models are presented in Table I. Each of the maternal involvement factors (relationship quality, behavioral involvement, and monitoring) was positively and significantly associated with adherence. Second, we examined the combined effect of the three factors on adherence. When taken together, the three factors accounted for a significant proportion of the variance in adherence (Satorra-Bentler scaled χ2 difference (3) = 125.87, p < .001), although only mothers’ monitoring was a unique predictor of adolescents’ adherence.
Table I.
Results of Structural Analyses to Examine the Association between Parental Involvement and Diabetes Outcomes
| Adolescents' adherence behavior |
Adolescents' metabolic control (HbA1c) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Maternal involvement |
Paternal involvement |
Maternal involvement |
Paternal involvement |
|||||
| Models | ba | R2 | ba | R2 | ba | R2 | ba | R2 |
| Affective-only | – | 0.225 | – | 0.182 | – | 0.023 | – | 0.074 |
| Relationship quality | 0.474* | – | 0.426* | – | −0.151* | – | −0.273* | – |
| Monitoring-only | – | 0.316 | – | 0.148 | – | 0.012 | – | 0.104 |
| Monitoring component | 0.562* | – | 0.385* | – | −0.110 | – | −0.323* | – |
| Instrumental-only | – | 0.047 | – | 0.064 | – | 0.000 | – | 0.061 |
| Behavioral involvement | 0.216* | – | 0.254* | – | 0.018 | – | −0.247* | – |
| Full model | – | 0.364 | – | 0.262 | – | 0.033 | – | 0.119 |
| Relationship quality | 0.107 | – | 0.277* | – | −0.104 | – | −0.085 | – |
| Monitoring | 0.619* | – | 0.548* | – | −0.123 | – | −0.388* | – |
| Behavioral involvement | −0.205 | – | −0.396* | – | 0.120 | – | 0.143 | – |
aPath coefficients are presented in standardized units; *p < .05.
In the second set of structural models, we examined associations between maternal involvement and HbA1c (see Table I). When examined individually, only higher relationship quality was associated with better (lower) HbA1c. When examined together, none of the factors was uniquely associated with HbA1c. Results suggested that the three maternal involvement factors did not explain a significant amount of variation in adolescents’ metabolic control (Satorra-Bentler scaled χ2 difference (3) = 4.12, p = .25).
Paternal Models
In the first set of structural models for adolescents’ reports on fathers, we examined the association between the three components of paternal involvement and adolescents’ adherence (see Table I). Each of the paternal involvement factors (relationship quality, behavioral involvement, and monitoring) was individually associated with better adherence. When examined simultaneously, fathers’ relationship quality and monitoring were both uniquely associated with better adherence, whereas fathers’ behavioral involvement was associated with poorer adherence. Analyses suggested that the three paternal involvement factors explained a significant amount of variation in adolescents’ adherence (Satorra-Bentler scaled χ2 difference (3) = 42.96, p < .001).
In the final set of structural models, we examined the association between paternal involvement and HbA1c (see Table I). All three paternal involvement factors were individually associated with better (lower) HbA1c. When taken together, only fathers’ Monitoring was uniquely associated with HbA1c. Results indicated that the three parental involvement factors accounted for a significant amount of variation in adolescents’ metabolic control (Satorra-Bentler χ2 difference (3) = 22.77, p < .001).
Discussion
The results of this study suggest that parental involvement in adolescents’ diabetes is not a single, unidimensional construct, but rather is comprised of three separate, yet related, latent factors of Relationship Quality, Behavioral Involvement, and Monitoring, consistent with empirical investigations within the Pediatric and Developmental Psychology literatures (Berg et al., 2009; Dishion & McMahon, 1998; Ellis et al., 2007). These findings are important for family assessment in that they suggest that parental behavior constructs, although related, are not synonymous; parental involvement should be assessed using multidimensional, multifaceted approaches involving multiple measures (Dishion & McMahon, 1998; Ellis et al., 2007).
