Abstract
It is now established that pathological transactive response DNA-binding protein with a Mr of 43 kD (TDP-43) on sodium dodecyl sulfate-polyacrylamide gel electrophoresis is the major disease protein in amyotrophic lateral sclerosis (ALS) and frontotemporal lobar degeneration (FTLD) with ubiquitin-positive inclusions (now known as FTLD-TDP). In fact, the discovery of pathological TDP-43 solidified the idea that these disorders are multi-system diseases and this led to the concept of a TDP-43 proteinopathy as a spectrum of disorders comprised of different clinical and pathological entities extending from ALS to ALS with cognitive impairment/dementia and FTLD-TDP without or with motor neuron disease (FTLD-MND). These align along a broad disease continuum sharing similar pathogenetic mechanisms linked to pathological TDP-43. We here review salient findings in the development of a concept of TDP-43 proteinopathy as a novel group of neurodegenerative diseases similar in concept to α-synucleinopathies and tauopathies.
Keywords: amyotrophic lateral sclerosis, frontotemporal lobar degeneration, multi-system disease, proteinopathy, transactive response DNA-binding protein with a Mr of 43 kD (TDP-43)
INTRODUCTION
With the advent of new technologies in medicine and related biomedical sciences, concepts of neurodegenerative diseases continue to be refined, and novel disease entities emerge. For example, based on advances over the past 25 years, we now know that nearly all neurodegenerative disease are protein misfolding disorders characterized by pathological central nervous system (CNS) protein aggregates, alterations in the solubility and metabolism of corresponding disease proteins, and mutations in genes that encode major disease proteins of familial disorders and their sporadic counterparts, including the genes encoding tau, amyloid-β, α-synuclein, and others. The phenotypic features of these diseases are highly variable, but correlations between genetic abnormalities, clinical features and underlying neuropathology, as well as mechanisms of neurodegeneration, are recognized. However, we are far from understanding the precise relationships between genotypes and disease phenothypes in common as well as uncommon disorders such as Alzheimer’s disease (AD) and Parkinson’s disease (PD) in addition to frontotemporal degeneration (FTD) and amyotrophic lateral sclerosis (ALS). In this review, we summarize recent advances in ALS and FTD that have resulted from development of the concept that these disorders represent a spectrum of manifestations of TDP-43 proteinopathy that are so-named because they are linked to pathological abnormalities in the nuclear protein known as the human immunodeficiency virus type 1 transactive response DNA-binding protein with a Mr of 43 kD (TDP-43) on sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) which is commonly referred now to as TDP-43.
Historically, amyotrophic lateral sclerosis (ALS) has been considered to be the prototypical pyramidal motor system neurodegenerative disease. The presence of additional features has usually been considered to exclude the diagnosis of classical ALS, and therefore ALS with additional features was referred to as an ALS-Plus syndrome according to El Escorial clinical diagnostic criteria.1,2 In fact, the 1998 El Escorial revised criteria for a diagnosis of ALS include: (i) evidence of lower motor neuron (LMN) degeneration by clinical, electrophysiological or neuropathologic examination; (ii) evidence of upper motor neuron (UMN) degeneration by clinical examination; and (iii) progressive spread of symptoms or signs within a region or to other regions, as determined by history or examination. Further, these criteria included the absence of: (i) electrophysiological and pathological evidence of other disease processes that might explain the signs of LMN and/or UMN degeneration; and (ii) neuroimaging evidence of other disease processes, which might explain the observed clinical and electrophysiological signs.1 In terms of neuropathology, degeneration of the UMN and LMN with motor neuron cytoplasmic inclusions immunoreactive for ubiquitin and corticospinal tract degeneration are considered to be diagnostic for ALS.3 The spectrum of inclusions found in ALS is heterogeneous, morphologically including: (i) filamentous aggregations/threads/skeins; (ii) small granules and Bunina bodies; and (iii) larger frayed, basophilic, and Lewy body-like inclusions. However, besides this diagnostic LMN and UMN degeneration, ubiquitin-inclusion pathology had increasingly been described in a more widespread distribution, such as the ubiquitin-positive neuronal inclusions found in the neocortex or hippocampus, especially in association with dementia (ALS-D).4,5 The concept of ALS goes back to Jean-Martin Charcot (1825–1893), who described this disorder more than 100 years ago, which is the most prevalent neurodegenerative motor neuron disease (MND), while the concept of FTD emerged at about the same time with a report of Arnold Pick (1851–1924), who described cases of a dementia with severe, circumscribed atrophy of frontotemporal regions, now known as Pick’s disease (PiD), which is one of the most widely recognized forms of FTD. Cases with dementia in which argyrophilic intraneuronal inclusions (Pick bodies) and ballooned neurons are seen in the post mortem brain solidified the concept of PiD because these lesions distinguished these patients from those with other types of dementias such asAD, which was first reported by Alois Alzheimer (1864–1915) to be a cognitive disorder associated with neurofibrillary tangles and amyloid plaques. However, it became increasingly clear that many patients with PiD-like clinical features did not show neuropathological evidence of PiD, and a plethora of alternative terms were used for these non-PiD and non-AD dementias.6–8 Not surprisingly, the classification of FTD, which also is referred to as frontotemporal lobar degeneration (FTLD), has been fraught with controversy due in large part to substantial gaps in the understanding of the cellular and molecular neuropathological correlates of the clinical manifestations of FTLDs. As the clinical manifestations of different FTLD variants do not enable prediction of the neuropathological or genetic basis of the dementia in a given patient, it was recommended that the clinically diverse variants of FTLD should be referred to collectively as FTLD to emphasize the shared clinical features enabling differentiation from other dementias during life, but without making assumptions about their neuropathological correlates or underlying disease processes.9 More recent evidence on the convergence of the different clinical syndromes in both FTLDs with tau pathology (i.e., tauopathies which account for ~45% of FTLD cases) or without associated tau pathology during the disease course supports this notion.10,11 Moreover, “ubiquitin only dementia” has been shown to account for ~50% of FTLD cases, and FTLD-U is distinguished from FTLD tauopathies (i.e. FTLD-Tau) by the presence of frontotemporal degeneration and ubiquitin-positive, but tau- and α-synuclein-negative inclusions. The cardinal clinical features of all FTLD variants are non-amnestic cognitive impairments encompassing changes in social behavior often with disinhibition and language difficulties.10 Using ubiquitin and novel monoclonal antibodies generated from FTLD-U brains, at least four morphological subtypes of FTLD-U were identified based on the type and distribution of these ubiquitin-positive inclusions throughout the frontotemporal cortex and hippocampus.12,13 In 2006, the notion that pathological TDP-43 is involved in human disease was proposed when TDP-43 was discovered by Neumann et al. to be the major disease protein in FTLD-U (now known as FTLD-TDP), FTLD with MND (FTLD-MND) and ALS, suggesting a common pathogenesis linked to TDP-43 abnormalities in these disorders, which was rapidly confirmed by Arai et al.14,15
Thus, we recently proposed a classification scheme in which pathological TDP-43 is the major disease defining pathology in so-called primary TDP-43 proteinopathies, which mainly includes ALS, FTLD-TDP and their transition forms, while a second category of disorders includes neurodegenerative diseases wherein there is concomitant TDP-43 pathologies, and a third group comprises those neurodegenerative conditions with minor or no significant TDP-43 pathology.16 This scheme reflects the considerable overlap of clinicopathological features between all neurodegenerative diseases as reviewed elsewhere.17 Recently, detailed clinico-pathological studies on the whole spectrum of TDP-43-related neurodegeneration have become available, and have contributed to establishing the significance of pathological TDP-43 for ALS and FTLD-U.18 Here, we focus this review on the major TDP-43 proteinopathies.
