Abstract
Given the increasing number of operational nuclear reactors worldwide, combined with the continued use of radioactive materials in both healthcare and industry, the unlikely occurrence of a civilian nuclear incident poses a small but real danger. This article provides an overview of the most important historical, medical, and scientific aspects associated with the most notable nuclear incidents to date. We have discussed fundamental principles of radiation monitoring, triage considerations, and the short- and long-term management of radiation exposure victims. The provision and maintenance of adequate radiation safety among first responders and emergency personnel are emphasized. Finally, an outline is included of decontamination, therapeutic, and prophylactic considerations pertaining to exposure to various radioactive materials.
Keywords: Civilian nuclear incident, radiation monitoring, radiation syndromes, radioactive exposure
INTRODUCTION
As of January 2011, there were 442 operational nuclear reactors in the world, with an additional 65 reactors being under construction.[1] Although the nuclear industry maintains very high safety standards, the potential for an unintentional reactor malfunction and release of radioactive materials into the environment represents a significant danger. In addition, there are significant risks associated with the medical use of radioactive materials, as well as storage and transport of spent nuclear fuels.[2,3] Major incidents involving the civilian use of nuclear power were few, and most of them were self-limited.
The potential for major nuclear disaster is real, and it is essential that contingency plans are ready in the case of a major civilian nuclear mishap, whether due to human factors or out of our control. Exemplified by the recent nuclear incident at the Fukushima Daiichi nuclear plant in Japan, some factors beyond ordinary human control (i.e., large natural disasters) may lead to significant radiation releases and potentially hazardous radioactive contamination. This article will summarize both the history of notable civilian nuclear incidents (CNIs) and the cumulative knowledge pertaining to the medical management of victims of radiation exposure.
SCIENTIFIC DEFINITIONS AND PRINCIPLES
Ionizing radiation is also referred to simply as radiation, and entails particle or wave energy forceful enough to alter atomic behavior and/or stability.[4] Radiation is emitted when unstable radioactive atoms try to become stable by the emission of high-energy waves (gamma waves) or particles (alpha and beta), in a process known as radioactive decay. These unstable atoms are also known as radionuclides or radioisotopes. Particle and wave release generally occurs from two sources: (a) radionuclides present from the inception of our planet (radium, thorium, and uranium) and (b) man-made sources such as nuclear reactors or nuclear weapons.[4] Different types of ionizing radiation are characterized by varied levels of penetration [Figure 1].
Figure 1.
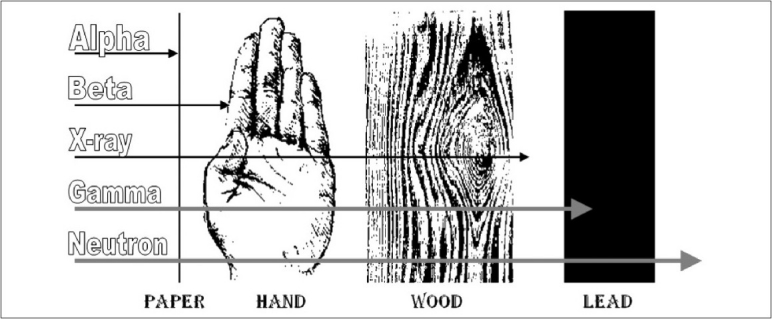
Different types of ionizing radiation can be characterized by their depth of penetration. Alpha and beta particles have the lowest penetration, while neutrons and gamma rays are capable of penetrating materials up to and including lead. The machine-generated x-rays, physically identical to gamma rays and thus not included in our discussion, have been added for illustrative purposes. [Modified from Canadian Nuclear Safety Commission Website. Available at: http://nuclearsafety.gc.ca/eng/readingroom/publications/gauges/index.cfm]
Alpha particles have two protons and two neutrons that are released from an atomic nucleus. An alpha particle is similar to a helium atom nucleus. Radium, polonium, uranium, radon, and thorium emit alpha particles. They are heavy (high mass) particles and contain high energy that is typically released over short distances (usually about 1 inch).[5] Thus, they cannot penetrate skin, but can be very harmful if consumed or inhaled, or if they enter the hematologic system.[4,5]
Beta particles are also very energetic and are emitted from the nucleus. They are smaller than alpha particles, less charged, slower, and interact with a lower intensity than alpha particles. These particles are emitted by tritium, carbon-4, strontium, phosphorus-32, phosphorus-33, and sulfur-35. They travel large distances, but are easily stopped by materials such as clothing and aluminum. They are capable of penetrating skin thereby causing cutaneous burns. They too are harmful if swallowed or inhaled.[4,5]
Gamma rays are photons and travel like light. They lose energy slowly. Therefore, they can travel hundreds of feet. They have no mass, nor do they have a charge, and they penetrate the body tissues very easily.[4,5] They interact less energetically/intensely with matter than alpha or beta particles. Very dense materials are needed to protect living organisms from their effects, such as concrete (feet) or a lead (inches). Man-made sources of gamma rays include cobalt-60, zinc-65, radium-226, and cesium-137. Potassium-40 is a naturally occurring gamma source.
Neutrons are uncharged particles emitted from nuclei of certain elements. Neutrons, much like x-rays, can be artificially produced. A collision between a neutron and an atom results in the atom absorbing a portion of the neutron's energy. Once the neutron has given off most of its energy, it can be “captured” by an atom and the newly formed atom may give off a high energy gamma ray.
Units of radiation are grouped into those of measurement or absorption. Radioactivity can be measured in Becquerel (Bq)/s or Curie (Ci). One Becquerel signifies one disintegration event per second (1 Ci = 3.7 × 1010 Bq or disintegrations/s). The absorbed radiation is measured in Gray (Gy) or rad, while the effective dose is measured in rem, and Sievert (Sv). It should be noted that Bq, Gy, and Sv are SI units (International System of Units), and Ci, rad, and rem are non-SI units.
Radiation-related injury occurs because of the deposition of energy in tissues.[6] The energy deposited by ionizing radiation is called the absorbed dose (also known as the total ionizing dose or TID). It equals the energy deposited per unit mass of medium, which may be measured as Joules/kg (J/kg) and represented by the SI unit, Gy, or the US customary unit, rad [Table 1].[7]
Table 1.
Measuring radioactivity - Units, symbols, and conversions
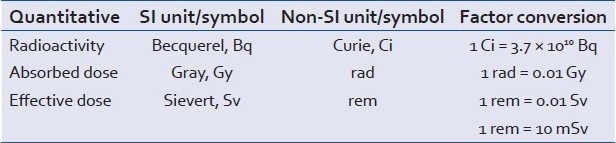
The effective dose takes into consideration the fact that radiation does not affect all body parts/tissues equally. The effective dose (E) to an individual is estimated by calculating a weighted average of the equivalent dose (H) to different body tissues, with the weighting factors (W) designed to reflect the different radiosensitivities of the tissues: E = ΣiHiWi.[8] The unit for an effective dose is Sv, or rem. It is measured in J/kg.
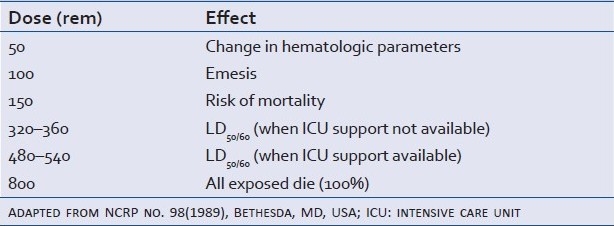
The sensitivity of tissue to radiation is proportional to the proliferation rate of the cells within exposed tissue(s) and will vary inversely with the differentiation of the cells in question.[9] The most sensitive to least sensitive systems are hematologic and reproductive system, skin, teeth and bone, and finally, the nervous system. Immediate effects include radiation sickness and burns, with cancer and cataracts among delayed effects.[9] Acute effects occur with uniform exposure of the entire body while the same delivered dose to an extremity may only cause a local effect. The LD50/60 is the dose at which 50% of the exposed subjects will die within 60 days. Table 2 demonstrates dose-and-effect relationships of radiation exposure.
