Abstract
This case report describes the development and implementation of the Train-the-Trainer: Maternal Depression Screening Program (TTT), a novel approach to disseminating perinatal depression screening. We trained screeners according to a standard pyramid scheme of train-the-trainer programs: three experts trained representatives from health care agencies (the TTT trainers), who in turn trained their staff and implemented depression screening at their home agencies. The TTT trainers had little or no prior mental health experience so “enhanced” components were added to ensure thorough instruction. Although TTT was implemented primarily as a services project, we evaluated both the statewide dissemination and the screening rates achieved by TTT programs. Thirty-two social service or health agencies implemented maternal depression screening in 20 counties throughout Iowa; this reached 58.2% of the Iowa population. For the 16 agencies that provided screening data, the average screening rate (number of women screened/number eligible to be screened) for the first 3 months of screening was 73.2%, 80.5% and 79.0%. We compared screening rates of our TTT programs with those of Healthy Start, a program in which screening was established via an intensive consultation model. We found the screening rates in 62.5% of TTT agencies were comparable to those in Healthy Start. Our “enhanced” train-the-trainer method is a promising approach for broadly implementing depression-screening programs in agencies serving pregnant and postpartum women.
Keywords: Screening, Perinatal depression, Dissemination, Train-the-trainer
Introduction
Perinatal depression affects approximately 19% of pregnant and postpartum women [1], with symptoms including fatigue, cognitive impairment, and loss of interest and motivation. These symptoms not only diminish mothers’ capacity for sensitive parenting [2], but also place infants at risk for broad developmental delays [3]. Several recent public health initiatives have promoted early identification and treatment of depression during pregnancy and the postpartum period: New Jersey legislation mandated screening for maternal depression [4]; a national home-visiting program for low-income mothers similarly mandated screening [5]; multiple “position statements” by professional health care organizations have also advocated screening [6, 7]; moreover, in 2009, the incoming president of the American College of Obstetricians and Gynecologists announced perinatal depression as his presidential initiative [8].
Because informal clinical assessments fail to identify depressed women [9], reliable systematic screening is recommended by the U.S. Preventive Services Task Force [10]. Maternal and child health programs and primary care clinics are ideally situated to implement perinatal depression screening and referral; however, lack of training often leaves them unprepared to perform this essential role [11, 12].
To educate providers, several instructional approaches have been developed. In the U.S., educational approaches include face-to-face group training [13], web-based resources [14, 15], and one-to-one professional consultation [16-18]; each has limitations. Although face-to-face group and web-based training can occur on a large scale, they address a general audience and lack the guidance needed to tailor screening programs. In contrast, one-to-one training addresses individual agency needs, but is costly. In the U.K., perinatal depression screening programs have been disseminated via a train-the-trainer approach [19]. Although this approach is effective, it still included local training delivered by a professional, which is often not feasible in the U.S.
The opportunity to develop and disseminate a novel train-the-trainer program arose when numerous maternal and child health agencies in Iowa requested one-to-one professional consultation to help them plan and implement perinatal depression screening. These requests emerged after perinatal depression screening had been implemented in the State’s Healthy Start program; unfortunately, the Healthy Start one-to-one training approach was impractical because the agencies were numerous and widely distributed. We developed an “enhanced” train-the-trainer approach—the Maternal Depression Screening: Train-the-Trainer Program, or TTT—to teach this new screening practice to health and social service professionals with limited or no background in mental health.
We describe the development and dissemination of this enhanced train-the-trainer program. Additionally, we report on how successful these agencies were in putting the program into practice.
Method
TTT: Program Description
TTT combines aspects of a standard train-the-trainer and one-to-one professional consultation approach. Like the standard train-the-trainer approach, our core team of experts in perinatal depression educated representatives from outside agencies to become trainers for their agencies’ staff. Nevertheless, two “enhanced components” were also added to TTT. First, in standard train-the-trainer programs, trainers typically attend workshops and then use the workshop materials to train their own staff. In contrast, the TTT program required trainers to develop their own training materials with one-to-one consultation from the core team of perinatal depression experts. Second, in standard train-the-trainer programs, training provided by the experts is usually limited to the first days of the workshop. In the TTT program, in contrast, the core team of perinatal depression experts consulted one-to-one with trainers, together working to tailor the screening protocols for their own agencies. The core team also maintained contact during the initial stages of the implementation process. Table 1 summarizes the TTT training cycle. The description, rationale, and procedures for the “enhanced” program components are described here.