BIOLOGY OF TDP-43
TDP-43 is a 414 amino acid nuclear protein encoded by the TARDBP gene on chromosome 1 (for reviews, see19–22). While the functions of TDP-43 are not yet completely understood, TARDBP was first identified as a gene encoding a 43 kD protein that binds to the transactivating responsive DNA sequence of human immunodeficiency virus type 1. Subsequently, TDP-43 was also shown to be involved in the splicing of the cystic fibrosis transmembrane conductance regulator gene, the apolipoprotein A-II gene and possibly others.20,22–30 TDP-43 is a highly conserved protein ubiquitously expressed in many tissues including the CNS where it is present in neuronal and glial nuclei and to a lesser extent in the cytoplasm. It contains two RNA-recognition motifs and a glycine-rich carboxy terminal region that may be required for exon skipping and splicing inhibitory activity as well as binding to other nuclear proteins. This is consistent with the finding that the carboxy terminal domain binds to several proteins of the heterogeneous nuclear ribonucleoprotein family involved in the biogenesis of mRNA. Other studies also identified TDP-43 as a multi-functional RNA binding protein involved in: (i) exon-skipping of cystic fibrosis transmembrane conductance regulator and apolipoprotein A-II genes;20,25,26 (ii) exon-inclusion of the survival of motor neuron gene;31 (iii) stabilization of low molecular weight neurofilament protein mRNA through a direct interaction with its 3′ untranslated region;29 and (iv) modulation of cyclin-dependent kinase 6 expression24,32 and microRNA biogenesis.33 TDP-43 has also been shown to bind to the proximal promoter of the mouse SP-10 gene (acrosomal vesicle protein 1), which is involved in spermatogenesis, thereby implicating TDP-43 in regulating its expression.23 Finally, other reported functions of TDP-43 include: (i) acting as scaffold for nuclear bodies (i.e., Gemini of coiled bodies) through interaction with survival of motor neuron protein;34 (ii) cell cycle regulation and apoptosis;24,32 and (iii) mRNA transport and regulation of local translation at synapses.30 Thus, the physiological functions of TDP-43 are diverse but incompletely characterized, and they likely involve the regulation of multiple biological processes through TDP-43 binding to DNA, RNA, and/or proteins.
CLINICO-PATHOLOGICAL CORRELATIONS IN THE MAJOR TDP-43 PROTEINOPATHIES
The concept of linking ALS and FTLD-U precedes the discovery of TDP-43 based on the shared accumulation of ubiquitin-positive cellular inclusions, as well as on the clinical evidence of overlapping symptoms. Initially, TDP-43 pathology in FTLD-U, FTLD-MND or ALS was reported only in select CNS areas.14,15 However, increasing evidence indicates that the deposition of pathological TPD-43 aggregates occurs in multiple brain areas in ALS as well as FTLD-TDP35–40 (Fig. 1). Detailed reviews on the significance of clinical overlap and transition forms between ALS, ALS-D, FTLD-MND and FTLD-U have recently been published41–43 and consensus criteria on the diagnosis of frontotemporal cognitive and behavioral syndromes in ALS have emerged.44 Likewise, the spectrum of TDP-43 pathology and the associated recommended neuropathological nomenclature, including the morphological subtypes, have been the subject of detailed reviews.19,45–49 We recently published a study on whole CNS TDP-43 pathology in a large cohort of cases representing the most common forms of TDP-43 proteinopathy, both according to their clinical phenotype (pure ALS, pure FTD, or a combination of both in FTLD-MND), as well as to their morphological subtypes.18 Based on this work and an astonishingly large number of other studies reported since 2006, we conclude that there is significant overlap of both clinical and pathological features among the major TDP-43 proteinopathies. In fact, ALS, ALS-D/FTLD-MND and FTLD-U may be situated at different points along one continuous and broad clinico-pathological spectrum of multisystem degenerations. Other than the defining clinical syndromes in pyramidal motor system and cognitive domains, extrapyramidal signs were the most common clinical features, consistent with the robust pathology found in the striatum and substantia nigra.18 FTLD-U subtype 1 (characterized by frequent long neuritic profiles predominantly in the superficial cortical layers) appears to represent the most “cortical variant