Table 2.
Dose and effect relationships of radiation exposure
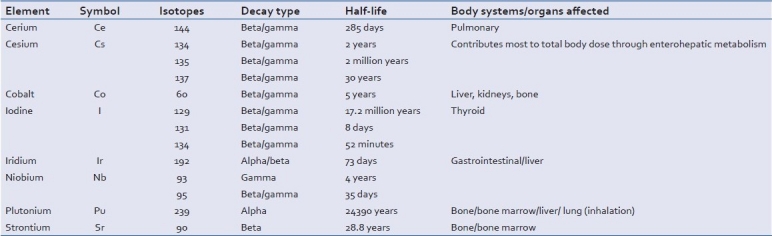
The food chain can also be involved in the spread of the radiation risk. For example, in the current Fukushima Daiichi plant disaster, radioactive particles had become bound to dust and traveled through the atmosphere before setting down.[10] Contamination occurred merely from having the particles fall into the water or on to crops. Any particles, for example, that fall onto a pasture may be eaten by dairy cattle and get into the milk supply. Also, large leafy vegetables may accumulate more radioactive particles than those with smaller leaves. Research has demonstrated that insects and predators can also move radioactive particles into the environment through food chain,[11] and that cesium-137 has been identified as a contaminant in US fish supplies.[12] Agricultural counter measures have been taken in the past to reduce the radioactive contamination of farm animals and farm animal products and may again be needed to be considered in the future.[13] Unfortunately, there is no reliable literature on the intake of contaminated foods and its long- or short-term effects on humans. A list of selected radioactive elements commonly involved in nuclear incidents, along with associated radiation type(s) and effects on the human body, can be seen in Table 3.
Table 3.
Selected radioactive elements commonly involved in nuclear incidents, along with associated radiation type(s) and effects on the human body
NUCLEAR INCIDENT CATEGORIES
Nuclear-based weapons
Although an “all-out” global nuclear conflagration is unlikely, the isolated use of nuclear-based weapons (NBWs) by terrorist organizations continues to be a threat.[14,15] Radioactive materials have been recovered from various illegal market sources which, combined with inadequate monitoring and control systems, raise a concern that some of the illegal transactions may have gone undetected.[14] A nuclear detonation carried out by the terrorists represents the most extreme scenario. In addition to the tremendous damage to the physical infrastructure, a large number of casualties could be expected as radiation exposures of greater than 3.5 Gy are lethal within 30 days in the absence of prompt and aggressive medical treatment.[16] Other possible scenarios of NBW use include the dispersal of radioactive substances with or without the use of explosives, as well as direct attacks on nuclear reactors.[15]
Civilian nuclear incidents
These occurrences are characterized by unintentional releases or exposures of radioactive materials to the surrounding environment, usually involving some form of mechanical or systems failure or lack of oversight. Here, specific patterns of radioactive exposure can vary depending on the nature of the event and the type of nuclear material involved. Inciting causes may involve a combination of multiple factors. For example, human factors were heavily involved in the Chernobyl incident while natural factors that are out of human control were primarily involved in the Fukushima Daiichi nuclear incident.[17]
NOTABLE CIVILIAN NUCLEAR INCIDENTS
Sources of data on radiation injury can be divided into four major categories: nuclear bomb denotations, civilian industrial incidents, therapeutic radiation, and animal models.[18] Despite almost 70 years of research on this subject, there are many gaps in the available body of information. Most of the data on the nuclear bomb detonation have come from the experience with the Hiroshima and Nagasaki explosions in 1945. What follows is a detailed discussion of most notable civilian industrial incidents that have resulted in radiation-related injury, including acute radiation sickness and associated radiation injury syndromes. The knowledge and understanding of nuclear incidents that occurred in the past may assist clinicians in the prompt recognition of various radiation injury signs and symptoms and, in doing so, quickly and appropriately triage the injured to medical facilities best equipped to handle victims of radiation exposure.
Perhaps the greatest challenge in summarizing the CNIs stems from the fact the there were no unified and/or standardized procedures utilized by the involved countries to document or report the events. Likewise, there was no unified approach in the medical treatment of the injured. Thus, it is difficult to assess the efficacy of commonly utilized treatments. Accurate medical and scientific accounts are scarce. Between 1944 and 2003, there were 426 radiation incidents worldwide affecting well in excess of 130,000 people.[19] Most of the reported experience with radiation injury and its sequelae, however, comes from the Chernobyl accident in 1986. All other major incidents led to only a few injured civilians. It is also difficult to extrapolate the statistics on the injured to the rest of the population due to demographics of the population in question (i.e., mainly young healthy men).[18]
Out of the seven major incidents involving large exposures to nuclear materials, two warrant a more detailed discussion in the context of this review – the Chernobyl (Soviet Union, 1986) incident and the Goiania (Brazil, 1987) incident.[20] Both occurrences affected large populations and covered large geographic areas. Incidents involving nuclear power plants in the United States, including the Three Mile Island (TMI) power plant, although very serious, fortunately did not result in significant contamination of the surrounding areas.[21] Some are predicting that the Fukushima Daiichi nuclear incident may ultimately be more devastating than the Chernobyl incident, but at the time of writing this article, details were limited.[22,23]
The Chernobyl incident
The Chernobyl power plant is located in the northeastern part of Ukraine (former Soviet Union) near the border with Belarus. On the evening of April 25, 1986, engineers at the power plant were performing an electrical test of reactor 4. After the failure of recognition of an imminent system failure, resultant explosion blew off the heavy steel and concrete lid of the reactor on April 26. This explosion, driven by the ignition of gases and steam, resulted in >50 tons of radioactive materials to be released into the atmosphere.[24] Only the station staff and the rescue services (mainly firemen) received radiation doses that endangered life. The fire ended on May 6th. During this period, a substantial atmospheric release of radioactive contaminants occurred. Largest releases took place on April 26, May 4, and May 5.[20] The meteorological situation at the time of the accident resulted in the radioactive plume moving northward toward the town of Pripyat and further toward Belarus and Northern Europe. This spared the highly populated cities immediately to the south including Kiev (3 million residents).
Several groups were affected by the accident. First were emergency workers, who can be further divided into two groups: (a) approximately 600 persons involved in the emergency response during the first day of the accident, and (b) hundreds of thousands of people who, from 1986 to 1989, were sent into the power station or the surrounding zone for decontamination work, concrete and steel “sarcophagus” construction around the destroyed reactor, as well as other clean-up operations. Second were members of the general public, which included around 100,000 people living within the 30-km vicinity of the power plant (later declared inhabitable), and >5 million people living in the south, many of whom (especially children) were evacuated during the summer following the incident.[25]
At the time of the accident, the plant personnel and the auxiliary staff experienced acute radiation effects from several sources: (a) short-term external gamma and beta radiation from the gas emission cloud; (b) short-term gamma and beta radiation from fragments of the damaged reactor core that were scattered throughout the power plant; (c) inhalation gases and aerosols containing a mixture of radionuclides; and (d) deposition of radioactive particles on the skin/clothing and further external/internal contamination.[26]
Radiation doses received by the population within the 30-km radius around Chernobyl have been estimated to be at around 1.5–5 cGy to the whole body, 10–20 cGy to the skin, and 1.5–20 cGy to the thyroid.[24,25] This population was evacuated by May 6 completely. Of the 303 victims at the site of the accident who had been initially hospitalized, 30 died from burns and consequences of acute radiation sickness.[24] A thousand more were affected by thyroid and bone marrow cancers.[25]
Major radionuclide contaminants in the Chernobyl incident included isotopes of iodine (131 and 132), cesium (134 and 137), niobium-95, cerium-144, ruthenium (103 and106), and plutonium-239.[24] More than 90% of the fallout was in the form of radioactive iodine and cesium, which helps explain bone marrow and thyroid malignancies among those who developed cancer.