Table 1.
TTT training cycle
| Workshop #1 (Month 1) |
|
| Trainer Assignments following Workshop #1 (Months 1–4) |
|
| Workshop #2 (Month 4) |
|
| Trainer Assignments following Workshop #2 |
|
| Upon completion (variable timing 6–9 months) |
|
All participating agencies were required to use the EPDS, a 10-item scale validated for use with perinatal women as well as a cutoff score of ≥12
Rogers’ Diffusion of Innovations Theory was used as a lecture framework as this theory emphasizes two key y points: implementation of an innovation is not likely to be immediate and staff will vary in their willingness to adopt a new practice
Perinatal Depression Slides
Trainers were typically social workers, nurses, or other health professionals, who were not necessarily knowledgeable about perinatal depression prior to attending the workshop. Attending one workshop about perinatal depression did not seem to be sufficient preparation to begin providing training. Our experts therefore provided trainers with PowerPoint slide templates and supplementary informational brochures. Using these materials, which were developed specifically for this services project, trainers developed their own set of four lectures; this reinforced their familiarity with the material in preparation for providing their own trainings on this topic.
The Power Point templates were four sets of slides, one for each curriculum topic (Table 1). Each slide included a “slide title” and a “notes section” describing what information to add to the slide. Trainers filled in the slide, guided by the title, the notes, and supplemental brochures containing easy-to-understand summaries of current research on perinatal depression. The templates minimized the time required to develop their own presentations and ensured that they would present uniform material to their own staff. Expert mentors checked the slides for accuracy; inaccurate slides were corrected by the trainer, and returned to the mentor for review.
Depression Screening Protocol
Two elements of each agency’s screening protocol were standardized: the screening tool and the cutoff score. All agencies were required to use (1) the Edinburgh Postnatal Depression Scale (EPDS), a 10-item, self-report scale for pregnant and postpartum women [20] and, (2) a cutoff score of 12 or greater. Because the participating agencies were diverse, other aspects of the screening protocols were tailored to the individual agency. Trainers and their agency supervisors collaboratively developed the protocols, tailoring them using a structured set of questions on a “Question/Answer”-style worksheet as a guide (e.g., “who will implement the screening?” and “when will clients be screened?”). Through this process, trainers and supervisors developed a screening protocol that indicated who would provide the screening, the screening schedule, a list of referrals, and emergency procedures.
One-to-one Consultation
Throughout the program, TTT mentors—all experts in perinatal depression—worked with trainers individually, providing feedback on the trainers’ training slides and the agencies’ screening protocols. While trainers were developing their materials, mentoring occurred via email. After trainers completed their assignments, mentors, trainers, and supervisors had a one-hour teleconference to finalize plans for training the agency staff and address any concerns regarding implementation.
Participants
Across three TTT cycles (2005–2008), 42 individuals were trained from 32 agencies, in 20 counties in Iowa and one in Missouri (Table 2). Some agencies sent more than one participant. Although all 32 agencies reported that they had implemented screening in their program, 16 provided 3 months of data on screening rates after screening had been implemented. Before enrollment in TTT, none of these 16 agencies systematically screened women for depression.
Table 2.
