Abstract
OBJECTIVES:
This study aimed to determine the knowledge about asthma and the prevalence, disclosure and evaluation of the use of complementary and alternative medicine (CAM) among asthmatic patients.
METHODS:
This cross-sectional study was conducted on 95 patients diagnosed with asthma in a primary healthcare centre in Kuala Lumpur, Malaysia using a self-administered questionnaire.
RESULTS:
Ninety-five patients with a mean age of 47.06 years (±12.8) participated, the majority were female (66.7%), Malay (72.6%). The prevalence of ever-CAM use was 61.1%. The non-ever-CAM users’ mean age was 51±13.9 years while the ever-CAM users’ mean age was 44.5 ±11.5 years (P = 0.021). Sixty-three females (66.8%) used CAM compared to 14 males (43.8%) (P = 0.014). Thirty-six (62.1%) CAM users had not discussed use of CAM with their doctors. The main reason of non-disclosure was the doctor never asked (55.6%), and the main sources of information about CAM were family and relatives (46.6%). There was no significant difference between use of CAM and knowledge about asthma. The majority of asthmatic patients used rubs (39%), foods (16.9%) and herbs (16.9%). About 76% of asthmatic patients perceived CAM as good for their disease management. On linear multiple regression, Malay race (P = 0.026) and female gender (P = 0.006) were significant predictors of CAM use.
CONCLUSION:
Use of CAM among asthmatic patients is relatively high, particularly among females. The majority of asthmatic patients valued the use of CAM. Non-disclosure was high in this study. Health education of asthmatic patients about CAM is highly recommended.
Keywords: Asthma, complementary and alternative medicine, disclosure, Malaysia
Use of Complementary and alternative medicine (CAM) has gained worldwide popularity in the last few decades.[1–3] This can be attributed to increased public awareness about wellness and disease prevention. In addition, various philosophical modalities of CAM have attracted the psychological views of the public towards holistic medicine.[4]
Patients with chronic diseases including asthma, have a greater tendency to use CAM as they are more concerned about the adverse effects of conventional medicine, dissatisfaction with their medical care, particularly communication with doctors,[5] as well as their subjective feeling of health improvement with use of CAM.[6] The prevalence of the use of CAM among adult asthmatic patients varies from 4-79%.[7] In Asia, little is known about the prevalence of the use of CAM among asthmatic patients. Ng et al.[8] reported a prevalence rate of 27.2% in Singapore and Al Moamary[9] reported a rate of 30% in Saudi Arabia. In Malaysia, a study conducted in 2004[10] reported 41% CAM use among asthmatic patients. On the other hand, patients’ disclosure of the use of CAM to their doctors remains poor[11] despite the increased CAM use and awareness among general practitioners.[12]
The Malaysian population is a mixture of Malay (58%), Chinese (26%), Indian (7%), and other minor ethnic groups (9%).[13] The use of CAM in the form of biologically-based therapy including herbal use for health problems in Malaysia was 88.9%[3] and CAM use among patients with chronic disease was 63.9%.[14] The high rates of use of CAM in Malaysia raise the concern regarding the use of CAM among asthmatic patients, as to what are the sources of information and communication for their healthcare providers. The aim of this study was to determine the prevalence of the use of CAM, knowledge about asthma, common modalities, disclosure, and sources of information about CAM among adult asthmatic patients in primary healthcare clinics.
Methods
Participants
This cross-sectional study was conducted on 95 patients diagnosed with asthma in the outpatient clinic in Primary Health Care Centre of General Hospital of Kuala Lumpur during the period from July 2009 to September 2009. The inclusion criteria were patients suffering from asthma for more than a year and aged more than 18 years.
Instrument
A pre-tested self-administered, 25-item questionnaire in English and Bahasa Malaysia was distributed to the participants. It composed of three parts; sociodemographic data, knowledge about the disease and CAM use including definition of CAM, modalities, sources of information, disclosure and general evaluation of use of CAM. The questionnaire defined CAM as any type of product or practice that was utilized to prevent or treat the asthma attack, which was not prescribed by the patient's healthcare provider. Knowledge was assessed by five questions (“true” or “false”) obtained from a previous study by Ho et al. (2003).[15]
Data collection
The questionnaire was distributed to the patients while they were in the waiting room to see their doctor. The covering letter described the intent of the study, conveyed assurance of anonymity, and emphasized that the patient's decision to complete or decline to complete the survey would not affect his/her healthcare quality in any way. Consent was obtained from the participants. The hospital and faculty committee approved the study. Questionnaires with at least 10% of items left incomplete were excluded from data analysis.