The Goiania incident
The accident in Goiania, Brazil, began on September 13, 1987, when a radiotherapy device was taken from a closed clinic in Goiania (population approximately 1 million) and sold as scrap to a junk dealer. The source consisted of a sealed radioactive cesium-137 isotope in the form of a highly soluble chloride salt. The capsule was opened; the 100-g mass of the luminescent material was very attractive, especially to children who considered it to be a “magical material” and began to play with it. This resulted in a significant dispersion of cesium-137 on clothing, paper, walls, and floors, and also led to internal exposure in many individuals. The accident was undetected for 16 days and came to light during September 28–29 when people began to show signs of radiation sickness. Two hundred and forty nine patients were contaminated in total. Twenty of them were eventually hospitalized, with four fatalities.[20,27] The impact on local agriculture was also significant (>40% decrease in local food sales).
Other civilian incidents
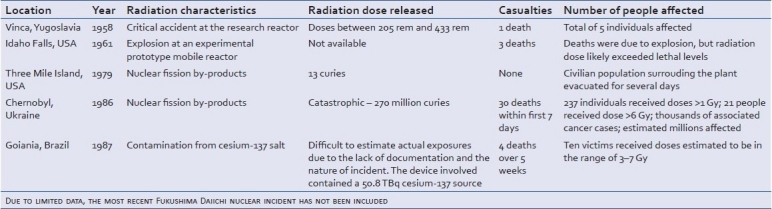
The TMI incident in 1979 in Pennsylvania, one of the most notable nuclear mishaps in the US history, was minor by comparison to the Chernobyl power plant explosion. The amount of radiation released at TMI was 13 curies as compared to 270 million curies released in Chernobyl.[21] The most notable civilian nuclear accidents are summarized in Table 4.[28–31]
Table 4.
Summary of most significant civilian nuclear incidents
Most recently, the nuclear incident in Fukishima, Japan, prompted a discussion regarding nuclear power safety.[17] After the 9.0 magnitude earthquake and the ensuing tsunami wave on the coast of Japan on March 11, 2011, partial core meltdowns occurred at the reactors of the Fukushima nuclear plant.[32] The total amount of radioactive contamination is still unknown, but is likely to increase. While it is too early to properly examine the medical aspects of this nuclear incident, there continues to be a significant potential for adverse medical and socioeconomic consequences of this combined natural and man-made disaster, the extent of which remains to be fully determined.
RADIATION MONITORING
The monitoring of radiation dosage, both instantaneous and cumulative, is more complicated than it might seem. The need for accurate and unbiased radiation monitoring is exemplified by the recent confusion regarding measurement levels around the Fukushima nuclear facility.[33] Sampling may involve various potential locations and sources for the assessment of the presence and the intensity of radioactivity from both the physical surroundings and the affected individuals.
When monitoring radiation among those exposed to fallout or those in direct contact with radioactive materials, accurate assessment involves multiple sources and samples in order to adequately assess the level of exposure and risk. Sources that can be sampled include blood, urine, fecal matter, nasal secretions/swabs, tissue samples, fluid irrigation, and clothing articles. It is important to remember that secondary exposure (i.e., healthcare personnel exposure by proximity to direct radiation disaster victims) can also result in significant doses of radiation. Radioactive contamination is assessed and then reassessed using a radiation detector held at a relatively constant distance from the skin over the entire body.[14]
Monitoring needs to be performed often, and should be continued until the threat has been minimized or eliminated. During the decontamination procedure, monitoring reassessments should continue until a goal of residual contamination of no greater than twice the background radiation is achieved or until only 10% reduction is noted between two consecutive rounds of decontamination.[14] As previously shown, radioactive contamination can be distributed unevenly over “patchy” areas, depending on environmental factors such as wind patterns or precipitation.[34] Perhaps the most important lessons from previous civilian incidents were that safety protocols must be followed strictly, especially for the emergency and clean-up workers at the contaminated site. Furthermore, the early recognition of severe radioactive contamination and activation of emergency response systems may save lives. Dosimeters and other radiation safety devices must be stored on site at all nuclear facilities, and should be maintained in a perfect working order.
Elements involved in radiation injury
The risk of adverse effects from radiation exposure is proportional to the total dose absorbed and the rate at which the dose is delivered. For example, cellular repair mechanisms may be able to effectively cope with continued low-dose radiation rates, but are unlikely to handle similar doses of radiation if they are delivered more rapidly.[14] Therefore, one could speculate that acute, rather than chronic, radiation exposure is more likely to cause malignant transformation within the affected tissues.[35]
Before discussing the different possible types of radioactive contamination, it is important to understand and know the different types of radioactive elements (or radionuclides) that could be involved in a nuclear disaster. For example, major elements found in the Chernobyl incident fallout were iodine-131 and cesium-137.[34] Other radioactive isotopes including niobium, cerium, ruthenium, plutonium, and strontium were also found. Highly radioactive sources are also available in the industry and could be used maliciously, such as cobalt-60 and cesium-137, previously used in radiotherapy machines, and cesium-137 and iridium-192, used in industrial radiographic devices [Table 3].[15]
Whole body exposure
Radiation injury is caused by the deposition of free energy into tissue, which promotes the creation of free radicals and breakdown of DNA and other cellular structures and processes. The risk of adverse effects is proportional to the total absorbed dose a person receives and the rate at which that dose is delivered. Rapidly dividing cells in the human body (intestinal mucosa, bone marrow) are most susceptible to radiation damage.[14] The acute radiation syndrome develops after whole body or significant partial body irradiation of greater than 1 Gy is delivered at a relatively high dose rate. There are several distinct syndromes that may occur in acute radiation sickness, which we will review with regard to body systems in the subsequent paragraphs.
Depending on the absorbed dose, the symptoms of acute radiation sickness may manifest within days to weeks of exposure. There are three phases of the clinical course following the exposure. In the prodromal phase, the acute radiation syndrome manifests within 48 h to 6 days of exposure. In the latent phase, the exposed person may show signs of improvement, but this is transient, and is followed by the manifest illness phase, in which the overt syndrome manifestations develop. This last phase may persist for weeks and is most difficult to manage, often due to intense immune suppression. Depending on the radiation dose and the intensity of medical treatment, the patient will likely live if he or she survives this phase.[36]
The hematopoetic syndrome is caused by the irradiation of bone marrow stem and progenitor cells and is seen with whole body radiation greater than 1 Gy. In the weeks after radiation exposure, acute pancytopenia occurs, which predisposes the body to severe infection, sepsis, bleeding, and poor wound healing. This syndrome takes on special significance in cases of combined radiation and traumatic injury, where surgical procedures (celiotomy, wound debridement, or skeletal fixation) are completed before the onset of the hematopoetic syndrome and associated sequelae.[37]
The gastrointestinal syndrome is characterized by the loss of intestinal crypts and breakdown of the mucosal barrier. At doses greater than 12 Gy, it carries mortality greater than that associated with the hematopoietic syndrome. The most frequent symptoms associated with the gastrointestinal syndrome are abdominal pain, diarrhea, nausea, and vomiting. Symptoms may begin as early as 4–6 h following exposure. This is usually followed by a latent phase of 5–7 days, where one can see severe diarrhea, vomiting, and high fevers. The disease process may progress quickly to bowel obstruction or perforation and may result in severe electrolyte abnormalities, acute renal failure, and sepsis.
The cerebrovascular syndrome is less well defined than the other syndromes and usually presents with fevers, hypotension, change in mental status, ataxia, and seizures. It may be difficult to distinguish from the gastrointestinal syndrome, but should be suspected with radiation doses greater than 20-30 Gy. The ensuing circulatory collapse once the full syndrome begins may bring about death in <48 h.
The cutaneous syndrome from radiation burns is characterized by loss of epidermis and dermis, and may be associated with profound localized edema. It may also lead to the extremity compartment syndrome. Patients presenting with burns immediately following exposure are more likely to have thermal rather than a radiation burn, which usually develops after a latent period.[36]
In the absence of dosimetry, clinical signs may need to be followed to assess the severity of exposure. If no vomiting has occurred within 4 h of the exposure, severe clinical effects are unlikely. If the time to emesis is less than 2 h, the total body dose is at least 3 Gy. The median radiation dose for patients who have emesis in less than an hour from exposure is 6.5 Gy.[27] This easy clinical assessment may be done in cases when dosimeters are not readily available and there is no clinical laboratory on site.
