Abstract
Background
The United States lung allocation score (LAS) allows rapid organ allocation to higher acuity patients. Although, waitlist time and waitlist mortality have improved, the costs of lung transplantation (LTx) in these higher acuity patients are largely unknown. We hypothesize that LTx in high LAS recipients is associated with increased charges and resource utilization.
Methods and Materials
Clinical and financial data for LTx patients at our institution in the post-LAS era (5/2005–2009) were reviewed with follow-up through 12/2009. Patients were stratified by LAS quartiles (Q). Total hospital charges for index admission and all admissions within 1yr of LTx were compared between Q4 versus the Q1–3 using Rank-Sum and Kruskal-Wallis tests, as charge data were not normally distributed.
Results
84 LTx’s were performed during the study period. 63 (75%) survived 1yr; 10 (11.9%) died during the index admission. Median LAS was 37.5 (interquartile range (IQR) 34.3–44.8). LAS quartiles were: Q1,30.1–34.3, n=21; Q2,34.4–37.5, n=21; Q3,37.6–44.8, n=21; Q4,44.9–94.3, n=21. Charges for index admission were: Q4,$276,668 (IQR191,301–300,156) vs. Q1–3, $153,995(IQR 129,796–176,849), P<0.001. Index admission median length of stay was greater in Q4 (Q4:35d IQR 23–46 vs Q1–3:15d IQR11–22, P=0.003). For 1yr charges: Q4, $292,247 (IQR 229,192–421,597) vs. Q1–3, $188,342 (IQR 153,455–252,045), P=0.002. Index admission and 1yr charges in Q4 were higher than other quartiles when examined individually.
Conclusions
This is the first study to show increased charges in high LAS patients. Charges for the index admission and hospital care in the year post-LTx were higher in the highest LAS quartile compared to patients in the lowest 75% of LAS.
Keywords: Lung Transplantation, Resource Utilization
Background
The lung allocation score (LAS) has shifted the demographics of United States (US) lung transplantation (LTx), with increased numbers of critically ill patients receiving LTx. Several studies have examined the impact of high LAS on post-LTx survival, although the system was not initially designed for this purpose. High LAS is known to negatively impact short-term mortality in IPF patients, and predicts decreased 1-year survival and increased postoperative complications in all LTx patients.(1–3) LTx is a resource-intensive surgical therapy requiring careful follow-up.(4–6) However, the effects of high LAS on actual resource utilization are unknown. Therefore, we used an institutional cohort of patients to test the hypothesis that high LAS is associated with increased hospital charges and resource utilization.
Methods
Patient Data
This was a retrospective review of the prospectively maintained LTx database at the Johns Hopkins Hospital. LTx patients in the post-LAS era (5/2005) were included. Patients with prior LTx and children (<18yrs) were excluded. Patients undergoing re-transplantation were excluded because prior national cohort studies examining the impact of LAS on survival have only used primary LTx recipients.(1, 3) Following institutional review board approval, relevant clinical information was extracted from the LTx database. Demographic variables included age, gender, race, cardiovascular co-morbidities, pulmonary function testing, wait-list time, and transplant diagnosis. Donor and operative information (ischemic time, cardiopulmonary bypass (CPB) and induction therapy) were included. LAS was calculated as detailed by Egan et al.,(7) and recorded for each patient. For patients with multiple LAS values, the one immediately prior to transplantation was used.
Outcomes
Postoperative data included: length of stay (LOS), in-hospital infections, rejection episodes during index hospitalization, mechanical ventilation duration, re-intubation, tracheostomy, renal replacement therapy (RRT), extra-corporeal mechanical oxygenation (ECMO), and in-hospital mortality. The Social Security Death Index was queried for survival status.
Perioperative Care
LTx was performed using standardized techniques. CPB was used only for patients with pulmonary hypertension or patients intolerant of single lung ventilation. Induction therapy was utilized at the transplant surgeon’s discretion, as well as triple immuno-suppression based on Tacrolimus, Mycophenolate Mofetil, and steroids. A standardized care pathway for the initial post-operative period was utilized in all patients and provided by a multidisciplinary team in the ICU and hospital wards. Inhaled nitric oxide is routinely initiated intraoperatively and weaned on the first postoperative day. Follow-up and outpatient care are standardized. When necessary, patients are readmitted to the Johns Hopkins Hospital.