Breakdown of trainers and agencies for three TTT cycles
| TTT cycle | Number of trainers | Number of new agenciesa |
Number of agencies with complete data for research purposes |
|---|---|---|---|
| TTT-1 | 14 | 14 | 3 |
| TTT-2 | 15 | 11 | 6 |
| TTT-3 | 13 | 7 | 7 |
| Total | 42 | 32 | 16 |
Some agencies participated in more than one TTT cycle in order to have multiple trainers available to train new staff
Procedure
Recruitment
With help from the staff at the Iowa Department of Public Health Early Childhood Program, TTT was advertised to maternal and child health agencies throughout Iowa. The descriptive materials listed two eligibility criteria: prospective TTT trainers needed the written support of the agency supervisor and a bachelor’s degree. Interested agencies could request an exception to the educational requirement, primarily in hospital settings where agency supervisors believed that experienced LPN staff could implement the screening program. In all instances except one—in which no other staff member other than an LPN level staff was interested in the program—non BA trainers were paired with BA level trainers from the same agency.
TTT Workshops, Assignments, and Screening Implementation
For each TTT cycle (Table 1), trainers attended Workshop 1, were assigned an expert mentor, and completed the trainer assignments. Three months later, trainers attended Workshop 2 and completed a second set of assignments. Typically 2 to 3 months after Workshop 2, trainers teleconferenced with their mentor and supervisor. All TTT workshops were held in Des Moines, a centrally located city with the largest population in Iowa. Once trainers completed all program requirements, they trained their staff and implemented maternal depression screening in their agencies. For trainer hours and travel expenses, the agencies were compensated $350 when all certificate requirements were completed. Agencies received an additional $150 when they provided 3 months of screening data.
Evaluation
All research procedures were approved by the University’s Institutional Review Board. At the beginning of each TTT training cycle, trainers were invited to participate in the study by giving their consent for the use of TTT evaluation materials for research purposes. All TTT participants were eligible to participate in the research evaluation component. The data gathered enabled us to assess both the scope of dissemination and the effectiveness of implementation.
Scope of Dissemination Four variables quantified dissemination: (1) the number of trainers; (2) the number of agencies that established screening via the TTT program; (3) the geographic dispersion of TTT screening programs; and (4) the estimated population coverage (EPC), which indexed the scope of dissemination. The EPC was calculated using the TTT agency zip codes, which revealed the percentage of the Iowa population within a 20 mile radius [21]. A 20 mile radius captures 90% of patient admissions [22], and was thus used to determine the EPC of an agency.
Effectiveness of Screening: Screening Rate The screening rate was defined as the number of women screened/number of women eligible to be screened. Thus a screening rate of 100% means that all eligible women were screened. Eligibility for screening was agency specific and defined as the women that the agency indicated would be screened in their screening protocol. The screening rate data for each of the 16 agencies that provided data were obtained from the returned “screening tracking form.” On this form, agencies reported the following three variables for 3 months: (1) the number of women eligible for screening during a given month, (2) the number of women who completed the EPDS at least once during that month, and (3) their EPDS scores.
Results
Scope of Dissemination
Number of Trainers and Agencies
Across three cycles, 42 trainers completed the TTT program. All 32 agencies whose trainer/s completed TTT also implemented a depression screening program (see Table 2 for breakdown of TTT agencies across the 3 cycles). The participating agencies were broadly categorized as either primary health care or social service.
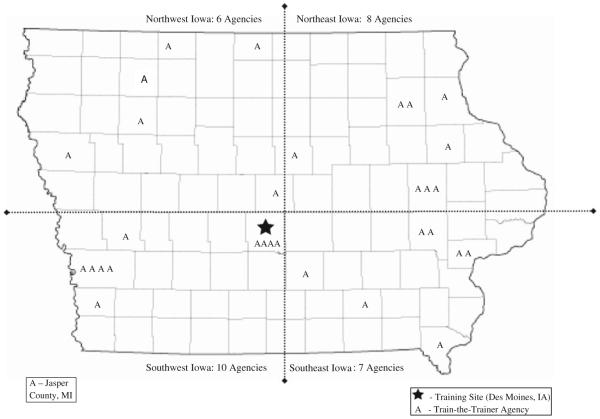
Geographic Dispersion of TTT Agencies and Population Coverage
The geographical distribution of the 32 screening programs (Fig. 1) indicates that they were established in 20 counties throughout Iowa, with one program near the Missouri border. Because some agencies shared the same zip code, estimates of the population covered were based on 26 of the 32 TTT agencies with unique zip codes. The cumulative results of the maximal coverage calculation, presented for each of the three TTT program cycles (Table 3), indicate the 26 TTT agencies with unique zip codes cover 1,705,539 people, or 58.2% of the Iowa population (Table 3).