Localized exposure
Localized exposure results from direct handling of a radioactive material, and because the dose rate decreases quickly with the distance from the object, the whole body effect can be minimal. Thus, morbidity and mortality is likely to be lower than that with the whole body exposure. Localized radiation injury usually presents as delayed erythema with blistering and desquamation, usually >10 days after initial exposure.[14] The extent of the penetration of the radiation is an important outcome determinant in cases of local exposure. With a heavy radioactive fallout, beta radiation causes superficial skin burns, especially on body surfaces not covered by clothing.[15]
Internal contamination
Internal contamination occurs due to the dispersal of a powdered, liquid, or gaseous radioactive material, which may enter the body by inhalation, ingestion, or through contact with skin, wounds, or burns. Effective treatment requires knowledge of both the radionuclide and the chemical form of the contaminant. Internal contamination may be treated in several ways, including dilution of the contaminant, reduction of absorption, blockage, displacement by nonradioactive materials, and chelation (see the section on general therapeutic approaches).[15]
External contamination
Radioactive contamination of clothing and exposed skin does not necessarily constitute a medical emergency. Immediate life-threatening injuries should be treated first, and then, once stabilized, the patient should be decontaminated. With proper decontamination, as much as 90% of radioactive contamination may be eliminated (see the section above on the general approach to radiation incident victims). All exposed areas should be gently scrubbed and clothing should be disposed of in properly labeled plastic bags/containers.
Contaminated burns and wounds
If an open wound has been contaminated with a radioactive material, it should be gently rinsed with water and treated according to a proper aseptic technique. The wound should be excised if it is suspected to be contaminated with an alpha-emitting radionuclide, as it is usually long-lived.[15] If there was greater than 1 Gy of total body exposure, the wound should be closed as soon as possible to prevent complications involved with combined injury syndrome once the patient becomes pancytopenic and more susceptible to infection.
Secondary exposure
Exposure of the remote staff and emergency responders is always a risk, especially in catastrophic events, such as the Chernobyl or Fukushima plant explosions. Individuals involved in emergency and rescue efforts should be continuously monitored for total body exposure, and as soon as their doses exceed established thresholds, other unexposed individuals should take their place. Emergency responders should also follow basic principles of external contamination, change their clothes, and shower frequently. After the Chernobyl incident, 58 firemen and clean-up workers were exposed to intense external contamination for days and failed to follow basic safety rules such as showering and changing clothes regularly. Nineteen of these firemen eventually died from complications of the cutaneous syndrome. When workers who were in the reactor area at the time of the accident were later decontaminated, the medical staff at the site wore protective clothing, used proper technique, and received very low radiation doses (less than 0.01 Gy).[27]
Societal and psychosocial aspects of civilian nuclear incidents
The impact of any disaster invokes a sense of stress and fear, and nuclear incidents are no less traumatic. Fortunately, nuclear incidents are not as commonly encountered as natural disasters (i.e., floods, hurricanes, tornados). However, the lack of familiarity during the response to a nuclear incident and its outcomes can increase the associated stress among both victims and providers. After nuclear weapon detonation, it is estimated that approximately 75% of affected people will have some degree of psychological symptoms.[15] Others have theorized that in disaster scenarios, such as domestic terrorism, psychiatric disorders will be among the most common findings in both the victims and the society at large.[38] High-risk patients during a nuclear incident include patients with a history of mental illness in addition to children, pregnant women, and women with young children, followed by emergency and other involved workers.[15]
During a nuclear incident, openness and communication is the key to maintaining trust and order in a society.[15] Health physicists, although primarily consumed with the details of the actual nuclear incident itself, are invaluable to physicians who may not have sufficient training in radiation victim care.[39,40] While people are often courageous and altruistic during natural disasters (such as fire), a disaster involving an “invisible force” of radiation poses an unfamiliar threat that may lead to panic and contagious somatization.[38] Public and written briefings may be an option to effectively reach large groups of people and to decrease the overall sense of panic and uncertainty.[39]
An area of medicine that is often overlooked during disasters is the need for palliative care. Palliative care is aimed at patients facing life-threatening illness so it is reasonable that patients who are likely to die from a nuclear incident should also receive palliative care. The framework of identifying patients in need of palliative care and delivering the appropriate palliative care depends on the nature of the incident/disaster. Planning should include balancing scarce resources, the triage process, and identifying services that can be reasonably provided given the nature of the mass casualty incident.[41] While the general focus of end-of-life care is on the patient, palliative care should extend to all individuals involved in that patient's care, both family and healthcare providers. Physicians may be forced to deal with ethical issues not usually encountered in daily practice with the need to triage patients, prioritize limited resources, and face altered standards of care unique to the incident. Educational curriculum should be established prior to the event to empower healthcare providers with a practical yet virtue-based ethical framework to handle medical care under extreme conditions.[42]
GENERAL MANAGEMENT: SECURITY AND MASS TRIAGE
The management of events involving the dispersal of radioactive materials can be divided into three phases: preparation, dealing with the acute crisis, and management of its consequences. All phases are important, but if planning and preparation are done correctly, management becomes much easier.
Preparation
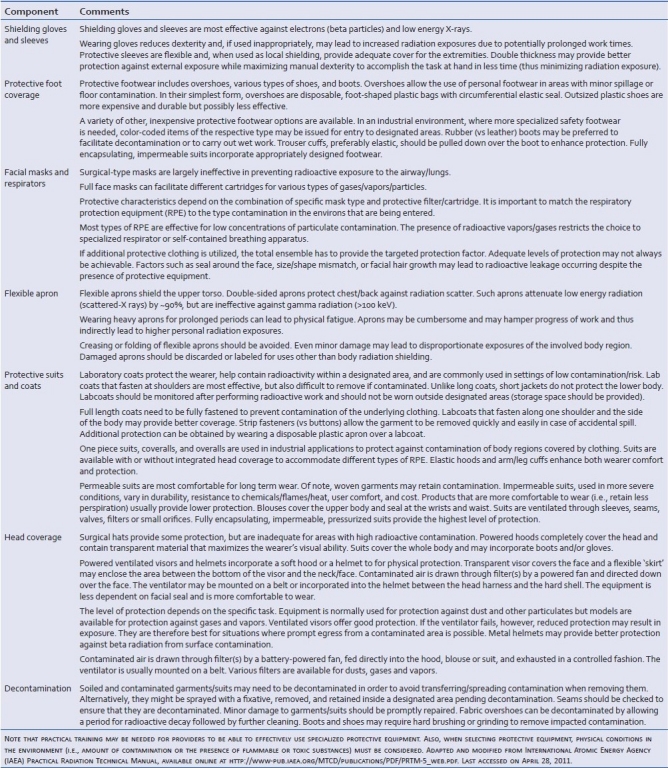
The preparation phase of a disaster response includes planning, clarification of command and control, assignment of organizational tasks, development of communications systems, and assessment of the equipment required.[15] All levels of healthcare should be involved with Emergency Operations Planning. An emergency response plan should outline the respective roles and responsibilities of each participant and the various steps to be taken should an event occur.[43] Components of an effective Emergency Operations Plan (EOP) include personnel and resource management, worker health and safety, and effective communications. The implementation of the EOP should be a community exercise involving not only medical personnel, but also local public safety, public health, and mental health services. Finally, first responders from fire departments, emergency medical services, law enforcement, and other agencies should be involved in all aspects of planning and drilling.[43] All potential responders to civilian nuclear incidents should be familiar with general types and uses of specialized protective equipment [Table 5]. Moreover, familiarity with and appropriate use of nuclear protective equipment should be included in plans and drills directed at nuclear incident preparedness.
Table 5.