Charges Data
Hospital charges are obtained through the billing department as reported to the Maryland State authorities, and represent all hospital charges for the index admission only, including charges incurred during the operation. Charges data are categorized as follows: Routine charges, operating room facility use, operating room supply use, pharmacy charges, laboratory charges, radiology charges, and physical therapy charges. An organ acquisition fee is unique to this patient population, and represents charges related to the organ recovery process and is included with index admission charges for all patients. This fee is determined at the beginning of each calendar year, and incurred evenly by all LTx patients in the same calendar year. For any patient hospitalized pre-LTx, index admission charges begin with the date of transplant. For patients with 1 year of follow-up, charges accumulated during all inpatient re-admissions in the first post-LTx year were compared among LAS quartiles. Financial information was inflation-adjusted according to the US Department of Labor Consumer Price Index in US dollars for 2009.
Statistical Analysis
Patients were stratified into quartiles (Q) by LAS. Differences between Q1–3 and Q4 patients were compared using two-tailed student’s t-test for normally distributed continuous variables. For nonparametric continuous data, Wilcoxon rank-sum test was used. Chi-square analysis was used for categorical variables. Continuous variables are presented with the mean±standard deviation (SD). Categorical variables are shown in whole numbers and percentages. All charges data are presented as medians with interquartile ranges (IQR), as these data were not normally distributed. To confirm a non-parametric distribution, the data were visually inspected in graphical form and checked for skewness. Wilcoxon rank-sum test compared index admission and one-year charges data between Q1–3 and Q4. To determine differences between individual quartiles, the Kruskall-Wallis non-parametric analysis of variance was used. Post-hoc testing analyzed individual differences among the quartiles. To test for an LAS threshold predictive of increased charges, receiver operating characteristic (ROC) curves were used. The outcome measure for high charges was defined as the upper 25% of index admission charges. An area under the curve (AUC) above 0.7 was deemed significant.
After logarithmic transformation of charges data, linear regression tested for a correlation between LAS and index admission charges. A multivariable linear regression model was constructed to determine the relative contributions of individual variables toward index admission charges. In addition to variables associated with charges on exploratory univariate analysis (p<0.1), those with biological plausibility were incorporated in a forwards and backwards stepwise fashion into the model. The likelihood ratio test and Akaike’s information criterion were used in a nested model approach to identify which covariates increased the explanatory power of the model. Coefficients are presented with 95% confidence intervals (CI). The final model incorporated: LAS, pre-LTx intensive care unit (ICU), ventilation time, tracheostomy, RRT, inhospital infection, and in-hospital mortality.
Postoperative complications were compared between Q1–3 and Q4. 1-year survival was estimated using the Kaplan-Meier method, and the log-rank test compared survival by LAS quartiles. P-values≤0.05 were considered significant. Analysis was performed using Stata v9.2 (StataCorp, College Station, Texas).
Results
Cohort Statistics
Between 5/2005 and 6/2009, 84 patients received LTx at our institution. The mean age was 49±13years with 47% females (n=40). Recipient race distribution was:81% Caucasian (n=68), 17% African American (n=14), and 2% Hispanic (n=2). Diagnoses were: Chronic obstructive pulmonary disease (COPD) in 25 (29.7%), idiopathic pulmonary fibrosis (IPF) in 18 (21.4%), cystic fibrosis (CF) in 16 (19.0%), primary pulmonary hypertension in 4 (4.7%), bronchiolitis obliterans syndrome in 6 (7.1%), sarcoidosis in 5 (6.0%), and other in 10 (11.9%) of patients. 73 (87%) patients received bilateral LTx (BLTx). 19 (23%) patients’ required ICU care pre-LTx. The majority of patients (67%) received induction immunotherapy with daclizumab (Zenapax, Hoffmann-LaRoche Inc, Nutley, NJ). Median wait-list time was 70 (IQR:19–527) days. During the study, the number of adult LTx’s remained constant, ranging from 14–21 LTx’s annually.
LAS results
Mean LAS for the entire cohort was 42.5 (±14.4). LAS quartiles were: Q1, 30.1–34.3, n=21; Q2, 34.4–37.5, n=21; Q3, 37.6–44.8, n=21; Q4, 44.9–94.3, n=21. Baseline demographic information was compared between Q1–3 and Q4 (Table 1). Patients in Q4 had shorter wait-list times and were more likely to require pre-LTx ICU care, have diabetes mellitus, and had higher oxygen requirements. Predicted forced expiratory volume in 1 second (FEV1) was lower in Q1–3. Ischemia time was similar in both groups, as were all examined donor characteristics.