Fig. 1.
Scope of dissemination
Table 3.
Estimated population coverage (EPC) of TTT agencies
| TTT training cycles | Number of TTT agencies |
Cumulative number of TTT agencies w/unique Zipcodes |
Cumulative EPC number (percent) of Iowans |
|---|---|---|---|
| TTT-1 | 14 | 13 | 1,079,278 (36.83) |
| TTT-II | 11 | 22 | 1,496,950 (51.09) |
| TTT-III | 7 | 26 | 1,705,539 (58.21) |
Effectiveness of Screening Implementation: Screening Rates
Agency Screening Rates
The screening rates for the 16 TTT programs providing data are listed in Table 4. Across all 16 agencies, in the first month of implementing screening, rates ranged from 0 to 100% (mean = 73.2%). During month two, rates ranged from 10 to 100% (mean = 80.5%). During month three, rates ranged from 14 to 100% (mean = 79.0%). Aggregating these data from the 16 agencies indicates 1711 of 2694 (63.5%) women were screened for depression.
Table 4.
Screening rates of TTT agencies
| Agencies | Month 1 (%) | Month 2 (%) | Month 3 (%) | z-test (vs. Healthy Start 98.8%) |
Follow-up screening rates |
|---|---|---|---|---|---|
| TTT agencies with screening rates comparable to healthy start | |||||
| TTT Agency #1-6 | 100 | 100 | 100 | n/a | n/a |
| TTT Agency #7 | 94 | 87 | 100 | n/a | n/a |
| TTT Agency #8 | 64 | 71 | 100 | n/a | n/a |
| TTT Agency #9 | 90 | 89 | 95 | z = 0.35 | n/a |
| TTT Agency #10 | 67 | 67 | 83 | z = 1.34 | n/a |
| TTT agencies with screening rates significantly lower than healthy start | |||||
| TTT Agency #11 | 51 | 85 | 88 | z = 3.99 | 93% |
| TTT Agency #12 | 60 | 54 | 63 | z = 5.46 | 80% |
| TTT Agency #13 | 81 | 74 | 53 | z = 10.01 | Not available |
| TTT Agency #14 | 47 | 51 | 44 | z = 11.07 | 100% |
| TTT Agency #15 | 17 | 10 | 23 | z = 17.62 | Not available |
| TTT Agency #16 | 0 | 100 | 14 | z = 10.84 | 100% |
The six programs which did not have high screening rates during the immediate 3 month post-implementation phase were asked to provide follow-up data. Additional data was received from 4 of these 6 programs
To assess whether screening was implemented immediately or gradually, analyses were conducted with growth-curve modeling techniques (GCM) [23, 24]. To detect any significant systematic change in screening rates over time, we first tested a linear model from the three data points (months 1, 2, and 3 post-implementation). The average slope of screening rates did not differ significantly from zero, t(15) = 1.57, p = ns. Thus, on average, screening rates did not change systematically over the first 3 months.
Screening Rate: Comparisons to Healthy Start
To judge how effectively the “enhanced” train-the-trainer approach was implemented as compared to one-to-one professional consultation training, we compared the screening rates from TTT agencies and Healthy Start. Accordingly, we had collected data from Healthy Start during the 6 months before the first TTT program cycle, finding an average screening rate of 98.8%. Table 4 shows the screening rates of the 16 TTT programs 3 months after screening was implemented: 50% of 16 TTT programs (N = 8) achieved perfect rates (100% of eligible women were screened), matching the rate achieved by Healthy Start. Each of the remaining eight TTT programs with screening rates below that of Healthy Start, were compared to the 98.8% rate using two-proportion z-tests (Table 4) [25]. Of these eight agencies, two did not differ significantly from Healthy Start, while six had significantly lower screening rates. Considered together, our results indicate that 3 months after depression screening was implemented, 62.5% (10/16) of the agencies using TTT had already achieved screening rates comparable to Healthy Start.
