Abstract
Objectives.
This study examined the joint protective contribution of psychosocial and behavioral factors to cognitive functioning and 10-year change, beyond the influence of sociodemographic factors, physical risk factors, health status, and engagement in cognitive activities.
Methods.
Participants were from the National Study of Midlife in the United States (MIDUS), ages 32–84 at Time 2, and a subsample, the Boston Longitudinal Study (BOLOS), ages 34–84 at Time 2. We computed a composite protective measure including control beliefs, quality of social support, and physical exercise variables at two occasions, 9–10 years apart. Cognition was assessed at Time 2 in MIDUS and at both occasions in BOLOS. Multiple regressions were used for analysis.
Results.
In MIDUS, the more of the protective factors, the better the cognitive performance, and the protective composite moderated education differences in memory. In BOLOS, the Time 1 composite predicted change in reasoning abilities, with a greater protective effect for those with lower education.
Discussion.
A combination of modifiable psychosocial and behavioral factors has both concurrent and long-term protective effects on cognition in adulthood. The results are promising in that educational disparities in memory and reasoning were reduced, suggesting possible interventions to protect against cognitive declines.
Keywords: Aging, Cognition, Control beliefs, Health, Physical exercise, Social support
ALTHOUGH there is evidence for average declines in cognition with aging, there is wide variability in the nature and extent of these changes (Hofer & Alwin, 2008). A large number of theoretical models and empirical evidence from cross-sectional, longitudinal, and intervention studies suggest the potential of behaviors and beliefs to enhance cognitive functioning (for a review, see Hertzog, Kramer, Wilson, & Lindenberger, 2008). The consensus is that cognitive performance can be optimized and maintained by modifiable lifestyle factors and engagement in health-promoting or protective behaviors (Yaffe et al., 2009). Previous studies (e.g., Lachman, Agrigoroaei, Murphy, & Tun, 2010; Small & McEvoy, 2008) have shown that engaging in frequent cognitive activities is associated with superior cognitive performance. Three other modifiable psychosocial and behavioral factors are consistently found to show positive associations with cognition: control beliefs, quality of social support, and physical exercise. Although their individual benefits have been shown in past work, they have not been studied together, in an additive approach, or considered in the context of physical health or physical risk factors such as being overweight, smoking, having alcohol, or drug problems, in a national sample of adults with a wide age range. Thus, the goal of the present study was to examine the combined contribution of psychological, social, and physical factors to cognitive functioning and change and to consider their possible protective effects beyond the role of sociodemographic variables, the well-established risk factors, and cognitive activities.
Between-person Heterogeneity in Cognition
There is widespread evidence for age differences in cognitive abilities (Salthouse, 2009). Within age groups, interindividual differences have traditionally been explained by sociodemographic inequalities such as level of educational attainment (Alley, Suthers, & Crimmins, 2007). Another explanatory factor, that is becoming more and more visible in the theoretical and empirical models of cognitive decline, is physical health. The conjoint trajectories of health and cognition are complex (Spiro & Brady, 2008). There is evidence that physical health and cognitive functioning are interdependent, in the sense that they share common variance and underlying etiologies. Beside the role of physical health level, those adults with health risk factors such as being overweight (Nilsson & Nilsson, 2009), smoking (Anstey, von Sanden, Salim, & O’Kearney, 2007), and having alcohol problems (Lopes, Furtado, Ferrioli, Litvoc, & de Campos Bottino, 2010) are more likely to have poor cognitive performance. In addition, there is increasing evidence that modifiable psychological, social, and physical behavioral factors including a sense of control, quality of social support, and physical exercise are associated with improved cognitive performance (Colcombe & Kramer, 2003; Miller & Lachman, 2000; Seeman, Lusignolo, Albert, & Berkman, 2001).
The contribution of control beliefs
According to a variety of studies, one central ingredient for good cognitive performance is control beliefs (Bielak et al., 2007; Caplan & Schooler, 2003; Lachman, 2006; Miller & Lachman, 2000). Control beliefs involve the perception that one can influence what happens in one's life and to what extent one's actions can bring about desired outcomes, such as good cognitive functioning. It includes beliefs or expectations about one's abilities and perceptions about external constraints (Lachman, 2006). A lowered sense of control may have affective, behavioral, motivational, and physiological effects, including greater levels of stress and anxiety (Kirschbaum et al., 1995), lower levels of effort, persistence, and strategy use (Hertzog, McGuire, & Lineweaver, 1998; Lachman & Andreoletti, 2006), as well as less frequent engagement in memory tasks (West & Yassuda, 2004), which can impact cognitive performance. Although much of the work has been cross-sectional and correlational, there is longitudinal evidence that those who have higher control beliefs improve more on cognitive tests with practice and also are less likely to show aging-related declines in cognitive functioning over time (Caplan & Schooler, 2003).
