Abstract
Chest trauma is one important factor for total morbidity and mortality in traumatized emergency patients. The complexity of injury in trauma patients makes it challenging to provide an optimal oxygenation while protecting the lung from further ventilator-induced injury to it. On the other hand, lung trauma needs to be treated on an individual basis, depending on the magnitude, location and type of lung or chest injury. Several aspects of ventilatory management in emergency patients are summarized herein and may give the clinician an overview of the treatment possibilities for chest trauma victims.
Keywords: Chest trauma, instability of rib cage, mechanical ventilation, pneumothorax, spontaneous breathing
INTRODUCTION
The lethality of isolated chest traumas is about 5% to 8%. Up to 25% of all deaths caused by trauma are related to chest injuries,[1] and mortality dramatically increases as a function of increased chest trauma force.[2] Direct forces, abrupt deceleration and other mechanisms can cause injury to thoracic structures like major intrathoracic vessels or the heart. Chest injuries often occur in combination with other severe injuries, such as extremity, head and brain and abdominal injuries.[1]
Chest trauma, as shown in Table 1, can occur after vehicle collisions, assaults, falls and explosive blasts via a variety of different mechanisms.[3] In elderly patients, a minor trauma can cause a more serious injury due to the increased stiffness of the rib cage as a function of advanced age. In contrast, in children, the elasticity of the osseous structures of the chest can lead to an underestimation of parenchymateous injuries.
Table 1.
Injuries after chest trauma
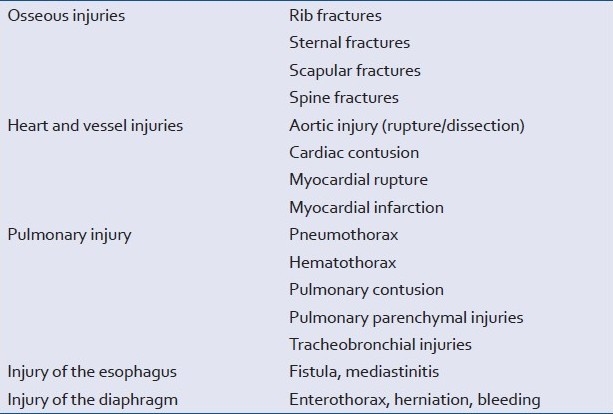
Penetrating injuries are mostly caused by gunshot, stitch or impalement damage, and the impact of a blunt trauma is typically conducted to many different intrathoracic structures; hence nearly all organs of the thoracic cavity can be involved in chest trauma. The most common types of collateral damage that result from chest trauma include injuries to ribs, lung contusion, hematoma of the chest wall, pleural effusion, pneumothorax and hematothorax.[4–6]
PATHOPHYSIOLOGICAL ASPECTS
Respiratory impairment
Damage to the osseous structure of the thorax by rib and sternum fractures destabilizes the rib cage and impairs spontaneous breathing mechanics substantially. This condition is amplified by pain, which further reduces breathing function. Direct traumatic damage to the lung (i.e., lung contusion), in combination with a concurrent increase in vascular permeability of the lung capillaries in the injured area, leads to an extravasation of protein-rich fluid with an altered surfactant composition, eventually resulting in slow but progressive respiratory failure.[7,8]
The disturbance of diffusion, the reduction of compliance and functional residual capacity and ventilation-perfusion mismatch create an intrapulmonary shunt with subsequent elevated PaCO2 levels and reduced oxygenation.[9,10] After severe chest trauma, intrapulmonary shunting can also be caused by a disruption of pulmonary capillaries and extravasation into the alveolar spaces. Aspiration of blood and/ or gastric contents, fat embolism to the lung due to long bone fractures and systemic inflammatory response syndrome may additionally exacerbate respiratory deficits and may lead to acute lung injury (ALI) or acute respiratory distress syndrome (ARDS).[11]
After alveolar overdistension and rupture, extra-alveolar gas has the potential (supported by mechanical ventilation) to move along the pressure gradient through the damaged alveolar wall into the bronchovascular space and pulmonary interstitium, causing pulmonic interstitial emphysema.[12] The extra-alveolar gas may push further into the pleural cavity, mediastinum and subcutaneous tissues. As a consequence, bronchoalveolar fistula, pneumothorax or tension pneumothorax, and emphysema may develop.
Cardiovascular impairment
A reduction in normal intraventricular filling by tension pneumothorax, pericardial tamponade or massive hemorrhage may result in a life-threatening reduction in cardiac output. Moreover, intracardiac structural damage or heart contusions with concomitant arrhythmias are additional contributors to reduced cardiac output.
DIAGNOSTIC STRATEGIES
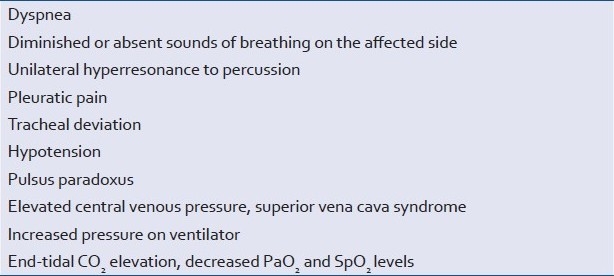
Patient history can provide clues about the severity of trauma and the resultant injuries. Instability of the thorax, signs of hemorrhagic shock, low cardiac output and intrathoracic bowel sounds indicating diaphragm rupture are the clinical signs of severe chest trauma. Table 2 provides an overview of chest injury indicators.
Table 2.
Clinical signs of chest trauma

The location of a chest injury may provide signs of associated injuries. Fractures of the 1st to 3rd ribs indicate severe causative forces because of their protected location and may be associated with mediastinal injury. Therefore, injuries of large blood vessels (aorta) or tracheal/ bronchial structures may be associated and must be specifically excluded. Lower rib (9th to 12th ribs)[13] fractures are more often associated with hepatic injury on the right side, splenic laceration on the left side or renal injury on the posterior lower chest wall.
Exact preclinical diagnosis is typically difficult. A spiral computed tomography (CT) scan of the chest and an echocardiogram provide the most diagnostic information concerning intrathoracic injuries. If necessary, chest x-ray, bronchoscopy, pulmonal angio-CT, and an electrocardiogram may provide further diagnostic information. Clinicians must be aware that patients remain at risk for deterioration and that radiographic findings may develop with a time delay of up to four hours or more after injury.
THERAPEUTIC STRATEGIES FOR SELECTED INJURIES
1) Chest wall osseous injuries
Injuries of one or two ribs are typically not dangerous and can be handled without hospital admission; however, at any level of rib fracture, the risk of pneumothorax and pulmonary contusion exists.
