Abstract
Background
Adolescents are developmentally in a period of transition—from children cared for by their parents to young adults capable of self-care, independent judgment, and self-directed problem solving. We wished to develop a behavioral contract for adolescent diabetes management that addresses some negotiable points of conflict within the parent–child relationship regarding self-monitoring and then assess its effectiveness in a pilot study as part of a novel cell phone–based glucose monitoring system.
Methods
In the first phase of this study we used semistructured interview techniques to determine the major sources of diabetes-related conflict in the adolescent–parent relationship, to identify factors that could facilitate or inhibit control, and to determine reasonable goals and expectations. These data were then used to inform development of a behavioral contract that addressed the negotiable sources of conflict between parents and their adolescent. The second phase of this research was a 3-month pilot study to measure how a novel cell phone glucose monitoring system would support the contract and have an effect on glucose management, family conflict, and quality of life.
Results
Interviews were conducted with 10 adolescent–caregiver pairs. The major theme of contention was nagging about diabetes management. Two additional themes emerged as points of negotiation for the behavioral contract: glucose testing and contact with the diabetes clinical team. Ten adolescent–parent pairs participated in the pilot test of the system and contract. There was a significant improvement in the Diabetes Self-Management Profile from 55.2 to 61.1 (P < 0.01). A significant reduction in hemoglobin A1c also occurred, from 8.1% at the start of the trial to 7.6% at 3 months (P < 0.04).
Conclusions
This study confirms previous findings that mobile technologies do offer significant potential in improving the care of adolescents with type 1 diabetes. Moreover, behavioral contracts may be an important adjunct to reduce nagging and improve outcomes with behavioral changes.
Background
Adolescents are developmentally in a period of transition—from children cared for by their parents to young adults capable of self-care, independent judgment, and self-directed problem solving. For adolescents with diabetes, parental involvement in their disease management generally decreases with increasing age and disease duration.1–3 However, some parental involvement is important in order to avoid deterioration in adherence and subsequent worsening of glycemic control.2–4 Parents and adolescents need to find a balance between dependence and autonomy because both too much and too little parental involvement in diabetes management can be detrimental.1,5,6 Anderson and Coyne7 highlighted how well-intentioned parental assistance can result in interpersonal conflict between youth with chronic health problems and their parents, a process known as “miscarried helping.” Parents of chronically ill children are faced with two sets of tasks: (1) taking responsibility for management of the disease at home in order to ward off the immediate threat of medical crises and (2) helping the child take developmentally appropriate steps in managing his or her own health. The construct of “miscarried helping,” when this leads to conflict, has proven to be consistent across a diverse group of families of youth with poorly controlled diabetes.8 Yet, research suggests that there is no specific “family profile” for predicting miscarried helping in families of youth with diabetes.9
Various studies have demonstrated that diabetes-specific and general family conflicts are both associated with lower treatment adherence in adolescents.1,5,10–12 Conversely, low levels of family stress, high family cohesion and organization, and good communication skills are associated with higher levels of regimen adherence and better glycemic control.13 Given these findings, it seems reasonable to postulate that interventions that target parent–child conflict could improve treatment adherence and subsequently improve glycemic control.
Much parent–adolescent conflict centers on self-monitoring of blood glucose behaviors. Parents experience stress trying to ensure that their child is testing his or her blood glucose and making appropriate insulin, diet, and exercise adjustments.14 Behavioral contracts are written documents that are mutually agreed upon by the involved parties and specify expected behaviors or responsibilities of the involved parties as well as consequences for success or failure.15–17 Behavioral contracts have been studied previously in the diabetes population to improve self-management.18,19 These contracts have traditionally detailed various kinds of positive reinforcement that can be earned by patients who fulfill specified improvements in particular diabetes self-management behaviors.20 They have not, however, previously, been customarily used as a tool for decreasing parent–child conflict.