Statistical analysis
Analysis was done using Statistical Package of Social Sciences (SPSS) software, Version 17. Descriptive statistics were used for demographic characteristics and CAM information. Student's t-test and Chi square test were used in bivariate analysis. Simple logistic regression was used to calculate odds ratio for variables with more than two categories. Multiple logistic regression was used to identify the predictors.
Results
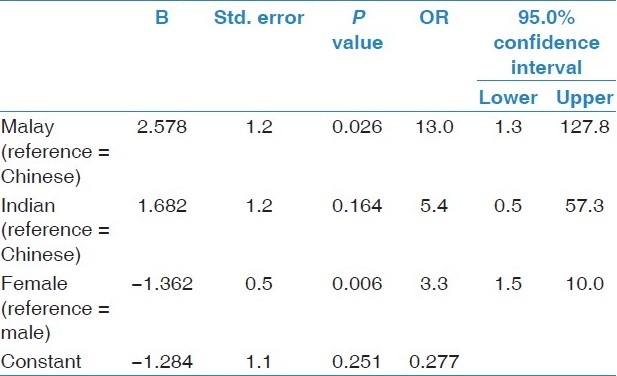
Ninety-five patients fulfilled the inclusion criteria. The mean age was 47.06 years (±12.8). There were 63 (66.3%) females and 32 (32.7%) males. The majority of the respondents were Malay (69, 72.6%), followed by Indian (20, 21.1%) and Chinese (6, 6.3%). Seventy-six (80%) participants had not completed their tertiary education while 19 (20%) had a university degree. The majority of the population had disease duration of more than two years (71.6%) [Table 1]. Fifty-eight (61.1%) respondents reported that they had used CAM at least once since the diagnosis of asthma. Forty-five (47.4%) respondents were still using CAM. The non-ever-CAM users’ mean age was 51 ± 13.9 years while the ever-CAM users′ mean age was 44.5 ± 11.5 years. This difference in age between the two groups was statistically significant (P = 0.021). The association between sociodemographic factors and use of CAM was assessed using Chi square test. Sixty-three females (66.8%) used CAM compared to 14 males (43.8%) (OR = 3.0, 95% CI 1.2-7.2, P = 0.014). No significant association was found with other sociodemographic factors [Table 2]. On multiple logistic regression, significant predictors of CAM use were female gender (OR = 3.3, 95% CI 1.5-10.0, P = 0.006) and Malay race (OR = 13.0, 95% CI 1.3-127.8, P = 0.026). The total model was significant ( P = 0.003) and accounted for 0.19 of the variance [Table 3].
Table 1.
Demographic characteristics of the study population
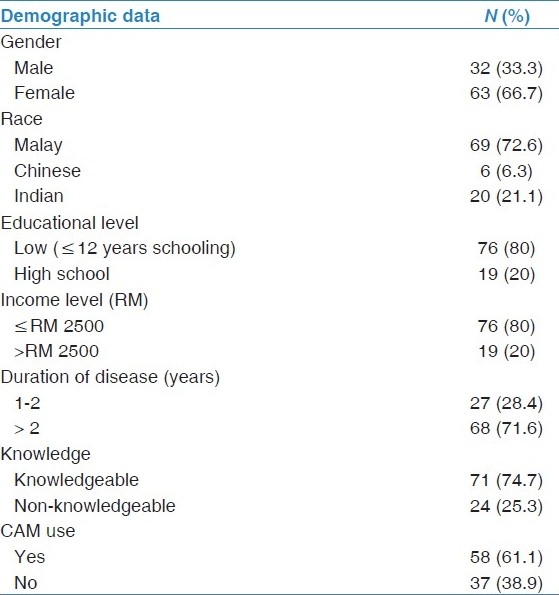
Table 2.