More than two rib fractures put the patient at significant risk of complications.
Fractures of more than two adjacent ribs at two different locations result in thorax instability with paradoxical motion. This flail chest condition is most often accompanied by an underlying pulmonary parenchymal injury and can be life threatening.
The pleural cavity generates negative pressure during inspiration, and the chest wall moves outwards during inspiration; however, in the case of flail chest, the floating segment of chest wall and soft tissue will move paradoxically in an inward direction, resulting in elevated respiratory effort, dyspnea and hypoxemia.[14]
Therapeutic aspects
A sufficient reduction in pain is critical to optimizing patient ventilation. Therein, the systemic administration of painkillers, regional anesthesia with intercostal blockades, pleural catheters and thoracic epidurals as well as paravertebral blockades may be helpful.
Epidural analgesia has been demonstrated to beneficially impact ventilatory function in patients suffering from blunt chest trauma[15] and is associated with a decreased rate of nosocomial pneumonia and a reduced duration of mechanical ventilation in patients after rib fractures.[16] Pneumatic stabilization is based on the use of positive intrathoracic pressure provided by noninvasive positive-pressure ventilation (NPPV) by mask; or after intubation, by invasive positive-pressure ventilation (IPPV).[17]
Preventing atelectasis and pneumonia requires additional chest physiotherapy. Frequent flexible bronchoscopy typically provides sufficient removal of secretions and blood from the lungs. In severe cases of chest wall instability, reconstruction of vertebrosternal ribs 3, 6 and 9 at an early stage may be required.[18] Surgical stabilization has been found to be associated with a faster recovery of pulmonary function and a shorter ICU time in a select group of flail chest patients who required prolonged ventilatory support.[17,19]
2) Pneumothorax
Injuries of the lungs or the thoracic wall can create a pleural injury, resulting in the collection of air in the pleural space, which is associated with a collapse of the lung. Consequently, all penetrating thoracic injuries and most blunt chest injuries are associated with pneumothorax. Occult pneumothorax among victims of blunt trauma appears in 2% to 55% of patients who undergo CT scans.[20] The closed form, or a small pneumothorax, is mostly inconspicuous; however, tension pneumothorax may occur when the amount of air in the pleural space increases and the loss of air is impaired or impossible due to a valve mechanism. This results in a displacement of the mediastinal structures and the lungs and induces a reduction of venous flow to the heart, reducing cardiac output. Clinical signs of pneumothorax, which can vary depending on its extent, are summarized in Table 3. Many patients after penetrating trauma have been diagnosed to have a hemopneumothorax, in the absence of clinical findings. Chest radiograph or CT scan should be the initial test for all patients with penetrating chest injuries[21] or blunt thoracic trauma.[22] Ultrasound is also useful in the diagnosis of pneumothorax and hematothorax.[6,23]
Table 3.
Clinical signs of pneumothorax
Therapeutic aspects
Thorax drainage should be performed except in asymptomatic patients with occult pneumothorax, although they should be closely observed.[24] Patients who are mechanically ventilated should be treated immediately with a tube thoracostomy to prevent the development of tension pneumothorax.
Suspected tension pneumothorax is typically treated with immediate decompression of the pleural space by blunt dissection and finger decompression. This is a reliable and safe procedure prior to chest tube insertion. Needle thoracocentesis should be the technique of last resort during hospital and trauma reception, because of significant failure rates; and the delay in providing formal pleural decompression, caused due to incorrect needle placement.[25]
Thorax drainage is typically performed to drain air as well as blood and to reduce the air leak due to bronchopulmonal fistulas. The optimal tube size depends on the air leakage rate, wherein a tube size of 28 or 32 French is normally sufficient for patients who develop pneumothorax during mechanical ventilation or for traumatic pneumothoraces with the risk of a large air leak due to bronchopulmonal fistulas. Larger chest tubes or an additional chest tube should be considered if an additional drainage of blood is necessary.
The application of negative pressure to the drainage system may be necessary to maintain lung expansion, but it has the potential to increase fistula flow and retard closure.[26] Pleural drainage systems can vary in their ability to evacuate large gas flows (6-50 L/min).[27] Some patients have highly variable fistula flows, which can be influenced by body position. These patients should choose a body position that produces the smallest possible fistula gas flow. Patients with high fistula flows, wherein reexpansion of the lungs cannot be achieved, may require further surgical treatment (i.e., fistula closure or lobectomy).
Nonconventional efforts were made to decrease bronchopulmonary flow. The principle behind these methods is either an intermittent thoracostomy tube closure during mechanical inhalation and a release during exhalation[28,29]; or a “counter-pressure” in the form of positive intrapleural pressure, similar to the positive intrapulmonary pressure at the end of expiration (PEEP).[30,32] Such methods are only allowed under careful monitoring in the ICU setting.
If mechanical ventilation is needed, the ventilator setting should support fistula closure and limit inflationary pressure (peak, plateau and end-expiratory) and volume. Early spontaneous breathing might support fistula closure.
3) Hematothorax or hematopneumothorax
Sources of massive bleeding can include aortic rupture, myocardial rupture and injuries to hilar structures. Other sources could be injuries to the chest wall with lesions on intercostal or mammary blood vessels. The hemodynamic reduction of cardiac output may reach the level of hemorrhagic shock.
Therapeutic aspects
Thoracic drainage is the therapy of choice. The intent of thoracic draining is the drainage and quantification of blood, removal of possible coexisting pneumothorax, and tamponade of the bleeding source. Arterial hemorrhage is life threatening; therefore, the amount of blood loss must be closely monitored.
An initial blood loss in excess of 1,500 mL (≥20 mL/kg) or a blood loss of about 300-500 mL/h via the chest tube should lead to a surgical thoracotomy to stop bleeding.[33,34]
If a hematothorax is not drained, coagulated blood can produce a clotted hemothorax, empyema and fibrothorax, with a prolonged disturbance of ventilation, which results in extended hospitalization. If the chest tube does not effectively drain the blood, thoracoscopic drainage is a further possibility within the first week.[18]
4) Respiratory duct injury
Tracheal or bronchial injuries mostly occur as a component of multiple trauma, and the majority of patients with such injuries die before hospital admission.[35] Injuries of the upper airways are usually caused by blunt or, to a lesser extent, penetrating chest traumas. Injury of the cranial part of the trachea is uncommon, but it can occur even from a direct, low-energy blow.
Approximately 80% of tracheobronchial ruptures are located around the carina (approximately a 2-cm radius) and are caused by high-energy trauma. The right main bronchus is involved more often than the left main bronchus.[36,37] Such injuries usually involve the pars membranacea of the trachea; whereas in the main bronchi, the ruptures are transversal between two chondral rings.