Screening Rates: Follow-up
In spring 2009, 1 to 2 years after the agencies first implemented screening, we assessed the screening rates of six agencies that had reported low rates during the first two TTT cycles. We aimed to assess whether their rates improved over time. Screening rates of the third TTT cycle were not assessed because these agencies had only recently implemented screening. The data in Table 4 show that four of these six agencies that provided follow-up data on screening rates had indeed increased screening.
Discussion
In implementing this services project we gathered data showing our novel “enhanced” train-the-trainer approach could widely disseminate depression screening in social services and health programs serving pregnant and post-partum women. Indeed, all 32 participating agencies reported they had implemented screening. These agencies were diverse; including both primary health care and social service agencies, indicating TTT can be applied in many types of settings. Moreover, growth curve analyses of screening data revealed that agencies implemented screening immediately, without ongoing consultation from mentors. Such successful dissemination of screening techniques is not a foregone conclusion. In a U.K study of the standard train-the-trainer method, out of 113 participants responding, only 73 followed through and trained their staff [19].
The TTT program broadly disseminated screening programs across Iowa. In 3 years, maternal depression screening was established in 32 agencies in 20.2% (20/99) of Iowa counties. Because several screening programs were established in agencies serving major population centers, (e.g., Des Moines), within three TTT cycles over half of the Iowa population could be potentially served by one of these TTT agencies. Half of the programs provided screening data that strongly support the utility of screening. Most programs established via TTT achieved immediate high screening rates. Additionally, some of the agencies that initially had difficulty establishing screening programs improved significantly by the 1 to 2 year follow-up without additional help from the TTT team. For example, agencies #11 and #12 (Table 4), eventually established high screening rates without additional help from the TTT team. Implementation of this new practice simply required more time than the initial 3 months. For agency #16 (Table 4), which had the lowest initial screening rate, the trainer attributed low screening rates to staff forgetfulness and actively intervened by installing a computer reminder system. This minor addition boosted screening rates to 100%, suggesting that sometimes additional minor modifications are required to ensure the program is implemented. Only two agencies with initially low screening rates (#13 and #15), did not provide follow-up screening data, thus we were unable to determine whether their screening rates had improved. When trainers from both of these agencies returned the initial 3 months of screening data, both trainers rated their staff (using a four point Likert scale) as only “somewhat willing” to screen for perinatal depression, suggesting that their initial low rates may have been due to staff resistance. The initially low screening rates in these two agencies echo the findings of other investigators indicating that the establishment of screening is not immediate even when all required steps are in place including educating staff, establishing a screening protocol and referral sources. In one study, screening mothers for depression during pediatric well-child visits was not immediately implemented by all staff: only 46% of eligible charts included a completed EPDS over the first 3 months of that program [16]. In future programs, ongoing follow-up of agencies by the mentoring team would be a useful program component for agencies that might experience initial low screening rates.
For over half of the programs reporting, screening rates did not significantly differ from those at Healthy Start, where training was conducted via one-to-one professional consultation. This suggests that effective screening can be established through the professional development of lay staff, without intensive one-to-one consultation. Notably, compared to one-to-one professional consultation, establishing depression screening via the “enhanced” train-the-trainer model is not only likely to be less expensive, but also more sustainable.
The most important measure of the effectiveness of the program is the number of women screened. In the 3 months following implementation, 16 of the 32 reporting agencies screened a total of 1711 women. All 32 TTT agencies implemented screening and continued to screen after the 3 month evaluation period, confirming that the TTT program facilitated screening for far more perinatal women than would otherwise have been screened. In addition, trainers often recounted that their systematic screening of all pregnant or postpartum women increased the identification of affected women. One trainer with considerable prior experience in home-visiting noted that “before the implementation of EPDS screening, we missed so many women who needed case management services and referral.”
