Abstract
Background
The risk of developing non-Hodgkin lymphoma (NHL) is greatly increased in HIV infection. The aim of this study was to determine if elevated serum levels of molecules associated with B cell activation precede the diagnosis of AIDS-associated NHL.
Methods
Serum levels of B cell activation-associated molecules, interleukin-6 (IL6), interleukin-10 (IL10), soluble CD23 (sCD23), soluble CD27 (sCD27), soluble CD30 (sCD30), C-reactive protein (CRP), and IgE were determined in 179 NHL cases and HIV+ controls in the Multicenter AIDS Cohort Study, collected at up to three time points per subject, 0–5 years prior to AIDS-NHL diagnosis.
Results
Serum IL6, IL10, CRP, sCD23, sCD27, and sCD30 levels were all significantly elevated in the AIDS-NHL group, when compared to HIV+ controls or to AIDS controls, after adjusting for CD4 T cell number. Elevated serum levels of B cell activation-associated molecules were seen to be associated with the development of systemic (non-CNS) NHL, but not with the development of primary CNS lymphoma.
Conclusions
Levels of certain B cell stimulatory cytokines and molecules associated with immune activation are elevated for several years preceding the diagnosis of systemic AIDS-NHL. This observation is consistent with the hypothesis that chronic B cell activation contributes to the development of these hematologic malignancies.
Impact
Marked differences in serum levels of several molecules are seen for several years pre-diagnosis in those who eventually develop AIDS-NHL. Some of these molecules may serve as candidate biomarkers and provide valuable information to better define the etiology of NHL.
Keywords: lymphoma, B cell, cytokines, AIDS, immune activation
INTRODUCTION
The risk of developing B cell non-Hodgkin lymphoma (NHL) is greatly increased in the setting of HIV infection (1–5). NHL is now the most common AIDS-related malignancy (6), and is a major cause of HIV infection-associated death in developed countries, where NHL accounts for 23–30% of AIDS-related causes of death (7–9). While a decreased incidence of AIDS-NHL is associated with the use of highly active antiretroviral therapy (HAART), not all subtypes of AIDS-NHL have decreased in incidence in the HAART era (9–11). In fact, HAART may allow some HIV+ subjects who would have died of opportunistic infections to survive longer with continued immune system dysfunction, resulting in an increased opportunity for developing lymphoma over time (12). Also, some forms of AIDS-NHL occur relatively early in the course of HIV disease, so these lymphomas often arise prior to the initiation of HAART, or even prior to the recognition of HIV infection.
There are several subtypes of AIDS-associated NHL (AIDS-NHL), including Burkitt lymphoma (BL), diffuse large B cell lymphoma (DLBCL), primary central nervous system lymphomas (PCNSL), and primary effusion lymphoma (PEL) (13–16). These different AIDS-NHL subtypes differ in anatomical distribution, Epstein-Barr virus (EBV) or human herpesvirus type 8 infection of neoplastic cells, and in the frequency of various molecular lesions, including chromosomal translocations and mutations involving immunoglobulin genes and/or oncogenes. Many AIDS-NHL, including virtually all PCNSL, are EBV-positive (EBV+) lymphomas (17). Loss of immunoregulatory control of EBV-infected B cells as a result of HIV infection-induced immune deficiency is believed to contribute directly to the genesis of such EBV+ AIDS-NHL (5, 14). In fact, a study from the Amsterdam Cohort Study on AIDS showed that EBV-specific CTL decreased in 5/5 patients who went on to develop EBV+ AIDS-NHL, but not in the two subjects who developed EBV-negative lymphomas (18, 19). In the HAART era, the incidence of those forms of AIDS-NHL that are typically EBV+ has decreased much more than that of those subtypes of AIDS-NHL that are not necessarily EBV+ (10, 12, 14, 20), consistent with the view that these EBV+ tumors result from loss of EBV-specific T cell function, which is restored by HAART
In contrast, most AIDS-NHL of the BL subtype are not EBV+, and are characterized by a chromosomal translocation that involves the rearrangement of the c-MYC oncogene (MYC) and the immunoglobulin heavy chain gene (IgH) switch region (14). The MYC:IgH rearrangement is believed to result from an error in IgH class switch recombination (CSR), a somatic DNA recombination event that occurs normally in activated B cells, which shifts the variable region from μ to another Ig heavy chain gene (γ, α, ε), and results in the production of antibodies of isotypes different from IgM. IgH CSR is driven by exposure to various B cell-stimulatory cytokines, and is mediated by the activity of activation-induced cytidine deaminase (AICDA), a DNA modifying enzyme. Similarly, many AIDS-NHL of the DLBCL subtype also are EBV-negative. These lymphomas are associated with the mutation, translocation and/or overexpression of BCL-6 and other oncogenes, and they tend to occur earlier in the course of HIV disease progression than PCNSL (15, 16, 21–25). The mutation of BCL-6 and other NHL-associated oncogenes is believed to occur during the process of somatic hypermutation (SHM), another DNA-modifying event that occurs normally following B cell activation, which results in the generation of antibodies that have enhanced binding affinity for antigen. SHM of Ig gene variable regions also is mediated by AICDA.
Therefore, at least two general types of pathogenetic mechanisms appear to contribute to the genesis of AIDS-NHL: 1) loss of immunoregulation of EBV-infected B cells, due to the loss of T cell function that is associated with HIV infection, and, 2) chronic B cell hyper-activation, which is associated with DNA-modifying events (SHM and IgH CSR) that can contribute to lymphomagenic molecular lesions (oncogene mutations/translocations) (5).
HIV infection is characterized by chronic B cell hyperactivation, driven by the overproduction of B cell-stimulatory cytokines such as interleukin (IL) 6, as well as by chronic antigenic stimulation (4, 26, 27). It has been known for some time that IL6 levels are elevated prior to the development of AIDS-NHL (28). Also, high expressor genotypes for two B cell stimulatory cytokines, SDF-1 and IL10, and for CCR5, a receptor for B cell stimulatory chemokines, are associated with the development of AIDS-NHL (29–31). In our prior work examining a single time point close to but preceding the diagnosis of AIDS-NHL, HIV+ subjects who developed AIDS-NHL had especially elevated serum levels of several B cell stimulatory molecules (IL6, IL10, CXCL13, soluble CD23 [sCD23]), and molecules associated with immune activation (sCD27, sCD30, sCD44, IgE), higher than the already elevated levels seen in HIV+ subjects who did not develop lymphoma (4, 29, 32–39). In addition, elevated expression of AICDA gene (AICDA) expression in circulating lymphocytes was seen for several years preceding lymphoma diagnosis (40). However, little is known about the length of time preceding AIDS-NHL diagnosis that serum levels of these B cell stimulatory molecules are elevated.
In this study, we sought to better define the longitudinal expression, preceding AIDS-NHL diagnosis, of B cell-stimulatory cytokines (IL6, IL10), of a cytokine-like B cell activation-associated molecule that is associated with the induction of IgH CSR (sCD23) (41, 42), of an immunoglobulin isotype that indicates the activity of IgH CSR (IgE), of two molecules from the tumor necrosis factor (TNF)-receptor superfamily that reflect immune system activation (sCD27, sCD30) (43), and of a molecule that is a marker for the activity of pro-inflammatory cytokines (C-reactive protein [CRP]). This was done using up to three archival, pre-lymphoma diagnosis serum specimens from subjects in the Multicenter AIDS Cohort Study (MACS) who developed AIDS-NHL, as well as from appropriate MACS HIV-seropositive controls who had not developed AIDS-NHL. Elevated levels of several of these B cell stimulation-associated molecules were seen for an extended period of time (more than three years) preceding the diagnosis of AIDS-NHL, especially in those who developed systemic (non-PCNSL) AIDS-NHL which would be expected to be associated with chronic B cell hyper-activation.
MATERIALS AND METHODS
Study Design
This study is a nested case-control design, utilizing serum samples from participants in the Multicenter AIDS Cohort Study (MACS). MACS participants are homosexual men who have had study visits at six month intervals to examine the natural history of HIV infection and AIDS (44). Subjects were utilized from men who were enrolled in 1984–85 or in 1987–1991. At each visit, detailed histories and blood samples were obtained, and serum archived in a central repository. Clinical information from each visit was obtained from the participants and by review of external registries, and confirmed by medical record review. The protocols and questionnaires utilized in the MACS have been approved by the Institutional Review Board at each center.
Cases consisted of HIV-infected MACS subjects diagnosed with AIDS-NHL prior to April, 2003, for whom at least one serum sample from a time point preceding AIDS-NHL diagnosis was available in the MACS repository, and a matched HIV-infected (HIV+) control could be identified as described below (n=179). Longitudinal serum samples were obtained at up to three time points prior to NHL diagnosis: >3 years pre-NHL (closest to 4 years), 1–3 years pre-NHL (closest to 2 years), and 0–1 year pre-NHL (closest to 0.5 year). The median time between serum samples at each time point and NHL diagnosis was 4.0, 2.0, and 0.6 years, respectively.