Dyspnea, hemoptysis, emphysema, pneumothorax and pneumomediastinum that reaccumulates despite tube thoracostomy and continuous air loss after placement of a chest tube are clinical manifestations of tracheobronchial injury.[38] Diagnosis is achieved by bronchoscopy and is often difficult. Signs of airway-vascular communication — such as hemoptysis and sudden cardiovascular or neurologic dysfunction; air in arterial aspiration; and air in retinal vessels — may alert the clinician to symptoms of life-threatening systemic air embolism.
Therapeutic aspects
Intubation should be performed during spontaneous breathing if possible because positive-pressure ventilation may enlarge an incomplete rupture and may worsen symptoms. Ruptures above the carina can be protected with a single- or double-lumen tube, whereas ruptures at the carina level or more distal ones make a double-lumen tube indispensable.[39] Further distally, a univent bronchial blocker may be necessary to isolate the affected bronchopulmonary segment and to promote healing.[40,41] Surgical closure is usually necessary.[33] In cases of systemic air embolism where the source is suspected on one side, one-lung ventilation may be applied. In cases of bilateral sources of airway-vascular communication, the ventilation pressure should be kept as low as possible to decrease a further collection of air in the vascular system.
5) Lung contusion
Lung contusion is the most frequently diagnosed intrathoracic injury that results from blunt trauma.[42] Isolated lung contusions are considered more benign.[43] The risk of pulmonary contusion appears to correlate with the severity of forces and the proximity of the zone of the impact to the patient.[44] In the early phase of injury, the impairment of oxygenation seems to correlate with the involved lung tissue.[45] Clinically, gas exchange impairment is obvious. Chest x-ray with irregular, nonlobular opacification provides no indication of the severity of contusion and cannot lead to a reliable prognosis. Thorax CT scan and blood gases are better indicators of the grade of lung contusion.[46,47]
Therapeutic aspects
Respiratory relief can be achieved by positive-pressure ventilation (i.e., continuous positive airway pressure, CPAP), sufficient pain management, physiotherapy and pulmonary drainage (to prevent pneumonia). Pulmonary drainage may be successfully supported by high-frequency chest wall oscillation (HFCWO).[48] In severe cases, the need for volume and blood substitution can add further damage to the lung parenchyma by capillary leakage. In cases of impaired gas exchange, intubation and mechanical ventilation are necessary. Additionally, early fixation of concomitant long bone fractures may prevent further pulmonary complications, such as acute respiratory distress syndrome (ARDS).
Other related injuries after chest trauma include rare traumatic diaphragmatic rupture, which requires surgical repair.[49]
VENTILATION STRATEGIES
The presence of pulmonary contusion with or without flail chest is usually associated with a high incidence of ventilatory support requirements[50]; however, there is often no clear correlation between the affected lung volume and the severity and duration of hypoxemia.[3] Respiratory support can avoid asynchronous paradoxical movements and can achieve pneumatic stabilization. A general optimal ventilatory strategy that is applicable to all patients after chest trauma does not exist. Understanding the pathophysiology of individual patients, with their specific kinds of lung damage after trauma, and accordingly devising and implementing ventilation strategies may support the respiratory system and prevent further ventilator-associated lung injury (VALI). VALI has the potential to induce acute lung injury (ALI) or ARDS, as well as multiple organ failure.[51,52]
The risk factors for developing trauma-associated ARDS include direct pulmonary injury, direct chest wall injury, aspiration, hemorrhagic shock, massive transfusion, old age, underlying diseases, malignancy, severe traumatic brain injury, and quadriplegia.[53,54]
Clinicians need to be aware that barotrauma, as well as VALI in general, results from elevated pulmonary pressures, large tidal volumes, overdistension and an increased fraction of inspired oxygen, viz., FiO2 >0.6. Limiting plateau airway pressures and reducing tidal volumes help minimize the risk of VALI. Therefore, it is helpful that physiological parameters (e.g., SpO2, CO2, pH) need not be corrected to physiologic norms, as previously described.[55] One exception involves patients with elevated intracranial pressures (ICPs), where normoventilation should be achieved. In trauma patients, wherein thorax injury is combined with head injuries (about 18% of fatally injured car drivers),[56] an additional goal is to optimize the cerebral perfusion pressure. Hypercapnia and acidosis compromise cerebral perfusion and should therefore be avoided in these patients.
In addition to VALI, other problems can occur in combination with mechanical ventilation. One important complication is the reduction of cardiac output due to elevated intrathoracic pressure created by positive-pressure ventilation with resultant reduced venous return and hypotension. The challenge for the physician is to achieve the fine balance between ventilation, oxygenation and adequate cardiac output in chest trauma patients.
Clinicians can select between two different strategies to apply mechanical ventilation: noninvasive positive-pressure ventilation (NPPV) and invasive positive-pressure ventilation (IPPV).
Noninvasive positive-pressure ventilation
NPPV delivers positive pressure to patients through nasal, facial or helmet interfaces, without an endotracheal airway, and should be used in cooperative patients without hemodynamic instability, facial injuries and a risk of aspiration. NPPV is typically associated with fewer serious complications, a shorter stay at the ICU, shorter periods of ventilation and improvements in oxygenation.[57,58] NPPV may reduce the incidence of intubation in patients with chest trauma–induced hypoxemia.[59] Therefore, NPPV should be considered the first choice in the absence of contraindications. In the event of noncompliance or failure to respond, intubation and IPPV are indicated.
The advantages of noninvasive ventilation are the avoidance of complications related to endotracheal intubation, avoidance of sedation and paralysis and the easy removal and reinstitution of NPPV, if needed. There are no guidelines for administering continuous or intermittent NPPV therapy, and so it should be adapted to the patient's needs.
The disadvantages of NPPV are typically related to the interface (a mask with an air leak and necrosis) and the lack of a protected airway. However, tracheal intubation should never be delayed if the respiratory status worsens under NPPV.
Invasive positive-pressure ventilation
The choice of endotracheal tube depends on the type of injury and the requirements of further surgery. Trauma patients with maxillofacial injury, full stomach, cervical spine instability, neck hematoma, laryngeal injury or respiratory distress may require more extensive airway management.[50,61] IPPV should be primarily selected in patients who need a definitive airway and need to be protected from aspiration.