of degeneration” in comparison with subtypes 2 (with neuronal cytoplasmic inclusions in superficial and deep cortical layers) and 3 (with abundance of small neuritic profiles and neuronal cytoplasmic inclusions predominantly in the superficial cortical layers).12,18 In terms of LMN pathology, the latter two subtypes (especially subtype 2) are closer to the MND phenotype when compared with subtype 1 (Fig. 2). Further, cases with predominantly neuronal intracytoplasmic inclusions (i.e., subtype 212) can present with clinical MND in addition to FTD,50 whereas cases with predominantly dystrophic neurites (i.e., subtype 112) tend to show semantic dementia, and when neuronal cytoplasmic inclusions and dystrophic neurites are coupled with neuronal intranuclear inclusions, albeit less frequent (i.e., subtype 312), FTD or progressive nonfluent aphasia is common with or without clinical MND.50 These clinico-pathological correlations continue to be affirmed in recent studies of additional cohorts of post mortem cases based on TDP-43 staining.51,52 Notably, FTLD-U patients with numerous neuronal cytoplasmic inclusions, as seen in subtypes 2 or 3,have shorter survival times than those with subtype 1,18,51,53 potentially indicating a link to the involvement of LMNs in decreased survival, as it was previously shown that FTLD-MND has significantly shorter survival than FTLD-U.54 We also showed that inclusion formation is present to a greater extent than neuronal loss and gliosis in neocortex of ALS cases which may signify that TPD-43 pathology develops very early in the disease state and precedes overt neurodegeneration by some as yet unspecified period of time.18 However, in advanced disease stages, TDP-43 inclusion pathology and reactive tissue changes can be similarly abundant due to more profound degenerative changes.18 For the future, other proteins linked to disease progression may be identified in TDP-43 inclusions, but their role in mechanisms of neurodegeneration in TDP-43 proteinopathies will need to be defined.55
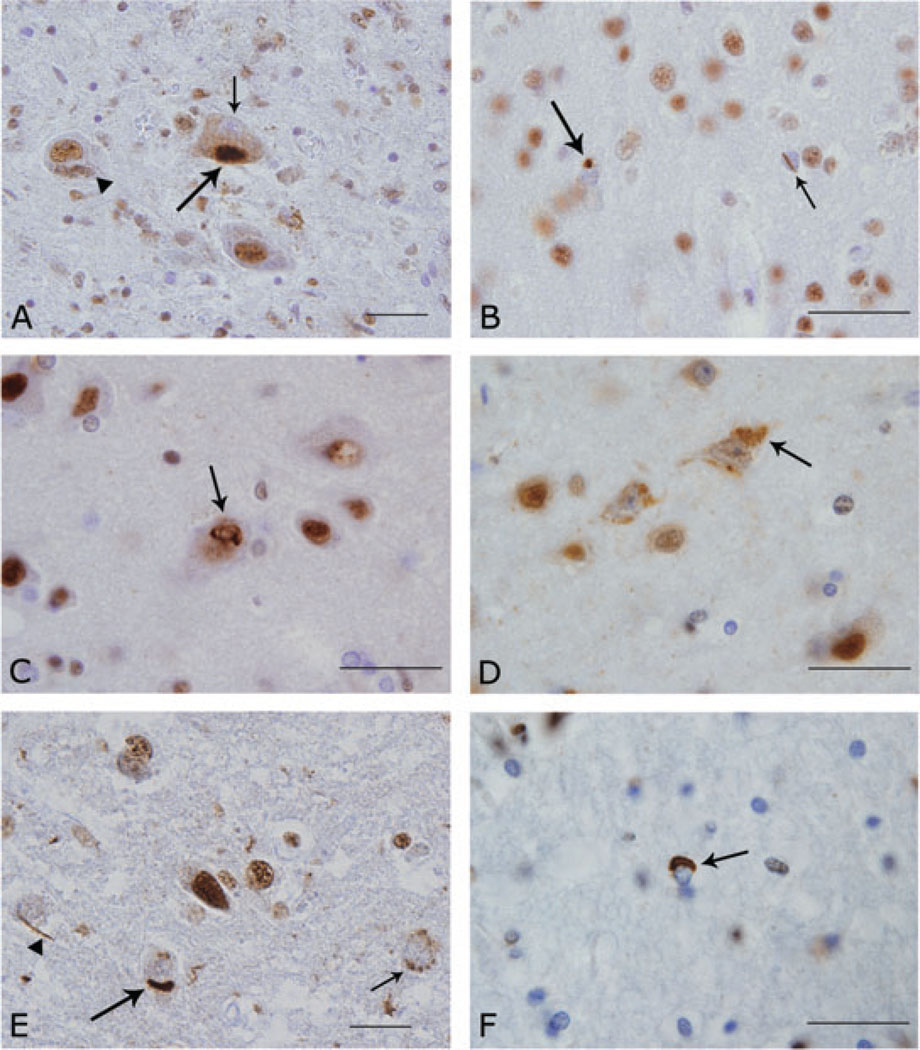
Fig. 1.
Anti-(TAR) DNA binding protein with aMr of 43 (TDP-43) immunohistochemistry in ALS with dementia (A–D,F) and frontotemporal lobar degeneration (FTLD)-TDP (E) (bar = 20 µm). A. Lewy body-like inclusion (large arrow) in the substantia nigra; note the nucleus devoid of the endogenous TDP-43 staining (“cleared nucleus”) (small arrow) that is present in the affected neuron, but not in an unaffected neuron (arrowhead). B. Neuronal cytoplasmic inclusions (large arrow) and neuronal intranuclear inclusion (short arrow) in the visual cortex. C. Fibrillar or skein-like curled inclusions in the sensory cortex (arrow). D. Cleared nuclei coupled with cytoplasmic, granular, or diffuse staining (“pre-inclusions”) (large arrow) in Wernicke’s area. E. Hypothalamus showing dense neuronal cytoplasmic inclusion (large arrow), smaller granular neuronal cytoplasmic TDP-43 immunoreactivity (small arrow), and dystrophic cellular processes (arrowhead). F. Oligodendrocyte with cytoplasmic inclusion in the white matter of cingulate gyrus.
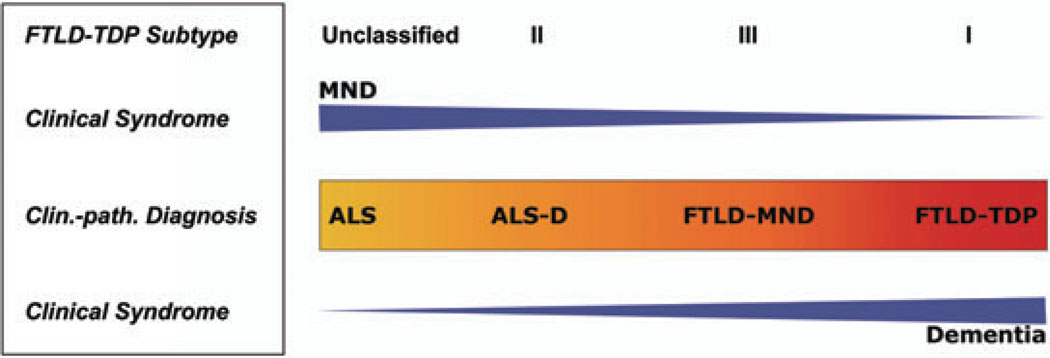
Fig. 2.
(TAR) DNA binding protein with a Mr of 43 (TDP-43) multisystem diseases: clinico-pathological spectrum. Schematic illustration of the concept of a clinico-pathological spectrum of the major TPD-43 diseases extending from frontotemporal lobar degeneration (FTLD)-U (ubiquitin-positive) or FTLD-TDP at one end to ALS at the other. Blue arrowhead-like triangles denote clinical syndrome with motor neuron disease decreasing and dementia increasing from left to right. Color change in central box denotes increasing or decreasing spread and severity of TDP-43 pathology in the brain and spinal cord, as an approximate estimation. Specifically, yellow represents predominant involvement of the spinal cord and red represents predominant involvement of cortical areas. Other brain areas are not as explicitly represented in this color-coded diagram. FTLD-U subtype refers to the classification of the cortical pattern of TDP-43 or ubiquitin-positive inclusions according to Sampathu et al.12 with the addition of an unclassified type denoting the absence of TDP-43 lesions or the presence of a degree of TDP-43 pathology burden that was not sufficient for subtyping. MND = motor neuron disease, ALS-D = ALS with dementia, FTLD-MND = frontotemporal degeneration with MND.
