Abstract
Background and Objectives
Discrepancy between angiographic percent (%) diameter stenosis and fractional flow reserve (FFR) exists in non-left main bifurcation lesions. The aim of this study was to compare angiographic stenosis severity and FFR in jailed ostial left circumflex artery (LCX) lesions after left main (LM)-to-left anterior descending artery (LAD) crossover stenting.
Subjects and Methods
Twenty-nine (n=29) patients with distal LM or ostial LAD lesions treated by LM-to-LAD crossover stenting were consecutively enrolled. After successful stenting, FFR was measured at the jailed LCX. Additional intervention was performed in lesions with FFR <0.8.
Results
The mean reference diameter of LCX was 3.1±0.4 mm, and percent diameter stenosis after crossover stenting was 56±21%. Angiographically significant stenosis (>50%) at the ostial LCX occurred in 59% (17/29) of cases. Among them, only five (29%) lesions had functional significance, and underwent additional procedure. During follow-up, three patients in the deferral group and two patients in the additional intervention group had target lesion revascularization.
Conclusion
There was a discrepancy between angiographic percent diameter stenosis and FFR in jailed LCX lesions after LM crossover stenting.
Keywords: Coronary disease, Physiology, Stents, Angiography
Introduction
Recent studies evaluating percutaneous coronary intervention (PCI) with drug-eluting stent (DES) for left main (LM) disease have shown promising results.1),2) However, the decision to intervene the jailed left circumflex coronary artery (LCX) after an LM stent extending into the left anterior descending coronary artery (LAD) is difficult in some cases if based on angiogram alone. Previous studies suggested that measurement of fractional flow reserve (FFR) across jailed side branch lesions prevents unnecessary complex interventions in bifurcation lesions.3-5) However, the safety and efficacy of the same strategy for jailed LCX after LM-to-LAD crossover stenting when a larger amount of myocardium may be in jeopardy remains unvalidated. The aim of this study was to compare angiographic stenosis severity and FFR in jailed ostial LCX lesions after LM-to-LAD crossover stenting.
Subjects and Methods
Patient population
Patients who underwent LM-to-LAD crossover stenting and met the following criteria were prospectively enrolled from 3 centers in the Republic of Korea: 1) significant de novo coronary artery disease in distal LM or ostial LAD and, 2) reference vessel diameter of LCX over 2.5 mm by visual estimation. Patients were excluded if any one of the following conditions was present: predilation of LCx before main branch stent implantation, significant non-ostial LCx lesion, infarct-related artery or angiographically visible thrombus, primary myocardial disease, left ventricular hypertrophy, contraindications to adenosine, or intolerance to aspirin or clopidogrel. The study protocol was approved by the Institutional Review Board and all patients gave informed consent prior to study enrollment.
Study procedure
PCI was performed according to standard interventional techniques. Before the index procedure, all patients received oral aspirin (a loading dose of 200 mg) and clopidogrel (a loading dose of 300-600 mg before the procedure). Oral antiplatelet therapy during the study period followed guidelines recommending a combination of aspirin (100 mg daily; indefinitely) and clopidogrel (75 mg daily; more than 12 months). Intravenous boluses of heparin (100 U/kg) were administered before intervention and the dosage was adjusted to maintain an activated clotting time exceeding 250 seconds during the procedure.6) All coronary angiograms were analyzed using standard definitions and measurements by Quantitative Coronary Angiography (QCA; Quantcor QCA, version 4.0, Pie Medical Imaging, Maastricht, the Netherlands) by an experienced physician blinded to the FFR values.
Fractional flow reserve measurements
FFR is defined as the ratio between distal coronary pressure and aortic pressure, both measured simultaneously at maximal hyperemia. After successful insertion of LM-to-LAD crossover stenting, FFR was measured down the jailed LCX using a 0.014-inch pressure guide wire (PressureWire, Radi Medical Systems, Uppsala, Sweden). The pressure wire was passed through the struts of the stent and positioned more than 10 mm distal to the LCX ostium to assess ostial-narrowing severity. Hyperemia was induced with intracoronary bolus administration (80 µg) or intravenous continuous infusion (140 µg/kg/min) of adenosine.7) Lesions with an FFR less than 0.80 were considered to be functionally significant stenosis. In such cases, additional procedures, such as kissing balloon or provisional stenting, were performed at the physician's discretion.