Table 1.
| Variables | Q 1–3 (N=63) | Q 4 (N=21) | P-value |
|---|---|---|---|
| Demographic Information | |||
| Mean age, years (SD) | 44.8 (14.1) | 50.6 (12.9) | 0.08 |
| Male gender, # (%) | 30 (47) | 14 (67) | 0.1 |
| Diabetes mellitus, # (%) | 8 (13) | 7 (33) | 0.04 |
| Coronary artery disease, # (%) | 1 (1.6) | 0 (0) | 0.6 |
| BMI, kg/cm2 (SD) | 23.7 (4.6) | 24.8 (5.2) | 0.4 |
| Hypertension, # (%) | 17 (27) | 4 (20) | 0.5 |
| Creatinine, mg/mol (SD) | 0.8 (0.2) | 0.9 (0.3) | 0.1 |
| O2 requirement, L/min | 2.9 (1.6) | 8.0 (6.4) | <0.001 |
| FEV1, % predicted (SD) | 30.4 (24.7) | 43.8 (23.2) | 0.04 |
| FVC, % predicted (SD) | 44.7 (14.2) | 50.2 (22.0) | 0.2 |
| ICU prior to LTx, # (%) | 5 (8) | 14 (67) | <0.001 |
| Primary Diagnosis | |||
| COPD | 25 (40%) | 0 (0) | 0.01 |
| Idiopathic pulmonary fibrosis | 12 (19%) | 6 (29%) | 0.4 |
| Cystic Fibrosis | 10 (16%) | 6 (29%) | 0.2 |
| Sarcoidosis | 2 (3%) | 3 (14%) | 0.1 |
| Primary pulmonary hypertension | 2 (3%) | 2 (10%) | 0.2 |
| Other | 12 (19%) | 4 (19%) | 0.9 |
| Transplant/Donor Variables | |||
| Donor age, years (SD) | 42.1 (15.3) | 42.1 (14.3) | 0.9 |
| Donor smoking history, # (%) | 27 (43.5) | 12 (57.1) | 0.5 |
| Left lung ischemic time, minutes (SD) | 235 (88) | 275 (98) | 0.08 |
| Right lung ischemic time, minutes (SD) | 194 (81) | 231 (72) | 0.08 |
| Bilateral LTx, # (%) | 55 (87) | 18 (86) | 0.9 |
| Median wait list time, days(IQR) | 133 (30–677) | 24 (7–149) | 0.006 |
Outcomes and Survival
Mean follow-up was 19±14months. Re-admission rates between Q4 and Q1–3 were similar. Q4 patients had longer median hospital and ICU LOS; patients in Q4 also had longer duration of mechanical ventilation, more re-intubations, and greater need for tracheostomy. No difference was seen for RRT, in-hospital infections, or in-hospital mortality (Table 2).
Table 2.
Postoperative Outcomes According to LAS Group
| Variables | Q 1–3 (N=63) | Q 4 (N=21) | P-value* |
|---|---|---|---|
| Median hospital LOS, days (IQR) | 15 (11–22) | 35 (23–46) | 0.003 |
| Median ICU LOS, days (IQR) | 3 (2–4) | 6 (3–15) | 0.01 |
| Readmissions, # (±SD) | 3.4 (±2.9) | 3.3 (±2.2) | 0.9 |
| In-hospital treated rejection, # (±SD) | 1 (±1.6) | 0 (±0) | 0.6 |
| In-hospital infection, # (%) | 38 (60%) | 16 (76%) | 0.1 |
| Median time of mechanical ventilation, hrs (IQR) | 31 (21–41) | 43 ( 29–121) | 0.05 |
| Re-intubation, # (%) | 8 (12%) | 7 (35%) | 0.02 |
| Tracheostomy, # (%) | 9 (14%) | 7 (33%) | 0.03 |
| Renal replacement therapy, # (%) | 10 (16%) | 4 (19%) | 0.7 |
| In-hospital mortality, # (%) | 8 (12%) | 2 (10%) | 0.7 |
P value based on results of either one-way student’s t-test(continuous variables) or Chi-square test(categorical variables)
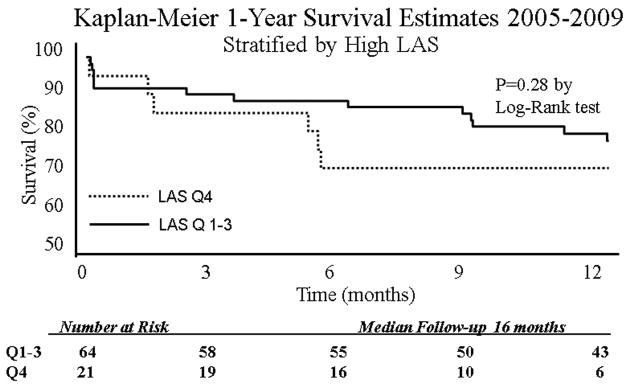
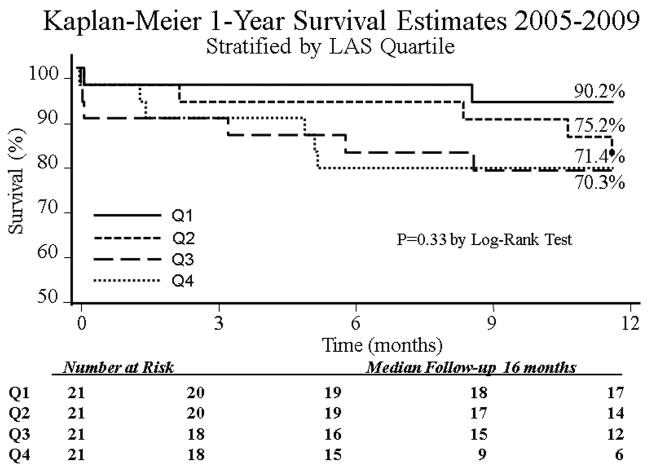
During the study, 27 (32.1%) patients died and 17 (20.2%) patients did not survive one year. When the cohort was analyzed without stratification, overall 1-year survival was 76.2%. After stratification by Q1–3 versus Q4 there was no difference in 30-day, 90-day, or 1-year KM survival. However, there was a trend toward improved survival in Q1–3 (Figure 1). Further division into individual LAS quartiles revealed no significant survival differences, however a trend toward improved 1-year survival was evident for Q1 patients (90.2% versus 71.4% for Q4) (Figure 2).