The contribution of social support
Social interactions involve a combination of supportive and stressful experiences. There is ample evidence that social exchanges, broadly defined, are related to cognitive functioning (Béland, Zunzunegui, Alvarado, Otero, & del Ser, 2005; Seeman et al., 2001). With respect to support from others, some have shown that emotional support, but not instrumental support, is positively related to better overall cognitive performance (Seeman et al., 2001). Among the explanatory mechanisms that have been considered, physiological factors such as stress hormones, immune functioning, and inflammatory processes affect the central nervous system and may be exacerbated for those with lower social support (Berkman, Glass, Brissette, & Seeman, 2000).
The contribution of physical exercise
The benefits of physical exercise for cognitive outcomes are widely documented (Colcombe & Kramer, 2003; Jedrziewski, Lee, & Trojanowski, 2007). As shown by interventions and epidemiologic studies, those who engage in regular exercise are more likely to perform better on cognitive tasks such as memory (Lachman, Neupert, Bertrand, & Jette, 2006), executive functioning (Kramer et al., 1999), and speed of processing (Dik, Deeg, Visser, & Jonker, 2003). Studies have suggested that the effects of exercise are most pronounced for executive functioning (Colcombe & Kramer, 2003; Hall, Smith, & Keele, 2001). With respect to long-term effects of physical activities, some results showed that engaging in exercise between the ages of 15 and 25 can lead to better cognition in old age (Dik et al., 2003). Possible mechanisms linking exercise and cognitive health include increased levels of oxygenation (Hertzog et al., 2008). Also, work on brain changes has revealed an increase in neuromuscular activity and cerebral blood flow (Rogers, Meyer, & Mortel, 1990) and the release of neurotrophins and catecholamines (McMorris, Collard, Corbett, Dicks, & Swain, 2008) as processes associated with physical activity that are also beneficial for cognition.
The combined effects of psychosocial and behavioral factors
Previous studies on predictors of cognitive functioning focus on the independent contributions of key factors. More recently, there has been an emphasis on the cumulative effects of multiple sources. For example, Sabia et al. (2009) showed that the total number of unhealthy risk behaviors in which one person engages, such as smoking, heavy drinking, unhealthy nutrition, and lack of physical activity, was associated with low cognitive performance in later life. The procedure of aggregating different sources of influence is consistent with studies from the medical literature suggesting that health-related lifestyle factors are not randomly distributed in the general population, but that they tend to occur in combination with each other within individuals (Poortiga, 2007). By analogy, one can think about the personal cardiovascular risk index or about allostatic load (Seeman et al., 2004) that comprise several health indicators and predict disease better than individual markers. We believe that developing a meaningful summary score of psychosocial and behavioral domains on which respondents had an adaptive level is theoretically and empirically interesting. Of interest is whether there is additive value for engaging in multiple adaptive behaviors by considering an index of protective factors. Only a modest literature has addressed the relationship between multiple protective psychosocial and behavioral factors and cognition (e.g., Albert et al., 1995; Newson & Kemps, 2006; Sturman et al., 2005), and we know of no studies showing their combined effects. One related study (Karp et al., 2006) considered the combined mental, physical, and social components embodied simultaneously in leisure activities and linked them to the risk for dementia. The most beneficial effects were obtained for those with higher scores in all three or in two of the components. Our study represents a similar approach with a focus on individual differences in normal cognitive functioning for a middle-aged and older sample. Compared with the previous work, largely focused on the positive association between engagement in mentally stimulating activities and cognition (e.g., Hertzog, 2009; Lachman et al., 2010), the current study considered the role of “noncognitive” behaviors and psychosocial factors. We analyzed frequent engagement in vigorous physical activities in combination with high control beliefs and quality of social support as protective factors for cognitive performance and change.