BIOCHEMISTRY OF PATHOLOGICAL TDP-43
From the biochemical perspective, the profile of the TDP-43 proteinopathies has been shown in sporadic and familial FTLD-U and ALS CNS tissues to comprise ubiquitination, variable hyperphosphorylation and N-terminal truncation of the TDP-43 protein. SDS-PAGE of sarkosyl-insoluble extracts isolated from affected cortical regions showed disease-specific bands at ~45 kD, ~25 kD, as well as high molecular weight aggregate smears in addition to the normal band at 43 kD.14,15,56,57 Since pathological TDP-43 is abnormally hyperphosphorylated, we and others have investigated the sites of TDP-43 phosphorylation. Notably, TDP-43 has 41 serine, 15 threonine and eight tyrosine residues. By predictive in silico analysis some of these are potential phosphorylation sites as shown by Hasegawa and colleagues who made phosphorylation-specific antibodies and demonstrated that TDP-43 becomes abnormally phosphorylated at residues 379, 403, 404, 409, and 410 in a small number of cases of FTLD-U and ALS.57,58 In our study of a larger cohort of post mortem cases, we used a similar approach, and we reported on the characteristics of our rat monoclonal antibodies 1D3 and 7A9 raised to diphosphopeptide S409/410 of TDP-43 (CSMDSKSpSpGW).59 These monoclonal antibodies were used to study the presence of S409/410 phosphorylation by immunohistochemistry and immunoblots in a large series of FTLD-U cases with/without MND, including familial cases with progranulin (GRN) or valosin containing protein (VCP) mutations or linkage to chromosome 9p, as well as 18 ALS cases and other neurodegenerative disease cases with or without concomitant TDP-43 pathology. Our data demonstrated that phosphorylation of S409/410 of TDP-43 is a highly consistent feature in TDP-43 inclusions of ALS and FTLD-U, thereby confirming the findings of Hasegawa and colleagues,57,58 as well as extending our initial findings that pathological TDP-43 is abnormally phosphorylated.15 Further, we extended these studies by showing phosphorylated TDP-43 in the inclusions of a more diverse and larger group of sporadic and familial forms of TDP-43 proteinopathies.59 Physiological nuclear TDP-43 was not detectable with these monoclonal antibodies by immunohistochemistry, while accumulations of phosphorylated C-terminal fragments were readily seen in Western blots in affected cortical brain regions from ALS and FTLD-U. At least four fragments were detected suggesting that they may represent the same C-terminal fragment with different degrees of phosphorylation, different C-terminal fragments with same sites of phosphorylation, or a combination of both. Indeed, these C-terminal fragments were often more abundant than phosphorylated full-length TDP-43 in the cortex. However, in the spinal cord the predominant p409/410-labeled TDP-43 protein species is full-length TDP-43,59 which is consistent with our previous findings that different TDP-43 species may form distinct inclusions in cortical versus spinal cord cells.60
ELECTRON MICROSCOPY OF PATHOLOGICAL TDP-43
Several studies focusing on the ultrastructure of the TDP-43-positive inclusions have shown that these lesions contain granular material and variably abundant filaments (with an average width of ~15 nm) that are TDP-43 immunoreactive.39,56,57,61–64 However, unlike other neurodegenerative disorders characterized by filamentous inclusions such as AD, PD and FTLD-Tau that are brain amyloidoses, TDP-43 inclusions do not demonstrate the properties of amyloid.46 Thus, TDP-43 proteinopathies are distinct because they are not CNS amyloidoses and may therefore provide insights into the consequences of protein misfolding, oligomerization and aggregate formation in the absence of amyloidogenesis.46 The idea of inclusion formation with different morphological stages following a certain sequence has been raised in the literature in ALS with and without dementia.62 For example, it has been suggested that diffuse punctuate cytoplasmic staining in the form of linear wisps (“fine skeins”) aggregate to form thicker and longer threads (“coarse skeins”); Similarly, dot-like inclusions were postulated to eventually form round inclusions in this disease.62 And, in keeping with this idea it was suggested, based on immunohistochemical and biochemical studies, that delocalization, accumulation and ubiquitination of TDP-43 in the cytoplasm of human motor neurons are early dysfunctions in the cascade of the events leading to motor neuron degeneration in ALS, preceding the formation of insoluble inclusion bodies.65
GENETICS OF PATHOLOGICAL TDP-43
Recent findings of mutations in the TARDP gene in cases of familial autosomal-dominant and rare sporadic ALS patients further corroborate the significance of pathological TPD-43 as being mechanistically implicated in the disease process.66–81 Although no mutations in the TARDP gene have yet been reported in either familial or sporadic FTLD-U,66,68,82,83 single patients with FTLD-MND and TARDBP mutations do exist.84 Significantly, many of the TARDBP variants display autosomal-dominant inheritance in familial ALS patients, suggesting that they may be pathogenic mutations. To date, more than 25 TARDBP genetic variants have been identified, and the majority of these are in the glycine-rich domain of TDP-43, suggesting that they may disrupt the normal exon skipping and splicing functions of TDP-43. Finally, a number of variants involved the substitution of serine and threonine residues, suggesting the possibility that this could lead to aberrant phosphorylation of TDP-43 and play a role in the onset or progression of disease.
Moreover, mutations in a gene encoding another DNA/RNA-binding protein with striking structural and functional similarities to TDP-43 called FUS (fused in sarcoma) or TLS (translocation in liposarcoma) have been reported recently to trigger degeneration of motor neurons.85–87 A mutation in angiogenin, a protein that is involved in RNA maturation, was recently reported; however, the inclusions were negative for TDP-43 and angiogenin, but positive for smooth muscle alpha-actin, probably a partner of angiogenin.88 Further,SETX is the gene coding for senataxin, which is involved in DNA repair and RNA processing, and it has been shown to be mutated in familial ALS.89 Notably, GRN gene mutations cause TDP-43 pathology which is restricted largely to subtype 3,13,56,90–92 and despite the lack of apparent clinical or neuropathological differences between cases with and without GRN gene abnormalities, a distinct phenotype appears to be present at the molecular level.93 Given that the number of patients with a family history of dementia and/or MND is higher than that of patients with GRN, VCP or TARDBP mutations, other genetic abnormalities, such as the chromosome 9p locus or others, might play a role as well.94 Promising are recent data by Rollinson and coworkers95 which suggest ubiquitin-associated protein 1 (encoded on chromosome 9p) as being a genetic risk factor for subjects diagnosed with FTLD according to current diagnostic criteria by Neary and colleagues.6