Association between sociodemographic variables and CAM use
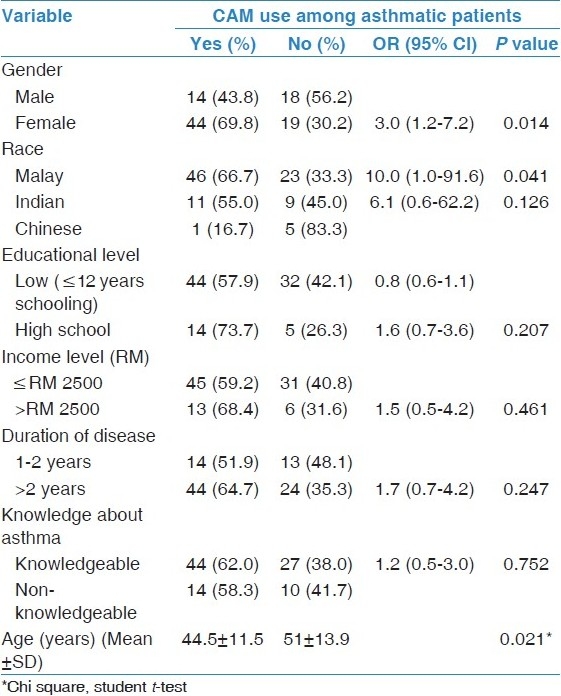
Table 3.
Multiple logistic regression, predictors of CAM use among asthmatic patients
CAM users who reported regularity on conventional treatment were 47 (81%) and CAM users with regular visit to clinic were 41 (71.1%). Thirty-six (62.1%) CAM users had not discussed use of CAM with their doctors. Regarding reasons of non-disclosure, 20 patients (55.6%) answered “the doctor never asked”, nine (25%) reported “they did not know they should”, while three (8.3%) answered “don’t think doctor knows about the topic” and three (8.3%) said “doctor would be dismissive”. Only one (2.8%) patient answered “not enough time during office visit”. There was no significant association between sociodemographic factors and disclosure of use of CAM and regularity on conventional treatment. The reasons given by asthmatic patients for the use of CAM were: “just to try” (24.1%), followed by “avoidance of side-effects” (22.4%) and “as emergency treatment (3.4%)” and “dissatisfaction with conventional care (3.4%)”. Figure 1 shows the reasons for the use of CAM in the study population.
Figure 1.
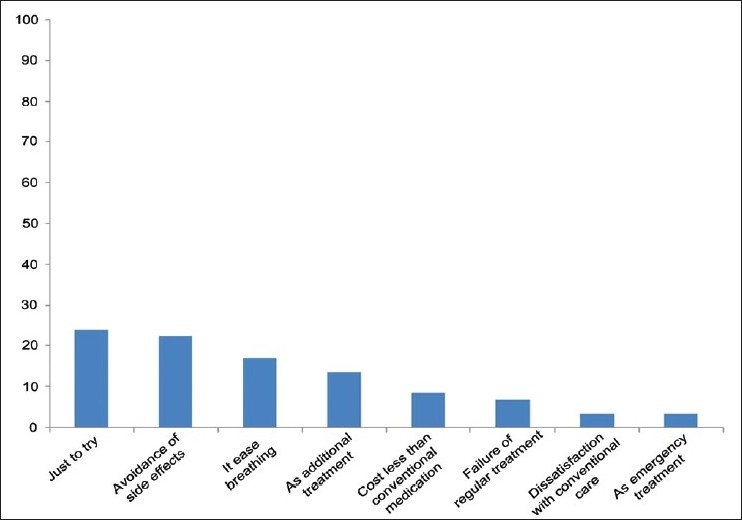
Asthmatic patients’ reasons for CAM use
The scores of the five questions about asthma knowledge were summed and recoded into two categories; knowledgeable and non-knowledgeable (median = 3 was used as the cutoff point). Of the total sample, 71 (74.7%) were knowledgeable about their disease. Among CAM users, 44 (62%) were knowledgeable. Among non-CAM users, there were 27 knowledgeable ones (38%). However, this difference was not statistically significant (OR = 1.16, 95% CI 0.45-2.98, P = 0.752).
Twenty-nine (50%) CAM users tried multiple modalities, while (50%) used only one modality. The commonest modality was the use of rubs such as oils and camphor followed by food or other nutritional supplements such as honey, fish oil, garlic, ginseng, Chinese and Indian herbs. The less common modality was manipulations including reflexology, cupping and massage. Figure 2 shows the different modalities of the use of CAM among asthmatic patients.
Figure 2.