The current study
The present study used data from the Midlife in the United States (MIDUS; Brim, Ryff, & Kessler, 2004) national longitudinal survey conducted in 1995–1996 and 2004–2005 and a subsample, the Boston Longitudinal Study (BOLOS). The BOLOS measurements were taken approximately one year after each of the MIDUS measurements. MIDUS was designed to investigate the role of behavioral, social, psychological, biological, and neurological factors in understanding physical and mental health as people age. Thus, it has the benefit of data on a diverse population in terms of sociodemographic profiles and levels of physical health and cognitive functioning. The general goal of the present study was to analyze whether a protective composite comprising a strong sense of control over life outcomes, high quality of social relationships with partners, friends and family, and frequent vigorous physical exercise is associated with better cognitive performance in MIDUS and maintaining better cognitive functioning over a 10-year period in BOLOS. We expected a main effect of this aggregate over and above the role of sociodemographic variables, physical risk factors, health status, and frequency of engagement in cognitive activities.
At MIDUS Time 2, when our variables of interest were measured cross-sectionally, we hypothesized that the more of the psychosocial and behavioral factors present, the better the cognitive performance. Also, we analyzed if the magnitude of the combined effect of the factors on cognitive functioning would vary for the older adults and those with lower education (i.e., those considered at higher risk for poor cognitive performance). We then examined to what extent changes in the number of protective factors from Time 1 to Time 2 were associated with better cognition at Time 2.
The BOLOS study allowed us to take a first look at individual differences in cognitive decline. We predicted that the protective composite at Time 1 would account for variations in change between the two waves of the BOLOS study. We also tested if change in the number of factors over time predicted change in cognition and whether the protective composite led to better levels of cognitive maintenance in older people and respondents with lower education, those considered most vulnerable to declines.
METHODS
Participants
A national probability sample (N = 4,238) of noninstitutionalized adults from the 48 contiguous states was selected using random-digit dialing (RDD) of telephone numbers with age and gender information about the household composition, with an overall response rate of 70% for the telephone interview (Brim et al., 2004). The study also included siblings (N = 949) of the main respondents, randomly selected from the RDD sample, as well as a subpopulation of twins (N = 1,913) obtained after screening a representative national sample of approximately 50,000 households. At Time 1 (N = 7,100), participants ranged in age from 24 to 75 years (M = 46.40, SD = 13.00). At Time 2, the longitudinal retention rate, adjusted for mortality, was 75% (N = 4,955), with age ranging from 32 to 84 years (M = 55.45, SD = 12.44). As is typically found, those who participated at the second wave showed positive selection on most variables (Table 1), compared with those who dropped out of the study.
Table 1.
Comparison Between the Longitudinal Participants and the Dropouts in Midlife in the United States Study
| Variable (Time 1) | Longitudinal (N = 4,955) | Dropouts (N = 2,145) | p Value |
| Age, mean (SD) in years | 46.48 (12.50) | 46.21 (14.10) | .457 |
| Women, % | 53.3 | 47.8 | <.001 |
| Education, mean (SD) in years | 14.02 (2.60) | 13.13 (2.60) | <.001 |
| Non-Hispanic White, % | 93.0 | 84.0 | <.001 |
| Waist circumference, mean (SD) in inches | 35.33 (5.75) | 35.63 (5.79) | .082 |
| Do smoke, % | 19.6 | 30.6 | <.001 |
| Do have alcohol or drug problems, % | 2.2 | 3.6 | .002 |
| Health status, mean (SD) | 0.26 (0.53) | 0.33 (0.64) | <.001 |
| Control beliefs, mean (SD) | 5.54 (1.00) | 5.38 (1.09) | <.001 |
| Quality of social support, mean (SD) | 3.18 (0.37) | 3.13 (0.43) | <.001 |
| Physical exercise, mean (SD) | 3.20 (1.69) | 2.96 (1.81) | <.001 |
Note: p values for means are derived from independent samples t-tests; p values for percentages are derived from χ2 tests.
Approximately 12 months after MIDUS Time 1, 302 MIDUS participants, ranging in age from 24 to 74 years (M = 47.89, SD = 13.74), who were from an oversample drawn in the Boston area, were successfully recruited to participate in BOLOS. Within one year of completion of the MIDUS Time 2, 222 people from BOLOS were located; 180 of them were recontacted (81% contact rate) and 151 (68%) participated. Their ages at Time 2 ranged from 34 to 84 years (M = 59.99, SD = 12.81). Compared with those who did not participate in BOLOS Time 2, longitudinal participants from the Boston area were more educated—M = 15.13 vs. M = 14.24, t(300) = –2.77, p = .006. However, they did not differ in terms of age, M = 49.21 vs. M = 46.57, t(300) = –1.68, p = .095, self-rated physical health, M = 7.50 vs. M = 7.24, t(300) = –1.32, p = .188, or sex distribution, women: 43.7% vs. 38.4%, χ2(1) = .88, p = .349.