BIOMARKERS OF PATHOLOGICAL TDP-43
Other recent studies have reported evidence of elevated TDP-43 plasma levels in clinically diagnosed FTD patients as well as in a subset of AD patients, which may reflect the presence of co-morbid TDP-43 pathology, and increased cerebrospinal fluid TDP-43 levels in FTLD-U and ALS patients as compared with controls.96–98 These are intriguing findings since they might offer the possibility of developing a diagnostic ante mortem assay and a biomarker to monitor responses to new interventions in clinical trials, but these studies need to be extended and the findings verified in larger patient and control cohorts, especially through post mortem follow-up studies. However, skeletal muscle of ALS patients, another potential ante mortem diagnostic approach, has been shown to be devoid of pathological TDP-43.99
CONCLUSIONS
In summary, TDP-43 diseases or proteinopathies represent a novel class of neurodegenerative disorders akin to α-synucleinopathies and tauopathies. Notwithstanding this, the definite pathogenetic role of TDP-43 inclusions in neurodegenerative diseases is not yet established.100–102 The widespread distribution of pathological TDP-43 establishes the diffuse involvement of the CNS, with different populations of neurons and glial cells being differentially vulnerable throughout the brain and spinal cord, as well as temporally throughout the disease course. The idea of a predominantly frontotemporal degeneration pattern in FTLD-TDP and a primarily pyramidal tract degeneration pattern in MND should be refined in favor of the concept that TDP-43 proteinopathies represent a broad clinico-pathological spectrum of a single disorder involving multiple systems and sharing similar disease mechanisms linked to pathological TDP-43.5,15,103,104
REFERENCES
- 1.Brooks BR, Miller RG, Swash M, Munsat TL. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000;1:293–299. doi: 10.1080/146608200300079536. [DOI] [PubMed] [Google Scholar]
- 2.Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of theWorld Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial “Clinical limits of amyotrophic lateral sclerosis” workshop contributors. J Neurol Sci. 1994;124 Suppl:96–107. doi: 10.1016/0022-510x(94)90191-0. [DOI] [PubMed] [Google Scholar]
- 3.Hirano A. Neuropathology of ALS: an overview. Neurology. 1996;47:S63–S66. doi: 10.1212/wnl.47.4_suppl_2.63s. [DOI] [PubMed] [Google Scholar]
- 4.Nakano T, Nakaso K, Nakashima K, Ohama E. Expression of ubiquitin-binding protein p62 in ubiquitin-immunoreactive intraneuronal inclusions in amyotrophic lateral sclerosis with dementia: analysis of five autopsy cases with broad clinicopathological spectrum. Acta Neuropathol. 2004;107:359–364. doi: 10.1007/s00401-004-0821-7. [DOI] [PubMed] [Google Scholar]
- 5.Mackenzie IR, Feldman HH. Ubiquitin immunohistochemistry suggests classic motor neuron disease, motor neuron disease with dementia, and frontotemporal dementia of the motor neuron disease type represent a clinicopathologic spectrum. J Neuropathol Exp Neurol. 2005;64:730–739. doi: 10.1097/01.jnen.0000174335.27708.0a. [DOI] [PubMed] [Google Scholar]
- 6.Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 7.Neary D, Snowden J, Mann D. Frontotemporal dementia. Lancet Neurol. 2005;4:771–780. doi: 10.1016/S1474-4422(05)70223-4. [DOI] [PubMed] [Google Scholar]
- 8.Geser F, Lee VM-Y, Trojanowski JQ. Frontotemporal dementias. In: Rosenberg RN, DiMauro S, Paulson H, Ptacek L, Nestler E, editors. The Molecular and genetic Basis of Neurological and Psychiatric Disease. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. pp. 330–338. [Google Scholar]
- 9.McKhann GM, Albert MS, Grossman M, Miller B, Dickson D, Trojanowski JQ. Clinical and pathological diagnosis of frontotemporal dementia: report of the Work Group on Frontotemporal Dementia and Pick’s Disease. Arch Neurol. 2001;58:1803–1809. doi: 10.1001/archneur.58.11.1803. [DOI] [PubMed] [Google Scholar]
- 10.Forman MS, Farmer J, Johnson JK, et al. Frontotemporal dementia: clinicopathological correlations. Ann Neurol. 2006;59:952–962. doi: 10.1002/ana.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kertesz A, McMonagle P, Blair M, Davidson W, Munoz DG. The evolution and pathology of frontotemporal dementia. Brain. 2005;128:1996–2005. doi: 10.1093/brain/awh598. [DOI] [PubMed] [Google Scholar]
- 12.Sampathu DM, Neumann M, Kwong LK, et al. Pathological heterogeneity of frontotemporal lobar degeneration with ubiquitin-positive inclusions delineated by ubiquitin immunohistochemistry and novel monoclonal antibodies. Am J Pathol. 2006;169:1343–1352. doi: 10.2353/ajpath.2006.060438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cairns NJ, Bigio EH, Mackenzie IR, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 2007;114:5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arai T, Hasegawa M, Akiyama H, et al. TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2006;351:602–611. doi: 10.1016/j.bbrc.2006.10.093. [DOI] [PubMed] [Google Scholar]
- 15.Neumann M, Sampathu DM, Kwong LK, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 16.Geser F, Martinez-Lage M, Kwong LK, Lee VM, Trojanowski JQ. Amyotrophic lateral sclerosis, frontotemporal dementia and beyond: the TDP-43 diseases. J Neurol. 2009;256:1205–1214. doi: 10.1007/s00415-009-5069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armstrong RA, Lantos PL, Cairns NJ. Overlap between neurodegenerative disorders. Neuropathology. 2005;25:111–124. doi: 10.1111/j.1440-1789.2005.00605.x. [DOI] [PubMed] [Google Scholar]
- 18.Geser F, Martinez-Lage M, Robinson J, et al. The clinical and pathological continuum of multisystem TDP-43 proteinopathies. Arch Neurol. 2009;66:180–189. doi: 10.1001/archneurol.2008.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bigio EH. TAR DNA-binding protein-43 in amyotrophic lateral sclerosis, frontotemporal lobar degeneration, and Alzheimer disease. Acta Neuropathol. 2008;116:135–140. doi: 10.1007/s00401-008-0405-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buratti E, Baralle FE. Multiple roles of TDP-43 in gene expression, splicing regulation, and human disease. Front Biosci. 2008;13:867–878. doi: 10.2741/2727. [DOI] [PubMed] [Google Scholar]