General types and descriptions of protective equipment available for various levels of nuclear incident responders
Managing the scene
The first responders to a radiation release have several important issues to take into account. According to the Radiation Emergency Medical Management (REMM) website, the first on-scene priority in the event of a radiological incident would be to notify the appropriate authorities.[44] After the terrorist attacks of 9/11, several Federal agencies have begun preparation for a potential radiological release. Within the Federal government, the Departments of Health and Human Services, Defense, Energy, and Homeland Security, as well as the Environmental Protection Agency and the United States Coast Guard are all involved in planning.[45] The lead agencies change depending on the nature of the incident.
In the event of a terrorist incident, the Federal Bureau of Investigation (FBI) is the lead federal agency. Their job is crisis management and security. During such an event, the FBI would work to ensure that there is no further threat and would establish control over the site of the attack as a crime scene.[15] This reiterates the importance of the initial major countermeasures to any disaster – protecting the public and controlling access to the accident site.[46] In completing this task, it is essential that Federal agencies mentioned above work well with state, local, tribal, territorial, regional, and private sector responders.[47]
Consequence management is the prevention of further damage, protection of the public, decontamination, and disposal of the radioactive material. During consequence management in a terrorist incident, the Federal Emergency Management Agency (FEMA) becomes the lead federal agency in the United States. In both phases, a federal joint operating center is established to work with other federal agencies. One major function of incident command is the assisting with public safety. Frequent communications and updates by a public safety officer can help reduce anxiety and panic among victims and responders.[14,48]
The next step in managing the scene is establishing an incident parameter. The determination of the parameter depends on physical factors, medical issues, and security needs. Physical factors paramount to the security parameter are numerous. The first issue to consider is the nature and severity of the radiation incident (radiologic dispersal devices [RDDs], radiation exposure devices [REDs], nuclear reactor incident). The second factor to consider is the possibility of coexisting threats such as chemicals, biologics, or explosives. The final factor that needs to be recognized when establishing an incident parameter is managing risks from the physical damage that may have already occurred. Security issues to consider include protecting and gathering forensic information, establishing and maintaining incident control, and protecting government and private institutions. One key feature to successfully establishing an incident parameter is the awareness that the boundaries may change over time as radiation worsens or decays.
After the incident command is established, the next step in managing the scene is to monitor the types and amounts of radiation. This monitoring begins as soon as safely possible and continues throughout the duration of the response and recovery. Once adequate monitoring is established, patient flow can begin.
Specific needs pertaining to the security parameter include maintaining responder and public safety. The focus is on saving the lives of those with traumatic injuries while controlling access to the disaster zone.[46] Another important medical aspect to consider is mental health and psychological impact. Several studies denote that the mental health impact is substantial in radiation emergencies, and effective communication may be a key component in dealing with this issue.[46] Media channels should convey consistent, effective messages to the public. Because there is usually a great deal of confusion and misinformation that accompanies nuclear emergencies, patients should be given accurate information and told where to go for treatment.
Management during crisis: Triage, treat, and transport
Initial management consists of on-the-scene triage and transportation of victims to the emergency department for treatment. During most mass casualty incidents, local emergency medical services providers are first to arrive and, therefore, provide the initial triage, treatment, and transport. Experience shows that during large-scale events, people self-transport or use nonemergency medical services mechanisms to go to the nearest hospital. For these reasons, it takes considerable time before a secure perimeter can be established.[47]
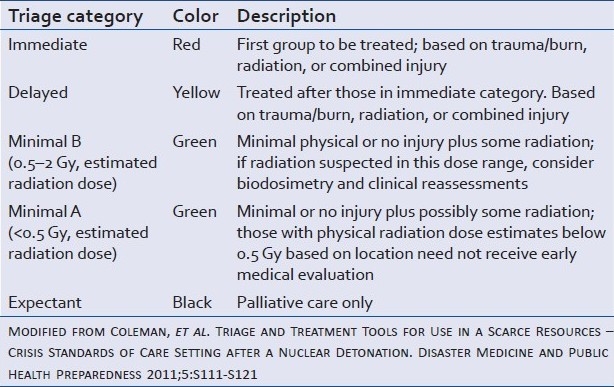
Triage determines the order in which patients are treated and transported to the nearest or most appropriate hospital. Triage for a radiological disaster is similar to natural disaster triage in that both involve effective distribution of limited resources. The first important principle of triage is based on the fact that minimally contaminated patients and those who are only exposed to radiation pose minimal threat to responders. Responders in the proximity of or in contact with a few individuals who are lightly contaminated externally will be exposed to ionizing radiation. This type of exposure, depending on the isotopes, usually involves very little risk.[43] For this reason, life-saving tasks should be performed on all patients prior to the management of radiation problems. That said, persons with life-threatening injuries should be handled as if they were contaminated and taken to a local hospital. It is well established that in mass casualty incidents, medical triage determines victim care requirements – immediate care, delayed care, palliative care, or no treatment – and establishes victim priority for transport to definitive care locations [Table 6].
Table 6.
Triage categories for injuries from radiation only and radiation plus trauma
Transported victims of a nuclear incident will fall into one of three categories: those who can self-evacuate, those who are ambulatory but require medical care, and the nonambulatory. Those who are uninjured or have minor injuries should be evacuated (upwind if possible) and then evaluated for possible contamination.
In order to determine where, when, and who to transport, the dose of radiation encountered needs to be estimated. Recommendations state that people should stay indoors for up to 2 days if a dose of 1 rem is likely to be reached, with evacuation for up to 1 week if the likely dose is 5 rem or higher.[15] Temporary relocation is recommended at a dose of 3 rem in the first month or 1 rem in the subsequent month. Permanent resettlement is recommended if the lifetime dose is expected to be 100 rem. If the first responders are unfamiliar with handling medical radiation cases, a health physicist can be consulted. A health physicist can work with first responders to provide reassurance, help prevent panic, and activate the medical radiation emergency plan.[39]
Following a large-scale disaster, it is often necessary to transport victims to hospitals in a wider area because the local trauma centers are quickly overwhelmed. This certainly holds true for a mass casualty incident involving radiation as patients will need to be transported to hospitals with specialty services for the management of radiation-related injuries.[47]
Immediate medical management and prophylactic approaches
General comments
Dedicated medical treatment is necessary for patients who received external exposure with absorbed doses greater than 1 Gy (equal to 100 rad). There are many tasks that need to be performed in an organized sequence so that the evaluation and treatment of victims exposed to radiation can proceed efficiently and safety of both the patient and the emergency medical staff can be maximized.[14]
Koenig et al.[14] list the following components of such evaluation: (a) first aid and resuscitation; (b) medical/surgical stabilization; (c) definitive treatment of life-threatening injuries; (d) prevention/reduction of internal contamination; (e) assessment of external contamination with concurrent decontamination; (f) treatment of minor associated injuries; (g) containment of radiation to the treatment area with the prevention of contamination of healthcare personnel; (h) reducing exposure of rescue/treatment personnel to external radiation; (i) assessment/treatment of internal radioactive contamination; (j) assessment of local radiation injuries; (k) patient counseling regarding long-term effects and risks of radiation exposure; and (l) long-term follow-up of patients with significant exposure and/or internal contamination.