For each case, all possible HIV+ controls were identified from among HIV-infected MACS subjects who had not developed lymphoma as of April 2003, matched on: 1) actual length of infection with HIV based on known date of HIV seroconversion [21 cases], or date of entry ± 1 year into MACS as HIV-seroprevalent [158 cases], and 2) expected sample availability at equivalent time points ± 1 year. One unique HIV+ control was randomly selected for each case; the median time that cases and HIV+ controls had been HIV-infected or seroprevalent at the time of AIDS-NHL diagnosis in the case was 6.8 and 6.9 years, respectively. In the subset of 21 cases and matched controls with a known date of seroconversion, the median HIV+ time to AIDS-NHL was 6.7 years (range 2.7–10.4) and 6.4 years (range 2.3–10.3), respectively. The characteristics of all AIDS-NHL cases and HIV+ controls, as determined from information obtained from the MACS database, are shown in Table 1. AIDS-NHL cases were stratified by primary tumor location as central nervous system (CNS, brain or other central nervous system site, n=58) or systemic (all other sites, n=121); systemic cases with known tumor subtype were further stratified into Burkitt/Burkitt-like lymphoma (BL, n=21), diffuse large B cell lymphoma (DLBCL, n=61), and other subtypes (n=3).
Table 1.
Characteristics of AIDS-NHL cases and controls
| All AIDS-NHL cases | HIV+ controls | AIDS-NHL subset with prior AIDS diagnosis | AIDS controls | |
|---|---|---|---|---|
| N | 179 | 179 | 100 | 100 |
| Age at time of case NHL diagnosis, median years (range) | 41 (24–60) | 39 (24–60) | 40 (24–57) | 38 (23–68) |
| Ethnicity, N (%) | ||||
| White, non-Hispanic | 149 (83) | 156 (87) | 81 (81) | 87 (87) |
| White, Hispanic | 19 (11) | 8 (4) | 11 (11) | 6 (6) |
| Black, non-Hispanic | 11 (6) | 10 (6) | 8 (8) | 4 (4) |
| Other | 0 | 5 (3) | 0 | 3 (3) |
| CD4 T cells, median cells/mm3 (range)a | ||||
| >3 years pre-NHL | 387 (5–1349) | 561 (3–2030) | 369 (5–1227) | 397 (19–1123) |
| 1–3 years pre-NHL | 209 (6–1178) | 522 (37–1544) | 144 (6–1178) | 238 (9–1132) |
| 0–1 year pre-NHL | 74 (0–707) | 468 (4–1255) | 32 (0–691) | 93 (0–1159) |
| HAART at time of sample, N (%)a | ||||
| >3 years pre-NHL | 1 (1) | 0 | 1 (1) | 0 |
| 1–3 years pre-NHL | 3 (2) | 4 (3) | 1 (1) | 1 (1) |
| 0–1 year pre-NHL | 5 (5) | 5 (5) | 1 (1) | 2 (2) |
| Tumor Subtype, N (%) | ||||
| Systemic NHL tumor | 121 (68) | 56 (56) | ||
| Diffuse Large B Cell | 61 (50) | 27 (48) | ||
| Burkitt Lymphoma/BL-like | 21 (17) | 8 (14) | ||
| Other subtypes | 6 (5) | 3 (5) | ||
| Not specified | 33 (27) | 18 (32) | ||
| CNS NHL tumor | 58 (32) | 44 (44) | ||
| Tumor EBV status, N (%) | ||||
| Not Tested | 92 (51) | 44 (44) | ||
| Tested | 87 (49) | 56 (56) | ||
| Negative | 28 (32) | 16 (29) | ||
| Positive | 59 (68) | 40 (71) |
includes cases and controls who had serum available for that study visit
In a subset of the AIDS-NHL cases (n=100), NHL was diagnosed subsequent to another AIDS-defining condition, according to the 1993 definition of the Centers for Disease Control and Prevention, excluding cases defined by CD4 T cell count alone (45). For this subset of cases, one unique AIDS control was randomly selected for each case from all MACS subjects with an AIDS diagnosis other than NHL, matched on: 1) year of AIDS diagnosis [± 1 year], 2) post-AIDS survival time (i.e., survived NHL-free longer than the case following AIDS diagnosis), and 3) expected sample availability at equivalent time points [± 1 year]. The median time between the initial AIDS diagnosis and NHL diagnosis was 1.2 years. The characteristics of this subset of AIDS-NHL cases and AIDS controls are also shown in Table 1.
Determination of immune markers in serum samples
Serum levels of immune markers were assessed by enzyme-linked immunosorbent assay (ELISA). Assays for sCD23 (detection limit = 13 units/ml) and sCD30 (detection limit = 6 units/ml) were performed according to the manufacturer’s protocols (Bender MedSystems USA, San Bruno, California). sCD27 was determined using the PeliKine-compact ELISA kit and Toolset according to the manufacturer’s protocol (CLB/Sanquin, Netherlands), with 1:20 dilutions on all samples (detection limit = 32 units/ml, taking dilution into account). C-reactive protein (CRP) was measured using the high sensitivity protocol (detection limit = 0.25 μg/ml), as described by the manufacturer (Virgo CRP 150, Hemagen, Columbia, Maryland). IL6 was measured using an ultrasensitive assay (Biosource/Invitrogen, Carlsbad, California), with color development time extended to 40 minutes to ensure consistent low level detection (detection limit = 0.2 pg/ml). IL10 was measured using a human IL10-specific assay (Biosource/Invitrogen)(detection limit = 2 pg/ml) that does not cross react with viral IL10 of Epstein-Barr Virus, as previously described (29).. Total serum IgE was determined utilizing the CIA-7.12 and CIA-4.15 monoclonal antibodies (46) as previously described (47), with the following modifications: plates were blocked with 10% fetal bovine serum, serum samples were diluted 1:10, and 50 μl per well of diluted sera and all subsequent reagents were incubated on a rotator (500 rpm). The IgE standard was pooled normal serum (generously provided by Andrew Saxon and Ke Zhang); when referenced to the WHO IgE standard NIBSC 75/502 (which is also pooled human sera), the mean conversion factor was 0.67 ng per IU. Taking the dilution into account, the limit of detection was 8 ng/ml.
Data analysis
IL6, CRP, sCD23, sCD27, sCD30, and IgE data were natural log-transformed and treated as continuous variables, with results below the detection limit (value of lowest standard on standard curve) set equal to half the value of the detection limit; univariate analyses were performed using t-tests. IL10 data were analyzed as binary variables (detectable IL10 ≥ 2 pg/ml vs. undetectable), using chi square statistic. Correlations were calculated separately for cases and controls at each time point for continuous variables using Spearman’s correlation coefficients.
Absolute CD4 T cell count (CD4 count) data were available from the MACS database, and were used to control for possible differences in HIV disease progression. At each of the pre-NHL time points, age- and CD4 count-adjusted conditional logistic regression models were generated to compare AIDS-NHL cases to matched HIV+ controls. Odds ratios (ORs) and 95% confidence intervals (CI) were generated to estimate the risk of AIDS-NHL associated with one log-unit increase in concentration for continuous variables or detectable versus undetectable for IL10. Models were also generated adjusting for rate of change of CD4 count (CD4 slope, cells/mm3/year) or baseline HIV RNA viral load (VL log10 copies/ml, 18 months after first HIV-seropositive MACS study visit) (48, 49), which included fewer case-control pairs due to missing data, especially for VL (data not shown). Age- and CD4 count-adjusted models were further tested with stratification by systemic versus CNS AIDS-NHL, and by NHL sub-type (DLBCL and BL) among systemic AIDS-NHL.
Similar models were generated to compare the subset of AIDS-NHL cases with prior AIDS to AIDS controls, adjusted only for age since they were matched based on progression to AIDS. An additional model adjusted for age and CD4 count did not meaningfully affect the OR estimates (data not shown).