Mothers’ and fathers’ involvement were best described by the same three factor model, which supports the idea that mothers and fathers may be more similar than different in their parental involvement The three-factor model did meet the most fundamental form of factorial invariance (i.e., configural), supporting further comparisons of mothers and fathers (Widaman & Reise, 1995). However, the current findings are only a beginning step toward understanding mother and father similarities. Other aspects of parenting (e.g., whether the methods for the attainment of knowledge of adolescents’ diabetes management—self-disclosure, etc.—matter) remain underinvestigated empirically, particularly in terms of studies involving fathers (Marsiglio, Day, & Lamb, 2000). Therefore, additional work that examines similarities and dissimilarities of mothers’ and fathers’ parenting behaviors remains warranted.
The extent to which these forms of parental involvement were uniquely associated with diabetes outcomes differed across mothers and fathers. For both perceptions of mothers’ and fathers’ involvement, all three factors individually predicted better adherence. The same picture emerged when linking fathers’ involvement and metabolic control. When entered together, both Mothers’ Relationship Quality and Monitoring predicted better adherence; only Relationship Quality uniquely predicted metabolic control. When considered together, fathers’ Relationship Quality and Monitoring predicted better adherence, but Behavioral Involvement was associated with poorer adherence. For metabolic control, only fathers’ monitoring were uniquely predictive of better metabolic control. The results for behavioral involvement most likely reflect the overlap that it has with the other components of involvement. There are two possible explanations for the unexpected negative association between fathers’ behavioral involvement and adherence: (1) once relationship quality and monitoring are taken into account, behavioral involvement may be somewhat detrimental for adherence, consistent with the notions of intrusive or psychological control being harmful for positive youth outcomes (Barber, 1996; Wiebe et al., 2005) or (2) given the cross-sectional nature of our findings, fathers may have increased their behavioral involvement in response to adolescents’ poor adherence.
While prior Pediatric Psychology research has established the importance of both acceptance and monitoring to disease management success, few researchers have attempted to examine simultaneously the connections of different forms of parental involvement to adherence and metabolic control (Ellis et al., 2007). When accounting for the shared variance between measures of parental involvement in the current study, we found that adolescents’ reports of both mother and father monitoring were uniquely predictive of adherence, with fathers’ monitoring also predicting better metabolic control. Adolescents’ perceptions of the quality of the relationship with their fathers were uniquely important for understanding adherence. Although the diabetes literature has frequently focused on parental involvement in the form of behavioral involvement (who is responsible for diabetes management, Laffel et al., 2003), prior findings may partially reflect the variance behavioral involvement shares with the quality of the relationship and monitoring. These results have important implications for the assessment of family functioning in pediatric populations and strongly indicate the value of taking a more multidimensional approach to the assessment of parenting behaviors.
The broader developmental literature would lead us to predict that the components of parental involvement identified in this study are important across adolescence and into emerging adulthood (Aquilino, 2006). However, the current findings—coupled with prior research showing the frequency of parental behavioral involvement decreases with increasing development of children and adolescence (Palmer et al., 2004, Wysocki et al., 1996)—suggests that in late adolescence and emerging adulthood the importance of Behavioral Involvement for diabetes management may diminish.
The results of this study should be interpreted in the context of some limitations. First, analyses of the structure of parental involvement are necessarily limited by the measures that are included in the investigation. Caution must be exercised in the interpretation of our Behavioral Involvement factor as we did not include a more traditional measure of who is taking responsibility for specific diabetes tasks (e.g., Diabetes Responsibility and Conflict Scale: Rubin, Young-Hyman, & Peyrot, 1989). Had our study included measures of psychological control or overprotection, additional factors may have emerged. Second, cross-sectional relationships between factors of parental involvement and diabetes outcomes cannot be used to address directions of causality. Our ongoing longitudinal work will be able to address whether different forms of parental involvement predict subsequent diabetes outcomes and/or are a response to poor versus good management. Third, our current results are drawn from adolescents’ reports and do not include parents’ reports. We acknowledge that parents’ perspectives could differ from those of their children (Palmer et al., 2004). Finally, the sample consisted of primarily Caucasian and middle-class individuals. Further investigations using more diverse samples are needed before generalizations of these findings can be made.