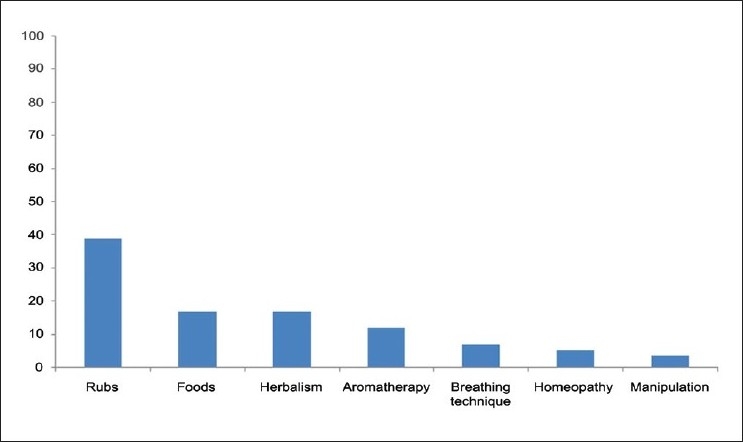
Modalities of CAM use among asthmatic patients
Regarding the source of information about CAM, family and relatives were the main source of information (46.6%) followed by friends (34.5%), media (10.3%) and healthcare providers including CAM practitioners (8.6%). Figure 3 shows the sources of information for CAM.
Figure 3.
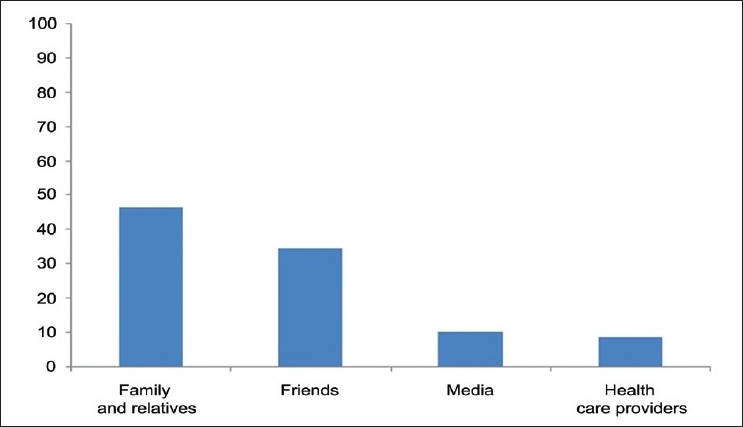
Sources of information for CAM use among asthmatic patients
The general patients’ evaluation about CAM showed that the majority of asthmatics (75.8%) valued CAM as good for their disease, while 24.2% of them reported no benefit of CAM for asthma.
Discussion
The findings of this study provide the prevalence and characteristics of ever-CAM use (61.1%) among adult asthmatic patients in primary care clinics in Kuala Lumpur, Malaysia. The CAM use among asthmatics (41%) reported by Mokhtar and Chan[10] in Malaysia was less than our results which can be attributed to the location of the study. The Mokhtar and Chan[10] study was conducted in Ipoh, Third largest city in Malaysia, while this study was conducted in Kuala Lumpur, the capital of Malaysia. Generally, the prevalence of Malaysian asthmatic patients was higher than other Asian countries.[8,9]
In this study, rubs were used by the majority of the study population (39.0%), followed by foods and herbalism (16.9% each). In the literature, the use of rub has been found to be common among Hispanic[16] and African-American asthmatic patients.[17]
The mean age of CAM users (44 years) was lower than non-CAM users (51 years). Conboy et al.[4] explained that younger people value the interaction and communication with CAM practitioners where the practitioner-patient interview takes longer and more detailed information is gathered compared to the doctor-patient interactions in primary care clinics, particularly government clinics.
In general, female gender had been associated with use of CAM in many studies.[18–20] Female asthmatic patients were also more likely to use CAM than men asthmatics in the UK[21] and Germany.[22] Our finding of this study supports the previous findings in the literature. There was no significant association in this study between use of CAM and sociodemographic factors (race, income and educational level) and knowledge in contrast to other studies. This might be due to our small sample size.[8,23]
The majority of CAM users in this study were influenced by family and relatives. Similarly, use of CAM has been strongly associated with a family influence[14,18] and cultural tradition.[24] Not surprisingly, healthcare providers have a low influence on asthmatic patients’ information about CAM since there was a high rate of non-disclosure among our population. Unlike asthmatic patients, diabetic and hypertensive CAM users in Malaysia reported that doctors were a main source of information about CAM.[14] Probably, diabetic and hypertensive patients’ concerns about the complications of their diseases make them talk openly to their health providers.