Decontamination and related maneuvers
Following the attacks of September 11, 2001, procedures for decontamination have been incorporated into mass casualty incident protocols for most healthcare systems.[14] However, most institutions are unlikely to be prepared to receive massive numbers of victims exposed to radioactive materials.[14] Contamination of skin or wound surfaces is usually not life threatening to the victim or the healthcare workers caring for the patient. That said, decontamination is best carried out before transport to a healthcare facility or before the patient physically enters the emergency department. In general, the removal of shoes and outer clothing will reduce the external radiation to around 10% of the originally measured level. Residual contamination is measured using a radiation detector held at a relatively constant distance from the skin over the entire body. This is then followed by whole body decontamination using soap and warm water, which further reduces any residual contamination. A balance between mechanical removal and skin damage has to be observed when performing mechanical brushing over skin surfaces. Any open wounds need to be covered to minimize internal contamination. The decontamination procedure should be continued until a goal of residual contamination of no greater than twice the background radiation is achieved or until only 10% reduction is noted between two consecutive attempts.[14] The cleaning of contaminated open wounds depends on the nature of the injury; while lacerations may need to be locally excised if the usual techniques are not sufficient in removing contamination, most abrasions can be cleaned using standard protocols. Puncture wounds can be decontaminated using lavage/irrigator devices. Wounds containing impacted radioactive shrapnel require special care in order to avoid healthcare staff exposure. At times, amputation may be required in order to adequately remove the source of radiation from the penetrating wound.[14]
For suspected ingestions of radioactive materials, the administration of aluminum hydroxide (especially for strontium isotope ingestion) or magnesium carbonate antacids may reduce gastrointestinal absorption. If radioactive ingestion occurred less than 2 h prior to presentation, gastric lavage may also be beneficial in reducing internal contamination. The use of cathartics and enemas may be beneficial in reducing the gastrointestinal transit time (and thus the radioactive exposure time) for larger ingestions or for patients who present in a delayed fashion.[14]
Summary of commonly used medical approaches to radiation exposure
There are three general treatment strategies available for acute radiation exposure: (a) radioprotection; (b) radiation mitigation; and (c) radionuclide elimination.[14] Although details of each of the above approaches are beyond the scope of this general review, the ensuing paragraphs will briefly outline each of the three strategies, with representative therapies listed and referenced to help direct the reader to more definitive sources.[36] However, it is important to note that many of the therapies currently approved or under investigation have significant potential side effects and should be used cautiously and under radiation expert guidance/supervision.[49]
Radioprotective agents currently utilized or under study include membrane-permeable nitroxides, phosphorylated aminothiols (i.e., amifostine), keratinocyte growth factor, isoflavone genistein, angiotensin-converting enzyme inhibitors, nonandrogenic steroid androstenediol, and alpha-tocopherol.[14,49–51] Radiation mitigating agents include androstenediol, glutamine, colony-stimulating factors, and pentoxifylline.[14,36,52,53] Radionuclide eliminators include aluminum antacids, ferric hexacyanoferrate (i.e., Prussian blue), bicarbonate, barium sulfate, calcium gluconate, calcium and zinc diethylenetriaminenepentaacetate (Ca-/Zn-DTPA), penicillamine, potassium iodide, and sodium alginate.[14,54,55]
Long-term consequences of radiation exposure
Fortunately for mankind, there have only been four instances of true radiation mass casualty event.[46] The most detailed studies of radioactive release survivors come from the atomic bomb detonations in Japan in 1945. Just years after the attacks in Hiroshima, Japan, Dr. Takuso Yamawaki began noticing a rise in leukemia rates in his clinical cases. Two years after the United States unleashed the atomic bomb on Japan, President Harry Truman created the Atomic Bomb Casualty Commission (ABCC). The 1947 commission was tasked with examining the medical effects of the radiation release on Japanese victims. The ABCC became the Radiation Effects Research Foundation (RERF) in 1975. Through their work, it has since been determined that approximately 40% of the atomic bomb survivors are alive today. Of interest, about 80% of those exposed before the age of 20 are alive today.[56] It is known that after the attacks, the proportion of leukemia rose with a subsequent rise in solid organ cancers. As the ABCC continued to follow the patients, it was apparent that risks for radiation-induced leukemia differed in two major respects from those for most solid cancers. First, radiation caused a larger percent increase in leukemia rates. Second, the increase appeared sooner after exposure, especially in children. The ABCC noted that the excess leukemia began appearing about 2 years after radiation exposure, and the excess peaked at about 6-8 years after exposure.[56]
In the Life Span Study (LSS) cohort commissioned by the ABCC, researchers determined that although leukemia accounts for only about 3% of all cancer deaths and less than 1% of all deaths; it constitutes about 16% of all excess cancer deaths from radiation exposure in Japanese survivors. Furthermore, in the unexposed Japanese population, the lifetime risk of leukemia is about 7 cases per 1000 people. For typical survivors in the LSS, who received a 0.005 Gy or greater dose (a mean dose of about 0.2 Gy), the lifetime leukemia risk increased to about 10 cases per 1000 (or relative risk of nearly 1.5). That said, today little, if any, excess of leukemia is occurring in Japan.[57]
On March 28, 1979, an accident at the TMI nuclear power plant in Pennsylvania produced the release of xenon and iodine radioisotopes into the environment in what was considered a minimal release.[58] Most conclude that this radiation release was about equivalent to a chest x-ray. This event has been studied on several occasions and no definitive conclusions have been made. Interestingly, heart disease is the largest killer in the area around the power plant. A 1997 study by Wing et al. showed increases in all cancer (2%), lung cancer (8.2%), and leukemia (11.6%).[59] Additionally, a 2008 study showed an increased incidence of thyroid cancer in the county surrounding TMI. A causal relationship could not be established.[60] Other studies have also not been able to show definitive relationships.
On April 26, 1986, the Chernobyl nuclear power plant experienced a meltdown that caused a radioactive release. Located in Ukraine near the border of Belarus, the plant was rocked by two explosions that destroyed the core of unit 4 of the power plant and the roof of the building. This damage resulted in releases of radioactive gases, aerosols, and finely fragmented nuclear fuel particles. Iodine-131 and cesium-137 are the radionuclides that contributed to the worst nuclear accident ever. General summary of cancers associated with the Chernobyl incident can be seen in Table 7.
Table 7.
Summary of cancer in those exposed to radiation from the 1986 Chernobyl incident
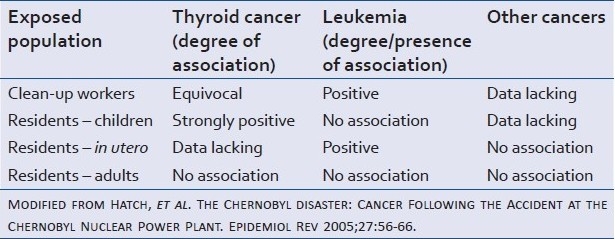
Relatively less is known about the long-term effects of this nuclear disaster because not as much time has passed as with the atomic bombs of Japan. What is known is that the incidence of leukemia and thyroid cancer has increased in the victims of the meltdown. The increase in leukemia is seen most impressively in workers who responded to the clean-up. A suggestion of increasing thyroid cancers was also seen in the earliest responders to the clean-up. Additionally, a large rise in thyroid cancer was seen in the children who lived in the contaminated area.[25]
Just 1 year after the Chernobyl disaster, on September 13, 1987, in Goiania, Brazil, two individuals removed the head of a radiotherapy device containing a 50.8 TBq cesium-137 source left behind in a vacant clinic.[61]. As the result of the damage to the source integrity and its sale at a junkyard, many Brazilians were irradiated and contaminated. Reports show that 129 persons were contaminated, 20 were hospitalized and 4 died acutely. Of the patients followed after the event, there have been three cancer-related deaths.
The long-term effects of the radiation release are not well studied in other situations. A 2007 paper examined two large unintended acute releases of uranium – at Kerr McGee's Sequoyah Fuels Corporation in Oklahoma and United Nuclear Corporation's Church Rock uranium mill in New Mexico. Both were incidents of a comparable magnitude to the TMI release. The predominantly Native American populations involved have not been well studied in terms of long-term effects.[21]
In conclusion, one could expect an increasing incidence of cancer following a large-scale nuclear release. Children may be especially vulnerable. Thyroid cancer and leukemia would likely dominate, with solid cancers following. For these reasons, anyone suspected of having received a whole-body dose of 100 mSv (10 rem) or more, even if there is no evidence of deterministic effects, is advised to undergo periodic health examinations.[43] Studies are still ongoing regarding the effects of the four largest civilian nuclear incidents in human history.