RESULTS
Increased serum levels of multiple immune biomarkers are seen up to three or more years prior to AIDS-NHL diagnosis
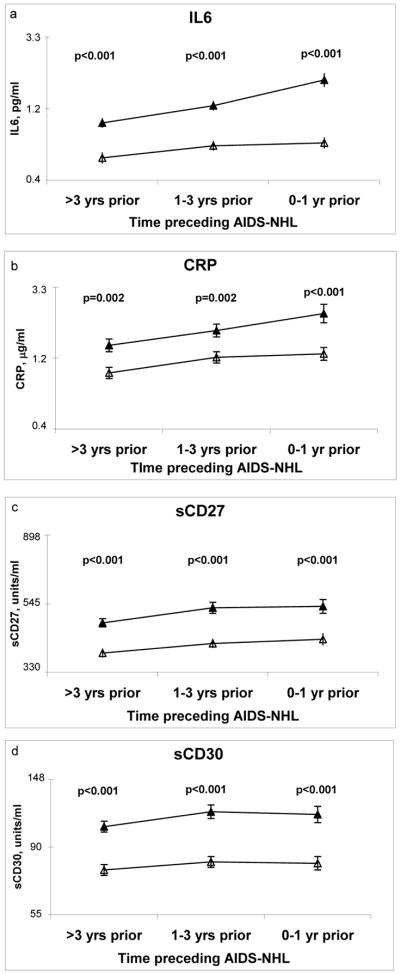
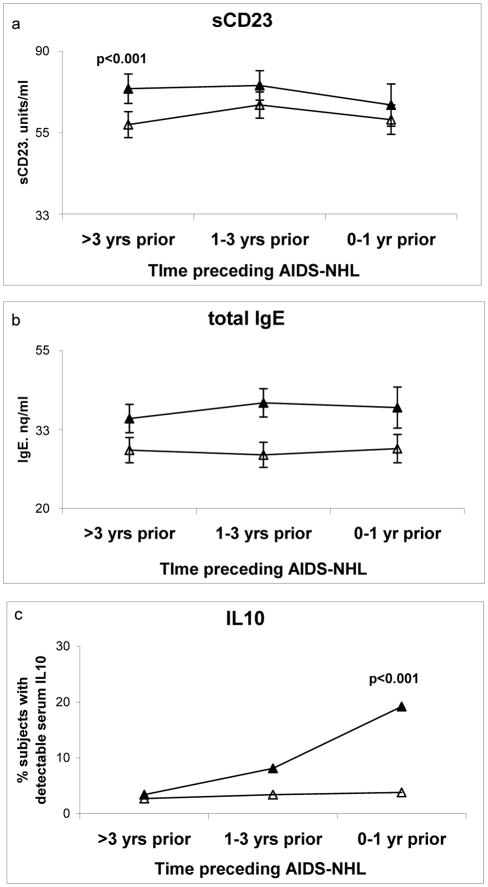
Univariate analyses of AIDS-NHL cases compared to HIV+ controls, without regards to matching, showed significantly higher mean serum levels of IL6, CRP, sCD27, and sCD30 in cases at all three time points (>3 years, 1–3 years, and 0–1 year) prior to lymphoma diagnosis (Figure 1A-D, p≤0.002). sCD23, a soluble form of the low-affinity cell surface Fc receptor for IgE, which has B cell stimulatory properties, showed elevated serum levels in cases, but was only statistically significantly elevated >3 years prior to lymphoma diagnosis (Figure 2A, p<0.001). Serum levels of IgE showed no significant differences between AIDS-NHL cases and HIV+ controls at any time point (Figure 2B). As expected from previous work on subjects from this same cohort study (29), the majority of all HIV+ subjects had undetectable levels (<2 pg/ml) of serum IL10. However, consistent with those prior observations, the frequency of detectable serum levels of IL10 (> 2 pg/ml) was clearly and significantly elevated in AIDS-NHL (Figure 2C), but only at the time point immediately preceding lymphoma diagnosis (0–1 years prior, p<0.001).
Figure 1. Mean serum levels of several B cell activation-associated molecules are consistently elevated more than three years preceding AIDS-associated lymphoma diagnosis.
Natural log-transformed mean values (± s.e.m.) for HIV-infected subjects who went on to develop AIDS-NHL (filled triangles) and HIV-infected controls without lymphoma (open triangles) for (a) interleukin 6 (IL6), (b) C′-reactive protein (CRP), (c) soluble CD27 (sCD27), and (d) sCD30, in the years prior to NHL diagnosis in the case; p values (univariate t-test) are shown only if <0.05
Figure 2. Mean serum levels of additional B cell activation-associated molecules may be elevated prior to lymphoma.
Natural log-transformed mean values (± s.e.m.) for (a) sCD23 and (b) total IgE, and (c) percentage of samples with detectable (≥2 pg/ml) serum IL10, are shown for all AIDS-NHL subjects (filled triangles) and HIV+ controls (open triangles); p values for continuous variables (univariate t-test), and frequency of detectable IL10 (chi square) are shown only if <0.05
CRP, which is produced by hepatocytes in response to IL6 and can be considered a marker for the bioactivity of IL6 (50), was significantly correlated with IL6 at all time points (r=0.37–0.48, Supplemental Table 1). sCD27 and sCD30, which are both members of the TNF receptor superfamily, showed strong correlations to each other at all time points (r=0.55–0.75), as well as to sCD23 (r=0.28–0.46); sCD23 showed no correlation with IgE (Supplemental Table 1).
Certain immune biomarkers are increased prior to NHL, even when diagnosis of lymphoma occurs after some other AIDS-defining condition
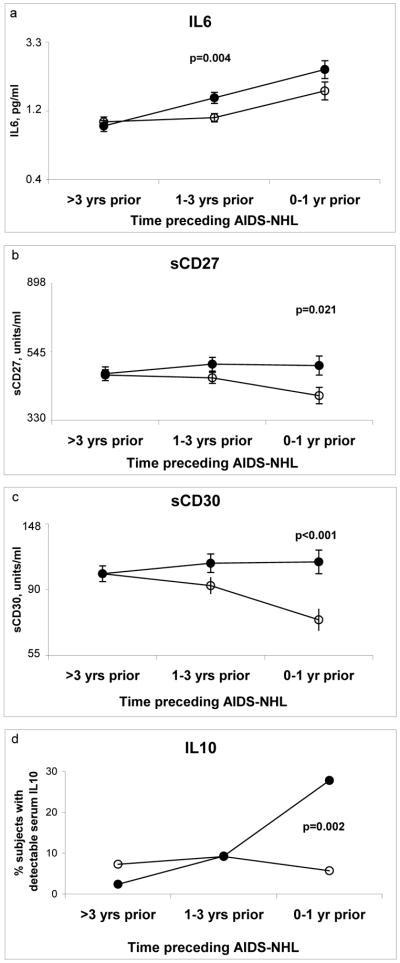
Among the 179 subjects who developed AIDS-NHL, 100 subjects were diagnosed with lymphoma after previously being diagnosed with another AIDS-defining condition. These cases were compared to a second group of HIV-infected controls who also had AIDS, matched by time of first AIDS diagnosis (AIDS controls).
There were no significant differences between NHL cases with prior AIDS and AIDS controls in serum levels of CRP, sCD23, or IgE at any time point pre-lymphoma (data not shown). At the time point furthest from lymphoma diagnosis (>3 years prior), there were no significant differences between AIDS-NHL cases and AIDS controls in mean serum levels of IL6, sCD27, sC30, or IL10 (Figure 3). However, at 1–3 years before lymphoma diagnosis, mean IL6 levels rose in the AIDS-NHL group, but stayed relatively stable in the AIDS control group, resulting in a significant difference (Figure 3A). Both cases and controls showed higher mean IL6 levels 0–1 year before lymphoma and so did not differ significantly at that time point. In contrast, mean serum levels of sCD27 (Figure 3B) and sCD30 (Figure 3C) were relatively stable in the AIDS-NHL cases over the time approaching lymphoma diagnosis, while AIDS controls showed declining mean levels over time, leading to significant differences at the time closest to lymphoma. For IL10, NHL cases with prior AIDS (Figure 3D) were similar to AIDS-NHL cases overall (Figure 2C), with increased frequency of detectable IL10 seen only at 0–1 year prior to lymphoma diagnosis.
Figure 3. Some B cell activation markers are elevated prior to lymphoma in those AIDS- NHL cases that had another AIDS-defining condition prior to NHL.
Natural log-transformed mean values (± s.e.m.) for (a) IL6, (b) sCD27, and (c) sCD30, and (d) percentage of subjects with detectable serum IL10, are shown for the subset of AIDS-NHL subjects (n=100) that had a primary AIDS diagnosis other than lymphoma, then went on to develop NHL (filled circles), and controls who had an AIDS diagnosis but did not develop lymphoma (open circles); p values for continuous variables (univariate t-test), and frequency of detectable IL10 (chi square) are shown only if <0.05
AIDS-NHL risk is significantly associated with increased pre-diagnosis levels of serum IL6, sCD27, sCD30, and IL10, even when taking differences in CD4 T cell numbers into account
In order to discriminate between effects associated with the development of NHL and those associated with the progression of HIV disease over time, all AIDS-NHL cases and HIV+ controls were matched based on duration of HIV infection. After matching, cases and controls differed in their absolute CD4 T helper cell counts, especially as the cases approached the time of lymphoma diagnosis (Table 1). In age-adjusted analyses, a decrease of 50 cells/mm3 in CD4 count was associated with an increased risk of NHL at >3 years (OR 1.15, 95% CI=1.08–1.22), 1–3 years (OR 1.42, 95% CI=1.26–1.60), or 0–1 year (OR 1.45, 95% CI=1.26–1.67) prior to NHL diagnosis. Independent of NHL risk, CD4 counts are an important indicator of immune system status in the context of HIV disease and may impact circulating immune biomarker levels. Therefore, in order to adjust for this potential confounder, logistic regression analyses for lymphoma risk in association with increased serum levels of immune biomarkers were performed controlling for CD4 counts at the time of each sample.