Measures
Cognition.—
Cognitive measures were collected by telephone at Time 2 in MIDUS and at Time 1 and Time 2 in person for BOLOS.
MIDUS cognitive battery.
In MIDUS, seven cognitive dimensions were tested using the Brief Test of Adult Cognition by Telephone (Lachman & Tun, 2008; Tun & Lachman, 2008). This included two measures of episodic memory (immediate and delayed free recall of 15 words), working memory span (backward digit span—the highest span achieved in repeating strings of digits in reverse order), verbal fluency (the number of words produced from the category of animals in 60 s), inductive reasoning (completing a pattern in a series of 5 numbers), processing speed (the number of digits produced by counting backward from 100 in 30 s), and attention switching and inhibitory control (the Stop and Go Switch Task; Tun & Lachman, 2008). For the latter task, reaction times were calculated with the mean of switch and nonswitch trial latencies on a task requiring alternating between the “normal” condition (i.e., respond “Go” to the stimulus “Green” and “Stop” to the stimulus “Red”) and the “reverse” condition (i.e., respond “Stop” to the stimulus “Green” and “Go” to the stimulus “Red”). Latencies were multiplied by (–1), so higher scores would correspond to faster reaction times. Following exploratory and confirmatory factor analysis (Lachman et al., 2010), two intercorrelated, r(4027) = .43, p < .001, cognitive factors were computed—episodic memory (immediate and delayed word recall) and executive functioning (all other measures). The two cognitive factor scores were computed as standardized means of the z-scored measures loading on the factors.
BOLOS cognitive battery.
As shown by the confirmatory factor analysis in Miller & Lachman (2000), tasks at BOLOS Time 1 formed a four-factor model: short-term memory, speed of processing, reasoning, and vocabulary. The memory factor was comprised of forward and backward digit span (participants were read a string of numbers and were asked to recall them in a forward and backward order, respectively) and Serial 7’s (participants were asked to count backwards by sevens from a given starting number; Folstein, Folstein, & McHugh, 1975). The speed factor contained letter comparison (participants judged two rows of letters to be the same or different; Salthouse, Kausler, & Saults, 1990) and digit symbol substitution (participants were given a series of blank boxes with symbols above them and had to fill in numbers corresponding to the symbols as indicated by a provided legend; Wechsler, 1997). The reasoning factor, which captured visuospatial reasoning and fluid intelligence, combined letter series—inductive reasoning (participants detected patterns in series of letters by determining the letter that would logically follow; Schaie, 1985) and Ravens Advanced Progressive Matrices—figural relations (Raven, Raven, & Court, 1991). Vocabulary was measured using the Wechsler Adult Intelligence Scale vocabulary task (participants were given a word to define and received points based on the completeness and accuracy of their response; Wechsler, 1997). To compute each factor, first, a z-score of each measure was taken, and then the mean of these z-scores was standardized. The Time 2 cognitive factors and measures were standardized using the means and SDs from Time 1.
Frequency of engaging in cognitive activities.—
The cognitive activity variable (see Lachman et al., 2010) was created by averaging the self-reported frequencies on a 6-point scale (1 = never to 6 = daily) of engaging in four cognitive activities: reading books, magazines, or newspapers; doing word games such as crossword, puzzles, or scrabble; attending educational lectures or courses; and writing (e.g., letters, journal entries).
Psychosocial and behavioral factors.—
Control beliefs.
Perceived control over outcomes in life was assessed with a 12-item composite (Cronbach's α Time 1 = .85; Time 2 = .87), computed by averaging scores on two subscales from the MIDUS sense of control scale (Lachman & Weaver, 1998), namely personal mastery (e.g., I can do just about anything I really set my mind to) and perceived constraints (e.g., What happens in my life is often beyond my control). The scores range from 1 (strongly agree) to 7 (strongly disagree) and were reverse coded for personal mastery. A higher value indicates higher sense of control.
Quality of social support.