Clinical events
Major adverse cardiac events were defined as a composite of death, myocardial infarction, and any repeat revascularization. Death was defined as all-cause mortality. Myocardial infarction was defined as greater than or equal to 3-fold elevation of creatine kinase-MB level, or new Q-waves in greater than or equal to 2 contiguous electrocardiogram leads. Target vessel revascularization (TVR) included target lesion revascularization and bypass surgery of the pertinent lesion. TVR was only based on the presence of symptoms and/or signs of ischemia. Stent thrombosis was defined according to the Academic Research Consortium guidelines.
Statistical analysis
Categorical variables are expressed as proportions. Continuous variables are expressed as means and standard deviations. Correlations between the FFR and percent diameter stenosis were evaluated using the Pearson correlation analysis with the Statistical Package for the Social Sciences (SPSS) statistical software, version 15.0 (SPSS, Inc., Chicago, IL, USA).
Results
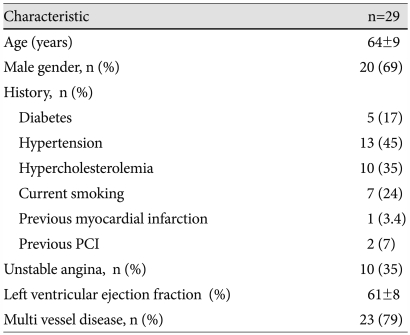
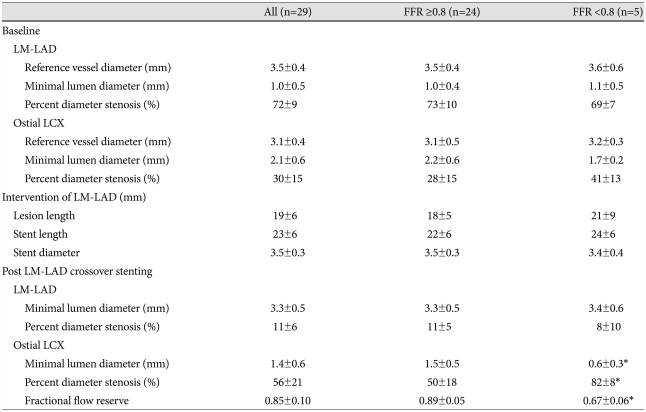
Twenty-nine (n=29) patients were enrolled in this study. The baseline characteristics and procedural results are summarized in Table 1 and 2. The mean age of the patients was 64±9 years and 69% were male. On the baseline coronary angiogram, 6 patients had distal LM disease and 23 patients had ostial LAD disease without significant distal LM disease. Intravenous adenosine was used in 7 cases (24.1%). The mean reference vessel diameter of the ostial LCX was 3.1±0.4 mm. The baseline mean percent diameter stenosis (%DS) of ostial LCX was 30±15%. After LM-to-LAD crossover stenting, mean %DS of ostial LCX was 56±21%. FFR of ostial LCX was greater than or equal to 0.80 in 24 patients (0.89±0.05), less than 0.80 in 5 patients (0.67±0.06). Among 5 patients, 3 achieved adequate results (FFR >0.90) after kissing balloon inflation, and the others by provisional T-stenting. When QCA was reanalyzed in 17 lesions with DS greater than in ostial LCX, the results were similar to that presented in Table 2. The angle between LAD and LCX was 124 degree in the FFR ≥0.8 group, and 114 degree in the FFR <0.8 group (p=0.35).
Table 1.
Patient baseline characteristics
Plus-minus values are mean±SD. PCI: percutaneous coronary intervention
Table 2.
