Abstract
Aim
Little is known about body image in children with endocrine conditions. We evaluated body image in children with congenital adrenal hyperplasia (CAH), familial male precocious puberty (FMPP), and Cushing's syndrome (CS).
Study design
We compared 67 patients (41 CAH, 12 FMPP, 14 CS) age 8–18 years with 55 age-matched controls.
Results
Patients expressed more weight unhappiness than controls (females: p <0.001; males: p ~ 0.01). This difference remained for females after adjusting for body mass index (BMI) (p ~ 0.03), but not for males (p ~ 0.12). Unhappiness with height and age of appearance was similar between groups. In female patients, higher BMI was a significant predictor of weight unhappiness (p ~ 0.01).
Conclusion
Adolescents with CAH, FMPP, and CS are at risk for negative body image regarding weight, but not height or age of appearance. Weight unhappiness is partially related to greater weight, but factors unrelated to physical findings seem to contribute to negative body image in female patients.
INTRODUCTION
Both early and late puberty, short stature, and obesity have been implicated as potential risk factors for negative body image in healthy adolescents. Previous studies suggest that early puberty is associated with negative body image in female but not male adolescents1,2. Early puberty has also been reported as a risk factor for depression2,3, and risk-taking behavior in girls4, while later maturation may predispose for poor self-image in boys5. In normally-timed puberty, body dissatisfaction in females has been correlated with increased weight6,7. Short stature has been suggested as a risk factor for negative body image, especially in males. However, several studies refute this notion8–10.
Patients with congenital adrenal hyperplasia (CAH), familial male precocious puberty (FMPP) and Cushing's syndrome (CS) are at risk for abnormal growth and development. CAH and FMPP represent two genetic causes of gonadotropin releasing hormone (GnRH)-independent causes of precocious puberty and androgen excess. Patients with CAH and FMPP are also at risk for development of secondary GnRH-dependent or central precocious puberty, and patients with CAH are at risk for obesity due to glucocorticoid therapy11,12. Although iatrogenic CS is common due to the widespread use of glucocorticoid medications for the treatment of various non-endocrine conditions, CS due to endogenous causes, such as pituitary tumors (Cushing's disease), is a rare endocrine condition. CS is characterized by decreased growth and excessive weight gain, placing these patients at risk for negative body image.
The aim of this study was to evaluate body image in patients with CAH, FMPP and CS, who are at risk for abnonnal growth and development. We compared body image in our patients with endocrine conditions to body image in age- and sex-matched controls, and evaluated clinical characteristics and parental stature as possible predictors of negative body image in these groups.
METHODS
Patients
From October 2002 through February 2005, we studied 67 patients (44 male, age 8–18 years) with endocrine disorders and 55 age- and sex-matched healthy children (23 male, age 9–16 years). Patients were recruited from ongoing research protocols at the National Institutes of Health Clinical Center, Bethesda, Maryland, and included 41 patients (age 9–18 years) with classic CAH, 12 patients (age 9–14 years) with FMPP, and 14 patients (age 10–18 years) with CS (Table 1). All patients with CAH were on glucocorticoid and mineralocorticoid replacement, patients with FMPP were receiving an anti-androgen and an aromatase inhibitor, and patients with CS were studied prior to surgical treatment. In addition, 40 patients (10 female and 19 male patients with CAH, 11 patients with FMPP) were receiving GnRH analog therapy (2 female and 19 male) or had completed GnRH analog therapy (8 female and 11 male) for secondary central precocious puberty. The average age of GnRH analog initiation was 7.6 years (range 4.8–10.9 years). All of the patients with CS had biochemically confirmed hypercortisolism. The average duration of CS based on onset of decreased growth velocity was 2.8 years (range 0.5–4.5 years). All patients with CS were evaluated before surgery for removal of a pituitary adenoma (13 patients) or before bilateral adrenalectomy (one patient with bilateral adrenal micronodular hyperplasia).
TABLE 1.