For all AIDS-NHL cases compared to HIV+ controls, increased serum levels of IL6, sCD27, and sCD30 remained statistically significant at all three time points after CD4 count adjustment (Table 2, upper half). Interestingly, in spite of the significant correlation seen between IL6 and CRP levels, adjusted ORs for CRP were no longer statistically significant at the time point closest to lymphoma diagnosis (where the CD4 differences were greatest and the sample size was smallest). Consistent with the univariate analyses, sCD23 levels were significantly increased only at the time furthest from lymphoma diagnosis, frequency of detectable IL10 was significantly increased only at 0–1 years prior to lymphoma, and IgE levels were not significantly increased at any time point preceding lymphoma diagnosis.
Table 2.
Odds Ratios (OR) and 95% confidence intervals (CI) for increased cytokine concentrations in NHL cases
| >3 years prior | 1–3 years prior | 0–1 year prior | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N, setsa | ORb | 95% CI | N, setsa | ORb | 95% CI | N, setsa | ORb | 95% CI | |
| all NHL cases vs. HIV+ controlsc | |||||||||
|
| |||||||||
| IL6 | 132 | 2.37 | 1.51 – 3.72 | 129 | 4.14 | 1.81 – 9.49 | 88 | 6.01 | 2.07 – 17.45 |
| CRP | 141 | 1.65 | 1.25 – 2.18 | 139 | 1.55 | 1.08 – 2.22 | 100 | 1.31 | 0.84 – 2.07 |
| sCD27 | 141 | 3.72 | 1.68 – 8.25 | 139 | 6.98 | 2.23 – 21.83 | 100 | 3.81 | 1.21 – 11.96 |
| sCD30 | 141 | 3.22 | 1.75 – 5.91 | 139 | 8.64 | 3.09 – 24.14 | 101 | 4.77 | 1.63 – 13.90 |
| sCD23 | 136 | 2.02 | 1.17 – 3.47 | 136 | 1.74 | 0.93 – 3.26 | 99 | 1.37 | 0.78 – 2.42 |
| IgE | 141 | 1.08 | 0.88 – 1.31 | 139 | 0.99 | 0.78 – 1.25 | 100 | 0.98 | 0.76 – 1.27 |
| IL10 | 141 | 0.78 | 0.17 – 3.64 | 139 | 1.26 | 0.28 – 5.57 | 100 | 7.74 | 1.06 – 56.59 |
|
| |||||||||
| NHL after other AIDS diagnosis vs. AIDS controlsd | |||||||||
|
| |||||||||
| IL6 | 79 | 1.00 | 0.60 – 1.69 | 81 | 2.08 | 1.13 – 3.86 | 49 | 1.47 | 0.90 – 2.40 |
| CRP | 82 | 1.34 | 0.94 – 1.92 | 86 | 1.34 | 0.98 – 1.85 | 54 | 1.03 | 0.77 – 1.38 |
| sCD27 | 82 | 1.04 | 0.45 – 2.40 | 86 | 1.79 | 0.82 – 3.93 | 54 | 2.47 | 1.02 – 5.96 |
| sCD30 | 82 | 0.93 | 0.51 – 1.68 | 86 | 2.00 | 1.02 – 3.91 | 54 | 4.85 | 1.92 – 12.28 |
| sCD23 | 82 | 1.30 | 0.75 – 2.28 | 86 | 1.34 | 0.81 – 2.21 | 53 | 1.31 | 0.77 – 2.24 |
| IgE | 82 | 1.23 | 0.99 – 1.55 | 86 | 1.13 | 0.95 – 1.36 | 54 | 1.12 | 0.91 – 1.39 |
| IL10 | 82 | 0.33 | 0.07 – 1.65 | 86 | 1.03 | 0.35 – 2.97 | 54 | 9.08 | 1.87 – 44.03 |
matched case-control sets
for all markers except IL10 ORs are in terms of one unit increase in natural log-transformed values; for IL10, ORs are in terms of detectable vs. undetectable. Statistically significant ORs are shown in bold.
sets matched on duration of HIV infection, analyses adjusted for age and CD4 T cell count
sets matched on time of initial AIDS diagnosis, analyses adjusted for age
To confirm that the observed associations between AIDS-NHL and increased serum levels of IL6, sCD27, sCD30, and IL10 were not merely a reflection of HIV disease progression, immune biomarker analyses were repeated controlling for age plus other prognostic indicators of HIV disease: rate of change of CD4 count (CD4 slope) or baseline HIV VL (48, 49). Increases in IL6, sCD27, and sCD30 levels remained significantly associated with increased risk of AIDS-NHL at all time points in both analyses (data not shown). Detectable IL10 remained significant at 0–1 year before lymphoma diagnosis with CD4 slope adjustment (n=93 case-control sets, OR 7.40, 95% CI=1.91–28.60), but lost significance when adjusted for VL, which may reflect instability in the estimates due to a reduced number of case-control sets (n=75, OR 4.76, 95% CI=0.86–26.27). In age-adjusted analyses, a decrease in CD4 slope of 50 cells/mm3/year (OR 1.55, 95% CI=1.23–1.94) or an increase in baseline VL of 1 log10 copies/ml (OR 6.31, 95% CI=3.13–12.72) was independently associated with an increased risk of AIDS-NHL.
Logistic regression analyses were also performed in the subset of NHL cases with prior AIDS and AIDS controls (Table 2, lower half). ORs were similar to the results obtained in univariate analyses, with significantly elevated ORs seen at 1–3 years before lymphoma for IL6, and at 0–1 year for sCD27, sCD30, and IL10. In addition, sCD30 had an OR of borderline significance at 1–3 years pre-lymphoma.
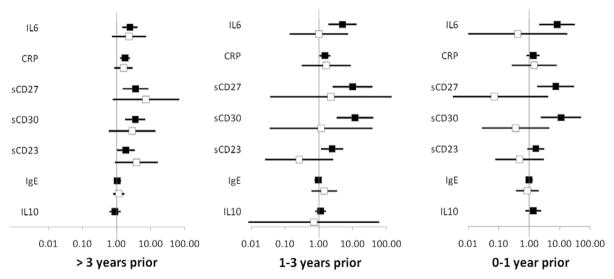
Elevated serum levels of immune biomarkers were seen to be associated with the development of systemic AIDS-NHL, but not with the development of primary CNS AIDS-NHL
Compared to similar forms of NHL in the non-HIV-infected population, primary tumors in AIDS-NHL are more likely to occur at sites other than lymph nodes (1, 12). In HIV-infected subjects with advanced HIV disease and low CD4 counts, a notable proportion of AIDS-NHL cases present with PCNSL (28, 51). Among the 179 cases of AIDS-NHL in this study, 58/179 (32%) of the primary tumors were located within the CNS, while the remaining 68% of cases presented with primary tumors outside the CNS (systemic). The AIDS-NHL cases were stratified on the basis of primary tumor location, and CD4 count-adjusted logistic regression analyses were performed compared to their matched HIV+ controls.
The stratification of AIDS-NHL cases according to CNS or systemic primary tumor location revealed stronger associations of elevated levels of biomarkers with risk of systemic lymphoma (Figure 4). Detectable IL10 could not be evaluated at 0–1 year and 3–5 years prior to PCNSL due to sparse data, and was not significantly associated with PCNSL at 1–3 years prior to diagnosis. Although elevated ORs were seen for several of the markers other than IL10, especially at >3 years pre-PCNSL, no statistically-significant association was seen at any time point prior to PCNSL. The systemic NHL cases recapitulated the results seen in the AIDS-NHL cases overall, with elevated serum levels of IL6, sCD27 and sCD30 significantly associated with AIDS-NHL at all time points preceding lymphoma diagnosis, and CRP at all but 0–1 year pre-lymphoma. Interestingly, elevated sCD23 levels, which were significantly associated only at >3 years prior to AIDS-NHL cases overall, emerged in the analyses of systemic AIDS-NHL cases as also significantly associated at 1–3 years prior to lymphoma diagnosis. In contrast, detectable IL10 was no longer significantly associated at the time point closest to systemic NHL diagnosis. No significant association was seen at any time point between serum IgE levels and systemic AIDS-NHL.
Figure 4. Elevated levels of B cell activation markers prior to AIDS-NHL are seen only in those subjects who develop systemic lymphoma.
CD4-adjusted odds ratios (OR) ± 95% confidence intervals (CI) for increased serum cytokine levels are shown for AIDS-NHL cases compared to matched HIV+ controls, stratified according to primary tumor location outside of the central nervous system (systemic, filled squares) or within the central nervous system (CNS, open squares). For all markers except IL10, ORs are in terms of one unit increase in natural log-transformed values; for IL10, ORs are in terms of detectable vs. undetectable. ORs are missing for IL10 for CNS tumors at two time-points (>3 years and 0–1 year) due to failure of the logistic regression model to converge on account of sparse data.