The current study addressed both conceptual and empirical questions regarding the structure of parental involvement in a sample of adolescents struggling with the chronic illness of type 1 diabetes. The results indicated that parental involvement from adolescents’ perspectives reflects a multidimensional construct. Future attempts to increase parental involvement will benefit from a consideration of its multidimensional nature, by targeting ways to increase overall Relationship Quality (Wysocki et al., 2006), Behavioral Involvement (Anderson, Brackett, Ho, & Laffel, 2000), and Monitoring. Such a multi-pronged approach at increasing parental involvement may confer additional benefits to adolescents’ diabetes management. Similar advantages to utilizing a multifaceted approach to assessment may be possible for enhancing the understanding of additional chronic medical conditions in Pediatric Psychology.
Funding
National Institute of Diabetes and Digestive and Kidney Diseases [Grant Number R01DK063044 to D.W. (PI) and C.B. (co-PI)].
Conflicts of interest: None declared.
Acknowledgements
We thank the families who participated, the staff of the Utah Diabetes Center and Michael Swinyard’s practice as well as the additional members of the ADAPT team (David Donaldson, Katie Fortenberry, Carol Foster, Donna Gelfand, Hai Le, Rob Lindsay, Jenni McCabe, Mary Murray, Jordan Pyper, Marie Simard, Nathan Story, and Michael Swinyard). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. Portions of this work were presented at the Midwest Conference on Pediatric Psychology, University of Kansas, Kansas City, MO in April, 2009.
References
- Alderfer M, Fiese B, Gold JI, Cutuli JJ, Holmbeck GN, Goldbeck L, et al. Evidence-based assessment in Pediatric Psychology: Family measures. Journal of Pediatric Psychology. 2008;33:1046–1061. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- America Diabetes Association. Standards of medical care in Diabetes—2007. Diabetes Care. 2007;30(Suppl 1):S1–S41. [Google Scholar]
- Anderson BJ, Auslander W, Jung K, Miller J. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15(4):477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Anderson BJ, Brackett J, Ho J, Laffel L. MB. An intervention to promote family teamwork in diabetes management tasks: Relationships among parental involvement, adherence to blood glucose monitoring, and glycemic control in youths with type 1 diabetes. In: Drotar Dennis., editor. Promoting adherence to medical treatment in childhood chronic illness. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 347–365. [Google Scholar]
- Anderson BJ, Ho J, Bracket J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: Relationships to blood-glucose monitoring, adherence, and metabolic control in young adolescents with IDDM. Journal of Pediatrics. 1997;130:257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- Aquilino WS. Family relationships and support systems in emerging adulthood. In: Arentt JJ, Tanner JL, editors. Emerging adults in America: Coming of age in the 21st Century. Washington, D.C: American Psychological Association; 2006. pp. 193–217. [Google Scholar]
- Armsden GC, Greenberg MT. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence. 1987;16:427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- Barber BK. Parental psychological control: Revisiting a neglected construct. Child Development. 1996;67:3296–3319. [PubMed] [Google Scholar]
- Bentler PM. EQS structural equations program, Version 6.1. Encino, CA: Multivariate Software; 2005. [Google Scholar]
- Berg CA, Butler JM, Osborn P, King G, Palmer DL, Butner J, et al. The role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 Diabetes. Diabetes Care. 2008;31:678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- Berg CA, Skinner M, Ko K, Butler JM, Palmer DL, Butner J, et al. The fit between stress appraisal and dyadic coping in predicting perceived coping effectiveness for adolescents with type 1 diabetes. Journal of Family Psychology. 2009;23:521–530. doi: 10.1037/a0015556. [DOI] [PubMed] [Google Scholar]
- Bernier A, Larose S, Whipple N. Leaving home for college: A potentially stressful event for adolescents with preoccupied attachment patterns. Attachment & Human Development. 2005;7:171–185. doi: 10.1080/14616730500147565. [DOI] [PubMed] [Google Scholar]
- Brown BB, Mounts N, Lamborn SD, Steinberg LS. Parenting practices and peer group affiliation in adolescence. Child Development. 1993;64:467–482. doi: 10.1111/j.1467-8624.1993.tb02922.x. [DOI] [PubMed] [Google Scholar]