Clinical Characteristics
| CAH (n = 41) |
FMPP (n = 12) |
Cushing (n = 14) |
Control (n = 55) |
|
|---|---|---|---|---|
| No. of males (%) | 27 (65.9) | 12 (100) | 5 (35.7) | 23 (41.8) |
| Age (years) | 12.6 ± 2.5 | 114 ± 1.8 | 13.9 ± 2.9 | 13.3 ± 2.2 |
| Female | 13.7 ± 2.6 | 13.9 ± 2.6 | 13.3 ± 2.1 | |
| Male | 12.1 ± 2.4 | 11.4 ± 1.8 | 13.9 ± 2.4 | 13.3 ± 2.2 |
| Bone age (years) | 13.8 ± 1.9 | 14.3 ± 2.6 | 13.9 ± 2.4 | |
| Height (SDS) | 0.0 ± 1.2 | 1.0 ± 1.3 | −0.9 ± 1.2 | 0.5 ± 1.1 |
| Female | −0.4 ± 1.2 | −0.9 ± 1.1 | 0.6 ± 1.0 | |
| Male | 0.2 ± 1.2 | 1.0 ± 1.3 | −0.9 ± 1.4 | 0.4 ± 1.1 |
| Weight (SDS) | 1.1 ± 1.5 | 1.2 ± 0.7 | 1.9 ± 0.9 | 0.4 ± 1.2 |
| Female | 0.6 ± 1.5 | 1.5 ± 0.6 | 0.4 ± 1.4 | |
| Male | 1.3 ± 1.4 | 1.2 ± 0.7 | 2.5 ± 1.1 | 0.4 ± 1.1 |
| Body mass index (SDS) | 1.2 ± 1.2 | 1.0 ± 0.8 | 2.1 ± 0.7 | 0.3 ± 1.2 |
| Female | 0.8 ± 1.3 | 1.9 ± 0.7 | 0.5 ± 0.8 | |
| Male | 1.4 ± 1.1 | 1.0 ± 0.8 | 2.6 ± 0.3 | −0.0 ± 1.6 |
| Tanner stage | 2.5 ± 1.5 | 3.1 ± 1.2 | 3.3 ± 1.3 | |
| Physical exam | ||||
| (breasts/testes) | ||||
| Tanner stage | 2.6 ± 1.3 | 3.3 ± 1.0 | 3.1 ± 1.1 | 3.1 ± 1.2 |
| Self-assessment | ||||
| (breasts/testes) | ||||
| Tanner stage | 2.8 ± 1.4 | 3.3 ± 1.0 | 4.0 ± 1.1 | |
| Physical exam | ||||
| (public hair) | ||||
| LHRH analogue, n (%) | 29 (70.7) | 11 (91.7) | 0 (0) |
Data are reported as means ± SD unless otherwise noted.
CAH = congenital adrenal hyperplasia; FMPP = familial male precocious puberty; Cushing = Cushing’s syndrome.
This study was approved by the institutional review boards at the National Institute of Mental Health and the National Institute of Child Health and Human Development. Each patient or a parent gave written informed consent, and children gave their assent.
Clinical protocol
All patients underwent a physical examination by either a trained nurse practitioner (MK) or a pediatric endocrinologist (CAS, EWL or DPM) as part of their routine evaluation. Pubertal stage was assessed by physical examination according to the criteria of Tanner for breast development in females13 and according to a modified genital staging method based on the average volume of both testes in males14. Specifically, testicular volumes <4 ml were defined as stage 1; 4 to <8 ml as stage 2, 8 to <12 ml as stage 3, 12 to <15 ml as stage 4, and ≥15 ml as stage 5. Healthy controls did not have a physical examination, but completed a self-assessment questionnaire (see below).
Within 1 to 2 days of physical examination, patients were given a standardized written body image questionnaire. Controls were administered the same questionnaire. Participants were asked to answer the following questions using a 5-point Likert scale: 1) How happy are you with your height? 2) How happy are you with your weight? 3) How happy are you with your overall body build and figure? 4) How happy are you with how old you look? Possible answers to each question were: 1) very unhappy, 2) somewhat happy, 3) neither unhappy nor happy, 4) somewhat happy, 5) very happy. Following these questions, participants were asked to complete a paper and pencil pubertal self-assessment. Females were given standardized drawings and a written description of the five Tanner stages of breast and pubic hair development; male patients were given drawings and a written description of five Tanner stages of genital and pubic hair development15. Participants were asked to look at each picture and circle the one that most closely resembled their own stage of development.
Statistical analysis
The data were analyzed using the statistical software SPSS (Chicago, IL). Body mass index (BMI), height and weight standard deviation scores (SDS) were determined using anthropometric reference data for US childrenl6. Midparental height was calculated using the following formulas: [mother's height + father's height + 13 cm]/2 for males, and [mother's height + father's height – 13 cm]/2 for females. Body image data were analyzed separately for females and males because of expected sex differences based on prior studies5,17–19. Answers to the body image questions were merged into two categories: unhappy (answer 1 or 2) or happy/neutral (answer 3, or 4 or 5) for each of the five body image questions.
First, all groups were compared on clinical characteristics (age, height SDS, weight SDS, BMI SDS, Tanner stage) using one way-ANOVA. Post-hoc analyses were performed using a Bonferroni correction for multiple comparisons when significant differences were found between the four groups.
Logistic regression was used to control for physical characteristics that were found to differ between patients and controls (i.e., BMI SDS). For the body image analyses (unhappy vs happy/neutral) using logistic regression, patient groups were merged into one group for each sex if they were similar to each other when adjusted for BMI SDS. In additional analyses, logistic regression was performed separately for patients and controls in order to identify potential predictors of negative body image. For the body image question related to height (question 1), potential predictors included height SDS, midparental height, father's height (male group) and mother's height (female group). For the body image question related to weight and overall body build (questions 2 and 3), potential predictors included weight SDS, BMI SDS, and GnRH analog treatment (patients). For the body image question related to age-appropriate appearance (question 4), potential predictors included height SDS, BMI SDS, pubertal stage, GnRH analog treatment (patients), midparental height, father's height (males) and mother's height (females).