Figure 1.
Kaplan Meier Estimates of 1-Year Survival Stratified by LAS Q1–3 Versus LAS Q4. By Log-Rank analysis, survival was similar between the two groups.
Figure 2.
Kaplan Meier Estimates of 1-Year Survival Stratified by Individual Quartiles. By Log-Rank analysis, survival was improved in Q1 patients (90% 1-yr survival) compared to the remaining three quartiles (p<0.05).
Hospital Charges
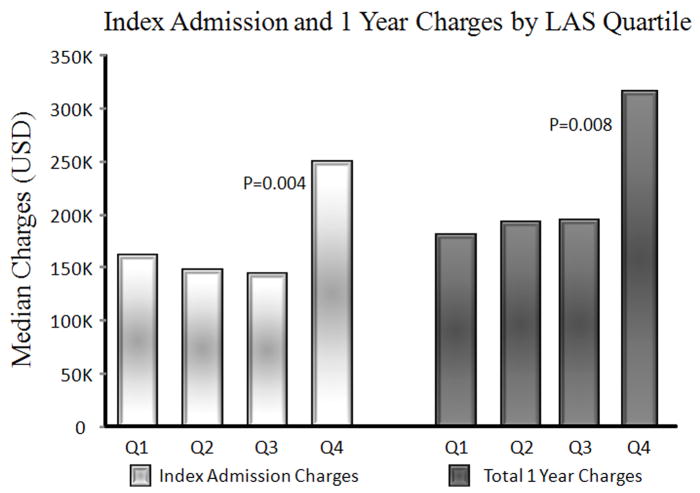
Median index admission charges were higher in LAS Q4 patients: $276,668 (IQR191,301–300,156) for Q4 compared with $153,995 (IQR129,796–176,849) for Q1–3, p<0.001 (Figure 3). Median index admission charges for individual quartiles are listed in Table 3). Total median 1-year hospital charges were greater in Q4 patients: $316,213 (IQR: 245,794–469,006 for Q4 versus $190,261 (IQR: 153,455–240,364) for Q1–3, p=0.002. After excluding index admission charges, there was no difference in median 1-year hospital charges between the two groups: $44,657 (IQR: 9,041–123,369) for Q4 compared to $27,875 (IQR: 13,831–7,160), p=0.3. Among patients who died within one year, there was no difference in total charges when comparing Q4 to Q1–3. When examining individual LAS quartiles, Q4 patients had significantly higher index admission charges compared with all other quartiles. There were no differences among Q1, Q2, or Q3 when analyzing index admission charges.
Figure 3.
Breakdown of Median Charges According to LAS Quartile. Rank-sum comparison showed index admission and total 1-year charges were higher for LAS Q4 patients compared with LAS Q1–3 patients (p=0.004 for Index Admission and p=0.008 for Total 1-year charges).
Table 3.