- Bumpus MF, Crouter AC, McHale SM. Linkages between negative work-to-family spillover and mothers’ and fathers’ knowledge of their young adolescents’ daily lives. The Journal of Early Adolescence. 2006;26(1):36–59. [Google Scholar]
- Collins WA, Russell G. Mother–child and father–child relationships in middle childhood and adolescence: A developmental analysis. Developmental Review. 1991;11:99–136. [Google Scholar]
- Day RD, Lewis C, O’Brien M, Lamb ME. Father and father involvement: Emerging constructs and theoretical orientations. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child and Family Psychology Review. 1998;1(1):61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Podolski C-L, Frey M, Narr-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology. 2007;32(8):907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin TN, Naar-King S, Frey MA. Toward conceptual clarity in a critical parenting construct: Parental monitoring in youth with chronic illness. Journal of Pediatric Psychology. 2008;33:799–808. doi: 10.1093/jpepsy/jsn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein S. The Mother–Father Peer Scale. Unpublished manuscript; 1983. [Google Scholar]
- Fan X, Chen M. Parental involvement and students’ academic achievement: A meta-analysis. Educational Psychology Review. 2001;13(1):1–22. [Google Scholar]
- Hawkins A, Palkovitz R. Beyond ticks and clicks: The need for more diverse and broader conceptualizations and measures of father involvement. The Journal of Men’s Studies. 1999;8(1):11–32. [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Holmbeck G. A developmental perspective on adolescent health and illness: An introduction to the special issues. Journal of Pediatric Psychology. 2002;27(5):409–416. doi: 10.1093/jpepsy/27.5.409. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler P. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB, Santiago JV. I get by with a little help from my family and friends: Adolescents’ support for diabetes care. Journal of Pediatric Psychology. 1995;20(4):449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Follansbee D, Skyler JS. Developmental and behavioral aspects of diabetes management in youngsters. Children’s Health Care. 1990;19:132–139. [Google Scholar]
- La Greca AM, Swales T, Klemp S, Madigan S. Self care behaviors among adolescents with diabetes. Proceedings of the Ninth Annual Sessions of the Society of Behavioral Medicine, Boston. 1988:A42. [Google Scholar]
- Laffel L. MB, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. Journal of Pediatrics. 2003;142(4):409–416. doi: 10.1067/mpd.2003.138. [DOI] [PubMed] [Google Scholar]
- Marsh H, Balla J, McDonald R. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychological Bulletin. 1988;103(3):391–410. [Google Scholar]
- Marsiglio W, Day R, Lamb M. Exploring fatherhood diversity: Implications for conceptualizing father involvement. Marriage & Family Review. 2000;29(4):269–293. [Google Scholar]
- Palmer DL, Berg CA, Wiebe DJ, Beveridge R, Korbel C, Upchurch R, et al. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29(1):35–46. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- Palmer DL, Berg CA, Butler J, Fortenberry K, Murray M, Lindsay R, et al. Mothers’, fathers’, and children’s perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology. 2009;34:95–104. doi: 10.1093/jpepsy/jsn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz EM, Eaton MM. Maternal intrusive support in the academic context: Transactional socialization processes. Developmental Psychology. 2001;37(2):174–186. doi: 10.1037/0012-1649.37.2.174. [DOI] [PubMed] [Google Scholar]
- Rubin RR, Young-Hyman D, Peyrot M. Parent–child responsibility and conflict in diabetes care. Diabetes Care. 1989;38:28A. [Google Scholar]
- Seiffge-Krenke I. ‘Come on, say something, Dad!’: Communication and coping in fathers of diabetic adolescents. Journal of Pediatric Psychology. 2002;27(5):439–450. doi: 10.1093/jpepsy/27.5.439. [DOI] [PubMed] [Google Scholar]
- Widaman K, Reise S. Exploring the measurement invariance of psychological instruments: Applications in the substance use domain. In: Bryant KJ, Windle M, West SG, editors. The science of prevention: Methodological advances from alcohol and substance abuse research. Washington, DC: American Psychological Association; 1995. pp. 281–324. [Google Scholar]
- Wiebe DJ, Berg CA, Palmer DL, Korbel C, Beveridge R, Upchurch R, et al. Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30(2):167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology. 2006;31(5):501–511. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. Journal of Pediatric Psychology. 2006;31:928–38. doi: 10.1093/jpepsy/jsj098. [DOI] [PubMed] [Google Scholar]