Ventilator setting
NPPV is part of a noninvasive technique that delivers continuous PEEP or CPAP, or it is used to maintain two positive airway pressures [pressure support ventilation (PSV) and PEEP]. The avoidance of airway and alveolar collapse by CPAP prevents atelectasis, maintains functional residual capacity and increases cardiac output. In the PSV mode, the patient triggers the ventilator to provide a variable flow of gas that increases until airway pressure reaches a selected limit. Patients with PSV control the respiratory rate and the inspiratory and expiratory times. The setting should be adjusted to provide the lowest inspiratory pressures or volumes needed to obtain improved gas exchange and patient comfort.[62] A pressure differential of 5 cm H2O should be maintained between the inspiratory positive airway pressure and expiratory positive airway pressure (EPAP), starting with an EPAP of 3 cm H2O. Inspiratory and expiratory pressures can be gradually increased over the course of 5 minutes if necessary. The impact of these pressure changes on oxygenation improvement should be monitored by using continuous pulse oximetry and end-tidal CO2.
Higher EPAP levels (≥12 cm H2O) may require IPPV. The implementation of the open lung concept with a PEEP ≥10 cm H2O increases normally aerated lung volume and arterial oxygenation in patients with severe chest trauma.[63] Otherwise, patients with significant lung contusion and poor lung compliance have an increased risk of barotrauma. In patients with hemorrhagic shock, PEEP levels higher than 5 cm H2O can exacerbate hypotension.
Therefore, this type of trauma patient needs a ventilator strategy that minimizes airway pressure[64] and incorporates permissive hypercapnia, meaning that the strategy of protective mechanical ventilation should be applied by limiting peak lung distension and preventing end-expiratory collapse with —
1. Low tidal volumes
Tidal volumes of 6 mL/kg of predicted body weight;
for men = [50+0.91 • (body height in cm – 152.4)] and
for women = [45.5+0.91 • (body height in cm – 152.4)].
2. Limited plateau pressure viz., <30 cm H2O
A plateau pressure <28 cm H2O is associated with less tidal hyperinflation and is even more protective than a plateau pressure (Pplat) <30 cm H2O in patients with a large, dependent and nonaerated lung compartment.[65] To adequately distend the lung, in several types of patients (e.g., with morbid obesity), higher, additional pressures [including elevated PEEP (as the first choice)] might be needed to lift the restricted chest wall away from the lung.
3. An FiO2 that is as low as possible
Unclear initial situations in polytraumatized patients require high FiO2 values. This is supported by studies that have shown a lower mortality in animals with hemorrhagic shock and with high FiO2 levels,[66] and a better prognosis in patients with head and brain injuries.[67] Under controlled conditions of an ICU, FiO2 should be adapted to obtain a PaO2 of 8-10 kPa per 60-80 mm Hg (or oxygenation saturation ≥90%). This can be optimized by using closed-loop control systems.[68]
4. Optimal PEEP
PEEP should be incrementally added to optimize oxygenation and CO2–elimination and may reach a range of 14-16 cm H2O in patients with severe lung injury.[69] A meta-analysis of the treatment of patients with acute lung injury and ARDS (which includes a fraction of patients with multiple trauma) compared the outcomes after treatment with higher (11-15 cm H2O) vs. lower (8-9 cm H2O) PEEP levels and showed that higher levels of PEEP were associated with improved hospital survival only among the subgroup of patients with ARDS.[70] However, severe hypotension and a substantial reduction of cardiac output have to be avoided.
5. Permissive hypercapnia
Elevated PaCO2 levels can be tolerated, so long as the pH is greater than 7.2, except in patients with elevated intracranial pressures.
Ventilator modes
Unfortunately, there is a limited amount of scientific data that can be used to guide the practitioner in the selection of the best mode of ventilation. Despite the several ventilator modes introduced into the clinical routine, there is no evidence that the choice between a volume-controlled mode and a pressure-controlled mode influences the mortality or morbidity of patients.[71] PSV assists respiratory muscles during noninvasive and invasive ventilation and is patient-triggered and flow-cycled (see above). In the event of leakage (i.e., bronchopulmonal fistula), PSV with an adjustable termination flow should be used to prevent prolonged inspiration.
Airway pressure release ventilation (APRV) is a mode that can permit spontaneous breathing at any time throughout the respiratory cycle. Airway pressure is transiently released to a lower level to create a deep expiration and to support the patient effort during CPAP breathing. Hereby, the lower pressure level is extremely shorter than the time of the upper pressure level. APRV has been shown to improve oxygenation in trauma patients and therefore may be a good option.[72–74]
High-frequency oscillation ventilation (HFOV) is an additional option for mechanical ventilation and is typically used as a rescue mode of ventilation in patients with severe respiratory distress.[75] With HFOV, the lung achieves a higher mean airway pressure in comparison to conventional mechanical ventilation and very low tidal volumes (44-210 mL),[76] preventing cyclical lung de-recruitment and overdistension. The potential beneficial effects of HFOV still need elaboration and evaluation in the chest trauma population.[77]
Under the assumption that mechanical ventilation patterns that produce variable airway pressures and inspiratory times may be advantageous to maximize lung recruitment and stabilization,[78] a new mode of “noisy ventilation” with variable tidal volumes and fixed respiratory frequencies to improve respiratory function has been introduced. However, this mode has not been demonstrated in human patients.[79,80]
Gas exchange through an artificial lung
Extracorporeal membrane oxygenation (ECMO) or extracorporeal life support (ECLS) is beneficial in treating ALI and ARDS after trauma[81–84] and can improve the survival of trauma patients.[85] Extracorporeal oxygenation needs systemic anticoagulation and is therefore difficult to apply in patients with multiple trauma[86] and is only provided in specialized centers.
