Abstract
Traumatic pulmonary artery or vein pseudoaneurysms are extremely rare and angiographic management is gaining grounds. These pseudoaneurysms are caused by both penetrating and blunt chest trauma. We presents a unique case of coexisted pulmonary vein and artery pseudoaneurysm due to penetrating chest trauma managed by angioembolization and inferior vena cava filter insertion for concomitant deep vein thrombosis (DVT) due to contraindication to anticoagulation. The present case represents only the second case of coexisted pulmonary vein and artery pseudoaneurysm and the first with associated DVT making management decision complicated.
Keywords: Chest trauma, coil embolization, gunshot wound, hemoptysis, pseudoaneurysm, pulmonary artery, pulmonary vein
INTRODUCTION
Traumatic pulmonary artery pseudoaneurysms (PAPAs) remain a rare entity with only 24 cases reported in the English literature. Most of these PAPAs are caused by penetrating thoracic injuries.[1] Hemoptysis and chest discomfort are the common presentation.[1,2] Management includes aneurysm resection, lung resection and coil embolization. We present the case of a 21-year-old-active male who developed a pulmonary artery and vein pseudoaneurysm 60 days postinjury after gunshot wound to the chest. This case is unique because of the concomitant venous pseudoaneurysm, history of deep vein thrombosis (DVT) and management decision.
CASE REPORT
A 21-year-old active duty Marine sustained a through-and-through gunshot wound to the right chest while under enemy fire. The patient initially underwent needle decompression in the field and was transferred to the nearest Forward Operation Base (FOB) for further management. Patient present to the FOB with GCS 15, systolic blood pressure of 80, pulse of 130 beats/min and oxygen saturation of 90%. Emergent tube thoracostomy was performed with approximately 2000 ml blood loss in the emergency room. He was taken to the operation room where he underwent repositioning of the chest tube and a second tube thoracostomy with initial output of 100 ml. On-table arteriogram showed intact aortic arch and pulmonary vasculature . Thoracotomy was considered, but a decision was made to observe patient because he was hemodynamically stable and chest tubes output where minimum after the second chest tube placement. Postoperative chest computed topography (CT) showed extensive pulmonary contusion, bullet track but no vascular injury. On postinjury day three, a chest X-ray was suspicious for retained hemothorax and a decision was made to explore the patient. At exploration via video-assisted thoracoscopy, active bleeding from intercostals artery at the posterior gunshot wound was noted and successfully ligated and the retained hemothorax was evacuated. There was no bleeding from the lung parenchyma during the thoracoscopy.
The patient arrived to our facility 9 days postinjury with right chest tube to suction, hemodynamically stable, saturation of 99% in room air and on enoxaparin 30 mg subcutaneously twice a day. The chest tube was place on water seal and then pulled out 24 hours later. Follow up chest X-ray was unremarkable. The patient was placed on therapeutic weight-based enoxaparin for his left common femoral vein thrombosis and discharged home with instruction to follow-up with the coumadin clinic for anticoagulation. However, patient was lost to follow-up and presented to an outside hospital with complaint of intermittent hemoptysis, non-productive cough and chest pain for 3 days. The patient was off his enoxaparin for 7 days when his symptoms began. Chest CT showed two enhancing lesion connected to the pulmonary artery concerning for arteriovenous malformation (AVM's). Per our institution policy, the patient was transferred to our facility for further management. On presentation, the patient was hemodynamically stable, vitals normal and without further episodes of hemoptysis. Chest CT angiogram showed a large (3.1 × 2.5-cm) pseudoaneurysm arising from a sub-segmented branch of the right upper lobe posterior segment pulmonary artery [Figures 1a and b] and a small (1.8 × 1.6-cm) segment from the right upper lobe pulmonary vein [Figure 2]. Bilateral duplex venous ultrasound was normal. Owing to the associated pulmonary vein pseudoaneurysm which is a relative contraindication for anticoagulation, the patient underwent uncomplicated coil embolization of the PAPA [Figure 3] and placement of retrievable inferior vena cava (IVC) filter and was discharged home after 24 hours of observation. At 30 and 120 days post-coiled embolization, the patient remained asymptomatic and chest CT showed persistent resolution of the pseudoaneurysm [Figure 4 and Figure 5]. The IVC filter was removed 5 months after placement without difficulty.