Median Charges Values According to LAS Quartile
| Charges Information | Quartile 1 (N=21) | Quartile 2 (N=21) | Quartile 3 (N=21) | Quartile 4 (N=21) | P-Value* |
|---|---|---|---|---|---|
| Index Admission, USD (IQR) | $160,170 (141,480–169,378) | $147,756 (121,846–181,851) | $153,995 (129,796–172,597) | $276,668† (191,301–300,156) | 0.003 |
| 1-Year Without Index Admission, USD (IQR) | $33,661 (20,760–93,179) | $14,351 (6,491–48,942) | $43,686 (19,618–71,650) | $44,657 (9,041–123,369) | 0.3 |
| Total 1-Year, USD (IQR) | $190,876 (164,613–264,606) | $181,408 (141,174–252,045) | $192,215 (163,935–240,364) | $292,247† (229,192–421,597) | 0.02 |
P-value based on results of Kruskall-Wallis non-parametric ANOVA
Individual pairwise post-hoc comparison by rank-sum after non-parametric Kruskall-Wallis ANOVA P<0.05(reference=Quartile 1)
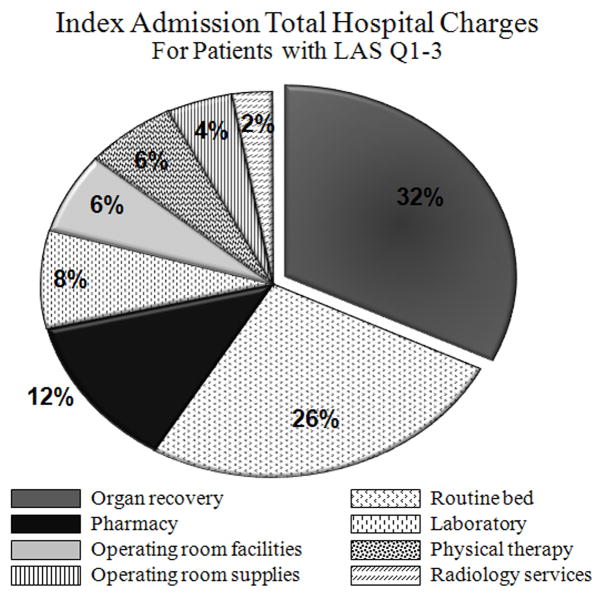
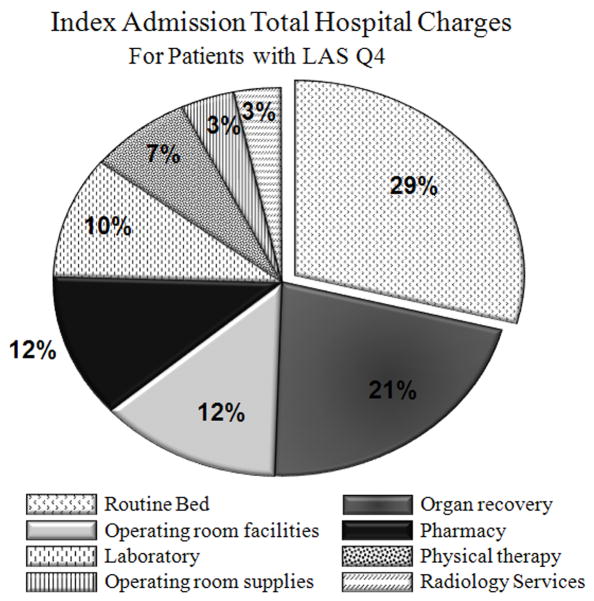
For LAS Q4 and Q1–3, the relative contributions of each charge category to total index hospitalization charges are depicted in Figures 4 and 5. Hospital charges according to category were compared between LAS Q4 and Q1–3. When analyzing index admission charges only, the following categories were higher for LAS Q4: OR supplies charges, OR facilities charges, routine ward and ICU care, pharmacy charges, and laboratory services. There was no difference in radiology or physical therapy services.
Figure 4.
Pie Chart Depicting Charges by Category for LAS Q1–3
Figure 5.
Pie Chart Depicting Charges by Category for LAS Q4
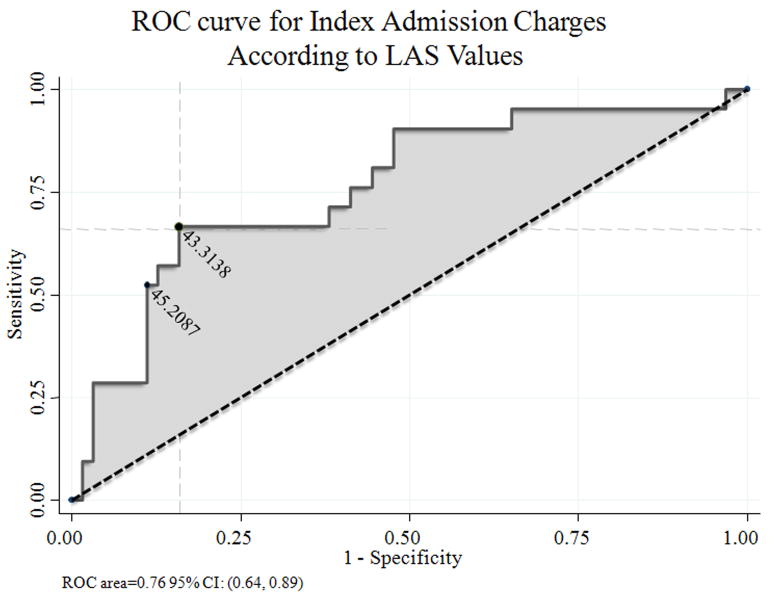
Area under the ROC curve was 0.76 (95% CI: 0.64–0.89) (Figure 6). An LAS of 43.314 had the best discriminatory power for predicting the upper 25% of index admission charges, with sensitivity of 67% and specificity 84%. Adjusting the LAS threshold to 45.2 achieved a specificity of 88% but decreased sensitivity to 54%.