Evaluation of inter-rater agreement (self-assessment vs physical examination) for patient pubertal staging was performed using the weighted kappa statistic. Statistical significance was defined as p<0.05. All values are expressed as means ± SD unless otherwise specified.
RESULTS
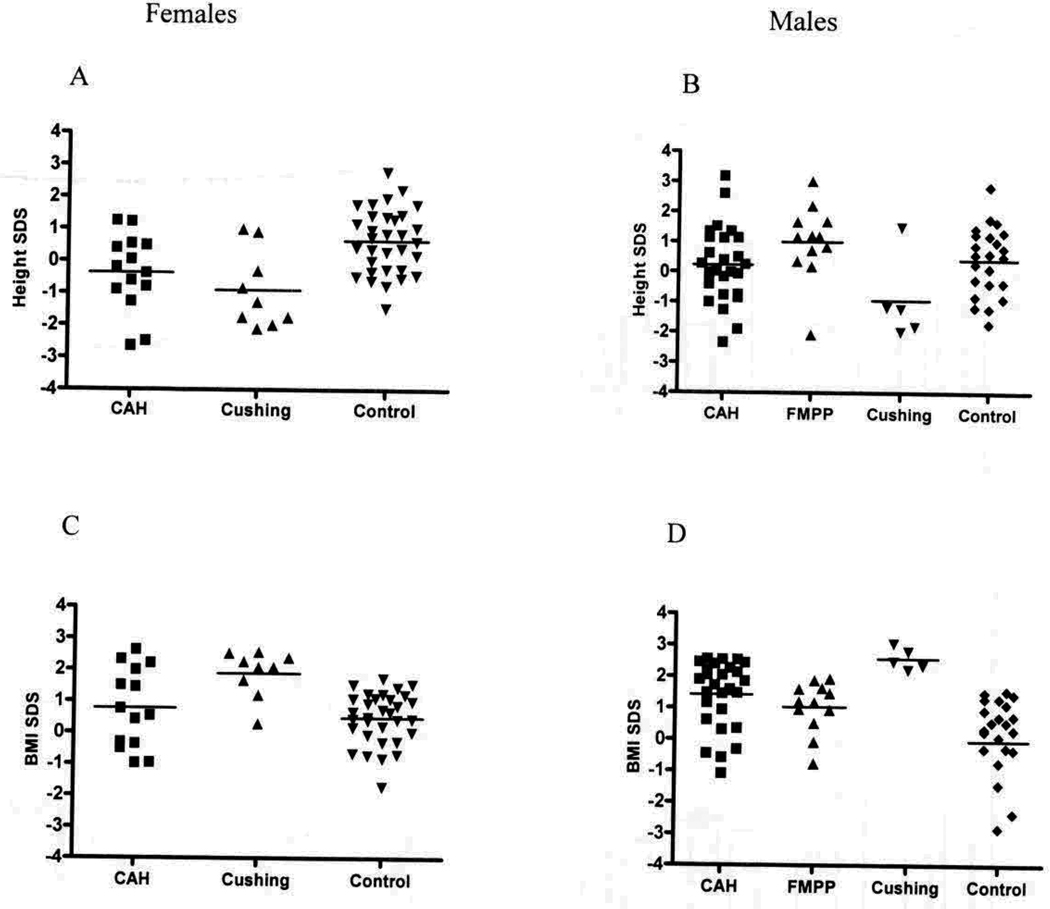
The majority (79%) of patients who participated in our study was exposed to excess sex steroids early in life due to a genetic condition (41 CAH, 12 FMPP) (Table 1). The remaining 21% had acquired CS due to a tumor. Controls were group matched to patients by age and sex. However, group differences were found for height SDS (p <0.001), weight SDS (p <0.001) and BMI SDS (p <0.001) (Fig. 1). Specifically, patients with CS were significantly shorter than both controls (p <0.001) and patients with FMPP (p <0.001) and they were significantly heavier than controls (p <0.001). Patients with CAH and CS had significantly higher BMI than controls (p <0.001 and p <0.001, respectively).
Fig. 1.
Anthropometrics in relation to patient group for height in (A) females and (B) males; and for weight in (C) females and (D) males. CAH = congenital adrenal hyperplasia; FMPP = familial male precocious puberty; Cushing = Cushing’s syndrome.