Figure 1.
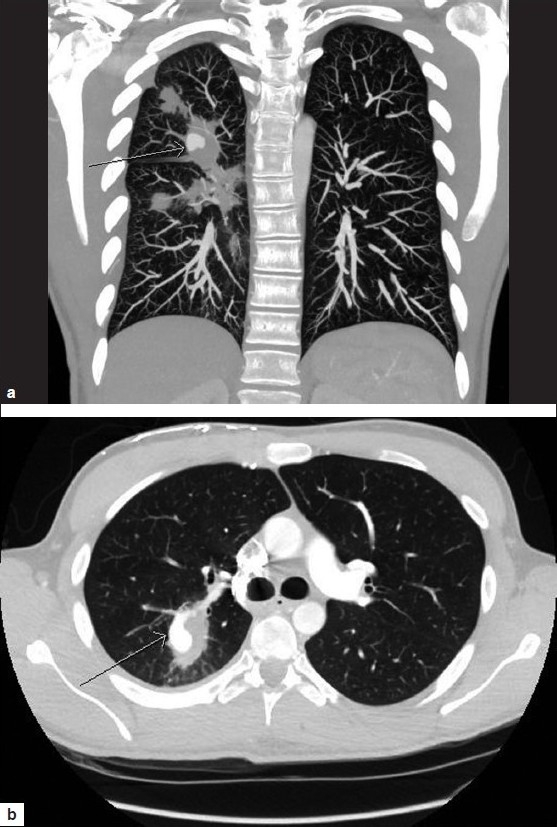
(a) CT scan showing pulmonary artery pseudoaneurysm. (b) CT scan showing pulmonary artery pseudoaneurysm
Figure 2.

CT scan showing pulmonary vein pseudoaneurysm
Figure 3.
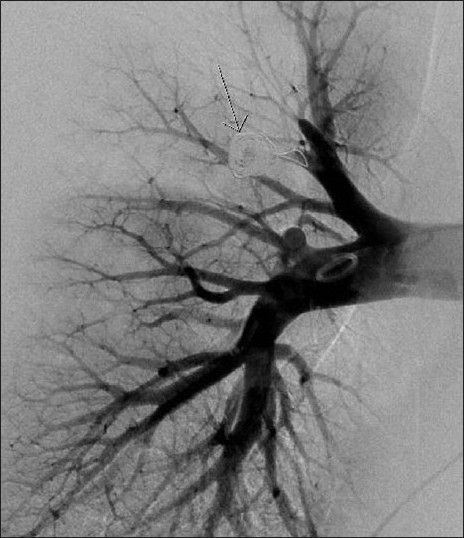
Angiogram demonstrating coiled pulmonary artery pseudoaneurysm
Figure 4.
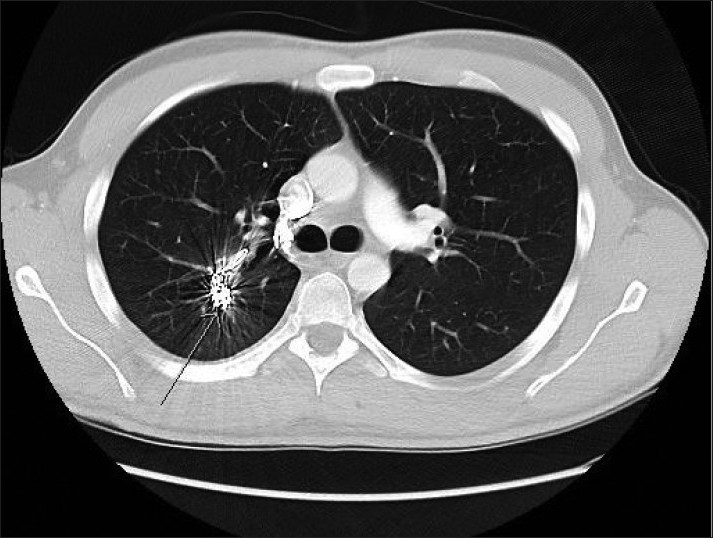
CT scan 30-days post-coiled embolization
Figure 5.