Independent lung ventilation
Chest trauma can lead to disproportionate or unilateral lung trauma. In such cases, the affected lung cannot be sufficiently ventilated without compromising the healthy lung with VALI. Conventional respiration methods may fail in such a condition of the lungs. Here independent lung ventilation should be considered to optimize the respiratory and hemodynamic situations. Non-synchronized independent ventilation can be used to provide the lungs with selective ventilator management, according to the different statuses of the affected and non-affected lungs.[87,88] In this way, after intubation with a double-lumen tube, two ventilators that are independently attached to the lungs can provide different ventilator modes, flows, pressure levels, rates, volumes and inspired oxygen. Independent lung ventilation provides the option of combining high-frequency jet ventilation to the affected side with protective lung ventilation to the non-affected side.[89–92]
The use of differential PEEP is another important factor for improving gas exchange in unilateral parenchymal lung injuries after trauma.[93–95] In bronchopleural fistula, the positive pressure (PEEP/ CPAP) and inflationary volume should be limited, and inverse-ratio inflationary holds should be avoided on the affected side. Further limitation in positive pressure can be achieved by reducing the rate of positive-pressure breaths with the affected lung. In very severe cases, the affected side may be left open to the atmosphere or connected to an oxygen-rich gas source, whereas the non-affected side is ventilated.[32,96]
CONCLUSIONS
Ventilation in patients after chest trauma is challenging because of the difficulty in achieving balance between sufficient ventilation and the avoidance of further harm to the lungs. Coexisting neurologic, osseous and vascular injuries may require more attention by the emergency physician than the pulmonary trauma itself. The goal of first-line clinical therapy for chest trauma patients is to achieve an adequate level of oxygenation and to protect the lungs from further injury using reduced tidal volumes (6 mL/kg pbw), a pressure limit below 30 cm H2O and a level of FiO2 as low as possible. The magnitude, location and type of lung or chest injury require a gradually adapted therapy tailored to individual patient's needs and which includes NIPPV or IPPV with i.e. APRV. Additionally, ECMO should be considered, as should independent, side-specific lung ventilation in combination with HFOV. Chest tube management, chest physiotherapy, extensive bronchial drainage, bronchial alveolar lavage sampling and other options, such as the use of bronchial blockers and the performance of a tracheostomy, should be incorporated into the management of ventilation in chest trauma patients.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Devitt JH, McLean RF, Koch JP. Anaesthetic management of acute blunt thoracic trauma. Can J Anaesth. 1991;38:506–10. doi: 10.1007/BF03007590. [DOI] [PubMed] [Google Scholar]
- 2.Pape HC, Remmers D, Rice J, Ebisch M, Krettek C, Tscherne H. Appraisal of early evaluation of blunt chest trauma: Development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Cohn SM. Pulmonary contusion: Review of the clinical entity. J Trauma. 1997;42:973–9. doi: 10.1097/00005373-199705000-00033. [DOI] [PubMed] [Google Scholar]
- 4.Szucs-Farkas Z, Kaelin I, Flach PM, Rosskopf A, Ruder TD, Triantafyllou M, et al. Detection of chest trauma with whole-body low-dose linear slit digital radiography: a multireader study. AJR Am J Roentgenol. 2010;194:W388–95. doi: 10.2214/AJR.09.3378. [DOI] [PubMed] [Google Scholar]
- 5.Wustner A, Gehmacher O, Hammerle S, Schenkenbach C, Hafele H, Mathis G. Ultrasound diagnosis in blunt thoracic trauma. Ultraschall Med. 2005;26:285–90. doi: 10.1055/s-2005-858524. [DOI] [PubMed] [Google Scholar]
- 6.Brooks A, Davies B, Smethhurst M, Connolly J. Emergency ultrasound in the acute assessment of haemothorax. Emerg Med J. 2004;21:44–6. doi: 10.1136/emj.2003.005438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohn SM, Zieg PM. Experimental pulmonary contusion: Review of the literature and description of a new porcine model. J Trauma. 1996;41:565–71. doi: 10.1097/00005373-199609000-00036. [DOI] [PubMed] [Google Scholar]
- 8.Aufmkolk M, Fischer R, Voggenreiter G, Kleinschmidt C, Schmit-Neuerburg KP, Obertacke U. Local effect of lung contusion on lung surfactant composition in multiple trauma patients. Crit Care Med. 1999;27:1441–6. doi: 10.1097/00003246-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Wanek S, Mayberry JC. Blunt thoracic trauma: Flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20:71–81. doi: 10.1016/s0749-0704(03)00098-8. [DOI] [PubMed] [Google Scholar]
- 10.Ullman EA, Donley LP, Brady WJ. Pulmonary trauma emergency department evaluation and management. Emerg Med Clin North Am. 2003;21:291–313. doi: 10.1016/s0733-8627(03)00016-6. [DOI] [PubMed] [Google Scholar]
- 11.Raghavendran K, Notter RH, Davidson BA, Helinski JD, Kunkel SL, Knight PR. Lung contusion: Inflammatory mechanisms and interaction with other injuries. Shock. 2009;32:122–30. doi: 10.1097/SHK.0b013e31819c385c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thibeault DW, Lachman RS, Laul VR, Kwong MS. Pulmonary interstitial emphysema, pneumomediastinum, and pneumothorax.Occurrence in the newborn infant. Am J Dis Child. 1973;126:611–4. doi: 10.1001/archpedi.1973.02110190493005. [DOI] [PubMed] [Google Scholar]
- 13.Al-Hassani A, Abdulrahman H, Afifi I, Almadani A, Al-Den A, Al-Kuwari A, et al. Rib fracture patterns predict thoracic chest wall and abdominal solid organ injury. Am Surg. 2010;76:888–91. [PubMed] [Google Scholar]
- 14.Duff JH, Goldstein M, McLean AP, Agrawal SN, Munro DD, Gutelius JR. Flail chest: A clinical review and physiological study. J Trauma. 1968;8:63–74. [PubMed] [Google Scholar]
- 15.Mackersie RC, Shackford SR, Hoyt DB, Karagianes TG. Continuous epidural fentanyl analgesia: Ventilatory function improvement with routine use in treatment of blunt chest injury. J Trauma. 1987;27:1207–12. [PubMed] [Google Scholar]