The systemic AIDS-NHL cases were further stratified to determine if there was a pattern of elevated serum biomarkers associated with either of the major subtypes, DLBCL (n=61) and BL (n=21). In a univariate comparison of mean levels between DLBCL and BL cases, the only significant difference was higher levels of sCD23 at 1–3 years preceding the diagnosis of BL (p=0.02, data not shown). In CD4 count-adjusted logistic regression models comparing DLBCL or BL cases to matched HIV+ controls (Supplemental Table 2), some markers and time points could not be evaluated due to small sample size. Although there were elevated ORs for many markers in both the DLBCL and BL cases, statistically-significant associations were seen only with elevated levels of IL6, sCD27, and sCD30 >3 years and/or 1–3 years prior to DLBCL. It is likely that the lack of any significant association for any markers or timepoints with BL is due at least in part to the small number of cases of this subtype.
DISCUSSION
In this study, we have examined the longitudinal levels of several serum molecules associated with B cell and/or immune system activation, over a period of several years preceding AIDS-NHL diagnosis. These included two B cell-stimulatory cytokines, IL6 and IL10, and sCD23, a soluble Fc receptor for IgE that has cytokine-like B cell-stimulatory properties (41, 42). Additionally, we assessed serum levels of IgE, which is induced by Th2 cytokines, as well as serum levels of sCD27 and sCD30, two TNF-receptor superfamily molecules that reflect immune system activation (43), and CRP, a marker for inflammation, the production of which is driven by pro-inflammatory cytokines.
Elevated serum levels of IL6, CRP, sCD27, and sCD30, were consistently seen at all time points tested preceding lymphoma diagnosis, when comparing all AIDS-NHL cases (n=179) to HIV+ controls (Figure 1). Even after adjustment for CD4 T cell count (Table 2), CD4 slope, or HIV VL, to control for differences possibly related to HIV disease progression rather than AIDS-NHL, an increased association clearly persisted between the development of AIDS-NHL and elevated serum levels at all time points for IL6, sCD27, and sCD30. Increased frequency of detectable IL10 was also seen preceding AIDS-NHL cases both with and without CD4 adjustment, but only at the time closest to lymphoma diagnosis. With CD4 adjustment, CRP was no longer significant at 0–1 year prior to NHL, which may reflect an increasing contribution of more general HIV disease-related inflammation obscuring the earlier relationship with development of AIDS-NHL and/or may be due to the smaller number of samples available closest to lymphoma diagnosis. Similarly, elevated serum levels of sCD23 only at >3 years pre-lymphoma may suggest rising levels in HIV+ controls with time obscure earlier differences. IgE showed no significant association with AIDS-NHL in any analysis, in contrast to an early report (36), but consistent with later studies (38), which is likely due to differences in study design and differences in the immunoassays utilized. Hence, even when taking into account lower CD4 counts (or more rapid CD4 decline or higher baseline VL) over the same length of time of HIV infection, our data indicated the presence of a sustained environment of B cell and immune system hyper-activation for more than three years in those subjects who went on to develop AIDS-NHL.
A little more than half of the AIDS-NHL cases in the overall analyses (100/179) were diagnosed with lymphoma after some other AIDS-defining condition. We compared this subset of cases to an independent set of controls matched on time of AIDS diagnosis, and saw elevated serum levels of IL6, sCD27, and sCD30, but only at 0–1 and/or 1–3 years prior to lymphoma diagnosis. This suggests that although a prior AIDS-defining condition may disrupt an earlier pre-lymphoma B cell stimulatory environment and/or confound our ability to detect it, evidence of increased immune activation does emerge, especially in the year immediately preceding AIDS-NHL diagnosis. In light of differences seen between systemic and CNS AIDS-NHL cases (as discussed below), less immune activation might also be attributable at least in part to the fact that PCNSL occurred in a higher proportion of post-AIDS diagnosis cases (44%) than in the overall AIDS-NHL cases (32%).
IL6 is a pluripotent cytokine that can stimulate B cell proliferation and differentiation, and promote cell survival and tumor growth (52–55). IL6 production is driven by multiple stimuli, including exposure to lipopolysaccharide (LPS) or to HIV virions (56–58). IL6 also is associated with proinflammatory responses, as well as with Th17 responses, which are associated with autoimmunity (59, 60). Interestingly, those forms of autoimmunity that involve B cell activation and are mediated by autoantibody production have been seen to be associated with an enhanced risk for the development of B cell NHL (61). Previous cross-sectional studies have documented elevated IL6 preceding AIDS-NHL (28, 33). The observation that elevated serum levels of IL6 are repeatedly associated with AIDS-NHL for more than three years prior to diagnosis is consistent for a role for IL6-driven B cell stimulation in the development and/or growth of these lymphomas.
CD30 and CD27 are the receptors for CD30 ligand (CD153) and CD70, respectively, which are TNF-like immune stimulatory molecules (62–65). CD30 is characteristically expressed on Hodgkin lymphoma Reed-Sternberg cells, but is rarely expressed by NHL cells. sCD30 is produced by activated T cells, and may be a marker for Th2 immune responses that support B cell activation and differentiation into antibody-secreting plasma cells (66). CD27 is expressed on the surface of B cells following activation, and is a marker for memory B cells (67–70). In prior cross-sectional studies, we noted strong correlations between these two related molecules, and have reported elevated serum levels of both sCD30 and sCD27 preceding the diagnosis of AIDS-NHL (32, 35). Like IL6, the consistent elevation of these molecules for more than three years pre-lymphoma provide strong evidence for the role of sustained B cell activation in the development of AIDS-NHL. Elevated serum sCD30 also has been reported preceding the diagnosis of non-AIDS NHL (71), suggesting that an environment rich in B cell activation may be a feature that precedes many B cell lymphomas, regardless of HIV status.
IL10 is a B cell stimulatory cytokine that also can suppress Th1 responses, including anti-viral cell-mediated responses (72, 73). Our observations of IL10 in this study are consistent with our previous work, in which we found elevated serum levels of IL10 immediately preceding AIDS-NHL, as well as an association between IL10 genotype and the development of AIDS-NHL (29, 74). An elevated frequency of detectable IL10 only at the time point closest lymphoma diagnosis (<1 year pre-NHL) suggests that this cytokine is either tumor-produced, consistent with a report that IL10 is an autologous growth factor for AIDS-NHL (75), and/or is produced by, or in response to, the inflammatory microenvironment of the tumor.
When the results from those who developed PCNSL were compared to those who had systemic non-CNS NHL, it was seen that significantly elevated serum levels of B cell activation-associated molecules were seen only with the development of systemic lymphomas. This suggests that elevated serum levels of molecules associated with B cell activation are not associated with an increased risk for the development of PCNSL, which is characterized by EBV infection of tumor cells. Rather, elevated levels of B cell activation-associated molecules were seen preceding the development of those forms of AIDS-NHL (systemic AIDS-NHL, including BL and DLBCL) that contain molecular lesions believed to result from errors in B cell activation-associated DNA-modifying events. These findings are consistent with the view that EBV+ PCNSL result primarily from loss of effective immunoregulation of EBV infection, while systemic lymphomas, which are often EBV-negative tumors, are associated with chronic B cell activation over a prolonged period of time, resulting in the accumulation of genetic lesions due to IgH CSR or SHM (5, 76). The recent observation that elevated levels of AICDA expression occur pre-AIDS-NHL, but only in those who developed non-CNS lymphomas, is consistent with this conclusion (39). AICDA is a B cell activation associated DNA mutating molecule that plays a central role in both IgH CSR and SHM in germinal center B cells (77). Interestingly, AICDA expression can be induced in B cells by exposure to HIV (78), as well as other lymphomagenic viruses, including EBV and HCV (79–81), suggesting a direct role for HIV in the induction of B cell activation. Studies to quantify AICDA expression and its association with HIV levels in the same cases and controls included in this study are planned.
The assessment of additional cytokines and immune stimulatory molecules other than those that were quantified in this study would have been informative. However, we focused on those molecules for which we had compelling preliminary evidence in prior preliminary cross-sectional studies, and for which robust immunoassays were available, given the limited volume of pre-NHL diagnosis serum that is available. As multiplexed immunoassays are becoming more sensitive and reliable, we hope to assess additional biomarkers in the future.
In summary, levels of B cell stimulatory cytokines and of molecules associated with immune activation are elevated several years preceding the diagnosis of AIDS-NHL. These results are consistent with the hypothesis that chronic B cell hyper-activation contributes to the development of these lymphomas.