CT scan 120-days post-coiled embolization
DISCUSSION
Traumatic PAPAs are very rare with only 24 cases reported in the English literature. The paucity of cases is due to the following reasons: low flow pressure to allow healing by hemostasis and fibrosis preventing pseudoaneurysm and high mortality rate or need for immediate surgery after injury.[3] Most traumatic PAPAs are due to penetrating chest injuries among reported cases. Other non-traumatic etiology include mycotic, syphilitic or mycobacterial infection and vascular abnormalities such as cystic medial necrosis, Behcet's disease and Marfan syndrome.[4] Hemoptysis is the most common presentation due to leakage of blood into the bronchial tree by the aneurysm.[2] Other associated symptoms include chest pain, nonproductive cough and shortness of breath. Presentation ranges from few weeks to years after initial injury based on the few reported cases in the English literature. The longest latency so far is 30-years postinjury.[5,6] High clinical suspicious is required for diagnosis in patient with previous history of trauma who presents with hemoptysis; however, chest CT and/or pulmonary angiogram (gold standard) are required for diagnosis and confirmation since findings on chest radiographs are not specific.[6,7] Management depends on location, size and symptoms. Traditionally, lung resection was the main treatment; however, lung-sparing therapy such as aneurysectomy or coil embolization angiographically are gaining grounds.[1,2,3,6] Recently, fluoroscopically guided percutaneous injection of thrombin was employed in the management of angiographically inaccessible PAPA.[8] In an acute presentation, angiographical embolization is preferred because it allows for continue observation of the patient and prevents early lung resection.[9] Lesions that are not symptomatic require some form of therapy due to potential fatal rupture and subsequent exsanguinations. Similarly, most reports recommend some form of treatment despite possible spontaneous resolution for the same reason.
In this present case, a 23-year male developed traumatic pulmonary artery and vein pseudoaneurysm almost 60 days after gunshot wound to the chest. The patient was symptomatic and treatment option was very challenging due to the presence of pulmonary vein pseudoaneurysm and history of left common femoral vein DVT. Coil embolization of the artery pseudoaneurysm was performed, since this played a major role in patient's symptoms. The pulmonary vein pseudoaneurysm was very small, with low intraluminal pressures and therefore was not coil embolized [Figure 6]. Instead, IVC filter was placed due to the history of DVT and contraindication for anticoagulation. Thirty day follow-up chest CT showed successful coil embolization of the artery and resolution of the venous pseudoaneurysm. To the best of our knowledge this is the second case with both pulmonary artery and venous aneurysm after penetrating injury to the chest.
Figure 6.

Arrow indicating uncoiled pulmonary vein pseudoaneurysm
Knowledge about traumatic pulmonary artery or venous pseudoaneursym is limited due to the long latency on presentation, paucity of cases and high mortality associated with this entity. The current knowledge about traumatic pulmonary artery is from a few cases reports and our case adds to this limited database. In general, diagnosis should be suspected in any patient who presents with hemoptysis after chest trauma and a persistent organized area of consolidation on chest X-ray.[10] Chest CT and angiogram will confirm diagnosis and treatment should be initiated as soon as possible due to >50% mortality when these lesions rupture.[10] Off-note, we would like to emphasize that thoracotomy remains the current management of massive hemothorax despite our initial conservative management.