Procedural results
Plus-minus values are means±SD. *p<0.05. FFR: fractional flow reserve, LM: left main, LAD: left anterior descending coronary artery, LCX: left circumflex coronary artery
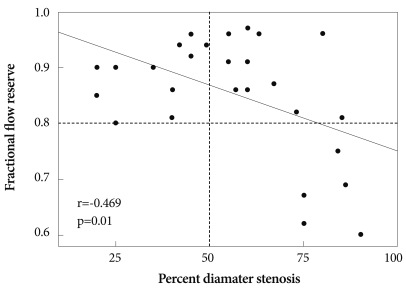
A plot of FFR as a function of %DS of the ostial LCX after stent deployment is shown in Fig. 1. Although there was a negative correlation between %DS and FFR (r=-0.469, p=0.01), no lesion with ≤50 %DS had FFR <0.80. Among 17 lesions with >50 %DS in ostial LCX, only 5 lesions (29%) were functionally significant. Even in 8 lesions with >70 %DS, 3 lesions remained functionally non-significant. The best cut-off value of %DS to predict functional significance (i.e., FFR <0.80) was 82% (sensitivity 60%, specificity 58%; area under the curve 0.958, 95% confidence interval 0.889-1.028).
Fig. 1.
Correlation between fractional flow reserve and percent diameter stenosis of ostial circumflex coronary artery after left main to left anterior descending coronary artery stenting.
Clinical follow-up was performed in all patients. Mean duration was 20±9 months (minimum 4, maximum 30). During the follow-up period, 3 patients in the deferral group underwent TLR. Two cases were related to LM-to-LAD stent restenosis, and the other was due to the progression of ostial LCX lesion. Two patients in the additional procedure group experienced adverse events (1 non-cardiac death, 1 TLR for LM-to-LAD stent restonsis). No stent thrombosis was observed in these patients.
Discussion
The major findings of the current study is that there is a discrepancy between angiographic percent diameter stenosis and FFR in jailed LCX lesions, and the FFR-guided jailed LCX PCI strategy could reduce the need for additional PCI.
Despite the emergence of DES, coronary bifurcation lesions still have a higher restenosis rate, particularly at the ostium of the side branch in comparison with simple lesions.8) It is important to assess the functional significance of jailed LCX lesions as 2 stent strategies, because LM diseases have been associated with worse outcomes than simple crossover stenting.9) Although one stent technique is preferable in this lesion type, the frequency of ostial LCX intervention after LM-to-LAD crossover stenting in this lesion type was >40% in a previous study,1) which might have been related to larger plaques and carina shifting-related wide angle in LM bifurcation lesions.
Assessment of the severity of bifurcation lesions and the performance of PCI in bifurcation remain challenging. Angiographic assessment of the severity of bifurcation lesions is hampered by the inherent limitations of angiography, such as overlap of adjacent vessels, angulation, and foreshortening of the origin of side branches.10-12) Intravascular ultrasound can provide delicate information about the anatomical change of bifurcation lesion. However, it may yield inaccurate information in this situation because of veiled ostium by stent strut. Previous studies by Koo et al.13) have demonstrated the feasibility and safety of physiological assessment with FFR of jailed side branches, and found a discrepancy between angiographic and functional evaluation of these lesions.5) We performed this study to apply the same strategy to jailed LCX lesions.
In the current study, angiographically significant stenosis (>50%) at the ostial LCX after LM-to-LAD crossover stenting occurred in 59% (17/29) of cases. Among them, only 5 (29%) patients had functionally significant obstruction of LCX by pressure wire criteria. Adequate coronary flow was preserved in 71% (12/17) patients with significant stenosis of ostial LCX after LM-to-LAD crossover stenting. Thus, the real functional state of ostial LCX can be widely different from that appears on angiography. In the clinical context, there were 3 cases of TLR in deferred lesions. Two cases were related to LM-to-LAD stent restenosis. Only 1 TLR case (4%) was developed in 24 deferred LCX lesions. There was no cardiac death, stent thrombosis or MI related to lesions in which PCI was deferred according to FFR. Unfortunately, this prospective pilot study was not powered to detect a difference in clinical outcome. With larger numbers one can anticipate that the need for revascularization of the ostial LCX after LM-to-LAD crossover stenting may be reduced, if the additional procedure is guided by FFR. However, further studies are needed to evaluate the efficacy of this strategy.
Limitations
There are several limitations to this study. First, this study included small number of patients. Second, a selection bias may have been introduced, because not all patients with distal LM or ostial LAD disease at three centers were evaluated for this study. Third, it was a non-randomized study. Because we did not compare with routine performance of additional procedures, it is difficult to confirm the benefits of our procedure. Finally, as we included only mild to moderate LCX ostial lesion with short lesion lengths, our results cannot be directly applied to more severe or diffuse lesions.