Supplementary Material
Acknowledgments
Financial Support: This work was supported by grants from the Leukemia and Lymphoma Society (USA) (6155– 03), and the National Institutes of Health (R01-CA57152, R01-CA73475, K07- CA140360), including the Specialized Program Of Research Excellence (SPORE) in Lymphoma (P50-CA96888), the UCLA Older Americans Independence Center (OAIC) and the OAIC Inflammatory Biology Core (P30-AG028748), and the Intramural Research Program, National Cancer Institute. The MACS is funded by the National Institute of Allergy and Infectious Diseases, with additional supplemental funding from the National Cancer Institute (UO1-AI-35042, UL1-RR025005 [GCRC], UO1-AI-35043, UO1-AI-35039, UO1-AI-35040, UO1-AI-35041).
Samples and data in this manuscript were collected by the Multicenter AIDS Cohort Study (MACS) with centers (Principal Investigators) at The Johns Hopkins Bloomberg School of Public Health (Joseph B. Margolick, Lisa P. Jacobson), Howard Brown Health Center, Feinberg School of Medicine, Northwestern University, and Cook County Bureau of Health Services (John P. Phair, Steven M. Wolinsky), University of California, Los Angeles (Roger Detels), and University of Pittsburgh (Charles R. Rinaldo); website located at http://www.statepi.jhsph.edu/macs/macs.html. Some of this work was carried out in the facilities of the UCLA AIDS Institute, which were supported, in part, by funds from the James B. Pendleton Charitable Trust and the McCarthy Family Foundation. The authors would like to thank Guadalupe Peña and Celeste Sanchez for assistance with sample and data management, Zheng Hu and Malgorzata Grodsky for assistance with analyses, and the MACS participants, without whom this and many other studies would not be possible.
References
- 1.Ziegler JL, Beckstead JA, Volberding PA, Abrams DI, Levine AM, Lukes RJ, et al. Non-Hodgkin’s lymphoma in 90 homosexual men. Relation to generalized lymphadenopathy and the acquired immunodeficiency syndrome. N Engl J Med. 1984;311:565–70. doi: 10.1056/NEJM198408303110904. [DOI] [PubMed] [Google Scholar]
- 2.Beral V, Peterman T, Berkelman R, Jaffe H. AIDS-associated non-Hodgkin lymphoma. Lancet. 1991;337:805–9. doi: 10.1016/0140-6736(91)92513-2. [DOI] [PubMed] [Google Scholar]
- 3.Armenian HK, Hoover DR, Rubb S, Metz S, Martinez-Maza O, Chmiel J, et al. Risk factors for non-Hodgkin’s lymphomas in acquired immunodeficiency syndrome (AIDS) Am J Epidemiol. 1996;143:374–9. doi: 10.1093/oxfordjournals.aje.a008751. [DOI] [PubMed] [Google Scholar]
- 4.Martinez-Maza O, Breen EC. B-cell activation and lymphoma in patients with HIV. Curr Opin Oncol. 2002;14:528–32. doi: 10.1097/00001622-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Epeldegui M, Widney DP, Martinez-Maza O. Pathogenesis of AIDS lymphoma: role of oncogenic viruses and B cell activation-associated molecular lesions. Curr Opin Oncol. 2006;18:444–8. doi: 10.1097/01.cco.0000239882.23839.e5. [DOI] [PubMed] [Google Scholar]
- 6.Grulich AE, Li Y, McDonald AM, Correll PK, Law MG, Kaldor JM. Decreasing rates of Kaposi’s sarcoma and non-Hodgkin’s lymphoma in the era of potent combination anti-retroviral therapy. AIDS. 2001;15:629–33. doi: 10.1097/00002030-200103300-00013. [DOI] [PubMed] [Google Scholar]
- 7.Bonnet F, Balestre E, Thiebaut R, Morlat P, Pellegrin JL, Neau D, et al. Factors associated with the occurrence of AIDS-related non-Hodgkin lymphoma in the era of highly active antiretroviral therapy: Aquitaine Cohort, France. Clin Infect Dis. 2006;42:411–7. doi: 10.1086/499054. [DOI] [PubMed] [Google Scholar]
- 8.Bonnet F, Lewden C, May T, Heripret L, Jougla E, Bevilacqua S, et al. Malignancy-related causes of death in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. Cancer. 2004;101:317–24. doi: 10.1002/cncr.20354. [DOI] [PubMed] [Google Scholar]
- 9.Matthews GV, Bower M, Mandalia S, Powles T, Nelson MR, Gazzard BG. Changes in acquired immunodeficiency syndrome-related lymphoma since the introduction of highly active antiretroviral therapy. Blood. 2000;96:2730–4. [PubMed] [Google Scholar]
- 10.Biggar RJ. AIDS-related cancers in the era of highly active antiretroviral therapy. Oncology (Huntingt) 2001;15:439–48. discussion 448–9. [PubMed] [Google Scholar]
- 11.Seaberg EC, Wiley D, Martínez-Maza O, Chmiel JS, Kingsley L, Tang Y, et al. Cancer incidence in the Multicenter AIDS Cohort Study before and during the HAART era: 1984–2007. Cancer. 2010;116:5507–5516. doi: 10.1002/cncr.25530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tulpule A, Levine A. AIDS-related lymphoma. Blood Rev. 1999;13:147–50. doi: 10.1054/blre.1999.0112. [DOI] [PubMed] [Google Scholar]
- 13.Carbone A, Gloghini A, Capello D, Gaidano G. Genetic pathways and histogenetic models of AIDS-related lymphomas. Eur J Cancer. 2001;37:1270–5. doi: 10.1016/s0959-8049(01)00119-8. [DOI] [PubMed] [Google Scholar]
- 14.Gaidano G, Capello D, Carbone A. The molecular basis of acquired immunodeficiency syndrome-related lymphomagenesis. Semin Oncol. 2000;27:431–41. [PubMed] [Google Scholar]
- 15.Gaidano G, Pastore C, Capello D, Migliazza A, Gloghini A, Saglio G, et al. Involvement of the bcl-6 gene in AIDS-related lymphomas. Ann Oncol. 1997;8 (Suppl 2):105–8. [PubMed] [Google Scholar]
- 16.Wang SS, Hartge P. Epidemiology. In: Armitage JO, Mauch PM, Harris NL, Coiffier B, Dalla-Favera R, editors. Non-Hodgkin Lymphomas. 2nd. Philadelphia, Pennsylvania: Lippincott, Williams and Wilkins; 2010. [Google Scholar]
- 17.MacMahon EM, Glass JD, Hayward SD, Mann RB, Becker PS, Charache P, et al. Epstein-Barr virus in AIDS-related primary central nervous system lymphoma. Lancet. 1991;338:969–73. doi: 10.1016/0140-6736(91)91837-k. [DOI] [PubMed] [Google Scholar]
- 18.Kersten MJ, Klein MR, Holwerda AM, Miedema F, van Oers MH. Epstein-Barr virus-specific cytotoxic T cell responses in HIV-1 infection: different kinetics in patients progressing to opportunistic infection or non-Hodgkin’s lymphoma. J Clin Invest. 1997;99:1525–33. doi: 10.1172/JCI119315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Baarle D, Hovenkamp E, Callan MF, Wolthers KC, Kostense S, Tan LC, et al. Dysfunctional Epstein-Barr virus (EBV)-specific CD8(+) T lymphocytes and increased EBV load in HIV-1 infected individuals progressing to AIDS-related non-Hodgkin lymphoma. Blood. 2001;98:146–55. doi: 10.1182/blood.v98.1.146. [DOI] [PubMed] [Google Scholar]
- 20.International Collaboration on HIV and Cancer. Highly active antiretroviral therapy and incidence of cancer in human immunodeficiency virus-infected adults. J Natl Cancer Inst. 2000;92:1823–30. doi: 10.1093/jnci/92.22.1823. [DOI] [PubMed] [Google Scholar]
- 21.Dalla-Favera R, Ye BH, Lo Coco F, Chang CC, Cechova K, Zhang J, et al. BCL-6 and the molecular pathogenesis of B-cell lymphoma. Cold Spring Harb Symp Quant Biol. 1994;59:117–23. doi: 10.1101/sqb.1994.059.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Gaidano G, Pasqualucci L, Capello D, Berra E, Deambrogi C, Rossi D, et al. Aberrant somatic hypermutation in multiple subtypes of AIDS-associated non-Hodgkin lymphoma. Blood. 2003;102:1833–41. doi: 10.1182/blood-2002-11-3606. [DOI] [PubMed] [Google Scholar]