The patients and controls were similar in chronological age and patient groups had similar bone ages. However, the majority of patients with CAH and FMPP received a GnRH agonist for the treatment of central precocious puberty. None of the patients with CS experienced early onset of central precocious puberty (Table 1). The self-assessment Tanner stage of both male and female controls was comparable to the self-assessment and physical examination Tanner stages of the patients (Table 1). Patients accurately estimated their pubertal development (kappa: males: genital development 0.53, pubic hair 0.80; females: breast development 0.71, pubic hair 0.70).
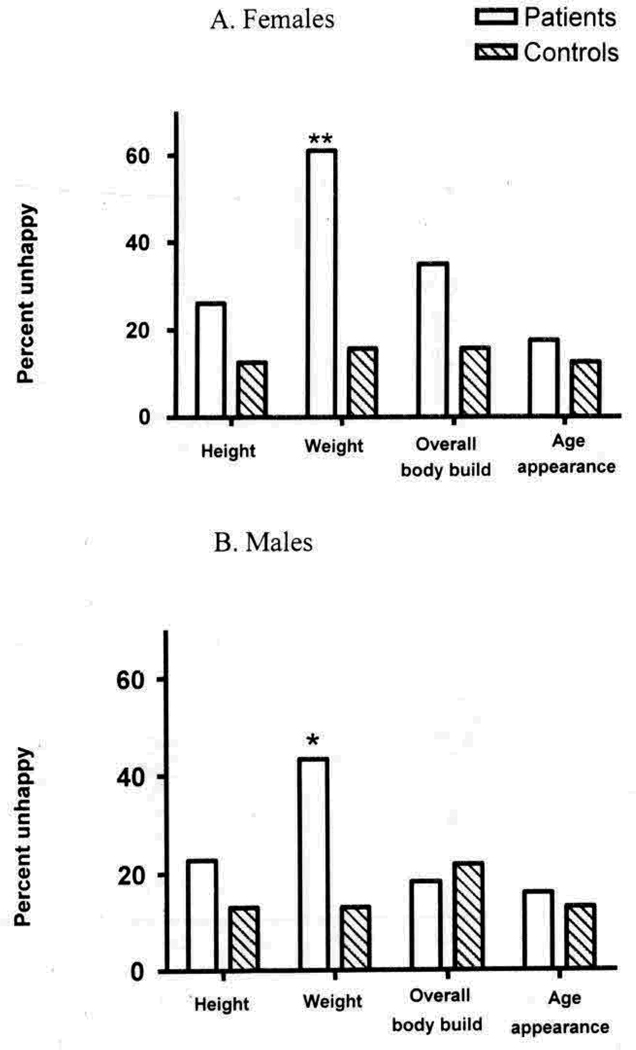
Body image questionnaires
All 67 patients and 55 controls completed the body image questionnaire. Body image unhappiness related to weight was more frequent in patients than controls (females: 60.9% vs 15.6%, p <0.001; males: 43.2% vs 13.0%, P = 0.01) (see Fig. 2). After adjusting for BMI SDS, this difference remained significant for females (odds ratio [OR] = 5.1, 95% confidence interval [CI]: 1.2, 21.6; P = 0.03), but was no longer significant for males (OR = 3.2, 95% CI: 0.7, 14.2; P = 0.12). Expression of body image unhappiness with height or age of appearance was similar between patients and controls.
Fig. 2.
Expression of negative body image for height, weight, overall body build and age of appearance in patients with congenital adrenal hyperplasia, familial male precocious puberty, and Cushing’s syndrome, and age- and sex-matched controls for (A) females and (B) males. ** p <0.001; * p <0.05.
Unhappiness with body build was more frequent in females with CS than in female controls (66.7% vs 15.6%; P = 0.001) and this difference remained significant after adjusting for BMI SDS (OR = 8.2, 95% CI: 1.1–59.3; p = 0.02). Expression of unhappiness with body build was similar between all other patient groups and controls.
In female patients, higher BMI SDS was found to be a significant predictor of unhappiness with weight (p = 0.01). No other predictors were found to be significant for any of the other body image questions for female patients, including height SDS, pubertal stage, age, midparental height, parental height, and GnRH analog treatment. Similarly, no significant predictors of negative body image were identified for any of the four questions for the female controls, male patients and male controls.