Conclusions
There was a discrepancy between angiographic percent diameter stenosis and FFR in jailed LCx lesions after LM-to-LAD stenting.
Acknowledgments
The authors thank Dr. Roberto Patarca for his editorial input.
This study was supported by a grant from the Korean Society of Circulation (2007), Republic of Korea. Dr. Yoon-Nyun Kim declares receipt of research grant No. RTI04-01-01 from the Regional Technology Innovation Program of the Ministry of Knowledge Economy (MKE), the Republic of Korea.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Kim YH, Park SW, Hong MK, et al. Comparison of simple and complex stenting techniques in the treatment of unprotected left main coronary artery bifurcation stenosis. Am J Cardiol. 2006;97:1597–1601. doi: 10.1016/j.amjcard.2005.12.051. [DOI] [PubMed] [Google Scholar]
- 2.Kim W, Kim YJ, Lee WJ, et al. Lesion location: its impacts on the procedural and postprocedural outcomes of unprotected left main coronary stenting. Korean Circ J. 2007;37:419–424. [Google Scholar]
- 3.Lim MJ, Kern MJ. Utility of coronary physiologic hemodynamics for bifurcation, aortoostial, and ostial branch stenoses to guide treatment decisions. Catheter Cardiovasc Interv. 2005;65:461–468. doi: 10.1002/ccd.20435. [DOI] [PubMed] [Google Scholar]
- 4.Koo BK, Kang HJ, Youn TJ, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633–637. doi: 10.1016/j.jacc.2005.04.054. [DOI] [PubMed] [Google Scholar]
- 5.Bellenger NG, Swallow R, Wald DS, et al. Haemodynamic significance of ostial side branch nipping following percutaneous intervention at bifurcations: a pressure wire pilot study. Heart. 2007;93:249–250. doi: 10.1136/hrt.2006.088690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jr, et al. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008;117:261–295. doi: 10.1161/CIRCULATIONAHA.107.188208. [DOI] [PubMed] [Google Scholar]
- 7.Suh JW, Koo BK, Jo SH, et al. Optimal dosage and method of administration of adenosine for measuring the coronary flow reserve and the fractional flow reserve in Koreans. Korean Circ J. 2006;36:300–307. [Google Scholar]
- 8.Colombo A, Moses JW, Morice MC, et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004;109:1244–1249. doi: 10.1161/01.CIR.0000118474.71662.E3. [DOI] [PubMed] [Google Scholar]
- 9.Toyofuku M, Kimura T, Morimoto T, et al. Three-year outcomes after sirolimus-eluting stent implantation for unprotected left main coronary artery disease: insights from the j-Cypher registry. Circulation. 2009;120:1866–1874. doi: 10.1161/CIRCULATIONAHA.109.873349. [DOI] [PubMed] [Google Scholar]
- 10.White CW, Wright CB, Doty DB, et al. Does visual interpretation of the coronary angiogram predict the physiologic importance of a coronary stenosis. N Engl J Med. 1984;310:819–824. doi: 10.1056/NEJM198403293101304. [DOI] [PubMed] [Google Scholar]
- 11.Marcus ML, Skorton DJ, Johnson MR, Collins SM, Harrison DG, Kerter RE. Visual estimate of percent diameter coronary stenosis: a battered gold standard. J Am Coll Cardiol. 1988;11:882–885. doi: 10.1016/0735-1097(88)90226-4. [DOI] [PubMed] [Google Scholar]
- 12.Ziaee A, Parham WA, Herrmann SC, Stewart RE, Lim MJ, Kern MJ. Lack of relation between imaging and physiology in ostial coronary artery narrowings. Am J Cardiol. 2004;93:1404–1407. doi: 10.1016/j.amjcard.2004.02.041. [DOI] [PubMed] [Google Scholar]
- 13.Koo BK, Park KW, Kang HJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29:726–732. doi: 10.1093/eurheartj/ehn045. [DOI] [PubMed] [Google Scholar]