In this study, a high percentage of patients (62.1%) did not inform their doctors about use of CAM, a similar high rate of non-disclosure among asthmatic patients (81%) was reported by Mokhtar and Chan.[10] The importance of CAM disclosure to health providers is essential as doctors need to be informed in order to assess the patient's needs, compliance, efficacy of CAM, and more importantly to identify any potential drug interaction and adverse drug reaction.[24] The main reason for non-disclosure by asthmatic patients was “doctor never asked” (55.6%), while it was the third reason in a systemic review done by Robinson and McGairl.[11] The second reason in this study “didn’t know they should” (25%) was in agreement with the Robinson and McGairl[11] review study. Fortunately, asthmatic patients did not have a negative attitude about their health providers as the reason “doctor would be dismissive” was low in comparison to a previous study conducted by Lim et al.[18]
This study found that dissatisfaction with conventional treatment was uncommon, asthmatic patients used CAM as a complementary rather than alternative medicine as most of our population complied with their medication regularly while perceiving CAM use as helpful for disease management. Even though the efficacy of the use of CAM has not been established, there are optimistic findings in regard with the safety and efficacy of the use of CAM in asthma.[25]
Limitations
The results of this study were limited by the small sample size and location. The majority of our population showed predominance of one ethnic group with low income and low educational level. Another limitation of this study is its quantitative approach and its close-ended questionnaire. This approach cannot explore in-depth information and cannot provide better understanding of patients’ attitude towards CAM.
Conclusion and Recommendation
CAM use among asthmatic patients is relatively high, particularly among females. They used it as complementary rather than alternative medicine. The majority of the asthmatic patients valued the use of CAM. Non-disclosure was a major concern in this study. The main reason for non-disclosure was that doctors and healthcare providers did not ask their patients about use of CAM. This finding indicates low awareness about use of CAM among healthcare providers and/or their ignorance of this important issue. Awareness about the use of CAM should be raised among healthcare providers and they should be encouraged to be involved in open communication with their patients about the use of CAM. A wide survey in the country, including primary care, private clinics as well as CAM clinics would probably explore more information about the use of CAM among asthmatic patients in Malaysia. Together with a quantitative approach, a qualitative approach is recommended as it would explore a greater depth of information about this issue in Malaysia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Featherstone CD, Godden S, Selvaraj M, Emslie M, Took-Zozaya EM. Characteristics associated with reported CAM use in patients attending six GP practices in the Tayside and Grampian regions of Scotland: A survey. Complement Ther Med. 2003;11:168–76. doi: 10.1016/s0965-2299(03)00067-0. [DOI] [PubMed] [Google Scholar]
- 2.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 3.Siti ZM, Tahir A, Ida Farah A, Ami Fazlin SM, Sondi S, Azman AH, et al. Use of traditional and complementary medicine in Malaysia: A baseline study. Complement Ther Med. 2009;17:292–9. doi: 10.1016/j.ctim.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Conboy L, Kaptchuk TJ, Eisenberg DM, Gottlieb B, Acevedo-Garcia D. The relationship between social factors and attitudes toward conventional and CAM practitioners. Complement Ther Clin Pract. 2007;13:146–57. doi: 10.1016/j.ctcp.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Vincent C, Furnham A. Why do patients turn to complementary medicine? An empirical study. Br J Clin Psychol. 1996;35:37–48. doi: 10.1111/j.2044-8260.1996.tb01160.x. [DOI] [PubMed] [Google Scholar]
- 6.Abadoglu O, Cakmak E, Kuzucu Demir S. The view of patients with asthma or chronic obstructive pulmonary disease (COPD) on complementary and alternative medicine. Allergol Immunopathol (Madr) 2008;36:21–5. doi: 10.1157/13115667. [DOI] [PubMed] [Google Scholar]