Screening rates were reported by only half of the agencies, which had accomplished the task of gathering screening data. Although not all of these agencies reported successful screening outcomes, our positive data may be biased through self-selection of successful programs. The 16 agencies that did not provide data on screening rates could have experienced significant challenges in implementing this program. Limitations of this services-research project include the lack of data on screening rates from all agencies as well as the assessment of fidelity to screening protocols. An important next step in validating our approach will be to conduct TTT as a research study, rather than a services project, to ensure that outcome data and fidelity assessment is systematically collected and evaluated.
In conclusion, although public health agencies are increasingly aware of the importance of screening for maternal depression [4, 6-8], health professionals lack confidence in managing this disorder [11, 12]. This services-project case report presents evidence that our “enhanced” train-the-trainer approach could close this gap by broadly and effectively disseminating maternal depression screening programs. More generally, given the global economic crisis, high unemployment rate and consequent increases in depression in the general population [26, 27], this training model might be extended to general primary settings to train staff in depression screening, and is particularly well suited to rural and frontier settings where training is limited due to travel or access limitations.
Acknowledgments
TTT-1 was supported with funding from the following agencies: Iowa Department of Public Health, Iowa Department of Human Services, Iowa Department of Human Rights, Iowa Department of Education, Iowa Head Start State Collaboration Office, Iowa Community Empowerment, Prevent Child Abuse Iowa, and Community Partnerships for Protecting Children. TTT-2 and TTT-3 were supported with funding from the Iowa Department of Management’s Community Empowerment program. The authors extend their appreciation to the Early Childhood Program staff of the Iowa Department of Public Health who helped to secure the funding for the first TTT program and assisted in the recruitment of agencies for all TTT cycles. These staff members include Ms. Gretchen Hageman MA, Ms. Stephanie Trusty RNC, BSN, and Ms. Jane Borst, RN MA. Finally, the ongoing assistance of Ms. Shanell Wagler from the Iowa Department of Management is greatly appreciated.
References
- 1.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 2.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A metaanalytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 3.Edhborg M, Lundh W, Seimyr L, Widstrom A-M. The long-term impact of postnatal depressed mood on mother-child interaction: A preliminary study. Journal of Reproductive and Infant Psychology. 2001;19:61–71. [Google Scholar]
- 4.Volume Section 2 of P.L.2000, c.167 (C.26:2-176) New Jersey: 2006. The Postpartum Depression Law. http://www.njleg.state.nj.us/2006/Bills/PL06/12_.HTM. [Google Scholar]
- 5.Segre LS, O’Hara MW. The status of postpartum depression screening in the United States. In: Henshaw C, Elliott S, editors. Screening for perinatal depression. Jessica Kinglsey Publishers; London: 2005. pp. 83–89. [Google Scholar]
- 6.The American College of Obstetricians and Gynecologists Psychosocial risk factors: Perinatal screening and intervention. Obstetrics and Gynecology. 2006;108:469–477. doi: 10.1097/00006250-200608000-00046. [DOI] [PubMed] [Google Scholar]
- 7.National Association of Pediatric Nurse Practitioners The PNP’s role in supporting infant and family well-being during the first year of life: Position statement. Journal of Pediatric Health Care. 2003;17:19A–20A. doi: 10.1067/mph.2003.51. [DOI] [PubMed] [Google Scholar]
- 8.Joseph GF. Transitions. Obstetrics and Gynecology. 2009;114:4–6. doi: 10.1097/AOG.0b013e3181ac7a5f. [DOI] [PubMed] [Google Scholar]