We included items reflecting social support and reverse coded items reflecting social strain for close relationships. This measure (Cronbach's α Time 1 = .87; Time 2 = .88) was the average of the ratings on 12 items assessing socioemotional aspects of social support (e.g., How much do members of your family really care about you?) and 12 items assessing social strain (e.g., How often do members of your family make too many demands on you?) the participants experienced in their relationships with family, friends, and spouse/partner (Lachman, Röcke, Rosnick, & Ryff, 2008; Walen & Lachman, 2000). The scores range from 1 (never) to 4 (often), with a higher value indicating greater quality of social support.
Physical exercise.
At Time 1, participants reported the frequency of engaging in vigorous physical activities (e.g., running or lifting heavy objects) to work up a sweat, during the summer months and the winter months (Cotter & Lachman, 2010). The physical exercise score was the mean of summer and winter ratings, which range from 1 (never) to 6 (several times a week or more). At Time 2, six questions assessing the participant's frequency of vigorous physical activities were used. These six questions referred to frequency of physical activities during the summer and the winter months, in three different settings (i.e., home, work, and leisure), with ratings from 1 (never) to 6 (several times a week). We computed the mean of the summer and winter ratings for all three settings and used the highest of these scores as the physical exercise score. At both occasions, a higher score indicates more frequent physical exercise.
Psychosocial and behavioral protective composite.
We assigned the participants a score of 0 (below the median) or 1 (equal to or above the median) for each psychosocial and behavioral factor: control beliefs (MIDUS Median Time 1 = 5.67; Time 2 = 5.67), quality of social support (MIDUS Median Time 1 = 3.21; Time 2 = 3.29), and physical exercise (MIDUS Median Time 1 = 4.50; Time 2 = 4); in BOLOS, the medians were 5.83 (Time 1) and 5.75 (Time 2) for control beliefs, 3.19 (Time 1) and 3.25 (Time 2) for quality of social support, 4.5 (Time 1) and 4 (Time 2) for physical exercise. At each occasion of measurement, one behavioral composite was obtained by summing the assigned scores, for the participants with available data on all protective factors. The decision to create the composite using an unweighted sum is based on previous work on accumulated risk (e.g., allostatic load, Gruenewald, Seeman, Karlamangla, & Sarkisian, 2009). Also, it allows a parsimonious measure that is invariant across all our dependent variables. The computed variables ranged from 0 to 3, with the higher values indicating a greater number of factors at the higher level. The distributions for each time point as well as for change over time are presented in Supplementary Tables 5–7 (in MIDUS, 20.9% of the participants increased their protective composite by one factor, 5.1% by two, and .5% by three; in BOLOS, the corresponding percentages were 30.4%, 5.2%, and 1.5%, respectively.
Sociodemographic variables.—
We examined age, sex (–1 = men, 1 = women), level of education in years (ranging from 6 to 20 years), and self-assessed race (–1 = non-Hispanic White, 1 = all others).
Physical Risk Factors
Waist circumference.—
The circumference of the waist, a reliable indicator of obesity (Chen & Guo, 2008), was measured in inches at the level of the navel and reported by the participant at both times in MIDUS. For the data analysis, this variable was standardized separately for men (Time 1: M = 37.55, SD = 4.40; Time 2: M = 39.46, SD = 4.91) and women (Time 1: M = 33.17, SD = 5.53; Time 2: M = 35.45, SD = 6.06).
Smoking.
At both occasions in MIDUS, participants were asked if they currently smoke cigarettes regularly (–1 = no, 1 = yes).
Alcohol or drug problems.
Participants reported if they have experienced or have been treated for alcohol or drug problems during the past 12 months, at MIDUS Time 1 and Time 2 (–1 = no, 1 = yes).
Health status.—
This measure taken at Time 1 assessed how many of the following conditions the participants reported ever having: diabetes; stroke; lupus; human immunodeficiency virus/acquired immunodeficiency syndrome; multiple sclerosis, epilepsy or other neurological disorders; cancer; or heart trouble (e.g., heart attack). Participants were assigned a score of 1 for any of the chronic conditions. The final score could range from 0 to 7.