- 16.Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136:426–30. doi: 10.1016/j.surg.2004.05.019. [DOI] [PubMed] [Google Scholar]
- 17.Abolhoda A, Livingston DH, Donahoo JS, Allen K. Diagnostic and therapeutic video assisted thoracic surgery (VATS) following chest trauma. Eur J Cardiothorac Surg. 1997;12:356–60. doi: 10.1016/s1010-7940(97)00192-9. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–32. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Pettiford BL, Luketich JD, Landreneau RJ. The management of flail chest. Thorac Surg Clin. 2007;17:25–33. doi: 10.1016/j.thorsurg.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Ball CG, Kirkpatrick AW, Laupland KB, Fox DI, Nicolaou S, Anderson IB, et al. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59:917–24. doi: 10.1097/01.ta.0000174663.46453.86. [DOI] [PubMed] [Google Scholar]
- 21.Bokhari F, Brakenridge S, Nagy K, Roberts R, Smith R, Joseph K, et al. Prospective evaluation of the sensitivity of physical examination in chest trauma. J Trauma. 2002;53:1135–8. doi: 10.1097/00005373-200212000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Ho ML, Gutierrez FR. Chest radiography in thoracic polytrauma. AJR Am J Roentgenol. 2009;192:599–612. doi: 10.2214/AJR.07.3324. [DOI] [PubMed] [Google Scholar]
- 23.Dulchavsky SA, Hamilton DR, Diebel LN, Sargsyan AE, Billica RD, Williams DR. Thoracic ultrasound diagnosis of pneumothorax. J Trauma. 1999;47:970–1. doi: 10.1097/00005373-199911000-00029. [DOI] [PubMed] [Google Scholar]
- 24.Barrios C, Tran T, Malinoski D, Lekawa M, Dolich M, Lush S, et al. Successful management of occult pneumothorax without tube thoracostomy despite positive pressure ventilation. Am Surg. 2008;74:958–61. [PubMed] [Google Scholar]
- 25.Fitzgerald M, Mackenzie CF, Marasco S, Hoyle R, Kossmann T. Pleural decompression and drainage during trauma reception and resuscitation. Injury. 2008;39:9–20. doi: 10.1016/j.injury.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 26.Powner DJ, Cline CD, Rodman GH., Jr Effect of chest-tube suction on gas flow through a bronchopleural fistula. Crit Care Med. 1985;13:99–101. doi: 10.1097/00003246-198502000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Baumann MH, Patel PB, Roney CW, Petrini MF. Comparison of function of commercially available pleural drainage units and catheters. Chest. 2003;123:1878–86. doi: 10.1378/chest.123.6.1878. [DOI] [PubMed] [Google Scholar]
- 28.Gallagher TJ, Smith RA, Kirby RR, Civetta JM. Intermittent inspiratory chest tube occlusion to limit bronchopleural cutaneous airleaks. Crit Care Med. 1976;4:328–32. doi: 10.1097/00003246-197611000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Blanch PB, Koens JC, Jr, Layon AJ. A new device that allows synchronous intermittent inspiratory chest tube occlusion with any mechanical ventilator. Chest. 1990;97:1426–30. doi: 10.1378/chest.97.6.1426. [DOI] [PubMed] [Google Scholar]
- 30.Downs JB, Chapman RL., Jr Treatment of bronchopleural fistula during continuous positive pressure ventilation. Chest. 1976;69:363–6. doi: 10.1378/chest.69.3.363. [DOI] [PubMed] [Google Scholar]
- 31.Phillips YY, Lonigan RM, Joyner LR. A simple technique for managing a bronchopleural fistula while maintaining positive pressure ventilation. Crit Care Med. 1979;7:351–3. doi: 10.1097/00003246-197908000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Taylor RW, Dellinger RP. Special Problems in Mechanical Ventilation. In: Marini JJ, Slutsky AS, editors. Physiological Basis of Ventilatory Support. New York: Marcel Dekker; 1998. pp. 1247–61. [Google Scholar]
- 33.Castelli I, Schlapfer R, Stulz P. Thoracic trauma. Anaesthesist. 1995;44:513–30. doi: 10.1007/s001010050184. [DOI] [PubMed] [Google Scholar]
- 34.Klein U, Laubinger R, Malich A, Hapich A, Gunkel W. Emergency treatment of thoracic trauma. Anaesthesist. 2006;55:1172–88. doi: 10.1007/s00101-006-1092-6. [DOI] [PubMed] [Google Scholar]
- 35.Balci AE, Eren N, Eren S, Ulkü R. Surgical treatment of post-traumatic tracheobronchial injuries: 14-year experience. Eur J Cardiothorac Surg. 2002;22:984–9. doi: 10.1016/s1010-7940(02)00591-2. [DOI] [PubMed] [Google Scholar]
- 36.Cassada DC, Munyikwa MP, Moniz MP, Dieter RA, Jr, Schuchmann GF, Enderson BL. Acute injuries of the trachea and major bronchi: Importance of early diagnosis. Ann Thorac Surg. 2000;69:1563–7. doi: 10.1016/s0003-4975(00)01077-8. [DOI] [PubMed] [Google Scholar]
- 37.Kiser AC, O’Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: Treatment and outcomes. Ann Thorac Surg. 2001;71:2059–65. doi: 10.1016/s0003-4975(00)02453-x. [DOI] [PubMed] [Google Scholar]
- 38.Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways from blunt trauma: Treatment of complex injuries. Ann Thorac Surg. 1992;54:177–83. doi: 10.1016/0003-4975(92)91177-b. [DOI] [PubMed] [Google Scholar]
- 39.Benumof JL, Partridge BL, Salvatierra C, Keating J. Margin of safety in positioning modern double-lumen endotracheal tubes. Anesthesiology. 1987;67:729–38. doi: 10.1097/00000542-198711000-00018. [DOI] [PubMed] [Google Scholar]
- 40.al Jishi N, Dyer D, Sharief N, al-Alaiyan S. Selective bronchial occlusion for treatment of bullous interstitial emphysema and bronchopleural fistula. J Pediatr Surg. 1994;29:1545–7. doi: 10.1016/0022-3468(94)90211-9. [DOI] [PubMed] [Google Scholar]
- 41.Sprung J, Krasna MJ, Yun A, Thomas P, Bourke DL. Treatment of a bronchopleural fistula with a Fogarty catheter and oxidized regenerated cellulose (surgicel) Chest. 1994;105:1879–81. doi: 10.1378/chest.105.6.1879. [DOI] [PubMed] [Google Scholar]
- 42.Raghavendran K, Davidson BA, Helinski JD, Marschke CJ, Manderscheid P, Woytash JA, et al. A rat model for isolated bilateral lung contusion from blunt chest trauma. Anesth Analg. 2005;101:1482–9. doi: 10.1213/01.ANE.0000180201.25746.1F. [DOI] [PubMed] [Google Scholar]
- 43.Rashid MA, Wikström T, Ortenwall P. Outcome of lung trauma. Eur J Surg. 2000;166:22–8. doi: 10.1080/110241500750009654. [DOI] [PubMed] [Google Scholar]
- 44.O’Connor JV, Kufera JA, Kerns TJ, Stein DM, Ho S, Dischinger PC, et al. Crash and occupant predictors of pulmonary contusion. J Trauma. 2009;66:1091–5. doi: 10.1097/TA.0b013e318164d097. [DOI] [PubMed] [Google Scholar]