Figure 6.
ROC Curve for Increased Index Admission Charges (Upper 25% of Index Admission Charges). Area under the curve was 0.76 (95% CI:0.64–0.89). An LAS of 45.2 had 88% specificity and 54% sensitivity for predicting outcome of interest.
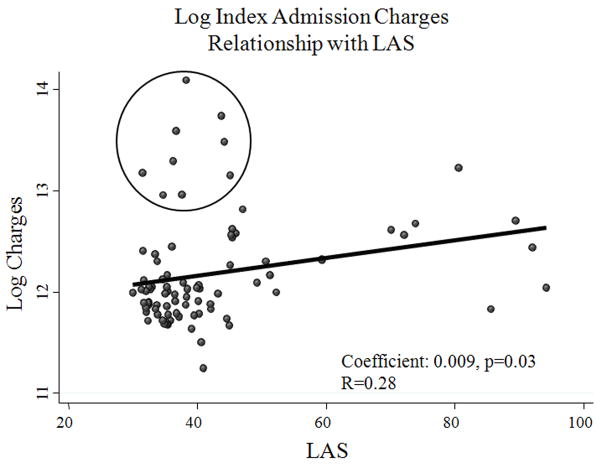
Linear Regression Analysis
Linear regression of charges data after logarithmic transformation revealed a positive correlation between LAS and index admission charges (coefficient: 0.009, 95%CI 0.001–0.017, p=0.03), with a Spearman r-value of 0.28 (Figure 7). Similarly, there was a positive correlation between LAS and 1-year charges including index admission (coefficient: 0.010, 95%CI 0.001–0.020, p=0.04), with a Spearman r-value of 0.23. Following adjustment with multivariable linear regression, ICU pre-LTx (coefficient: 0.22, 95% CI 0.001–0.44, p=0.05), duration of mechanical ventilation postoperatively (0.004, 95% CI 0.002–0.005, p<0.001), RRT (0.41, 95% CI 0.11–0.69, p<0.006), and tracheostomy (0.61, 95% CI 0.36–0.84, p<0.001) were significantly associated with index admission charges (Table 4).
Figure 7.
Scatter Plot of Log Linear Index Admission Charges According to LAS. There was a significant positive correlation (0.009, p=0.03), however weak goodness of fit for the linear model with spearman’s R-value=0.28.
Table 4.
Results of Linear Regression Analysis
| Variable | Coefficient | 95% CI | P-Value |
|---|---|---|---|
| Univariate* | |||
| LAS | 0.009† | 0.001–0.017 | 0.03 |
| Multivariable† | |||
| LAS | −0.002 | −0.009–0.004 | 0.4 |
| ICU before LTx | 0.23 | 0.00–0.46 | 0.05 |
| Duration of mechanical ventilation, hrs | 0.001 | 0.001–0.003 | 0.006 |
| Tracheostomy | 0.61 | 0.36–0.84 | <0.001 |
| Renal Replacement Therapy | 0.41 | 0.11–0.69 | <0.006 |
| In-hospital infection | 0.11 | −0.04–0.26 | 0.2 |
| In-hospital mortality | −0.19 | −0.48–0.09 | 0.2 |
P-value based on univariate Cox proportional hazards analysis
P-value based on multivariable Cox proportional hazards regression. The final model incorporated the following covariates: LAS, ICU before LTX, duration of mechanical ventilation, tracheostomy, renal replacement therapy. In-hospital infection, and in-hospital mortality
Discussion
This is the first study to evaluate the impact of high LAS on hospital charges and resource utilization. The analysis included 84 consecutive LTx recipients at our institution since inception of the LAS in 2005. Because high LAS patients are known to have worse 1-year survival and more complications (1, 3), we hypothesized that these patients would also incur greater hospital charges. Indeed, index admission charges were significantly greater in the highest quartile LAS patients. However, only a weak linear relationship between LAS and index admission charges was detected, and thus the LAS is an imperfect tool for predicting increased charges.