- 21.Mackenzie IR, Rademakers R. The role of transactive response DNA-binding protein-43 in amyotrophic lateral sclerosis and frontotemporal dementia. Curr Opin Neurol. 2008;21:693–700. doi: 10.1097/WCO.0b013e3283168d1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang IF, Wu LS, Shen CK. TDP-43: an emerging new player in neurodegenerative diseases. Trends Mol Med. 2008;14:479–485. doi: 10.1016/j.molmed.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Abhyankar MM, Urekar C, Reddi PP. A novel CpG-free vertebrate insulator silences the testis-specific SP-10 gene in somatic tissues: role for TDP-43 in insulator function. J Biol Chem. 2007;282:36143–36154. doi: 10.1074/jbc.M705811200. [DOI] [PubMed] [Google Scholar]
- 24.Ayala YM, Misteli T, Baralle FE. TDP-43 regulates retinoblastoma protein phosphorylation through the repression of cyclin-dependent kinase 6 expression. Proc Natl Acad Sci USA. 2008;105:3785–3789. doi: 10.1073/pnas.0800546105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buratti E, Brindisi A, Pagani F, Baralle FE. Nuclear factor TDP-43 binds to the polymorphic TG repeats in CFTR intron 8 and causes skipping of exon 9: a functional link with disease penetrance. Am J Hum Genet. 2004;74:1322–1325. doi: 10.1086/420978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buratti E, Dork T, Zuccato E, Pagani F, Romano M, Baralle FE. Nuclear factor TDP-43 and SR proteins promote in vitro and in vivo CFTR exon 9 skipping. EMBO J. 2001;20:1774–1784. doi: 10.1093/emboj/20.7.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mercado PA, Ayala YM, Romano M, Buratti E, Baralle FE. Depletion of TDP 43 overrides the need for exonic and intronic splicing enhancers in the human apoA-II gene. Nucleic Acids Res. 2005;33:6000–6010. doi: 10.1093/nar/gki897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ou SH, Wu F, Harrich D, Garcia-Martinez LF, Gaynor RB. Cloning and characterization of a novel cellular protein, TDP-43, that binds to human immunodeficiency virus type 1 TAR DNA sequence motifs. J Virol. 1995;69:3584–3596. doi: 10.1128/jvi.69.6.3584-3596.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strong MJ, Volkening K, Hammond R, et al. TDP43 is a human low molecular weight neurofilament (hNFL) mRNA-binding protein. Mol Cell Neurosci. 2007;35:320–327. doi: 10.1016/j.mcn.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Wang HY, Wang IF, Bose J, Shen CK. Structural diversity and functional implications of the eukaryotic TDP gene family. Genomics. 2004;83:130–139. doi: 10.1016/s0888-7543(03)00214-3. [DOI] [PubMed] [Google Scholar]
- 31.Bose JK, Wang IF, Hung L, Tarn WY, Shen CK. TDP-43 overexpression enhances exon 7 inclusion during the survival of motor neuron pre-mRNA splicing. J Biol Chem. 2008;283:28852–28859. doi: 10.1074/jbc.M805376200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ayala YM, Zago P, D’Ambrogio A, et al. Structural determinants of the cellular localization and shuttling of TDP-43. J Cell Sci. 2008;121:3778–3785. doi: 10.1242/jcs.038950. [DOI] [PubMed] [Google Scholar]
- 33.Gregory RI, Yan KP, Amuthan G, et al. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432:235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- 34.Wang IF, Reddy NM, Shen CK. Higher order arrangement of the eukaryotic nuclear bodies. Proc Natl Acad Sci USA. 2002;99:13583–13588. doi: 10.1073/pnas.212483099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brandmeir NJ, Geser F, Kwong LK, et al. Severe subcortical TDP-43 pathology in sporadic frontotemporal lobar degeneration with motor neuron disease. Acta Neuropathol. 2008;115:123–131. doi: 10.1007/s00401-007-0315-5. [DOI] [PubMed] [Google Scholar]
- 36.Davidson Y, Kelley T, Mackenzie IR, et al. Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol (Berl) 2007;113:521–533. doi: 10.1007/s00401-006-0189-y. [DOI] [PubMed] [Google Scholar]
- 37.Dickson DW, Josephs KA, Amador-Ortiz C. TDP-43 in differential diagnosis of motor neuron disorders. Acta Neuropathol (Berl) 2007;114:71–79. doi: 10.1007/s00401-007-0234-5. [DOI] [PubMed] [Google Scholar]
- 38.McCluskey LF, Elman LB, Martinez-Lage M, et al. Amyotrophic lateral sclerosis-plus syndrome with TAR DNA-binding protein-43 pathology. Arch Neurol. 2009;66:121–124. doi: 10.1001/archneur.66.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishihira Y, Tan CF, Onodera O, et al. Sporadic amyotrophic lateral sclerosis: two pathological patterns shown by analysis of distribution of TDP-43-immunoreactive neuronal and glial cytoplasmic inclusions. Acta Neuropathol. 2008;116:169–182. doi: 10.1007/s00401-008-0385-z. [DOI] [PubMed] [Google Scholar]
- 40.Nishihira Y, Tan CF, Toyoshima Y, et al. Sporadic amyotrophic lateral sclerosis: widespread multisystem degeneration with TDP-43 pathology in a patient after long-term survival on a respirator. Neuropathology. 2009 doi: 10.1111/j.1440-1789.2008.00999.x. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 41.Elman LB, McCluskey L, Grossman M. Motor neuron disease and frontotemporal lobar degeneration: a tale of two disorders linked to TDP-43. Neurosignals. 2008;16:85–90. doi: 10.1159/000109762. [DOI] [PubMed] [Google Scholar]
- 42.Liscic RM, Grinberg LT, Zidar J, Gitcho MA, Cairns NJ. ALS and FTLD: two faces of TDP-43 proteinopathy. Eur J Neurol. 2008;15:772–780. doi: 10.1111/j.1468-1331.2008.02195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strong MJ. The syndromes of frontotemporal dysfunction in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2008;9:323–338. doi: 10.1080/17482960802372371. [DOI] [PubMed] [Google Scholar]
- 44.Strong M, Grace G, Freedman M, et al. Consensus criteria for the diagnosis of frontotemporal cognitive and behavioural syndromes in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009;10:131–146. doi: 10.1080/17482960802654364. [DOI] [PubMed] [Google Scholar]
- 45.Dickson DW. TDP-43 immunoreactivity in neurodegenerative disorders: disease versus mechanism specificity. Acta Neuropathol. 2008;115:147–149. doi: 10.1007/s00401-007-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kwong LK, Neumann M, Sampathu DM, Lee VM, Trojanowski JQ. TDP-43 proteinopathy: the neuropathology underlying major forms of sporadic and familial frontotemporal lobar degeneration and motor neuron disease. Acta Neuropathol. 2007;114:63–70. doi: 10.1007/s00401-007-0226-5. [DOI] [PubMed] [Google Scholar]
- 47.Mackenzie IR, Neumann M, Bigio EH, et al. Nomenclature for neuropathologic subtypes of frontotemporal lobar degeneration: consensus recommendations. Acta Neuropathol. 2009;117:15–18. doi: 10.1007/s00401-008-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neumann M. Molecular Neuropathology of TDP-43 Proteinopathies. Int J Mol Sci. 2009;10:232–246. doi: 10.3390/ijms10010232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Neumann M, Kwong LK, Sampathu DM, Trojanowski JQ, Lee VM. TDP-43 proteinopathy in frontotemporal lobar degeneration and amyotrophic lateral sclerosis: protein misfolding diseases without amyloidosis. Arch Neurol. 2007;64:1388–1394. doi: 10.1001/archneur.64.10.1388. [DOI] [PubMed] [Google Scholar]