One of the limits to broad application of behavioral contracts in youth with diabetes is the difficulty in determining whether or not individuals are complying with the terms of the contract, particularly in a real-time fashion. Our previous experience with cell phone–based glucose monitoring suggested that this new technology would allow us to monitor in real-time self-monitoring of blood glucose behaviors agreed upon in contracts to enable contract enforcement. This novel technology allows a remote provider to assess whether self-monitoring has occurred and, via the mobile link, advise the patient about adjustments. This serves to allow providers to assume some of the responsibility for supervising glucose monitoring that parents have traditionally performed and that has often served as a source of parent–adolescent conflict. Moreover, the system provides accurate data on testing frequency and timing. The technology offers a way for keeping everyone “in the loop” regarding their child's management of his or her diabetes and decisions that are made. Cell phone glucose monitors make it possible to engineer contracts that not only specify self-monitoring of blood glucose behavior, but also the frequency and quality of parent–adolescent interactions regarding self-monitoring behavior. The technology facilitates and monitors the boundaries agreed upon by parents and their adolescents in the behavioral contract.
Therefore, the first aim of this study was to develop a behavioral contract for adolescent diabetes management that addresses some negotiable points of conflict within the parent–child relationship regarding self-monitoring behavior. The second aim was to conduct a pilot study to test the hypothesis that the combination of the behavioral contract and a novel cell phone glucose monitoring system could improve family dynamics, quality of life, management competence, and glucose control.
Subjects and Methods
In the first phase of this study we used semistructured interview techniques to determine the major sources of diabetes-related conflict in the adolescent–parent relationship, to identify factors that could facilitate or inhibit control, and to determine reasonable goals and expectations. These data were then used to inform development of a behavioral contract that addressed the negotiable sources of conflict between parents and their adolescent.
Subjects were recruited from the pediatric diabetes clinics at the James Whitcomb Riley Hospital for Children in Indianapolis, IN. Adolescents with type 1 diabetes between the ages of 14 and 18 years living with at least one parent participated. Eligibility criteria included normal cognitive development and no other chronic diseases except well-controlled asthma. Subjects had to be literate in English.
To develop the behavioral contract, a professional qualitative researcher trained three research assistants to conduct in-depth behavioral assessments. These semistructured personal interviews were used to gather information from each parent–adolescent pairing. The parent and adolescent were interviewed separately as well as simultaneously in order to ensure that family interactions did not influence individuals to answer differently than they would if alone.
Interviews took no longer than an hour and were taped and transcribed. The interviews covered:
Details of diabetes management, including blood glucose measurement, carbohydrate counting, and exercise measurement
Self-reported history of compliance with management
Parental involvement with diabetes management
Family conflict surrounding diabetes management
Typical adolescent and parental interactions with the diabetes team
Negotiable points of contention between parents and adolescent
A pediatrician and a social ecologist who both have experience with qualitative methods then did qualitative analyses of the interview data. Both were experienced with the target population through both care and previous research efforts.
The analysis followed a set procedure that we have used in previous work using grounded theory: (1) audio review of the tapes, (2) reading through the transcriptions, (3) discussions between investigators regarding key elements of subjects' perceptions of living with diabetes and how it impacts relationships, (4) determination of conceptual themes, and (5) assignment of relevant responses to thematic constructs.14,21,22
The second phase of this research was a 3-month pilot study to determine how well the behavioral contract performed in conjunction with our cell phone–based glucose monitoring system to aid adolescents in the self-management of their disease. Subjects for this phase of the study were recruited in an identical fashion to those of the first phase using the same eligibility criteria, through letters followed by participant-initiated phone inquiries. Subjects who participated in Phase I were not eligible to participate in Phase II. Additionally, adolescents had to intend to remain in the care of the same diabetes care provider for the study duration. The first 10 adolescent–parent pairs who responded were recruited, as this was felt to be a feasible number to be monitored by a nurse practitioner (NP) over time using new and untested technology.