CONCLUSION
Traumatic pulmonary artery or vein pseudoaneurysms are extremely rare with only 24 cases reported in the English literature. Hemoptysis is the common complaint and can present a few weeks to years from the initial injury. Historically, formal surgical resection has been required; however, angioembolization is gaining grounds and serving as future initial option for hemorrhage control in traumatic PAPA.
DOD DISCLAIMER
The views expressed in this case report are those of the author and do not reflect the official policy of the Department of the Navy (DON), Department of Defense (DOD) or US Government. We certify that all individuals who qualify as authors have been listed; each has participated in the conception and design of this work, the writing of the document, and the approval of the submission of this version; that the document represents valid work; that if we used information derived from another source, we obtained all necessary approvals to use it and made appropriate acknowledgements in the document; and that each takes public responsibility for it.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Rai VK, Malireddy K, Dearmond D, Myers J, Dent DL. Traumatic pseudoaneurysm of the pulmonary artery. J Trauma. 2010;69:730. doi: 10.1097/TA.0b013e3181e7dfac. [DOI] [PubMed] [Google Scholar]
- 2.Feretti GR, Thony F, Link KM, Durand M, Wollschläger K, Blin D, et al. False aneurysm of the pulmonary artery induced by a swan-Ganz catheter: clinic presentation and radiologic management. AJR Am J Roentgenol. 1996;167:941–5. doi: 10.2214/ajr.167.4.8819388. [DOI] [PubMed] [Google Scholar]
- 3.Khan AA, Bauer TL, Garcia MJ, Panasuk DB, Davis AL. Angiographic embolization of a traumatic pulmonary pseudoaneurysm. Ann Thorac Surg. 2005;79:2136–8. doi: 10.1016/j.athoracsur.2003.12.067. [DOI] [PubMed] [Google Scholar]
- 4.Bartter T, Irwin RS, Nash G. Aneurysms of the pulmonary arteries. Chest. 1998;94:1065–75. doi: 10.1378/chest.94.5.1065. [DOI] [PubMed] [Google Scholar]
- 5.Gavant ML, Winer-Muram HT. Traumatic pulmonary artery pseudoaneurysm. Can Assoc Radiol J. 1986;37:108–7. [PubMed] [Google Scholar]
- 6.Savage C, Zwischenberger JB, Ventura KC, Wittich GR. Hemoptysis secondary to pulmonary pseudoaneurysm 30 years after a gunshot wound. Ann Thorac Surg. 2001;71:1021–3. doi: 10.1016/s0003-4975(00)02277-3. [DOI] [PubMed] [Google Scholar]
- 7.Hubler B, Earls JP, Stevens K. Traumatic pulmonary arterial and venous pseudoaneurysms. AJR Am J Roentgenol. 1997;169:1354. doi: 10.2214/ajr.169.5.9353457. [DOI] [PubMed] [Google Scholar]
- 8.Sridhar SK, Sadler D, McFadden SD, Ball CG, Kirkpatrick AW. Percutaneous embolization of an angiographically inaccessible pulmonary artery pseudoaneurysm after blunt chest trauma: A case report and review of literature. J Trauma. 2010;69:729. doi: 10.1097/TA.0b013e3181d0f69f. [DOI] [PubMed] [Google Scholar]
- 9.Block M, Lefkowitz T, Ravenel J, Leon S, Hannegan C. Endovascular coil embolization for acute management of traumatic pulmonary artery pseudoaneurysm. J Thorac Cardiovasc Surg. 2004;128:784–5. doi: 10.1016/j.jtcvs.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 10.Reade CC, Jenkins NL, Bard MR, Kuszyk BS, Koutlas TC, Rotondo MF. Immediate diagnosis and nonoperative treatment of pulmonary artery pseudoaneurysm after blunt traumatic injury. J Trauma. 2006;60:894–96. doi: 10.1097/01.ta.0000214598.48638.b5. [DOI] [PubMed] [Google Scholar]