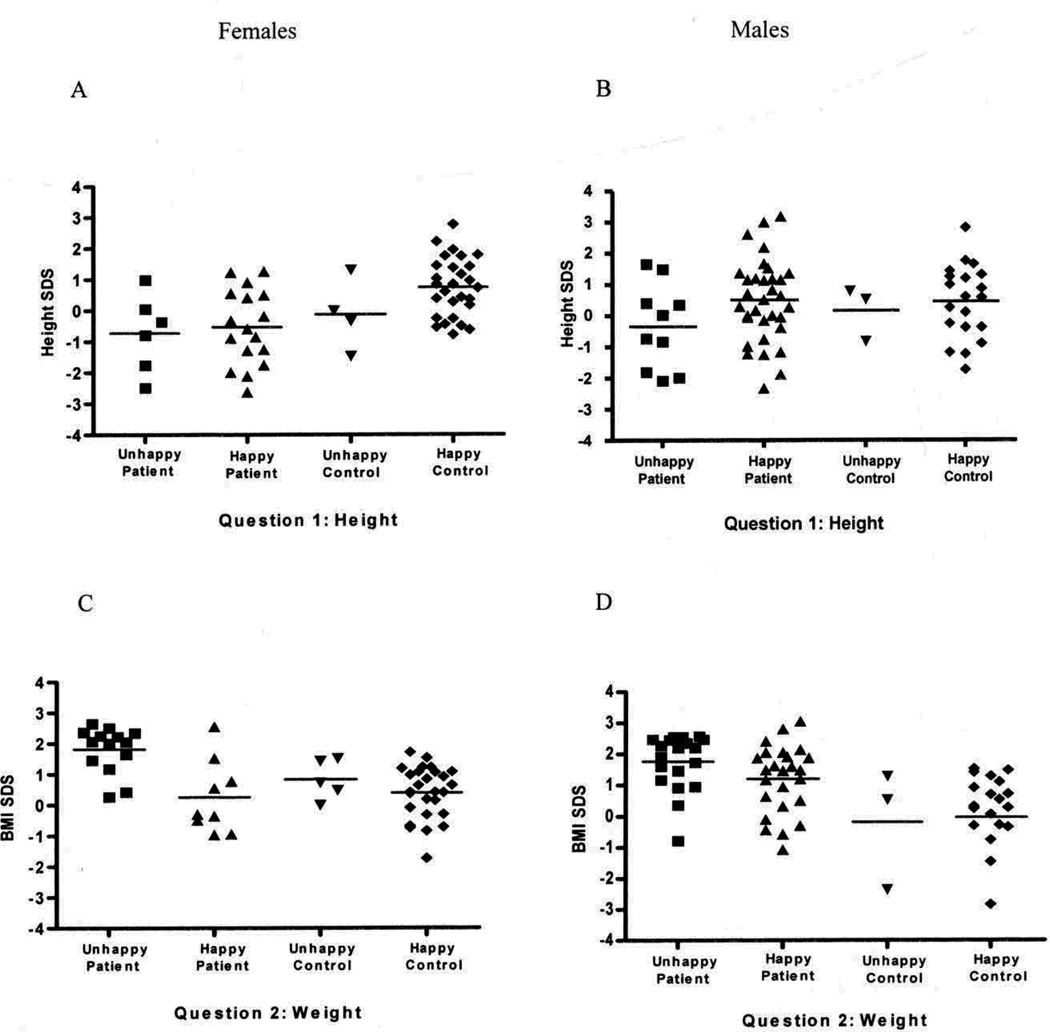
Female patients who expressed unhappiness with weight had a significantly higher weight SDS (1.59 ± 0.7 vs −0.06 ± l.4, p <0.001) and BMI SDS (1.8 ± 0.7 vs 0.26 ± 1.2, P <0.001) than female patients who were satisfied with their weight (Fig. 3). Unhappiness with weight in female controls, and male patients and controls was not associated with a higher weight or BMI. Interestingly, body image unhappiness with height, body build or age of appearance was not associated with any corresponding physical finding for both sexes and across groups (Fig. 3).
Fig. 3.
Anthropometrics in relation to expression of negative body image for height in (A) females and (B) males; and for weight in (C) females and (D) males.
DISCUSSION
We found that both female and male adolescents with CAH, FMPP, or CS are at risk for negative body image with respect to weight, but not height or age of appearance. Negative body image with respect to body build was more likely than controls only in females with CS. For male patients, body weight dissatisfaction was due to greater weight or BMI, whereas in females adjusting for BMI did not account for all of their negative body image even though it was a strong predictor. Excessive weight, therefore, may predispose adolescents with endocrine disorders to negative body image, but females are also at risk for negative body image that is unrelated to physical findings. Psychological and/or environmental factors that were not addressed in this study may have contributed to the female patients' negative body image.
Our findings are in partial agreement with previous studies that have demonstrated sex differences with respect to body image and self-esteem in adolescents20,21. While dissatisfaction during puberty in females has been correlated with weight22,23, dissatisfaction among males has been associated with delayed maturation3. In our study, dissatisfaction with weight was expressed by both female and male patients, but was greater in female patients. In addition, our female patients, but not male patients, had excess negative body image that was independent of physical findings.
Early puberty in girls has been reported as a risk factor for depression3,24, internalizing symptoms2 and risk-taking behavior4,17,24. However, there is also evidence that the psychosocial effects of early puberty may be short-term with resolution by adolescence25 or adulthood17. Prior to initiation of therapy, children with precocious puberty have behavioral problems and are not as socially competent as their peers20,21. However, the psychological effect of treating (and thus delaying) early puberty has not been studied. All of our patients with central precocious puberty were treated with GnRH analog, and being on GnRH analog therapy was not a predictor of body image unhappiness.