At the time of study entry, adolescents and their parents were oriented to the cell phone glucose meter (GlucoPack™, HealthPia, Palisades Park, NJ) system by an NP. The adolescent, at least one parent, and the NP reviewed the instruction manual together. The GlucoPack was programmed at that time with information personalizing it to the adolescent.
At the time of the first study visit, the NP also assisted both the adolescent and parent in the development of a behavioral contract. The exact points negotiated during this session were based on the findings from Phase I of the study. Based upon the contract, telephone or text-message (SMS) contacts were be made directly with the adolescent. Parents were also notified of this information by e-mail or telephone based upon the final contract. As part of this contract process, parents were asked to commit to a reduction in the frequency of questioning their child about his or her self-monitoring behavior. Rules for what constituted “appropriate” and “inappropriate” (i.e., nagging) behavior were established. These were based on both frequency and situational factors. In addition, a method to address contract violations was developed. Following the first contract breach the NP was to be notified by phone, SMS, or e-mail. After a second occurrence, the adolescent, parent, and NP were to discuss the issue together. If the contract was broken for a third time, all parties involved were to meet in person and renegotiate the contract boundaries. This involved discussion between research staff and the families to resolve the dispute and possibly renegotiate the contract.
Adolescents used the GlucoPack to measure blood glucose values during the study period. Test data were stored both on the phone and on an Internet site that the adolescent, NP, parent, and their physician and NP providers were able to access. The clinical use of the GlucoPack has been previously described.23 In brief, blood glucose data are uploaded automatically. The computer system evaluates the data and prompts the NP to contact the adolescent depending on the blood glucose values and/or frequency of testing. The NP can then text-message the patient directly to suggest regimen adjustments. Insulin adjustments were made by the NP using dose-adjustment algorithms. Subjects returned to the pediatric diabetes clinic for a routine visit at the end of the 3-month study period.
Data were gathered from all adolescents and participating parents at baseline and at the 3-month visit. We used previously validated tools to measure changes in a number of domains.
Study outcomes fell into five classifications
Usefulness of behavioral contract. Data gathered through surveys supplied data on whether the adolescents and their parents found the behavioral contracts and Glucopack to be useful and how well they functioned together.
Family dynamics. We used the Cornell Parent Behavior Description Scale24 to measure the antecedents and consequences of children's perceptions of the behavior of their parents towards them and the Helping for Health Inventory to measure levels of miscarried helping.
Psychological adjustment/quality of life. The Varney's Pediatric Quality of Life (PedsQL™) Diabetes Module was used to measure this variable.25
Competence in diabetes management. The Diabetes Self-Management Profile26 was used to assess self-management.
Glycemic control. We assessed this by change in hemoglobin A1c values.
Regression was used to test if any significant changes occurred in measures of interest over the study period. We performed calculations using the STATA version 9.0 statistical package (STATA Corp., College Station, TX).
All methods were approved by the Indiana University–Purdue University/Clarian Institutional Review Board. All parent participants provided informed consent for this study with assent from the adolescents.
Results
Qualitative interviews
Interviews were conducted with 10 adolescent–caregiver pairs. The major theme of contention was nagging about diabetes management. Two additional themes emerged as points of negotiation for the behavioral contract: glucose testing and contact with the diabetes clinical team. Sample quotations are presented based on their representativeness.
Nagging
Nagging quickly emerged as the main issue in parent/adolescent management of type 1 diabetes. Adolescents understand that parents have to be involved, and they even grasp why nagging occurs; however, this does not mean that they condone it. In general, both parties seem to want a compromise and believe that one can be reached:
Adolescent: Often [nagging] is good and it is fine and sometimes it does get to be too much. I mean, when I am supposed to do something, I would expect them to ask me and nag, but sometimes they do it more than that.
Parent: I worry that he will have a lot of complications and I know that it could kill him and I worry that all these people are on him about his diabetes. My biggest concern is that when he doesn't have all these people on him all the time that he won't take care of himself.
In general, parents seemed willing to relinquish control and try to nag less, but only if responsibility was assumed by another party.