- 45.Mizushima Y, Hiraide A, Shimazu T, Yoshioka T, Sugimoto H. Changes in contused lung volume and oxygenation in patients with pulmonary parenchymal injury after blunt chest trauma. Am J Emerg Med. 2000;18:385–9. doi: 10.1053/ajem.2000.7317. [DOI] [PubMed] [Google Scholar]
- 46.Omert L, Yeaney WW, Protetch J. Efficacy of thoracic computerized tomography in blunt chest trauma. Am Surg. 2001;67:660–4. [PubMed] [Google Scholar]
- 47.Keel M, Meier C. Chest injuries - what is new? Curr Opin Crit Care. 2007;13:674–9. doi: 10.1097/MCC.0b013e3282f1fe71. [DOI] [PubMed] [Google Scholar]
- 48.Anderson CA, Palmer CA, Ney AL, Becker B, Schaffel SD, Quickel RR. Evaluation of the safety of high-frequency chest wall oscillation (HFCWO) therapy in blunt thoracic trauma patients. J Trauma Manag Outcomes. 2008;2:8. doi: 10.1186/1752-2897-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cain JG, Tesfaye Y. Pulmonary trauma. Curr Opin Anaesthesiol. 2001;14:245–9. doi: 10.1097/00001503-200104000-00019. [DOI] [PubMed] [Google Scholar]
- 50.Rao PM, Puri GD, Bharadwaj N, Chari P, Acup D. ICU management of blunt chest trauma: Our experience. Ann Card Anaesth. 1998;1:31–5. [PubMed] [Google Scholar]
- 51.Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A. Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med. 2005;31:922–6. doi: 10.1007/s00134-005-2625-1. [DOI] [PubMed] [Google Scholar]
- 52.Slutsky AS. Ventilator-induced lung injury: From barotrauma to biotrauma. Respir Care. 2005;50:646–59. [PubMed] [Google Scholar]
- 53.Hoyt DB, Simons RK, Winchell RJ, Cushman J, Hollingsworth-Fridlund P, Holbrook T, et al. A risk analysis of pulmonary complications following major trauma. J Trauma. 1993;35:524–31. doi: 10.1097/00005373-199310000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Garber BG, Hebert PC, Yelle JD, Hodder RV, McGowan J. Adult respiratory distress syndrome: A systemic overview of incidence and risk factors. Crit Care Med. 1996;24:687–95. doi: 10.1097/00003246-199604000-00023. [DOI] [PubMed] [Google Scholar]
- 55.Ragaller M, Richter T. Acute lung injury and acute respiratory distress syndrome. J Emerg Trauma Shock. 3:43–51. doi: 10.4103/0974-2700.58663. 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ndiaye A, Chambost M, Chiron M. The fatal injuries of car drivers. Forensic Sci Int. 2009;184:21–7. doi: 10.1016/j.forsciint.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 57.Antonelli M, Conti G, Rocco M, Bufi M, De Blasi RA, Vivino G, et al. A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med. 1998;339:429–35. doi: 10.1056/NEJM199808133390703. [DOI] [PubMed] [Google Scholar]
- 58.Beltrame F, Lucangelo U, Gregori D, Gregoretti C. Noninvasive positive pressure ventilation in trauma patients with acute respiratory failure. Monaldi Arch Chest Dis. 1999;54:109–14. [PubMed] [Google Scholar]
- 59.Hernandez G, Fernandez R, Lopez-Reina P, Cuena R, Pedrosa A, Ortiz R, et al. Noninvasive ventilation reduces intubation in chest trauma-related hypoxemia: A randomized clinical trial. Chest. 2010;137:74–80. doi: 10.1378/chest.09-1114. [DOI] [PubMed] [Google Scholar]
- 60.Smith CE, Dejoy SJ. New equipment and techniques for airway management in trauma. Curr Opin Anaesthesiol. 2001;14:197–209. doi: 10.1097/00001503-200104000-00012. [DOI] [PubMed] [Google Scholar]
- 61.Abernathy JH, 3rd, Reeves ST. Airway catastrophes. Curr Opin Anaesthesiol. 2010;23:41–6. doi: 10.1097/ACO.0b013e328333b768. [DOI] [PubMed] [Google Scholar]
- 62.Jaber S, Chanques G, Jung B. Postoperative noninvasive ventilation. Anesthesiology. 2010;112:453–61. doi: 10.1097/ALN.0b013e3181c5e5f2. [DOI] [PubMed] [Google Scholar]
- 63.Schreiter D, Reske A, Stichert B, Seiwerts M, Bohm SH, Kloeppel R, et al. Alveolar recruitment in combination with sufficient positive end-expiratory pressure increases oxygenation and lung aeration in patients with severe chest trauma. Crit Care Med. 2004;32:968–75. doi: 10.1097/01.ccm.0000120050.85798.38. [DOI] [PubMed] [Google Scholar]
- 64.Shafi S, Gentilello L. Pre-hospital endotracheal intubation and positive pressure ventilation is associated with hypotension and decreased survival in hypovolemic trauma patients: An analysis of the National Trauma Data Bank. J Trauma. 2005;59:1140–5. doi: 10.1097/01.ta.0000196434.88182.77. [DOI] [PubMed] [Google Scholar]
- 65.Terragni PP, Rosboch G, Tealdi A, Corno E, Menaldo E, Davini O, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175:160–6. doi: 10.1164/rccm.200607-915OC. [DOI] [PubMed] [Google Scholar]
- 66.Meier J, Kemming GI, Kisch-Wedel H, Blum J, Pape A, Habler OP. Hyperoxic ventilation reduces six-hour mortality after partial fluid resuscitation from hemorrhagic shock. Shock. 2004;22:240–7. doi: 10.1097/01.shk.0000131192.02909.4c. [DOI] [PubMed] [Google Scholar]
- 67.Reinert M, Barth A, Rothen HU, Schaller B, Takala J, Seiler RW. Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen, lactate and glucose in patients with severe head injury. Acta Neurochir (Wien) 2003;145:341–9. doi: 10.1007/s00701-003-0027-0. [DOI] [PubMed] [Google Scholar]
- 68.Johannigman JA, Branson R, Lecroy D, Beck G. Autonomous control of inspired oxygen concentration during mechanical ventilation of the critically injured trauma patient. J Trauma. 2009;66:386–92. doi: 10.1097/TA.0b013e318197a4bb. [DOI] [PubMed] [Google Scholar]
- 69.Papadakos PJ, Karcz M, Lachmann B. Mechanical ventilation in trauma. Curr Opin Anaesthesiol. 2010;23:228–32. doi: 10.1097/ACO.0b013e328336ea6e. [DOI] [PubMed] [Google Scholar]
- 70.Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–73. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 71.Esteban A, Alía I, Gordo F, de Pablo R, Suarez J, González G, et al. Prospective randomized trial comparing pressure-controlled ventilation and volume-controlled ventilation in ARDS. For the Spanish Lung Failure Collaborative Group. Chest. 2000;117:1690–6. doi: 10.1378/chest.117.6.1690. [DOI] [PubMed] [Google Scholar]