As would be predicted, patients in Q4 differ in clinical characteristics from Q1–3. Consistent with other reports, Q4 patients were more likely to have diabetes mellitus, require pre-LTx ICU care, and had higher pre-LTx oxygen requirements.(1, 8) Consistent with one of the aims of the LAS, wait-list times were inversely correlated with LAS, as Q4 patients had shorter wait-list times by 109 days than Q1–3 patients.
Q4 patients had twice the median duration of hospitalization and ICU stays, as well as longer durations of mechanical ventilation post-LTx, higher reintubation rates, and greater need for tracheostomy. In contrast with large national cohort studies, no significant differences were found in 1-year survival.(1, 3) Though a trend toward improved survival in Q1 patients was present, this study was under-powered to detect significant survival differences.
Charges Analysis
Although Q4 patients had significantly higher index admission and total 1-year charges, there was no difference in 1-year charges when index admission charges were excluded. Readmission rates were similar among the groups. Together these findings suggest greater resource utilization in the peri-operative period for Q4 patients, although long-term utilization appears to be equivalent among all LTx recipients.
Because the focus of this study was to evaluate charges associated with LTx, all preoperative charges for patients hospitalized prior to LTx were omitted. We surmise that high LAS patients also incur higher hospital charges pre-LTx, but this was not examined in our study. For many critically ill patients in the upper quartile of LAS, transplantation represents the only viable option for improved survival and quality of life. The charges associated with caring for high LAS patients who never receive LTx are unknown, but are likely to be high, as these patients frequently require repeat hospitalizations with assisted ventilation and ICU care.
A detailed breakdown of hospital charges according to category yielded interesting results. Higher pharmacy and laboratory charges for Q4 patients are likely a function of their greater LOS. Increased OR charges for Q4 patients likely reflects longer intraoperative times and increased use of cardiopulmonary bypass in these patients. We would have expected Q4 patients to have poorer preoperative conditioning and therefore incur higher physical therapy charges postoperatively. However, this was not the case, likely because all LTx patients undergo vigorous postoperative physical therapy regimens and are admitted to a dedicated rehabilitation ward liberally.
Regression Analysis
Univariate linear regression showed LAS to have a positive correlation with index admission charges, albeit with a small coefficient. The low r-value suggests that LAS has only a weak linear relationship with hospital charges. On multivariable analysis, pre-LTx ICU care was the only preoperative variable associated with increased charges. This finding was expected as patients requiring pre-operative ICU care were eight times more likely to be in Q4. None of the charges associated with pre-LTx ICU care were included, suggesting that pre-LTx ICU is a strong marker of acuity which portends high post-LTx charges.
Not surprisingly, the need for post-LTx RRT was correlated with increased charges. For all patients needing renal replacement in this series, continuous RRT was used due to hemodynamic instability, which has been previously reported to have increased charges compared to intermittent RRT.(9) Duration of mechanical ventilation and tracheostomy were other predictors of increased charges in the multivariable model. The association between LAS and increased charges on univariate analysis was no longer evident in the multivariable model. However, as Q4 patients had longer duration of mechanical ventilation, we suspect the added charges associated with mechanical ventilation likely mask any detectable independent effect of LAS on hospital charges in the multivariable model.
An LAS threshold of approximately 45 was most predictive of increased index admission charges; previous reports using UNOS data have cited an LAS above 46 is associated with decreased 1-year survival.(1) This suggests a potential threshold for worse outcomes and increased resource utilization at an LAS of 45–46. However, patients with los LAS occasionally have high charges, as 9 (14%) patients in Q1–3 incurred index admission charges above the 75th percentile. Examining these 9 patients by diagnosis revealed 3 COPD, 3 IPF, 1 primary pulmonary hypertension, and 2 bronchiolitis obliterans syndrome.
Previous Work
Few studies have examined resource utilization in LTx, but no formal study has been published since inception of the LAS. The first US study was performed by Ramsey et al. in 1995, reporting average charges of nearly $165,000 in their first 25 LTx recipients.(5) Life expectancy was similar between wait-list patients versus LTx recipients, however quality-adjusted life years (QALY) were improved in LTx recipients. This led to the conclusion that LTx patients highly value improved quality of life derived from undergoing transplantation.
Gartner et al. published a single institutional review in 1997 of 20 LTx recipients, describing average charges of $154,000, and determining the survival gain from surgery must be 2.7 years to justify LTx from a societal perspective.(4) After adjusting for interval inflation differences, average charges published by Ramsey and Gartner were $216,000 and $232,000, respectively, which are greater than our findings for Q1–3 however are less than Q4. Thus, although the LAS era has improved waitlist mortality, patients who receive preferential allocation of organs with high LAS have greater hospital charges.