Glucose testing
The most significant area of nagging was around glucose testing. The number and times an adolescent was advised to test were variable, but almost no parents and adolescents felt that the child's current testing frequency was optimal. One teen expressed:
I think it could be better. I am 14. I am a teenager and I don't have enough a responsibility and sometimes when I forget to do something, I know it is going to affect everything else.
Another added:
I think it is possible for me to check more often and ask more questions if I am really confused on anything. I could probably talk to people more.
However, sometimes parents could go too far. When that occurred, the reminders crossed into nagging:
Like I go upstairs and watch TV, and they will come upstairs and ask if I tested and I will say no and they will tell me to go downstairs and count while I test.
Parents felt like they could not just leave it alone, however:
He is 15 and wants to be independent … I can't say that he forgets—he just doesn't do it—and he has been hospitalized 3 times in the last year and half and when you question him about it he just doesn't want you to ask. If I don't ask constantly and follow up if he is doing it, he just doesn't do it.
Most felt that appropriate negotiation and observation could lead to reduced nagging and improved management, though, as long as someone was keeping an eye on things.
Contact with the diabetes clinic team
When asked who was the most effective and easiest to talk to about diabetes, a surprisingly high number of participants indicated clinic personnel. If anything, the participants just wished that contact would be more regular. One teen expressed:
I just want to make sure that they know that I have things under control and that they know when they are not so under control.
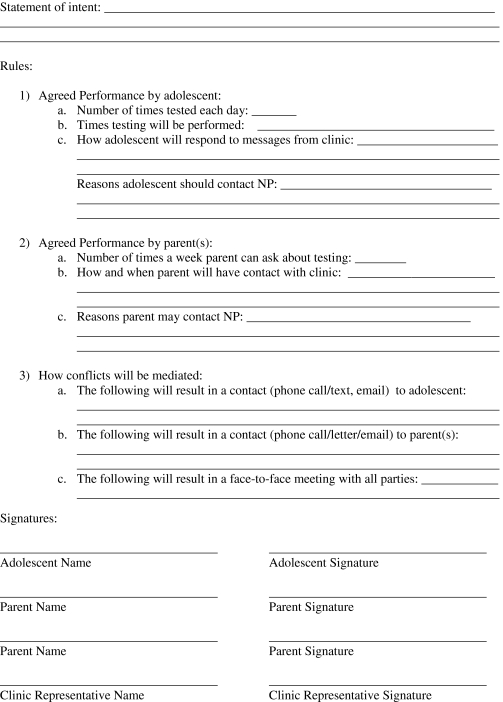
The Behavioral Contract
Based on these findings, we created a behavioral contract that allowed for negotiation of these key points (Appendix). The contract specifically stipulated when adolescents were supposed to test. Moreover, parents agreed limiting their amount of nagging. If any party violated the contract, specific plans were in place to address those breaks. How and when the clinic staff would contact both parent and adolescent participants was clearly identified so that participants would feel comfortable that concerns would be addressed. The process of negotiating the contract for the NP working with each individual parent–adolescent pair took about 20 min.
The GlucoPack device was used as the method of monitoring the contract. If adolescents checked their glucose levels less than negotiated, the NP intervened, as outlined above, in order to encourage better testing. If parents violated the nagging agreements, adolescents could notify the NP through text-messaging or a phone call.
Pilot Testing of Device with Behavioral Contract
Ten adolescent–parent pairs participated in the pilot test of the system and contract. Five of the adolescents were girls, and five were boys. All 10 pairs completed the study and filled out all study materials. The contract added about 20 min to each visit, which allowed the adolescent and parent to be interviewed separately and then together in order to agree upon the contract. During the 6-month study time period, no adolescent–parent pair had to renegotiate the initial contract. However, one parent was notified via the telephone by the NP that the adolescent was close to warranting a meeting to renegotiate a new behavioral contract.