CONCLUSIONS
Due to their long-lasting impact on both human health and the environment, nuclear incidents place our civilization in a precarious position. In our energy-addicted world, scarcity of natural resources and the impact of their use on the planet leave us with few choices with which to sustain our continued growth. Although nuclear energy represents a plentiful energy resource, major risks related to the use and storage of nuclear materials call for a renewed open debate regarding the use of nuclear energy in the 21st century. In this article, we presented a concise summary of the basic understanding of the science, history, management, monitoring, and aftermaths of nuclear incidents so that we may better understand the role of prevention, risks, and risk management in the provision of nuclear power as a solution to the energy needs of our planet, as well as acknowledging its use as a potential terrorist threat. The information provided herein presents the reader with the minimum knowledge necessary to become an informed participant in this important and ongoing dialog.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.ENS. European Nuclear Society: Nuclear plants world-wide. 2011. [Last cited on 2011 April 11]. Available from: http://www.euronuclear.org/1-information/map-worldwide.htm .
- 2.Keeney RL, von Winterfeldt D. Managing nuclear waste from power plants. Risk Anal. 1994;14:107–30. [Google Scholar]
- 3.Gerber TC, Carr JJ, Arai AE, Dixon RL, Ferrari VA, Gomes AS, et al. Ionizing radiation in cardiac imaging: A science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 2009;119:1056–65. doi: 10.1161/CIRCULATIONAHA.108.191650. [DOI] [PubMed] [Google Scholar]
- 4.Washington, DC: United States Environmental Protection Agency; 2007. EPA, United States Environmental Protection Agency: Ionizing radiation fact book. [Google Scholar]
- 5.DOH WS. Washington State Department of Health: What is ionizing radiation? W.S.D.o. Health. 2003 [Google Scholar]
- 6.Vorobiev AI. Acute radiation disease and biological dosimetry in 1993. Stem Cells. 1997;15(Suppl 2):269–74. doi: 10.1002/stem.5530150736. [DOI] [PubMed] [Google Scholar]
- 7.NRC. United States Nuclear Regulatory Commission basic references: Glossary. 2010. [Last cited on 2011 Apr 11]. Available from: http://www.nrc.gov/reading-rm/basic-ref/glossary.html .
- 8.Jacobi W. The concept of the effective dose-a proposal for the combination of organ doses. Radiat Environ Biophys. 1975;12:101–9. doi: 10.1007/BF01328971. [DOI] [PubMed] [Google Scholar]
- 9.Princeton_University. Open source radiation safety training. Module 1: Radiation properties. Open source radiation safety training. 2006. [Last cited on 2011 Apr 11]. Available from: http://web.princeton.edu/sites/ehs/osradtraining/radiationproperties/radiationproperties.htm .
- 10.Landau E. Radiation safety: what you should know. 2011. [Last cited on 2011 Apr 11]. Available from: http://www.wdtn.com/dpps/health/healthy_living/radiation-safety%3Awhat-you-should-know_3764849 .
- 11.Wiegert RG, Odum EP, Schnell JH. Forb-arthropod food chains in a one-year experimental field. Ecology. 1967;48:75–83. [Google Scholar]
- 12.Burger J, Gaines KF, Peles JD, Stephens WL, Jr, Boring CS, Brisbin IL, Jr, et al. Radiocesium in fish from the Savannah River and Steel Creek: potential food chain exposure to the public. Risk Anal. 2001;21:545–59. doi: 10.1111/0272-4332.213131. [DOI] [PubMed] [Google Scholar]
- 13.Segal MG. Agricultural countermeasures following deposition of radioactivity after a nuclear accident. Sci Total Environ. 1993;137:31–48. [Google Scholar]
- 14.Koenig KL, Goans RE, Hatchett RJ, Mettler FA, Jr, Schumacher TA, Noji EK, et al. Medical treatment of radiological casualties: Current concepts. Ann Emerg Med. 2005;45:643–52. doi: 10.1016/j.annemergmed.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 15.Mettler FA, Jr, Voelz GL. Major radiation exposure-what to expect and how to respond. N Engl J Med. 2002;346:1554–61. doi: 10.1056/NEJMra000365. [DOI] [PubMed] [Google Scholar]
- 16.Anno GH, Baum SJ, Withers HR, Young RW. Symptomatology of acute radiation effects in humans after exposure to doses of 0.5-30 Gy. Health Phys. 1989;56:821–38. doi: 10.1097/00004032-198906000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Diaz Maurin F. Fukushima: Consequences of systemic problems in nuclear plant design. Econ Polit Wkly. 2011;46:10–2. [Google Scholar]
- 18.DiCarlo AL, Maher C, Hick JL, Hanfling D, Dainiak N, Chao N, et al. Radiation injury after a nuclear detonation: Medical consequences and the need for scarce resources allocation. Disaster Med Public Health Prep. 2011;5(Suppl 1):S32–44. doi: 10.1001/dmp.2011.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dainiak N, Ricks RC. The evolving role of haematopoietic cell transplantation in radiation injury: Potentials and limitations. BJR Suppl. 2005;27:169–74. [Google Scholar]
- 20.Nenot JC. Overview of the radiological accidents in the world, updated December 1989. Int J Radiat Biol. 1990;57:1073–85. doi: 10.1080/09553009014551201. [DOI] [PubMed] [Google Scholar]
- 21.Brugge D, deLemos JL, Bui C. The Sequoyah corporation fuels release and the Church Rock spill: Unpublicized nuclear releases in American Indian communities. Am J Public Health. 2007;97:1595–600. doi: 10.2105/AJPH.2006.103044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Russia: 2011. Broadcast, Russia Today: Fukushima plutonium leak comparable to Chernobyl disaster. [Google Scholar]
- 23.Gundersen A. Fukushima Accident Severity Level Raised to ‘7’: Gundersen Discusses Lack of US Radiation Monitoring Data. 2011 [Google Scholar]
- 24.Linnemann RE. Soviet medical response to the Chernobyl nuclear accident. JAMA. 1987;258:637–43. [PubMed] [Google Scholar]
- 25.Hatch M, Ron E, Bouville A, Zablotska L, Howe G. The Chernobyl disaster: cancer following the accident at the Chernobyl nuclear power plant. Epidemiol Rev. 2005;27:56–66. doi: 10.1093/epirev/mxi012. [DOI] [PubMed] [Google Scholar]
- 26.Guskova AK. UNSCEAR 1988 Report. Appendix to Annex G. Early effects in man of high radiation doses. Acute radiation effects in victims of the Chernobyl accident. 1988 [Google Scholar]
- 27.Flynn DF, Goans RE. Nuclear terrorism: Triage and medical management of radiation and combined-injury casualties. Surg Clin North Am. 2006;86:601–36. doi: 10.1016/j.suc.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Cardis E, Howe G, Ron E, Bebeshko V, Bogdanova T, Bouville A, et al. Cancer consequences of the Chernobyl accident: 20 years on. J Radiol Prot. 2006;26:127–40. doi: 10.1088/0952-4746/26/2/001. [DOI] [PubMed] [Google Scholar]
- 29.Johnston WR. Database of radiological incidents and related events-Johnston's Archive: Vinca reactor accident, 1958. 2005. [Last cited on 2011 Apr 15]. Available from: http://www.johnstonsarchive.net/nuclear/radevents/1958YUG1.html .
- 30.Beitler S. Idaho Falls, ID Atomic Reactor Accident, Jan 1961. 2009. [Last cited on 2011 Apr 15]. Available from: http://www3.gendisasters.com/node/13374 .
- 31.Cardis E, Hatch M. The Chernobyl accident-an epidemiological perspective. Clin Oncol (R Coll Radiol) 2011;23:251–60. doi: 10.1016/j.clon.2011.01.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnoor JL. Lessons from Fukushima. Environ Sci Technol. 2011;45:3820. doi: 10.1021/es200937v. [DOI] [PubMed] [Google Scholar]
- 33.VOA-News. Confusion over radiation levels at japan nuclear plant. 2011. [Last cited on 2011 Apr 13]. Available from: http://www.voanews.com/english/news/asia/Confusion-Over-Radiation-Levels-at-Japan-Nuclear-Plant-118733894.html .