- 50.Mackenzie IR, Baborie A, Pickering-Brown S, et al. Heterogeneity of ubiquitin pathology in frontotemporal lobar degeneration: classification and relation to clinical phenotype. Acta Neuropathol (Berl) 2006;112:539–549. doi: 10.1007/s00401-006-0138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Josephs KA, Stroh A, Dugger B, Dickson DW. Evaluation of subcortical pathology and clinical correlations in FTLD-U subtypes. Acta Neuropathol. 2009;118:349–358. doi: 10.1007/s00401-009-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yokota O, Tsuchiya K, Arai T, et al. Clinicopathological characterization of Pick’s disease versus frontotemporal lobar degeneration with ubiquitin/TDP-43-positive inclusions. Acta Neuropathol. 2009;117:429–444. doi: 10.1007/s00401-009-0493-4. [DOI] [PubMed] [Google Scholar]
- 53.Grossman M, Wood EM, Moore P, et al. TDP-43 pathologic lesions and clinical phenotype in frontotemporal lobar degeneration with ubiquitin-positive inclusions. Arch Neurol. 2007;64:1449–1454. doi: 10.1001/archneur.64.10.1449. [DOI] [PubMed] [Google Scholar]
- 54.Josephs KA, Knopman DS, Whitwell JL, et al. Survival in two variants of tau-negative frontotemporal lobar degeneration: FTLD-U vs FTLD-MND. Neurology. 2005;65:645–647. doi: 10.1212/01.wnl.0000173178.67986.7f. [DOI] [PubMed] [Google Scholar]
- 55.Nakamura M, Ito H, Wate R, Nakano S, Hirano A, Kusaka H. Phosphorylated Smad2/3 immunoreactivity in sporadic and familial amyotrophic lateral sclerosis and its mouse model. Acta Neuropathol. 2008;115:327–334. doi: 10.1007/s00401-007-0337-z. [DOI] [PubMed] [Google Scholar]
- 56.Cairns NJ, Neumann M, Bigio EH, et al. TDP-43 in familial and sporadic frontotemporal lobar degeneration with ubiquitin inclusions. Am J Pathol. 2007;171:227–240. doi: 10.2353/ajpath.2007.070182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hasegawa M, Arai T, Nonaka T, et al. Phosphorylated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Ann Neurol. 2008;64:60–70. doi: 10.1002/ana.21425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Inukai Y, Nonaka T, Arai T, et al. Abnormal phosphorylation of Ser409/410 of TDP-43 in FTLD-U and ALS. FEBS Lett. 2008;582:2899–2904. doi: 10.1016/j.febslet.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 59.Neumann M, Kwong LK, Lee EB, et al. Phosphorylation of S409/410 of TDP-43 is a consistent feature in all sporadic and familial forms of TDP-43 proteinopathies. Acta Neuropathol. 2009;117:137–149. doi: 10.1007/s00401-008-0477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Igaz LM, Kwong LK, Xu Y, et al. Enrichment of C-terminal fragments in TAR DNA-binding protein-43 cytoplasmic inclusions in brain but not in spinal cord of frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Am J Pathol. 2008;173:182–194. doi: 10.2353/ajpath.2008.080003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lin WL, Dickson DW. Ultrastructural localization of TDP-43 in filamentous neuronal inclusions in various neurodegenerative diseases. Acta Neuropathol. 2008;116:205–213. doi: 10.1007/s00401-008-0408-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mori F, Tanji K, Zhang HX, et al. Maturation process of TDP-43-positive neuronal cytoplasmic inclusions in amyotrophic lateral sclerosis with and without dementia. Acta Neuropathol. 2008;116:193–203. doi: 10.1007/s00401-008-0396-9. [DOI] [PubMed] [Google Scholar]
- 63.Nishihira Y, Tan CF, Hoshi Y, et al. Sporadic amyotrophic lateral sclerosis of long duration is associated with relatively mild TDP-43 pathology. Acta Neuropathol. 2009;117:45–53. doi: 10.1007/s00401-008-0443-6. [DOI] [PubMed] [Google Scholar]
- 64.Thorpe JR, Tang H, Atherton J, Cairns NJ. Fine structural analysis of the neuronal inclusions of frontotemporal lobar degeneration with TDP-43 proteinopathy. J Neural Transm. 2008;115:1661–1671. doi: 10.1007/s00702-008-0137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Giordana MT, Piccinini M, Grifoni S, et al. TDP-43 Redistribution Is an Early Event in Sporadic Amyotrophic Lateral Sclerosis. Brain Pathol. 2009 doi: 10.1111/j.1750-3639.2009.00284.x. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Banks GT, Kuta A, Isaacs AM, Fisher EM. TDP-43 is a culprit in human neurodegeneration, and not just an innocent bystander. Mamm Genome. 2008;19:299–305. doi: 10.1007/s00335-008-9117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Daoud H, Valdmanis PN, Kabashi E, et al. Contribution of TARDBP mutations to sporadic amyotrophic lateral sclerosis. J Med Genet. 2009;46:112–114. doi: 10.1136/jmg.2008.062463. [DOI] [PubMed] [Google Scholar]
- 68.Gijselinck I, Sleegers K, Engelborghs S, et al. Neuronal inclusion protein TDP-43 has no primary genetic role in FTD and ALS. Neurobiol Aging. 2007;30:1329–1331. doi: 10.1016/j.neurobiolaging.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 69.Gitcho MA, Baloh RH, Chakraverty S, et al. TDP-43 A315T mutation in familial motor neuron disease. Ann Neurol. 2008;63:535–538. doi: 10.1002/ana.21344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guerreiro RJ, Schymick JC, Crews C, Singleton A, Hardy J, Traynor BJ. TDP-43 is not a common cause of sporadic amyotrophic lateral sclerosis. PLoS ONE. 2008;3:e2450. doi: 10.1371/journal.pone.0002450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kabashi E, Valdmanis PN, Dion P, et al. TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet. 2008;40:572–574. doi: 10.1038/ng.132. [DOI] [PubMed] [Google Scholar]
- 72.Kuhnlein P, Sperfeld AD, Vanmassenhove B, et al. Two German kindreds with familial amyotrophic lateral sclerosis due to TARDBP mutations. Arch Neurol. 2008;65:1185–1189. doi: 10.1001/archneur.65.9.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rutherford NJ, Zhang YJ, Baker M, et al. Novel mutations in TARDBP (TDP-43) in patients with familial amyotrophic lateral sclerosis. PLoS Genet. 2008;4:e1000193. doi: 10.1371/journal.pgen.1000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sreedharan J, Blair IP, Tripathi VB, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008;319:1668–1672. doi: 10.1126/science.1154584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Van Deerlin VM, Leverenz JB, Bekris LM, et al. TARDBP mutations in amyotrophic lateral sclerosis with TDP-43 neuropathology: a genetic and histopathological analysis. Lancet Neurol. 2008;7:409–416. doi: 10.1016/S1474-4422(08)70071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yokoseki A, Shiga A, Tan CF, et al. TDP-43 mutation in familial amyotrophic lateral sclerosis. Ann Neurol. 2008;63:538–542. doi: 10.1002/ana.21392. [DOI] [PubMed] [Google Scholar]