Baseline and 3-month data for the various scoring measures appear in Table 1. There was no significant difference in the Cornell Parent Behavior Description Scale from baseline (mean, 101.2; 95% confidence interval [CI], 95.7–106.7) to the 3-month endpoint (mean, 101.1; 95% CI, 96.2–106.0). There was also no significant change in the Pediatric Quality of Life scale from baseline (mean, 134.3; 95% CI, 123.7–144.9) to the 3-month endpoint (mean, 133.5; 95% CI, 126.1–140.9). There was, however, a significant improvement in the Diabetes Self-Management Profile from 55.2 (95% CI, 50.8–59.6) to 61.1 (95% CI, 55.5–66.7) (P < 0.01). A significant reduction in A1c also occurred, from 8.1% (95% CI, 7.3–8.9%) at the start of the trial to 7.6% (95% CI, 7.1–8.1%) at 3 months (P < 0.04).
Table 1.
Outcomes of Interest
| Outcome | Baseline (95% CI) | 3 months (95% CI) |
|---|---|---|
| Diabetes Self-Management Profile | 55.2 (50.8–59.6) | 61.1 (55.5–66.7) |
| Quality of Life Score | 134.3 (123.7–144.9) | 133.5 (126.1–140.9) |
| Cornell Parent Behavior Scale | 101.2 (95.7–106.7) | 101.1 (96.2–106.0) |
| Hemoglobin A1c (%) | 8.1 (7.3–8.9) | 7.6 (7.1–8.1) |
Those outcomes that showed statistically significant improvement at P < 0.5 are in bold type.
CI, confidence interval.
The NP spent an average of 1 h of time to text the adolescents in response to the flags the software system created each day. Actual phone call time was very low because most communication occurred by text-messaging. When adolescents were in school, texts were not returned immediately, so an additional half-hour of time was spent at night in following up on texts. One additional hour was spent updating electronic medical records with new insulin doses, notes, and notifying parents of any changes.
Conclusions
Although mobile technology holds much promise for improving the management of diabetes in adolescents, our previous work found that the use of a novel GlucoPack alone did not change any outcomes of interest, including A1c and behavioral measurements.27 We theorized that the addition of a behavioral contract would more explicitly change behavior and enhance the technology's ability to improve outcomes. In this pilot study, we found that to be so, because even with a small sample size, we found significant improvements in both A1c and in the Diabetes Self-Management Profile.
One advantage of using behavioral contracts rather than the other types of family-based interventions that have been used previously in this population is that behavioral contracts are relatively low-intensity interventions. This greatly enhances the ease of integrating them into routine follow-up clinical diabetes care. Low cost, minimal provider time commitment, and ease of use are essential for successful implementation of any intervention designed to improve adherence and glycemic control.
Our study does have limitations that warrant consideration. It was a small pilot study, and therefore the observed outcomes may not be generalizable. In addition, the study was conducted over a relatively short time frame. Whether the findings persist over a longer time frame needs to be evaluated. The technology was also not fully integrated into a standard clinic environment, in that it was being used as an adjunct to normal care and not by the patient's usual clinicians. More robust studies would alter normal clinical routines to use the technology.
In a previous study in which glucose values were transferred via modems to the clinics for review by an NP, we observed that parents were extremely satisfied with their child's glucose control being monitored remotely and reported feeling a sense of safety.27 In this study, using much more advanced technology, coupled with behavioral contracts, similar perceptions were reported by parents and were reinforced by similar perceptions by the adolescents. This suggests that remote monitoring may have benefits for satisfaction with care delivery that are not easily duplicated using existing methods. As this was not a full randomized controlled trial, we cannot be sure that the intervention led to the improvements, or whether other factors might be involved. Future work will be needed to determine this.