- 7.Slader CA, Reddel HK, Jenkins CR, Armour CL, Bosnic-Anticevich SZ. Complementary and alternative medicine use in asthma: Who is using what? Respirology. 2006;11:373–87. doi: 10.1111/j.1440-1843.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 8.Ng TP, Wong ML, Hong CY, Koh KT, Goh LG. The use of complementary and alternative medicine by asthma patients. QJM. 2003;96:747–53. doi: 10.1093/qjmed/hcg121. [DOI] [PubMed] [Google Scholar]
- 9.Al Moamary MS. Unconventional therapy use among asthma patients in a tertiary care center in Riyadh, Saudi Arabia. Ann Thorac Med. 2006;3:48–51. doi: 10.4103/1817-1737.39636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mokhtar N, Chan SC. Use of complementary medicine amongst asthmatic patients in primary care. Med J Malaysia. 2006;61:125–7. [PubMed] [Google Scholar]
- 11.Robinson A, McGrail MR. Disclosure of CAM use to medical practitioners: A review of qualitative and quantitative studies. Complement Ther Med. 2004;12:90–8. doi: 10.1016/j.ctim.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Maha N, Shaw A. Academic doctors’ views of complementary and alternative medicine (CAM) and its role within the NHS: An exploratory qualitative study. [Last cited on 2010 Nov 15];BMC Complement Altern Med [internet] 2007 May 7;17 doi: 10.1186/1472-6882-7-17. Available from: http://www.biomedcentral.com/content/pdf/1472-6882-7-17 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Encyclopedia of the Nations [internet] [Last cited on 2010 Dec 2nd]. Available from: http://www.nationsencyclopedia.com/economies/Asia-and-the-Pacifi c/Malaysia.html .
- 14.Hasan SS, Ahmed SI, Bukhari NI, Loon WC. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement Ther Clin Pract. 2009;15:152–7. doi: 10.1016/j.ctcp.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Ho J, Bender BG, Gavin LA, O’Connor SL, Wamboldt MZ, Wamboldt FS. Relations among asthma knowledge, treatment adherence, and outcome. J Allergy Clin Immunol. 2003;111:498–02. doi: 10.1067/mai.2003.160. [DOI] [PubMed] [Google Scholar]
- 16.Reznik M, Ozuah P, Franco K, Cohen R, Motlow F. Use of complementary therapy by adolescents with asthma. Arch Pediatr Adolesc Med. 2002;156:1042–4. doi: 10.1001/archpedi.156.10.1042. [DOI] [PubMed] [Google Scholar]
- 17.George M, Brick K, Hufford DJ, Jemmott LS, Weaver TE. Beliefs about asthma and complementary and alternative medicine in low-income inner-city African-American adults. J Gen Intern Med. 2006;21:1317–24. doi: 10.1111/j.1525-1497.2006.00624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim MK, Sadarangani P, Chan HL, Heng JY. Complementary and alternative medicine use in multiracial Singapore. Complement Ther Med. 2005;13:16–24. doi: 10.1016/j.ctim.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Loera JA, Reyes-Ortiz C, Kuo YF. Predictors of complementary and alternative medicine use among older Mexican Americans. Complement Ther Clin Pract. 2007;13:224–31. doi: 10.1016/j.ctcp.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ben-Arye E, Karkabi S, Shapira C, Schiff E, Lavie O, Keshet Y. Complementary Medicine in the primary care setting: Results of a survey of gender and cultural patterns in Israel. Gend Med. 2009;6:384–97. doi: 10.1016/j.genm.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Ernst E. Complementary therapies for asthma: What patients use? J Asthma. 1998;35:667–71. doi: 10.3109/02770909809048969. [DOI] [PubMed] [Google Scholar]
- 22.Schäfer T. Epidemiology of complementary alternative medicine for asthma and allergy in Europe and Germany. Ann Allergy Asthma Immunol. 2004;93:S5–10. doi: 10.1016/s1081-1206(10)61481-0. [DOI] [PubMed] [Google Scholar]
- 23.Kumar D, Bajaj S, Mehrotra R. Knowledge, attitude and practice of complementary and alternative medicines for diabetes. Public Health. 2006;120:705–11. doi: 10.1016/j.puhe.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Sidora-Arcoleo K, Yoos HL, Kitzman H, McMullen A, Anson E. Don’t ask, don’t tell: Parental nondisclosure of complementary and alternative medicine and over-the-counter medication use in children's asthma management. J Pediatr Health Care. 2008;22:221–9. doi: 10.1016/j.pedhc.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li XM, Brown L. Efficacy and mechanisms of action of traditional Chinese medicines for treating asthma and allergy. J Allergy Clin Immunol. 2009;123:297–06. doi: 10.1016/j.jaci.2008.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]