We did not observe a correlation between height and satisfaction with height, which is consistent with a growing body of literature suggesting that short children do not differ from age-matched controls on measures of self-esteem and selfperception8,10,26. Several studies have shown that short stature has minimal impact on psychological adaptation27,28, psychosocial functioning, and quality of life29 of adolescents when compared to control groups.
It is commonly assumed that the psychological well-being of overweight and obese children is impaired30, particularly in adolescent females7,31,32. Our data support this theory. Females who were unhappy with their weight and overall body build had significantly higher weight and BMI than the females who were satisfied with their weight. This finding was not replicated in the male group, but the trend was similar (unhappy patients tended to have higher BMI), suggesting that obesity is a moderator of psychological well-being in adolescent patients with endocrine disorders. The rapidity of weight gain in children may also influence their body image. Although studies regarding this topic are lacking, one might speculate that a rapid change in body weight could lead to a negative body image and may have contributed to the unhappiness expressed by the patients with CS.
While patients with CS and FMPP shave not been studied with respect to body image disturbances, there is a literature regarding patients with CAH and body image. Earlier studies of adult females with CAH found that quality of life was not impaired as compared to healthy controls, but significant impairment in body image was present33–35. Negative body image has been inferred based on studies that have shown decreased sexual activity and lack of sexual relationships in adult females with CAH. However, in a more recent study of both male and female adolescents with CAH, no difference in self-image was found between patients with CAH and controls36. High quality-of-life has also been reported in adult females with CAH, despite being socially shy and less sexually active, possibly reflecting compensatory coping mechanisms34. In our study, while over one-half of all males and females with CAH reported unhappiness with some aspect of their body, this finding is not significantly different from the patients with CS or FMPP, suggesting that having a history of ambiguous genitalia in females did not place them at higher likelihood for negative body image. Interestingly, females with CAH, unlike females with CS, did not report more unhappiness with their body build or figure more frequently than the female controls.
The reliability of pubertal self-assessment has been examined in a number of adolescent populations and the results are conflicting. Earlier studies report that healthy children with normal weight are able to accurately assess their pubertal development using standardized drawings37,38, while more recent studies suggest that these measures are not a reliable means to assess development39,40. Additionally, self-reporting is not accurate in obese and anorexic adolescents41,42 suggesting that body image may play a role. It is interesting to note that both male and female patients in our study accurately assessed their pubertal development. All of our patients were under the care of a pediatric endocrinologist, thus puberty may have been discussed at one or more prior visits. Our data suggest that pubertal self-assessment is accurate in adolescents with disorders of steroidogenesis.
There are several limitations to our study. The sample size of the patients with FMPP and CS was small; however, these are rare conditions. All of our patients are seen and followed at a clinical research center and might not accurately reflect patients seen in a more conventional patient care setting. Although the patient groups studied here were similar demographically, the healthy group did not permit control for the effects of a chronic illness.
Our data suggest that being overweight is the strongest predictor of body image disturbance in adolescents with endocrine conditions associated with abnormal growth and development. Adolescents with CAH, FMPP and CS are at risk for negative body image with respect to weight, but not height or age of appearance. Female adolescents with CAH or CS are also at risk for body image disturbances that are unrelated to their clinical findings. Further studies are needed to evaluate the psychological aspects of these 'endocrine conditions.
ACKNOWLEDGEMENTS
This research was supported in part by the Intramural Research Program of the National Institutes of Health and in part by the Congenital Adrenal hyperplasia Research, Education and Support (CARES) Foundation.
The authors thank Dr. Robert Wesley for assistance with data analysis.