- 77.Kamada M, Maruyama H, Tanaka E, et al. Screening for TARDBP mutations in Japanese familial amyotrophic lateral sclerosis. J Neurol Sci. 2009;284:69–71. doi: 10.1016/j.jns.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 78.Corrado L, Ratti A, Gellera C, et al. High frequency of TARDBP gene mutations in Italian patients with amyotrophic lateral sclerosis. Hum Mutat. 2009;30:688–694. doi: 10.1002/humu.20950. [DOI] [PubMed] [Google Scholar]
- 79.Lemmens R, Race V, Hersmus N, et al. TDP-43 M311V mutation in familial amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2009;80:354–355. doi: 10.1136/jnnp.2008.157677. [DOI] [PubMed] [Google Scholar]
- 80.Del Bo R, Ghezzi S, Corti S, et al. TARDBP (TDP-43) sequence analysis in patients with familial and sporadic ALS: identification of two novel mutations. Eur J Neurol. 2009;16:727–732. doi: 10.1111/j.1468-1331.2009.02574.x. [DOI] [PubMed] [Google Scholar]
- 81.Pamphlett R, Luquin N, McLean C, Jew SK, Adams L. TDP-43 neuropathology is similar in sporadic amyotrophic lateral sclerosis with or without TDP-43 mutations. Neuropathol Appl Neurobiol. 2009;35:222–225. doi: 10.1111/j.1365-2990.2008.00982.x. [DOI] [PubMed] [Google Scholar]
- 82.Rollinson S, Snowden JS, Neary D, Morrison KE, Mann DM, Pickering-Brown SM. TDP-43 gene analysis in frontotemporal lobar degeneration. Neurosci Lett. 2007;419:1–4. doi: 10.1016/j.neulet.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 83.Schumacher A, Friedrich P, Diehl-Schmid J, et al. No association of TDP-43 with sporadic frontotemporal dementia. Neurobiol Aging. 2009;30:157–159. doi: 10.1016/j.neurobiolaging.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 84.Benajiba L, Le BI, I, Camuzat A, et al. TARDBP mutations in motoneuron disease with frontotemporal lobar degeneration. Ann Neurol. 2009;65:470–473. doi: 10.1002/ana.21612. [DOI] [PubMed] [Google Scholar]
- 85.Kwiatkowski TJ, Jr, Bosco DA, Leclerc AL, et al. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science. 2009;323:1205–1208. doi: 10.1126/science.1166066. [DOI] [PubMed] [Google Scholar]
- 86.Vance C, Rogelj B, Hortobagyi T, et al. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323:1208–1211. doi: 10.1126/science.1165942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lagier-Tourenne C, Cleveland DW. Rethinking ALS: the FUS about TDP-43. Cell. 2009;136:1001–1004. doi: 10.1016/j.cell.2009.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Seilhean D, Cazeneuve C, Thuries V, et al. Accumulation of TDP-43 and alpha-actin in an amyotrophic lateral sclerosis patient with the K17I ANG mutation. Acta Neuropathol. 2009;118:561–573. doi: 10.1007/s00401-009-0545-9. [DOI] [PubMed] [Google Scholar]
- 89.Chen YZ, Bennett CL, Huynh HM, et al. DNA/RNA helicase gene mutations in a form of juvenile amyotrophic lateral sclerosis (ALS4) Am J Hum Genet. 2004;74:1128–1135. doi: 10.1086/421054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baker M, Mackenzie IR, Pickering-Brown SM, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442:916–919. doi: 10.1038/nature05016. [DOI] [PubMed] [Google Scholar]
- 91.Cruts M, Gijselinck I, van der Zee J, et al. Null mutations in progranulin cause ubiquitin-positive frontotemporal dementia linked to chromosome 17q21. Nature. 2006;442:920–924. doi: 10.1038/nature05017. [DOI] [PubMed] [Google Scholar]
- 92.Sleegers K, Brouwers N, Maurer-Stroh S, et al. Progranulin genetic variability contributes to amyotrophic lateral sclerosis. Neurology. 2008;71:253–259. doi: 10.1212/01.wnl.0000289191.54852.75. [DOI] [PubMed] [Google Scholar]
- 93.Chen-Plotkin AS, Geser F, Plotkin JB, et al. Variations in the progranulin gene affect global gene expression in frontotemporal lobar degeneration. Hum Mol Genet. 2008;17:1349–1362. doi: 10.1093/hmg/ddn023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Le Ber I, Camuzat A, Berger E, et al. Chromosome 9p-linked families with frontotemporal dementia associated with motor neuron disease. Neurology. 2009;72:1669–1676. doi: 10.1212/WNL.0b013e3181a55f1c. [DOI] [PubMed] [Google Scholar]
- 95.Rollinson S, Rizzu P, Sikkink S, et al. Ubiquitin associated protein 1 is a risk factor for frontotemporal lobar degeneration. Neurobiol Aging. 2009;30:656–665. doi: 10.1016/j.neurobiolaging.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Foulds P, McAuley E, Gibbons L, et al. TDP-43 protein in plasma may index TDP-43 brain pathology in Alzheimer’s disease and frontotemporal lobar degeneration. Acta Neuropathol. 2008;116:141–146. doi: 10.1007/s00401-008-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kasai T, Tokuda T, Ishigami N, et al. Increased TDP-43 protein in cerebrospinal fluid of patients with amyotrophic lateral sclerosis. Acta Neuropathol. 2009;117:55–62. doi: 10.1007/s00401-008-0456-1. [DOI] [PubMed] [Google Scholar]
- 98.Steinacker P, Hendrich C, Sperfeld AD, et al. TDP-43 in cerebrospinal fluid of patients with frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Arch Neurol. 2008;65:1481–1487. doi: 10.1001/archneur.65.11.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Soraru G, Orsetti V, Buratti E, et al. TDP-43 in skeletal muscle of patients affected with amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2009 doi: 10.3109/17482960902810890. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 100.Pamphlett R, Kum JS. TDP-43 inclusions do not protect motor neurons from sporadic ALS. Acta Neuropathol. 2008;116:221–222. doi: 10.1007/s00401-008-0392-0. [DOI] [PubMed] [Google Scholar]
- 101.Sanelli T, Xiao S, Horne P, Bilbao J, Zinman L, Robertson J. Evidence that TDP-43 is not the major ubiquitinated target within the pathological inclusions of amyotrophic lateral sclerosis. J Neuropathol Exp Neurol. 2007;66:1147–1153. doi: 10.1097/nen.0b013e31815c5edd. [DOI] [PubMed] [Google Scholar]
- 102.Robertson J, Sanelli T, Xiao S, et al. Lack of TDP-43 abnormalities in mutant SOD1 transgenic mice shows disparity with ALS. Neurosci Lett. 2007;420:128–132. doi: 10.1016/j.neulet.2007.03.066. [DOI] [PubMed] [Google Scholar]
- 103.Brownell B, Oppenheimer DR, Hughes JT. The central nervous system in motor neurone disease. J Neurol Neurosurg Psychiatry. 1970;33:338–357. doi: 10.1136/jnnp.33.3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Geser F, Brandmeir NJ, Kwong LK, et al. Evidence of multisystem disorder in whole-brain map of pathological TDP-43 in amyotrophic lateral sclerosis. Arch Neurol. 2008;65:636–641. doi: 10.1001/archneur.65.5.636. [DOI] [PubMed] [Google Scholar]