This study adds to previous findings that mobile technologies do offer significant potential in improving the care of adolescents with type 1 diabetes14,21,22 and provides preliminary data that the use of behavioral contracts may improve their performance. Moreover, behavioral contracts may be an important adjunct to reduce nagging and improve outcomes with behavioral changes. Such potential needs further exploration in larger, more robust studies and tighter integration of the contract and the technology in clinical care. As a next step, we hope to build a clinic around the use of this technology coupled with behavioral contracts in order to see how it performs in a normal clinical environment.
Appendix
Behavioral contract
The goal of this contract is to help arguments you may have about blood sugar testing. Specifically, we will ask parents to nag less and adolescents to test more and talk to the clinic if they fail to do so. First, we will explicitly agree on the intent of the contract. Then we will agree on rules as to what each of us will do in regards to testing. Finally, we will all agree on what will happen if one of us violates the contract.
Example Statement of Intent: The goal of this contract is set rules about (child's name) diabetes testing. We will declare how often (child's name) will test, how often (parents' names) can ask about it, and what will happen if people break the contract.
Acknowledgments
This research was funded by grants from the National Institutes of Health to A.E.C. (1 K23 DK067879-01 and 1 RO3 DK078704-01) and from the American Diabetes Association to D.G.M. (7-06-HB-04). Glucophones were provided by HealthPia for the purposes of this research. HealthPia was not involved in the design, conduct, or analysis of this study, nor were the company or its employees involved in the preparation or editing of this manuscript.
Author Disclosure Statement
No competing financial interests exist for any authors.
References
- 1.Anderson BJ. Brackett J. Ho J. Laffel LM. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22:713–721. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- 2.Wysocki T. Taylor A. Hough BS. Linscheid TR. Yeates KO. Naglieri JA. Deviation from developmentally appropriate self-care autonomy. Association with diabetes outcomes. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]
- 3.Anderson B. Auslander W. Jung K. Miller J. Santiago J. Assessing family sharing of diabetes responsibilities. J Pediatr Psychol. 1990;15:477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- 4.Anderson B. Ho J. Brackett J. Finkelstein D. Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130:257–265. doi: 10.1016/s0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- 5.Miller-Johnson S. Emery RE. Marvin RS. Clarke W. Lovinger R. Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. J Consult Clin Psychol. 1994;62:603–610. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- 6.Coyne JC. Anderson BJ. The “psychosomatic family” reconsidered: diabetes in context. J Marital Fam Ther. 1988;14:113–123. doi: 10.1111/j.1752-0606.1989.tb00793.x. [DOI] [PubMed] [Google Scholar]
- 7.Anderson BJ. Coyne JC. Family context and compliance behavior in chronically ill children. In: Krasnegor NA, editor; Epstein L, editor; Johnson SB, editor; Yaffe SJ, editor. Developmental Aspects of Health Compliance Behavior. Hillsdale, NJ: Lawrence Erlbaum Associates; 1993. pp. 77–89. [Google Scholar]
- 8.Harris MA. Antal H. Oelbaum R. Buckloh LM. White NH. Wysocki T. Good intentions gone awry: assessing parental “miscarried helping” in diabetes. Families Systems Health. 2008;26:393–403. [Google Scholar]
- 9.Harris MA. Oelbaum R. Antal H. Buckloh LM. Sadler M. White NH. Miscarried helping in families of youth with diabetes: demographic and diabetes-related profiling [abstract] Diabetes. 2007;56:A496. [Google Scholar]