Statistical Analysis
For the MIDUS analyses, we used all the available data. However, we removed the 151 BOLOS participants from the MIDUS analyses, to avoid redundancy. We used hierarchical multiple regression models to examine the effects of the protective composite on episodic memory and executive functioning over and above the role of sociodemographic variables, physical risk factors, health status, and cognitive activities (Step 2), and whether the age and education differences in cognition can be moderated by the number of behavioral factors (Step 3). In order to explore how change in the number of protective factors over time affected cognitive performance, we used as concurrent predictors the Time 1 protective composite and the difference between the two occasions (Time 2 level – Time 1 level). All regression models adjusted for the effects of sociodemographic variables, the physical risk factors, health status, and engagement in cognitive activities which were all measured at Time 2. As our sample also included siblings of the main respondents and a subpopulation of twins, we also ran models using the cluster option in STATA (StataCorp, 2009). This model takes dependencies into account using robust standard errors by clustering at the family level (see Supplementary Tables 8 and 9).
For the BOLOS analyses, we used all available data from the 151 longitudinal participants. The measures of the protective factors and all the covariates came from MIDUS variables, and cognitive performance was assessed in BOLOS within 12 months after the MIDUS Time 1 and Time 2 interviews. In order to look at predictors of change in cognition, we regressed the cognitive factor from Time 2 on the same factor measured at Time 1 and entered sociodemographic variables, physical risk factors, health status, and the protective composite from Time 1 (Cohen, Cohen, West, & Aiken, 2003). At the last step, we entered the interaction terms with education and age, in order to explore if the association between the protective composite and cognitive change varied by age or educational attainment. Moreover, a separate regression model tested whether change between Time 1 and Time 2 in the protective composite accounted for cognitive change in BOLOS, following the same procedure as for MIDUS. For correlations of all variables, see Supplementary Tables 10 and 11.
RESULTS
MIDUS
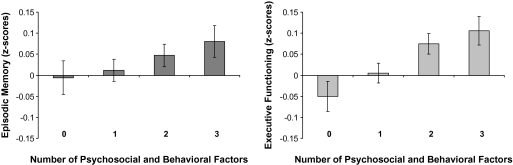
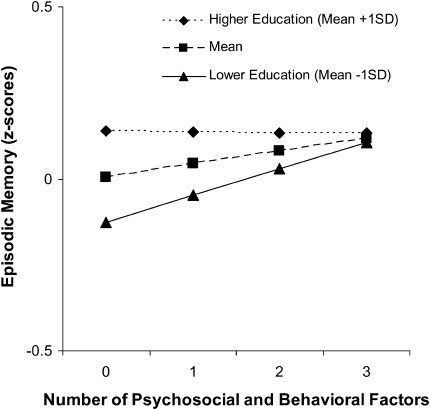
The results from the multiple regression models indicate sociodemographic differences in cognitive performance. In the first step of the regression model, advanced age was negatively associated with episodic memory—Table 2; β = –.33, t(3366) = –19.90, p < .001—and executive functioning—Table 3; β = .40, t(3375) = –26.61, p < .001. Also, a positive association was obtained between the level of formal education and cognition—memory: β = .13, t(3366) = 8.10, p < .001; executive functioning: β = .27, t(3375) = 18.23, p < .001. Thus, our results are consistent with previous research defining older adults and those with low education as groups most at risk for poor cognitive performance. Sociodemographic variables along with physical risk factors, health status, and engagement in cognitive activities accounted for a significant percent of variance in memory, R2 = .230, F(9, 3366) = 111.66, p < .001, and executive functioning, R2 = .364, F(9, 3375) = 214.68, p < .001. However, in line with our predictions, over and above the role of these covariates, the number of behavioral protective factors was positively associated with memory, β = .03, t(3365) = 2.15, p = .032, and executive functioning, β = .06, t(3374) = 3.88, p < .001, and added a significant percent of explained variance—R2 change = .001, F change (1, 3365) = 4.63, p = .032; R2 change = .003, F change (1, 3374) = 15.08, p < .001, respectively. The more protective domains people are engaged in, the better their cognitive performance (Figure 1), and the protective composite was equally beneficial across the board for people of all ages. The results revealed that the association between education and cognition was significantly reduced by the number of protective factors (Figure 2), but only for episodic memory—β = –.04, t(3363) = –2.43, p = .015. The memory scores of people with fewer years of formal education who engaged in three protective behaviors were more comparable to those of respondents with higher education. Finally, cognitive performance was significantly associated with increases in the number of protective factors between the two waves of MIDUS. While controlling for the Time 1 composite and all other covariates at Time 2, increasing the number of protective factors was significantly related to better executive functioning—β = .03, t(3373) = 2.10, p = .036. Over and above the psychosocial and behavioral profile at Time 1, engaging in more protective behaviors over time was related to higher Time 2 executive functioning (in MIDUS, among all participants who increased by one, two, or three factors, 35.96% increased in social support, 40.16% increased in control beliefs, and 50.51% increased in physical exercise; in BOLOS, the corresponding percentages were 40%, 36%, and 48%, respectively). However, positive changes in the protective composite were not significantly related to better episodic memory beyond the effects of the Time 1 composite—β = .01, t(3364) = .38, p = .706.