Obtaining data from 7 LTx centers in the United Kingdom, Anyanwu et al. published the largest multi-institutional study to examine cost-utility post-LTx.(10) Their study revealed the mean cost for a single LTx was $177,000, with additional costs of $48,000per QALY. The authors determined the cost-effectiveness of LTx could be improved with reduced rejection drug costs and improved quality of life post-LTx. A Canadian study by Vasiliadis et al. reached similar findings, with LTx patients realizing greater QALY’s.(6) Our study builds on the few previous studies by detailing charges according to category, and by examining the impact of high LAS on resource utilization.
Limitations
A limitation of this study is the use of hospital charges as a surrogate index for cost. However, the unique structure for medical reimbursement in the State of Maryland neutralizes this issue. A multi-institutional study across many states cannot be easily performed because of variable payments rates. To contain costs, the Maryland Health Services Cost Review Commission (HSCRC) determines payment rates for insurers—both private and public—including Medicare and Medicaid within Maryland hospitals. Thus, the common practice of “cost shifting” by overcharging privately insured patients is absent. The authors’ institution HSCRC rate for charge payment has been cost + 1−3% over the study interval. Accordingly, we believe this study represents the most accurate assessment of charges associated with LTx to date.
Conclusions
This is the first study to rigorously review the impact of LAS on hospital charges and resource utilization after LTx. Patients in the highest LAS quartile had significantly increased index admission and total 1-year hospital charges, as well as greater lengths of stay, when compared to patients in the lower 75% of LAS. However, the increased expenses appear to be confined to the index admission only. These results illuminate the increased charges and resource utilization associated with the transplantation of high LAS patients.
Acknowledgments
The authors would like to thank Jenna Pearce, BA, for her assistance managing the lung transplant database at the Johns Hopkins Hospital. Dr. Arnaoutakis is the Irene Piccinini Investigator in Cardiac Surgery and Dr. Allen is the Hugh R. Sharp Cardiac Surgery Research Fellow. No author has any relevant financial disclosures or relationships.
Footnotes
Presented at: Plenary Session, Saturday April 24th, 2010, Thirtieth annual meeting for International Society of Heart and Lung Transplantation, Chicago, Illinois
Conflicts: The authors have no conflicts of interest to disclose.
References
- 1.Merlo CA, Weiss ES, Orens JB, et al. Impact of U.S. Lung Allocation Score on survival after lung transplantation. J Heart Lung Transplant. 2009;28:769–775. doi: 10.1016/j.healun.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 2.Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS. Lung allocation score predicts survival in lung transplantation patients with pulmonary fibrosis. The Annals of thoracic surgery. 2009;88:1757–1764. doi: 10.1016/j.athoracsur.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Russo MJ, Iribarne A, Hong KN, et al. High lung allocation score is associated with increased morbidity and mortality following transplantation. Chest. 2010;137:651–657. doi: 10.1378/chest.09-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gartner SH, Sevick MA, Keenan RJ, Chen GJ. Cost-utility of lung transplantation: a pilot study. J Heart Lung Transplant. 1997;16:1129–1134. [PubMed] [Google Scholar]
- 5.Ramsey SD, Patrick DL, Albert RK, Larson EB, Wood DE, Raghu G. A pilot study. Vol. 108. University of Washington Medical Center Lung Transplant Study Group Chest; 1995. The cost-effectiveness of lung transplantation; pp. 1594–1601. [DOI] [PubMed] [Google Scholar]
- 6.Vasiliadis HM, Collet JP, Penrod JR, Ferraro P, Poirier C. A cost-effectiveness and cost-utility study of lung transplantation. J Heart Lung Transplant. 2005;24:1275–1283. doi: 10.1016/j.healun.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Egan TM, Murray S, Bustami RT, et al. Development of the new lung allocation system in the United States. Am J Transplant. 2006;6:1212–1227. doi: 10.1111/j.1600-6143.2006.01276.x. [DOI] [PubMed] [Google Scholar]
- 8.Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS. Survival after single versus bilateral lung transplantation for high-risk patients with pulmonary fibrosis. The Annals of thoracic surgery. 2009;88:1616–1625. doi: 10.1016/j.athoracsur.2009.06.044. discussion 1625–1616. [DOI] [PubMed] [Google Scholar]
- 9.Srisawat N, Lawsin L, Uchino S, Bellomo R, Kellum JA, BESTKI T. Cost of acute renal replacement therapy in the intensive care unit: results from The Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Study. Critical care (London, England) 2010;14:R46. doi: 10.1186/cc8933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anyanwu AC, McGuire A, Rogers CA, Murday AJ. An economic evaluation of lung transplantation. The Journal of thoracic and cardiovascular surgery. 2002;123:411–418. doi: 10.1067/mtc.2002.120342. discussion 418–420. [DOI] [PubMed] [Google Scholar]