REFERENCS
- 1.Graber JA, Lewinsohn PM, Seeley JR, Brooks-Gunn J. Is psychopathology associated with the timing of pubertal development? J Am Acad Child Adolesc Psychiatry. 1997;36:1768–1776. doi: 10.1097/00004583-199712000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Hayward C, Killen JD, Wilson DM, Hammer LD, Lilt IF, Kraemer HC, Haydel F, Varady A, Taylor CB. Psychiatric risk associated with early puberty in adolescent girls. J Am Acad Child Adolesc Psychiatry. 1997;36:255–262. [PubMed] [Google Scholar]
- 3.Kaltiala-Heino R, Kosunen E, Rimpela M. Pubertal timing, sexual behaviour and self-reported depression in middle adolescence. J Adolesc. 2003;26:531–545. doi: 10.1016/s0140-1971(03)00053-8. [DOI] [PubMed] [Google Scholar]
- 4.Wilson DM, Killen JD, Hayward C, Robinson TN, Hammer LD, Kraemer He, Varady A, Taylor CB. Timing and rate of sexual maturation and the onset of cigarette and alcohol use among teenage girls. Arch Pediatr Adolesc Med. 1994;148:789–795. doi: 10.1001/archpedi.1994.02170080019004. [DOI] [PubMed] [Google Scholar]
- 5.Nottelmann ED, Susman EJ, Inoff-Germain G, Cutler GB, Jr, Loriaux DL, Chrousos GP. Developmental processes in early adolescence: relationships between adolescent adjustment problems and chronologic age, pubertal stage, and puberty-related serum hormone levels. J Pediatr. 1987;110:473–480. doi: 10.1016/s0022-3476(87)80521-8. [DOI] [PubMed] [Google Scholar]
- 6.Hill AJ, Draper E, Stack J. A weight on children's minds: body shape dissatisfactions at 9-years old. Int J Obes Relat Metab Disord. 1994;18:383–389. [PubMed] [Google Scholar]
- 7.Mendelson BD, White DR. Development of self-body-esteem in overweight youngsters. Dev Psychol. 1985;21:90–96. [Google Scholar]
- 8.Ross JL, Sandberg DE, Rose SR, Leschek EW, Baron J, Chipman JJ, Cassorla FG, Quigley CA, Crowe BJ, Roberts K, Cutler GB., Jr Psychological adaptation in children with idiopathic short stature treated with growth hormone or placebo. J Clin Endocrinol Metab. 2004;89:4873–4878. doi: 10.1210/jc.2004-0791. [DOI] [PubMed] [Google Scholar]
- 9.Sandberg DE, Bukowski WM, Fung CM, Noll RB. Height and social adjustment: are extremes a cause for concern and action? Pediatrics. 2004;114:744–750. doi: 10.1542/peds.2003-1169-L. [DOI] [PubMed] [Google Scholar]
- 10.Downie AB, Mulligan 1, Stratford RJ, Bens PR, Voss LD. Are short normal children at a disadvantage? The Wessex growth study. BMJ. 1997;314:97–100. doi: 10.1136/bmj.314.7074.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cornean RE, Hindmarsh PC, Brook CG. Obesity in 21-hydroxylase deficient patients. Arch Dis Child. 1998;78:261–263. doi: 10.1136/adc.78.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merke DP, Bomstein SR. Congenital adrenal hyperplasia. Lancet. 2005;365:2125–2136. doi: 10.1016/S0140-6736(05)66736-0. [DOI] [PubMed] [Google Scholar]
- 13.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zachmann M, Prader A, Kind HP, Hafliger H, Budliger H. Testicular volume during adolescence. Cross-sectional and longitudinal studies. Helv Paediatr Acta. 1974;29:61–72. [PubMed] [Google Scholar]
- 15.Morris N, Udry R. Validation of a self-administered instrument to assess stage of adolescent development. 1 Youth Adoles. 1980;9:271–280. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- 16.Center for Disease Control. Epi InfoTM, version 3.3.2. 2000 [Google Scholar]
- 17.McCabe MP, Ricciardelli LA. A longitudinal study of pubertal timing and extreme body change behaviors among adolescent boys and girls. Adolescence. 2004;39:145–166. [PubMed] [Google Scholar]
- 18.Davison TE, McCabe MP. Adolescent body image and psychosocial functioning. 1 Soc Psychol. 2006;146:1530. doi: 10.3200/SOCP.146.1.15-30. [DOI] [PubMed] [Google Scholar]
- 19.Alsaker FD. Annotation: the impact of puberty. J Child Psychol Psychiatry. 1996;37:249–258. doi: 10.1111/j.1469-7610.1996.tb01403.x. [DOI] [PubMed] [Google Scholar]
- 20.Sonis WA, Comite F, Blue J, Pescovitz OH, Rahn CW, Hench KD, Cutler GB, Jr, Loriaux DL, Klein RP. Behavior problems and social competence in girls with true precocious puberty. J Pediatr. 1985;106:156–160. doi: 10.1016/s0022-3476(85)80489-3. [DOI] [PubMed] [Google Scholar]
- 21.Sonis WA, Comite F, Pescovitz OH, Hench K, Rahn CW, Cutler GB, Jr, Loriaux DL, Klein RP. Bio-behavioral aspects of precocious puberty. J Am Acad Child Psychiatry. 1986;25:674–679. doi: 10.1016/s0002-7138(09)60293-4. [DOI] [PubMed] [Google Scholar]