- 72.Sydow M, Burchardi H, Ephraim E, Zielmann S, Crozier TA. Long-term effects of two different ventilatory modes on oxygenation in acute lung injury.Comparison of airway pressure release ventilation and volume-controlled inverse ratio ventilation. Am J Respir Crit Care Med. 1994;149:1550–6. doi: 10.1164/ajrccm.149.6.8004312. [DOI] [PubMed] [Google Scholar]
- 73.Davis K, Jr, Johnson DJ, Branson RD, Campbell RS, Johannigman JA, Porembka D. Airway pressure release ventilation. Arch Surg. 1993;128:1348–52. doi: 10.1001/archsurg.1993.01420240056010. [DOI] [PubMed] [Google Scholar]
- 74.Dart BW, 4th, Maxwell RA, Richart CM, Brooks DK, Ciraulo DL, Barker DE, et al. Preliminary experience with airway pressure release ventilation in a trauma/surgical intensive care unit. J Trauma. 2005;59:71–6. doi: 10.1097/00005373-200507000-00010. [DOI] [PubMed] [Google Scholar]
- 75.Chan KP, Stewart TE, Mehta S. High-frequency oscillatory ventilation for adult patients with ARDS. Chest. 2007;131:1907–16. doi: 10.1378/chest.06-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hager DN, Fessler HE, Kaczka DW, Shanholtz CB, Fuld MK, Simon BA, et al. Tidal volume delivery during high-frequency oscillatory ventilation in adults with acute respiratory distress syndrome. Crit Care Med. 2007;35:1522–9. doi: 10.1097/01.CCM.0000266586.04676.55. [DOI] [PubMed] [Google Scholar]
- 77.Siau C, Stewart TE. Current role of high frequency oscillatory ventilation and airway pressure release ventilation in acute lung injury and acute respiratory distress syndrome. (vi).Clin Chest Med. 2008;29:265–75. doi: 10.1016/j.ccm.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 78.Pelosi P, Gama de Abreu M, Rocco PR. New and conventional strategies for lung recruitment in acute respiratory distress syndrome. Crit Care. 2010;14:210. doi: 10.1186/cc8851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Spieth PM, Carvalho AR, Güldner A, Pelosi P, Kirichuk O, Koch T, et al. Effects of different levels of pressure support variability in experimental lung injury. Anesthesiology. 2009;110:342–50. doi: 10.1097/ALN.0b013e318194d06e. [DOI] [PubMed] [Google Scholar]
- 80.Spieth PM, Carvalho AR, Pelosi P, Hoehn C, Meissner C, Kasper M, et al. Variable tidal volumes improve lung protective ventilation strategies in experimental lung injury. Am J Respir Crit Care Med. 2009;179:684–93. doi: 10.1164/rccm.200806-975OC. [DOI] [PubMed] [Google Scholar]
- 81.Anderson HL, 3rd, Shapiro MB, Delius RE, Steimle CN, Chapman RA, Bartlett RH. Extracorporeal life support for respiratory failure after multiple trauma. J Trauma. 1994;37:266–72. doi: 10.1097/00005373-199408000-00020. [DOI] [PubMed] [Google Scholar]
- 82.Voelckel W, Wenzel V, Rieger M, Antretter H, Padosch S, Schobersberger W. Temporary extracorporeal membrane oxygenation in the treatment of acute traumatic lung injury. Can J Anaesth. 1998;45:1097–102. doi: 10.1007/BF03012399. [DOI] [PubMed] [Google Scholar]
- 83.Senunas LE, Goulet JA, Greenfield ML, Bartlett RH. Extracorporeal life support for patients with significant orthopaedic trauma. Clin Orthop Relat Res. 1997;339:32–40. doi: 10.1097/00003086-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 84.Cordell-Smith JA, Roberts N, Peek GJ, Firmin RK. Traumatic lung injury treated by extracorporeal membrane oxygenation (ECMO) Injury. 2006;37:29–32. doi: 10.1016/j.injury.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 85.Michaels AJ, Schriener RJ, Kolla S, Awad SS, Rich PB, Reickert C, et al. Extracorporeal life support in pulmonary failure after trauma. J Trauma. 1999;46:638–45. doi: 10.1097/00005373-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 86.Marasco SF, Preovolos A, Lim K, Salamonsen RF. Thoracotomy in adults while on ECMO is associated with uncontrollable bleeding. Perfusion. 2007;22:23–6. doi: 10.1177/0267659106074789. [DOI] [PubMed] [Google Scholar]
- 87.Katsaragakis S, Stamou KM, Androulakis G. Independent lung ventilation for asymmetrical chest trauma: effect on ventilatory and haemodynamic parameters. Injury. 2005;36:501–4. doi: 10.1016/j.injury.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 88.Anantham D, Jagadesan R, Tiew PE. Clinical review: Independent lung ventilation in critical care. Crit Care. 2005;9:594–600. doi: 10.1186/cc3827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Terragni P, Rosboch GL, Corno E, Menaldo E, Tealdi A, Borasio P, et al. Independent high-frequency oscillatory ventilation in the management of asymmetric acute lung injury. Anesth Analg. 2005;100:1793–6. doi: 10.1213/01.ANE.0000151161.36330.CF. [DOI] [PubMed] [Google Scholar]
- 90.Miranda DR, Stoutenbeek C, Kingma L. Differential lung ventilation with HFPPV. Intensive Care Med. 1981;7:139–41. doi: 10.1007/BF01738617. [DOI] [PubMed] [Google Scholar]
- 91.Feeley TW, Keating D, Nishimura T. Independent lung ventilation using high-frequency ventilation in the management of a bronchopleural fistula. Anesthesiology. 1988;69:420–2. doi: 10.1097/00000542-198809000-00025. [DOI] [PubMed] [Google Scholar]
- 92.Rico FR, Cheng JD, Gestring ML, Piotrowski ES. Mechanical ventilation strategies in massive chest trauma. (xi).Crit Care Clin. 2007;23:299–315. doi: 10.1016/j.ccc.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 93.Zandstra DF, Stoutenbeek CP. Reflection of differential pulmonary perfusion in polytrauma patients on differential lung ventilation (DLV). A comparison of two CO2-derived methods. Intensive Care Med. 1989;15:151–4. doi: 10.1007/BF01058565. [DOI] [PubMed] [Google Scholar]
- 94.Lev A, Barzilay E, Geber D, Bishara H, Prego J. Differential lung ventilation: A review and 2 case reports. Resuscitation. 1987;15:77–86. doi: 10.1016/0300-9572(87)90019-0. [DOI] [PubMed] [Google Scholar]
- 95.Siegel JH, Stoklosa JC, Borg U, Wiles CE, 3rd, Sganga G, Geisler FH, et al. Quantification of asymmetric lung pathophysiology as a guide to the use of simultaneous independent lung ventilation in posttraumatic and septic adult respiratory distress syndrome. Ann Surg. 1985;202:425–39. doi: 10.1097/00000658-198510000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bonnet R, Wilms D. Long-term use of asynchronous independent lung ventilation: Effects on gas exchange and hemodynamics. Pneumologie. 1990;44:665–7. [PubMed] [Google Scholar]