- 23.Migliazza A, Martinotti S, Chen W, Fusco C, Ye BH, Knowles DM, et al. Frequent somatic hypermutation of the 5′ noncoding region of the BCL6 gene in B-cell lymphoma. Proc Natl Acad Sci USA. 1995;92:12520–4. doi: 10.1073/pnas.92.26.12520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pasqualucci L, Neumeister P, Goossens T, Nanjangud G, Chaganti RS, Kuppers R, et al. Hypermutation of multiple proto-oncogenes in B-cell diffuse large-cell lymphomas. Nature. 2001;412:341–6. doi: 10.1038/35085588. [DOI] [PubMed] [Google Scholar]
- 25.Pasqualucci L, Bereschenko O, Niu H, Klein U, Basso K, Guglielmino R, et al. Molecular pathogenesis of non-Hodgkin’s lymphoma: the role of Bcl-6. Leuk Lymphoma. 2003;44 (Suppl 3):S5–12. doi: 10.1080/10428190310001621588. [DOI] [PubMed] [Google Scholar]
- 26.Birx DL, Redfield RR, Tencer K, Fowler A, Burke DS, Tosato G. Induction of interleukin- 6 during human immunodeficiency virus infection. Blood. 1990;76:2303–10. [PubMed] [Google Scholar]
- 27.Breen EC, Rezai AR, Nakajima K, Beall GN, Mitsuyasu RT, Hirano T, et al. Infection with HIV is associated with elevated IL-6 levels and production. J Immunol. 1990;144:480–4. [PubMed] [Google Scholar]
- 28.Pluda JM, Venzon DJ, Tosato G, Lietzau J, Wyvill K, Nelson DL, et al. Parameters affecting the development of non-Hodgkin’s lymphoma in patients with severe human immunodeficiency virus infection receiving antiretroviral therapy. J Clin Oncol. 1993;11:1099–107. doi: 10.1200/JCO.1993.11.6.1099. [DOI] [PubMed] [Google Scholar]
- 29.Breen EC, Boscardin WJ, Detels R, Jacobson LP, Smith MW, O’Brien SJ, et al. Non-Hodgkin’s B cell lymphoma in persons with acquired immunodeficiency syndrome is associated with increased serum levels of IL10, or the IL10 promoter -592 C/C genotype. Clin Immunol. 2003;109:119–29. doi: 10.1016/s1521-6616(03)00214-6. [DOI] [PubMed] [Google Scholar]
- 30.Rabkin CS, Yang Q, Goedert JJ, Nguyen G, Mitsuya H, Sei S. Chemokine and chemokine receptor gene variants and risk of non-Hodgkin’s lymphoma in human immunodeficiency virus-1-infected individuals. Blood. 1999;93:1838–42. [PubMed] [Google Scholar]
- 31.Dean M, Jacobson LP, McFarlane G, Margolick JB, Jenkins FJ, Howard OM, et al. Reduced risk of AIDS lymphoma in individuals heterozygous for the CCR5-delta32 mutation. Cancer Res. 1999;59:3561–4. [PubMed] [Google Scholar]
- 32.Widney D, Gundapp G, Said JW, van der Meijden M, Bonavida B, Demidem A, et al. Aberrant expression of CD27 and soluble CD27 (sCD27) in HIV infection and in AIDS-associated lymphoma. Clin Immunol. 1999;93:114–23. doi: 10.1006/clim.1999.4782. [DOI] [PubMed] [Google Scholar]
- 33.Breen EC, van der Meijden M, Cumberland W, Kishimoto T, Detels R, Martinez-Maza O. The development of AIDS-associated Burkitt’s/small noncleaved cell lymphoma is preceded by elevated serum levels of interleukin 6. Clin Immunol. 1999;92:293–9. doi: 10.1006/clim.1999.4760. [DOI] [PubMed] [Google Scholar]
- 34.Breen EC, Epeldegui M, Boscardin WJ, Widney DP, Detels R, Martinez-Maza O. Elevated levels of soluble CD44 precede the development of AIDS-associated non- Hodgkin’s B-cell lymphoma. AIDS. 2005;19:1711–2. doi: 10.1097/01.aids.0000184924.04983.7c. [DOI] [PubMed] [Google Scholar]
- 35.Breen EC, Fatahi S, Epeldegui M, Boscardin WJ, Detels R, Martinez-Maza O. Elevated serum soluble CD30 precedes the development of AIDS-associated non-Hodgkin’s B cell lymphoma. Tumour Biol. 2006;27:187–94. doi: 10.1159/000093022. [DOI] [PubMed] [Google Scholar]
- 36.Yawetz S, Cumberland WG, van der Meyden M, Martinez-Maza O. Elevated serum levels of soluble CD23 (sCD23) precede the appearance ofacquired immunodeficiency syndrome--associated non-Hodgkin’s lymphoma. Blood. 1995;85:1843–9. [PubMed] [Google Scholar]
- 37.Schroeder JR, Saah AJ, Ambinder RF, Martinez-Maza O, Crabb Breen E, Variakojis D, et al. Serum sCD23 level in patients with AIDS-related non-Hodgkin’s lymphoma is associated with absence of Epstein-Barr virus in tumor tissue. Clin Immunol. 1999;93:239–44. doi: 10.1006/clim.1999.4793. [DOI] [PubMed] [Google Scholar]
- 38.Schroeder JR, Saah AJ, Hoover DR, Margolick JB, Ambinder RF, Martinez-Maza O, et al. Serum soluble CD23 level correlates with subsequent development of AIDS-related non-Hodgkin’s lymphoma. Cancer Epidemiol Biomarkers Prev. 1999;8:979–84. [PubMed] [Google Scholar]
- 39.Widney DP, Gui D, Popoviciu LM, Said JW, Breen EC, Huang X, et al. Expression and function of the chemokine, CXCL13, and its receptor, CXCR5, in AIDS-associated non-Hodgkin’s lymphoma. AIDS Research and Treatment. 2010 doi: 10.1155/2010/164586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Epeldegui M, Breen EC, Hung YP, Boscardin WJ, Detels R, Martinez-Maza O. Elevated expression of activation induced cytidine deaminase in peripheral blood mononuclear cells precedes AIDS-NHL diagnosis. AIDS. 2007;21:2265–2270. doi: 10.1097/QAD.0b013e3282ef9f59. [DOI] [PubMed] [Google Scholar]
- 41.Gordon J. CD23 and B cell activation. Clin Exp Allergy. 1992;22:199–204. doi: 10.1111/j.1365-2222.1992.tb03073.x. [DOI] [PubMed] [Google Scholar]
- 42.Gordon J. B-cell signalling via the C-type lectins CD23 and CD72. Immunol Today. 1994;15:411–7. doi: 10.1016/0167-5699(94)90270-4. [DOI] [PubMed] [Google Scholar]
- 43.Locksley RM, Killeen N, Lenardo MJ. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell. 2001;104:487–501. doi: 10.1016/s0092-8674(01)00237-9. [DOI] [PubMed] [Google Scholar]
- 44.Detels R, Phair J, Saah A, Rinaldo C, Muñoz A, Kaslow R, et al. Recent scientific contributions to understanding HIV/AIDS from the Multicenter AIDS Cohort Study. Journal of Epidemiology (Japan) 1992;2 (Suppl):S11–S19. [Google Scholar]
- 45.1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41:1–19. [PubMed] [Google Scholar]
- 46.Kanowith-Klein S, Saxon A. Fc epsilon receptors on human cell lines and peripheral blood lymphocytes detected by binding of IgE immune complexes. J Clin Immunol. 1985;5:38–45. doi: 10.1007/BF00915167. [DOI] [PubMed] [Google Scholar]
- 47.Zhang K, Clark EA, Saxon A. CD40 stimulation provides an IFN-gamma-independent and IL-4-dependent differentiation signal directly to human B cells for IgE production. J Immunol. 1991;146:1836–42. [PubMed] [Google Scholar]
- 48.Mellors JW, Margolick JB, Phair JP, Rinaldo CR, Detels R, Jacobson LP, et al. Prognostic value of HIV-1 RNA, CD4 cell count, and CD4 Cell count slope for progression to AIDS and death in untreated HIV-1 infection. JAMA. 2007;297:2349–50. doi: 10.1001/jama.297.21.2349. [DOI] [PubMed] [Google Scholar]
- 49.Mellors JW, Munoz A, Giorgi JV, Margolick JB, Tassoni CJ, Gupta P, et al. Plasma viral load and CD4+ lymphocytes as prognostic markers of HIV-1 infection. Ann Intern Med. 1997;126:946–54. doi: 10.7326/0003-4819-126-12-199706150-00003. [DOI] [PubMed] [Google Scholar]
- 50.Heinrich PC, Castell JV, Andus T. Interleukin-6 and the acute phase response. Biochem J. 1990;265:621–36. doi: 10.1042/bj2650621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Newell ME, Hoy JF, Cooper SG, DeGraaff B, Grulich AE, Bryant M, et al. Human immunodeficiency virus-related primary central nervous system lymphoma: factors influencing survival in 111 patients. Cancer. 2004;100:2627–36. doi: 10.1002/cncr.20300. [DOI] [PubMed] [Google Scholar]
- 52.Bertolini JN, Benson EM. The role of human interleukin-6 in B-cell isotype regulation and differentiation. Cell Immunol. 1990;125:197–209. doi: 10.1016/0008-8749(90)90074-2. [DOI] [PubMed] [Google Scholar]
- 53.Kishimoto T, Akira S, Narazaki M, Taga T. Interleukin-6 family of cytokines and gp130. Blood. 1995;86:1243–54. [PubMed] [Google Scholar]