- 22.Sweeting H, West P. Gender differences in weight related concerns in early to late adolescence. J Epidemiol Community Health. 2002;56:700–701. doi: 10.1136/jech.56.9.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kearney-Cooke A. Gender differences and self-esteem. J Gend Specif Med. 1999;2:46–52. [PubMed] [Google Scholar]
- 24.Stice E, Presnell K, Bearman SK. Relation of early menarche to depression, eating disorders, substance abuse, and comorbid psychopathology among adolescent girls. Dev Psychol. 2001;37:608–619. doi: 10.1037//0012-1649.37.5.608. [DOI] [PubMed] [Google Scholar]
- 25.Ehrhardt AA, Meyer-Bahlburg HF. Psychosocial aspects of precocious puberty. Horm Res. 1994;41 Suppl 2:30–35. doi: 10.1159/000183956. [DOI] [PubMed] [Google Scholar]
- 26.Sandberg DE, Voss LD. The psychosocial consequences of short stature: a review of the evidence. Best Pract Res Clin Endocrinol Metab. 2002;16:449–463. doi: 10.1053/beem.2002.0211. [DOI] [PubMed] [Google Scholar]
- 27.Duke-Duncan P, Riner PL, Dornbusch SM, et al. The effects of pubertal timing on body image, school behavior and deviance. J Youth Adoles. 1985;14:227235. doi: 10.1007/BF02090320. [DOI] [PubMed] [Google Scholar]
- 28.Zimet GD, Owens R, Dahms W, Cutler M, Litvene M, Cuttler L. Psychosocial outcome of children evaluated for short stature. Arch Pediatr Adolesc Med. 1997;151:1017–1023. doi: 10.1001/archpedi.1997.02170470051010. [DOI] [PubMed] [Google Scholar]
- 29.Theunissen NC, Karnp GA, Koopman HM, Zwindennan KA, Vogels T, Wit 1M. Quality of life and self-esteem in children treated for idiopathic short stature. J Pediatr. 2002;140:507–515. doi: 10.1067/mpd.2002.123766. [DOI] [PubMed] [Google Scholar]
- 30.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421–440. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 31.Friedman MA, Wilfley DE, Pike KM, Striegel-Moore RH, Rodin J. The relationship between weight and psychological functioning among adolescent girls. Obes Res. 1995;3:57–62. doi: 10.1002/j.1550-8528.1995.tb00121.x. [DOI] [PubMed] [Google Scholar]
- 32.Latner JD, Stunkard AJ, Wilson GT. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obes Res. 2005;13:1226–1231. doi: 10.1038/oby.2005.145. [DOI] [PubMed] [Google Scholar]
- 33.Kuhnle U, Bullinger M, Schwarz HP, Knorr D. Partnership and sexuality in adult female patients with congenital adrenal hyperplasia. First results of a cross-sectional quality-of-life evaluation. J Steroid Biochem Mol Bioi. 1993;45:123–126. doi: 10.1016/0960-0760(93)90131-f. [DOI] [PubMed] [Google Scholar]
- 34.Kuhnle U, Bullinger M, Schwarz HP. The quality of life in adult female patients with congenital adrenal hyperplasia: a comprehensive study of the impact of genital malformations and chronic disease on female patients life. Eur J Pediatr. 1995;154:708–716. doi: 10.1007/BF02276713. [DOI] [PubMed] [Google Scholar]
- 35.Kuhnle U, Bullinger M. Outcome of congenital adrenal hyperplasia. Pediatr Surg Int. 1997;12:511–515. doi: 10.1007/BF01258714. [DOI] [PubMed] [Google Scholar]
- 36.Berenbaum SA, Korman Bryk K, Duck SC, Resnick SM. Psychological adjustment in children and adults with congenital adrenal hyperplasia. J Pediatr. 2004;144:741–746. doi: 10.1016/j.jpeds.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 37.Duke PM, Litt IF, Gross RT. Adolescents' self-assessment of sexual maturation. Pediatrics. 1980;66:918–920. [PubMed] [Google Scholar]
- 38.Berg-Kelly K, Erdes L. Self-assessment of sexual maturity by mid-adolescents based on a global question. Acta Paediatr. 1997;86:10–17. doi: 10.1111/j.1651-2227.1997.tb08822.x. [DOI] [PubMed] [Google Scholar]
- 39.Schlossberger NM, Turner RA, Irwin CE., Jr Validity of self-report of pubertal maturation in early adolescents. J Adolesc Health. 1992;13:109–113. doi: 10.1016/1054-139x(92)90075-m. [DOI] [PubMed] [Google Scholar]
- 40.Desmangles JC, Lappe JM, Lipaczewski G, Haynatzki G. Accuracy of pubertal Tanner staging self-reporting. J Pediatr Endocrinol Metab. 2006;19:213–221. doi: 10.1515/jpem.2006.19.3.213. [DOI] [PubMed] [Google Scholar]
- 41.Bonat S, Pathomvanich A, Keil MF, Field AE, Yanovski JA. Self-assessment of pubertal stage in overweight children. Pediatrics. 2002;110:743–747. doi: 10.1542/peds.110.4.743. [DOI] [PubMed] [Google Scholar]
- 42.Hick KM, Katzman DK. Self-assessment of sexual maturation in adolescent females with anorexia nervosa. J Adolesc Health. 1999;24:206–211. doi: 10.1016/s1054-139x(98)00119-0. [DOI] [PubMed] [Google Scholar]