- 10.Anderson B. Miller J. Auslander W. Santiago J. Family characteristics of diabetic adolescents: relationship to metabolic control. Diabetes Care. 1981;4:586–594. doi: 10.2337/diacare.4.6.586. [DOI] [PubMed] [Google Scholar]
- 11.Hanson CL. Henggeler SW. Burghen GA. Model of associations between psychosocial variables and health-outcome measures of adolescents with IDDM. Diabetes Care. 1987;10:752–758. doi: 10.2337/diacare.10.6.752. [DOI] [PubMed] [Google Scholar]
- 12.Schafer LC. Glasgow RE. McCaul KD. Dreher M. Adherence to IDDM regimens: relationship to psychosocial variables and metabolic control. Diabetes Care. 1983;6:493–498. doi: 10.2337/diacare.6.5.493. [DOI] [PubMed] [Google Scholar]
- 13.Delamater AM. Jacobson AM. Anderson B. Cox D. Fisher L. Lustman P. Rubin R. Wysocki T. Psychosocial Therapies Working Group: Psychosocial therapies in diabetes: report of the Psychosocial Therapies Working Group. Diabetes Care. 2001;24:1286–1292. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- 14.Carroll AE. Marrero DG. How do parents perceive their adolescent's diabetes: a qualitative study. Diabet Med. 2006;23:1222–1224. doi: 10.1111/j.1464-5491.2006.01961.x. [DOI] [PubMed] [Google Scholar]
- 15.Wysocki T. Green LB. Huxtable K. Blood glucose monitoring by diabetic adolescents: compliance and metabolic control. Health Psychol. 1989;8:267–284. doi: 10.1037//0278-6133.8.3.267. [DOI] [PubMed] [Google Scholar]
- 16.DeRisi W. Butz G. Writing Behavioral Contracts: A Case Simulation Practice Manual. Champaign, IL: Research Press; 1975. [Google Scholar]
- 17.Zarb JM. Cognitive-Behavioral Assessment and Therapy with Adolescents. New York: Brunner/Mazel; 1992. [Google Scholar]
- 18.Carney RM. Schechter K. Davis T. Improving adherence to blood glucose monitoring in insulin-dependent diabetic children. Behav Ther. 1983;14:247–254. [Google Scholar]
- 19.Schafer LC. Glasgow RE. McCaul KD. Increasing the adherence of diabetic adolescents. J Behav Med. 1982;5:353–362. doi: 10.1007/BF00846162. [DOI] [PubMed] [Google Scholar]
- 20.Wysocki T. Behavioral assessment and intervention in pediatric diabetes. Behav Modification. 2006;30:72–92. doi: 10.1177/0145445505284275. [DOI] [PubMed] [Google Scholar]
- 21.Carroll AE. Marrero DG. The role of significant others in adolescent diabetes: a qualitative study. Diabetes Educ. 2006;32:243–252. doi: 10.1177/0145721706286893. [DOI] [PubMed] [Google Scholar]
- 22.Carroll AE. Marrero DG. What adolescents with type I diabetes and their parents want from testing technology: a qualitative study. Comput Inform Nurs. 2007;25:23–29. doi: 10.1097/00024665-200701000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Carroll AE. Marrero DG. Downs SM. The HealthPia GlucoPack Diabetes phone: a usability study. Diabetes Technol Ther. 2007;9:158–164. doi: 10.1089/dia.2006.0002. [DOI] [PubMed] [Google Scholar]
- 24.Marrero DG LN. Golden MP. Kershnar A. Myers GC. Family dynamics in adolescent diabetes mellitus: parental behavior, metabolic control. Psychological aspects of diabetes in children and adolescents. In: Kaplan SA, editor. Clinical Pediatric and Adolescent Endocrinology. Philadelphia: Saunders; 1982. pp. ix–392. [Google Scholar]
- 25.Varni JW. Burwinkle TM. Jacobs JR. Gottschalk M. Kaufman FR. Jones KL. The PedsQL in type 1 and type 2 diabetes. Diabetes Care. 2003;26:631–637. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- 26.Harris MA. Wysocki T. Sadler M. Wilkinson K. Harvey LM. Buckloh LM. Mauras N. White NH. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23:1301–1304. doi: 10.2337/diacare.23.9.1301. [DOI] [PubMed] [Google Scholar]
- 27.Carroll AE. Dimeglio LA. Stein S. Marrero DG. Using a cell phone-based glucose monitoring system for adolescent diabetes management. Diabetes Educ. 2011;37:59–66. doi: 10.1177/0145721710387163. [DOI] [PMC free article] [PubMed] [Google Scholar]