- 54.Wei LH, Kuo ML, Chen CA, Chou CH, Cheng WF, Chang MC, et al. The anti-apoptotic role of interleukin-6 in human cervical cancer is mediated by up-regulation of Mcl-1 through a PI 3-K/Akt pathway. Oncogene. 2001;20:5799–809. doi: 10.1038/sj.onc.1204733. [DOI] [PubMed] [Google Scholar]
- 55.Chauhan D, Kharbanda S, Ogata A, Urashima M, Teoh G, Robertson M, et al. Interleukin-6 inhibits Fas-induced apoptosis and stress-activated protein kinase activation in multiple myeloma cells. Blood. 1997;89:227–34. [PubMed] [Google Scholar]
- 56.Nakajima K, Martinez-Maza O, Hirano T, Breen EC, Nishanian PG, Salazar-Gonzalez JF, et al. Induction of IL-6 (B cell stimulatory factor-2/IFN-beta 2) production by HIV. J Immunol. 1989;142:531–6. [PubMed] [Google Scholar]
- 57.Takeshita S, Breen EC, Ivashchenko M, Nishanian PG, Kishimoto T, Vredevoe DL, et al. Induction of IL-6 and IL-10 production by recombinant HIV-1 envelope glycoprotein 41 (gp41) in the THP-1 human monocytic cell line. Cell Immunol. 1995;165:234–42. doi: 10.1006/cimm.1995.1210. [DOI] [PubMed] [Google Scholar]
- 58.Sawa Y, Ueki T, Hata M, Iwasawa K, Tsuruga E, Kojima HI, et al. LPS-induced IL-6, IL-8, VCAM-1, and ICAM-1 expression in human lymphatic endothelium. J Histochem Cytochem. 2008;56:97–109. doi: 10.1369/jhc.7A7299.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Annunziato F, Cosmi L, Liotta F, Maggi E, Romagnani S. The phenotype of human Th17 cells and their precursors, the cytokines that mediate their differentiation and the role of Th17 cells in inflammation. Int Immunol. 2008;20:1361–8. doi: 10.1093/intimm/dxn106. [DOI] [PubMed] [Google Scholar]
- 60.Romagnani S, Maggi E, Liotta F, Cosmi L, Annunziato F. Properties and origin of human Th17 cells. Mol Immunol. 2009;47:3–7. doi: 10.1016/j.molimm.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 61.Ekstrom Smedby K, Vajdic CM, Falster M, Engels EA, Martinez-Maza O, Turner J, et al. Autoimmune disorders and risk of non-Hodgkin lymphoma subtypes: a pooled analysis within the InterLymph Consortium. Blood. 2008;111:4029–38. doi: 10.1182/blood-2007-10-119974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gruss HJ, DaSilva N, Hu ZB, Uphoff CC, Goodwin RG, Drexler HG. Expression and regulation of CD30 ligand and CD30 in human leukemia-lymphoma cell lines. Leukemia. 1994;8:2083–94. [PubMed] [Google Scholar]
- 63.Gruss HJ, Boiani N, Williams DE, Armitage RJ, Smith CA, Goodwin RG. Pleiotropic effects of the CD30 ligand on CD30-expressing cells and lymphoma cell lines. Blood. 1994;83:2045–56. [PubMed] [Google Scholar]
- 64.Bowman MR, Crimmins MA, Yetz-Aldape J, Kriz R, Kelleher K, Herrmann S. The cloning of CD70 and its identification as the ligand for CD27. J Immunol. 1994;152:1756–61. [PubMed] [Google Scholar]
- 65.Hintzen RQ, Lens SM, Koopman G, Pals ST, Spits H, van Lier RA. CD70 represents the human ligand for CD27. Int Immunol. 1994;6:477–80. doi: 10.1093/intimm/6.3.477. [DOI] [PubMed] [Google Scholar]
- 66.Caligaris-Cappio F, Bertero MT, Converso M, Stacchini A, Vinante F, Romagnani S, et al. Circulating levels of soluble CD30, a marker of cells producing Th2-type cytokines, are increased in patients with systemic lupus erythematosus and correlate with disease activity. Clin Exp Rheumatol. 1995;13:339–43. [PubMed] [Google Scholar]
- 67.De Milito A, Morch C, Sonnerborg A, Chiodi F. Loss of memory (CD27) B lymphocytes in HIV-1 infection. AIDS. 2001;15:957–64. doi: 10.1097/00002030-200105250-00003. [DOI] [PubMed] [Google Scholar]
- 68.Agematsu K, Hokibara S, Nagumo H, Komiyama A. CD27: a memory B-cell marker. Immunol Today. 2000;21:204–6. doi: 10.1016/s0167-5699(00)01605-4. [DOI] [PubMed] [Google Scholar]
- 69.Tangye SG, Liu YJ, Aversa G, Phillips JH, de Vries JE. Identification of functional human splenic memory B cells by expression of CD148 and CD27. J Exp Med. 1998;188:1691–703. doi: 10.1084/jem.188.9.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Klein U, Rajewsky K, Kuppers R. Human immunoglobulin (Ig)M+IgD+ peripheral blood B cells expressing the CD27 cell surface antigen carry somatically mutated variable region genes: CD27 as a general marker for somatically mutated (memory) B cells. J Exp Med. 1998;188:1679–89. doi: 10.1084/jem.188.9.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Purdue MP, Lan Q, Martinez-Maza O, Oken MM, Hocking W, Huang WY, et al. A prospective study of serum soluble CD30 concentration and risk of non-Hodgkin lymphoma. Blood. 2009;114:2730–2. doi: 10.1182/blood-2009-04-217521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moore KW, O’Garra A, de Waal Malefyt R, Vieira P, Mosmann TR. Interleukin-10. Annu Rev Immunol. 1993;11:165–90. doi: 10.1146/annurev.iy.11.040193.001121. [DOI] [PubMed] [Google Scholar]
- 73.Mosmann TR, Moore KW. The role of IL-10 in crossregulation of TH1 and TH2 responses. Immunol Today. 1991;12:A49–53. doi: 10.1016/S0167-5699(05)80015-5. [DOI] [PubMed] [Google Scholar]
- 74.Wong HL, Breen EC, Pfeiffer RM, Aissani B, Martinson JJ, Margolick JB, et al. Cytokine signaling pathway polymorphisms and AIDS-related non-Hodgkin lymphoma risk in the multicenter AIDS cohort study. AIDS. 2010;24:1025–33. doi: 10.1097/QAD.0b013e328332d5b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Masood R, Zhang Y, Bond MW, Scadden DT, Moudgil T, Law RE, et al. Interleukin-10 is an autocrine growth factor for acquired immunodeficiency syndrome-related B-cell lymphoma. Blood. 1995;85:3423–30. [PubMed] [Google Scholar]
- 76.Vendrame E, Martinez-Maza O. Assessment of pre-diagnostic biomarkers of immune activation and inflammation: Insights on the etiology of lymphoma. J Proteome Res. 2011 Jan 7;10:113–119. doi: 10.1021/pr100729z. Epub 2010 Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Muramatsu M, Kinoshita K, Fagarasan S, Yamada S, Shinkai Y, Honjo T. Class switch recombination and hypermutation require activation-induced cytitine deaminase (AID), a potential RNA editing enzyme. Cell. 2000;102:553–63. doi: 10.1016/s0092-8674(00)00078-7. [DOI] [PubMed] [Google Scholar]
- 78.Epeldegui M, Thapa DR, De La Cruz J, Kitchen SG, Zack JA, Martinez-Maza O. CD40 Ligand (CD154) Incorporated into HIV Virions Induces Activation-Induced Cytidine Deaminase (AID) Expression in Human B Lymphocytes. PLoS One. 2010;5:e11488. doi: 10.1371/journal.pone.0011448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Epeldegui M, Hung YP, McQuay A, Ambinder RF, Martinez-Maza O. Infection of human B cells with Epstein-Barr virus results in the expression of somatic hypermutation-inducing molecules and in the accrual of oncogene mutations. Mol Immunol. 2007;44:934–42. doi: 10.1016/j.molimm.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 80.Machida K, Cheng KT, Sung VM, Shimodaira S, Lindsay KL, Levine AM, et al. Hepatitis C virus induces a mutator phenotype: enhanced mutations of immunoglobulin and protooncogenes. Proc Natl Acad Sci USA. 2004;101:4262–7. doi: 10.1073/pnas.0303971101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.He B, Raab-Traub N, Casali P, Cerutti A. EBV-encoded latent membrane protein 1 cooperates with BAFF/BLyS and APRIL to induce T cell-independent Ig heavy chain class switching. J Immunol. 2003;171:5215–24. doi: 10.4049/jimmunol.171.10.5215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.