- 34.GreenFacts. Scientific facts on the Chernobyl nuclear accident. 2011. [Last cited on 2011 Apr 13]. Available from: http://www.greenfacts.org/en/chernobyl/l-2/3-chernobyl-environment.htm .
- 35.Fajardo LF, Berthrong M, Anderson RE. New York, NY: Oxford University Press; 2001. Radiation Pathology. [Google Scholar]
- 36.Waselenko JK, MacVittie TJ, Blakely WF, Pesik N, Wiley AL, Dickerson WE, et al. Medical management of the acute radiation syndrome: Recommendations of the Strategic National Stockpile Radiation Working Group. Ann Intern Med. 2004;140:1037–51. doi: 10.7326/0003-4819-140-12-200406150-00015. [DOI] [PubMed] [Google Scholar]
- 37.Engelhardt M, Kaffenberger W, Abend M, Gerngross H, Willy C. Radiation and burn trauma (combined injury).Considerations in surgical treatment. Unfallchirurg. 2001;104:333–42. doi: 10.1007/s001130050736. [DOI] [PubMed] [Google Scholar]
- 38.DiGiovanni C., Jr Domestic terrorism with chemical or biological agents: psychiatric aspects. Am J Psychiatry. 1999;156:1500–5. doi: 10.1176/ajp.156.10.1500. [DOI] [PubMed] [Google Scholar]
- 39.Miller K. Erdman, Health physics considerations in medical radiation emergencies. Health Phys. 2004;87:S19–24. doi: 10.1097/00004032-200408001-00008. [DOI] [PubMed] [Google Scholar]
- 40.Miller CW, Whitcomb RC, Jr, Ansari A, McCurley C, Guinn A, Tucker F. The roles of medical health physicists in a medical radiation emergency. Health Phys. 2007;935(Supp 1):S187–90. doi: 10.1097/01.HP.0000281180.96259.a8. [DOI] [PubMed] [Google Scholar]
- 41.Matzo M, Wilkinson A, Lynn J, Gatto M, Phillips S. Palliative care considerations in mass casualty events with scarce resources. Biosecur Bioterror. 2009;7:199–210. doi: 10.1089/bsp.2009.0017. [DOI] [PubMed] [Google Scholar]
- 42.Holt GR. Making difficult ethical decisions in patient care during natural disasters and other mass casualty events. Otolaryngol Head Neck Surg. 2008;139:181–6. doi: 10.1016/j.otohns.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolbarst AB, Wiley AL, Jr, Nemhauser JB, Christensen DM, Hendee WR. Medical response to a major radiologic emergency: A primer for medical and public health practitioners. Radiology. 2010;254:660–77. doi: 10.1148/radiol.09090330. [DOI] [PubMed] [Google Scholar]
- 44.US-DHHS. United States Department of Health and Human Services. Radiation Emergency Medical Management. 2011. [Last cited on 2011 Apr 14]. Available from: http://www.remm.nlm.gov/index.html .
- 45.Davids MS, Case C, Jr, Confer DL, Weisdorf DJ, Weinstock DM. Medical management of radiation victims in the United States. Health Phys. 2010;98:833–7. doi: 10.1097/01.HP.0000346701.04476.0d. [DOI] [PubMed] [Google Scholar]
- 46.Hopmeier M, Abrahams J, Carr Z. Some considerations for mass casualty management in radiation emergencies. Health Phys. 2010;98:790–4. doi: 10.1097/HP.0b013e3181c6f380. [DOI] [PubMed] [Google Scholar]
- 47.Hrdina CM, Coleman CN, Bogucki S, Bader JL, Hayhurst RE, Forsha JD, et al. The “RTR” medical response system for nuclear and radiological mass-casualty incidents: A functional TRiage-TReatment-TRansport medical response model. Prehosp Disaster Med. 2009;24:167–78. doi: 10.1017/s1049023x00006774. [DOI] [PubMed] [Google Scholar]
- 48.USDHHS-REMM. United States Department of Health and Human Services. Radiation Emergency Medical Management. 2011. [Last cited on 2011 Apr 14]. Available from: http://www.remm.nlm.gov/index.html .
- 49.Koukourakis MI, Kyrias G, Kakolyris S, Kouroussis C, Frangiadaki C, Giatromanolaki A, et al. Subcutaneous administration of amifostine during fractionated radiotherapy: A randomized phase II study. J Clin Oncol. 2000;18:2226–33. doi: 10.1200/JCO.2000.18.11.2226. [DOI] [PubMed] [Google Scholar]
- 50.Milas L, Hunter N, Stephens LC, Peters LJ. Inhibition of radiation carcinogenesis in mice by S-2-(3-aminopropylamino)-ethylphosphorothioic acid. Cancer Res. 1984;44:5567–9. [PubMed] [Google Scholar]
- 51.Grdina DJ, Nagy B, Sigdestad CP. Radioprotectors in treatment therapy to reduce risk in secondary tumor induction. Pharmacol Ther. 1988;39:21–5. doi: 10.1016/0163-7258(88)90035-6. [DOI] [PubMed] [Google Scholar]
- 52.Farese AM, Hunt P, Grab LB, MacVittie TJ. Combined administration of recombinant human megakaryocyte growth and development factor and granulocyte colony-stimulating factor enhances multilineage hematopoietic reconstitution in nonhuman primates after radiation-induced marrow aplasia. J Clin Invest. 1996;97:2145–51. doi: 10.1172/JCI118652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.MacVittie TJ, Farese AM, Herodin F, Grab LB, Baum CM, McKearn JP. Combination therapy for radiation-induced bone marrow aplasia in nonhuman primates using synthokine SC-55494 and recombinant human granulocyte colony-stimulating factor. Blood. 1996;87:4129–35. [PubMed] [Google Scholar]
- 54.Brandão-Mello CE, Oliveira AR, Valverde NJ, Farina R, Cordeiro JM. Clinical and hematological aspects of 137Cs: The Goiania radiation accident. Health Phys. 1991;60:31–9. [PubMed] [Google Scholar]
- 55.US-FDA. US Food and Drug Administration. Calcium-DTPA and Zinc-DTPA Information Page. [Last cited on 2011 Apr 11]. Available from: http://www.fda.gov/Drugs/EmergencyPreparedness/BioterrorismandDrugPreparedness/ucm130311.htm .
- 56.Douple EB, Mabuchi K, Cullings HM, Preston DL, Kodama K, Shimizu Y, et al. Long-term radiation-related health effects in a unique human population: Lessons learned from the atomic bomb survivors of Hiroshima and Nagasaki. Disaster Med Public Health Prep. 2011;5(Suppl 1):S122–33. doi: 10.1001/dmp.2011.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.RERF. Radiation Effects Research Foundation. Leukemia risks among atomic-bomb survivors. 2007. [Last cited on 2011 Apr 11]. Available from: http://www.rerf.or.jp/radefx/late_e/leukemia.html .
- 58.Talbott EO, Youk AO, McHugh-Pemu KP, Zborowski JV. Long-term follow-up of the residents of the three mile island accident area: 1979-1998. Environ Health Perspect. 2003;111:341–8. doi: 10.1289/ehp.5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wing S, Richardson D, Armstrong D, Crawford-Brown D. A reevaluation of cancer incidence near the Three Mile Island nuclear plant: The collision of evidence and assumptions. Environ Health Perspect. 1997;105:52–7. doi: 10.1289/ehp.9710552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Levin RJ. Incidence of thyroid cancer in residents surrounding the Three Mile Island nuclear facility. Laryngoscope. 2008;118:618–28. doi: 10.1097/MLG.0b013e3181613ad2. [DOI] [PubMed] [Google Scholar]
- 61.J José de Lima Valverde N, Ferreira da Silva J, Tantalean OB. An update on three radiation accidents in South America. Health Phys. 2010;98:868–71. doi: 10.1097/01.HP.0000345070.33576.f9. [DOI] [PubMed] [Google Scholar]