- 9.Evins GG, Theofrastous JP, Galvin SL. Post-partum depression: A comparison of screening and routine clinical evaluation. American Journal of Obstetrics and Gynecology. 2000;182:1080–1082. doi: 10.1067/mob.2000.105409. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Preventive Services Task Force Screening for depression: Recommendations and rationale. Annals of Internal Medicine. 2002;136:760–764. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 11.Olson AL, Kemper KJ, Kelleher KJ, Hammond CS, Zuckerman BS, Dietrich AJ. Primary care pediatricians’ roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110:1169–1176. doi: 10.1542/peds.110.6.1169. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt LA, Greenberg BD, Holzman GB, Schulkin J. Treatment of depression by obstetrician-gynecologists: A survey study. Obstetrics and Gynecology. 1997;90:296–300. doi: 10.1016/S0029-7844(97)00255-X. [DOI] [PubMed] [Google Scholar]
- 13.O’Hara MW, Gorman LL, Wright EJ. Description and evaluation of the Iowa depression awareness, recognition, and treatment program. American Journal of Psychiatry. 1996;153:645–649. doi: 10.1176/ajp.153.5.645. [DOI] [PubMed] [Google Scholar]
- 14.Baker CD, Kamke H, O’Hara MW, Stuart S. Web-based training for implementing evidenced-based management of postpartum depression. Journal of the American Board Family Medicine. 2009;22:588–589. doi: 10.3122/jabfm.2009.05.080265. [DOI] [PubMed] [Google Scholar]
- 15.Wisner KL, Logsdon MC, Shanahan BR. Web-based education for postpartum depression: Conceptual development and impact. Archives of Women’s Mental Health. 2008;11:377–385. doi: 10.1007/s00737-008-0030-9. [DOI] [PubMed] [Google Scholar]
- 16.Chaudron LH, Szilagyi PG, Kitzman HJ, Wadkins HIM, Conwell Y. Detection of postpartum depressive symptoms by screening at well-child visits. Pediatrics. 2004;113:551–558. doi: 10.1542/peds.113.3.551. [DOI] [PubMed] [Google Scholar]
- 17.Gordon TEJ, Cardone IA, Kim JJ, Gordon SM, Silver RK. Universal perinatal depression screening in an academic medical center. Obstetrics and Gynecology. 2006;107:342–347. doi: 10.1097/01.AOG.0000194080.18261.92. [DOI] [PubMed] [Google Scholar]
- 18.Yonkers KA, Smith MV, Lin H, Howell HB, Shao L, Rosencheck RA. Depression screening of perinatal women: An evaluation of the healthy start depression initiative. Psychiatric Services. 2009;60:322–328. doi: 10.1176/appi.ps.60.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elliott SA, Ashton C, Gerrard J, Cox JL. Is trainer training an effective method for disseminating evidence-based practice for postnatal depression? Journal of Reproductive and Infant Psychology. 2003;21:219–228. [Google Scholar]
- 20.Cox J, Holden J. Perinatal mental health: A guide to the edinburgh postnatal depression scale (EPDS) Gaskell; London: 2003. [Google Scholar]
- 21.Fairchild G, Chen E, Rushton G, Segre AM, Polgreen PM. Identifying surveillance site locations in Iowa using a maximal population coverage model; International meeting on emerging diseases and surveillance; Vienna, Austria. 2009. [Google Scholar]
- 22.Gresenz CR, Rogowski J, Escarce JJ. Updated variable-radius measures of hospital competition. Health Services Research. 2004;39:417–430. doi: 10.1111/j.1475-6773.2004.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raudenbush SW, Bryk AS. Hierarchical linear modeling: Applications and data analysis methods (Advanced quantitative technology in the social sciences) Sage; California: 2001. [Google Scholar]
- 24.Raudenbush SW, Bryk AS, Congdon RT. Hierarchical linear and nonlinear modeling. Scientific Software International; Chicago: 2004. [Google Scholar]
- 25.Dimension Research . Z-Test for two proportions calculator. Illinois: 2005. http://www.dimensionresearch.com/resources/calculators/ztest.html. [Google Scholar]
- 26.Paul KI, Moser K. Unemployment impairs mental health: Meta-analyses. Journal of Vocational Behavior. 2009;74:264–282. [Google Scholar]
- 27.Uutela A. Economic crisis and mental health. Current Opinion in Psychiatry. 2010;23:127–130. doi: 10.1097/YCO.0b013e328336657d. [DOI] [PubMed] [Google Scholar]