Table 2.
Hierarchical Multiple Regression With Episodic Memory as the Dependent Variable (Midlife in the United States Study)
| Step 1 |
Step 2 |
Step 3 |
||||
| Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | |
| Age | –.03 (–.33)** | .001 | –.03 (–.33)** | .001 | –.03 (–.33)** | .001 |
| Sex | .44 (.22)** | .031 | .44 (.22)** | .031 | .44 (.22)** | .031 |
| Education | .05 (.13)** | .006 | .05 (.13)** | .006 | .05 (.13)** | .006 |
| Race | –.12 (–.07)** | .026 | –.12 (–.07)** | .026 | –.12 (–.07)** | .026 |
| Waist circumference | –.04 (–.04)* | .016 | –.04 (–.04)* | .016 | –.04 (–.04)* | .016 |
| Smoking | .01 (.01) | .021 | .01 (.01) | .021 | .01 (.01) | .021 |
| Alcohol or drug problems | –.05 (–.01) | .073 | –.04 (–.01) | .073 | –.04 (–.01) | .073 |
| Health status | –.04 (–.03) | .024 | –.03 (–.02) | .024 | –.03 (–.02) | .024 |
| Cognitive activity | .17 (.15)** | .018 | .16 (.14)** | .019 | .16 (.14)** | .019 |
| Protective composite | .04 (.03)* | .017 | .04 (.04)* | .017 | ||
| Protective composite × age | .00 (–.01) | .001 | ||||
| Protective composite × education | –.02 (–.04)* | .006 | ||||
Notes: Step 1: R2 = .230, F(9, 3366) = 111.66, p < .001; Step 2: R2 change = .001, F change (1, 3365) = 4.63, p = .032; Step 3: R2 change = .001, F change (2, 3363) = 2.94, p = .053. The outcome and all the predictors were measured at Time 2. Age, education, and the protective composite score were centered to the mean.
*p < .05; **p < .001.
Table 3.
Hierarchical Multiple Regression With Executive Functioning as the Dependent Variable (Midlife in the United States Study)
| Step 1 |
Step 2 |
Step 3 |
||||
| Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | |
| Age | –.03 (–.40)*** | .001 | –.03 (–.40)*** | .001 | –.03 (–.40)*** | .001 |
| Sex | –.21 (–.10)*** | .028 | –.20 (–.10)*** | .028 | –.20 (–.10)*** | .028 |
| Education | .10 (.27)*** | .006 | .10 (.27)*** | .006 | .10 (.27)*** | .006 |
| Race | –.21 (–.12)*** | .024 | –.20 (–.12)*** | .024 | –.20 (–.12)*** | .024 |
| Waist circumference | –.05 (–.05)** | .014 | –.04 (–.04)** | .014 | –.04 (–.04)** | .014 |
| Smoking | –.05 (–.04)* | .019 | –.05 (–.03)* | .019 | –.05 (–.03)* | .019 |
| Alcohol or drug problems | –.01 (.00) | .066 | –.01(.00) | .066 | .00 (.00) | .066 |
| Health status | –.07 (–.05)** | .021 | –.07 (–.05)** | .021 | –.07 (–.05)** | .021 |
| Cognitive activity | .19 (.17)*** | .017 | .18 (.16)*** | .017 | .18 (.16)*** | .017 |
| Protective composite | .06 (.06)*** | .015 | .06 (.06)*** | .015 | ||
| Protective composite × age | .00 (–.03) | .001 | ||||
| Protective composite × education | .00 (.00) | .006 | ||||
Notes: Step 1: R2 = .364, F(9, 3375) = 214.68, p < .001; Step 2: R2 change = .003, F change (1, 3374) = 15.08, p < .001; Step 3: R2 change = .001, F change (2, 3372) = 1.79, p = .167. The outcome and all the predictors were measured at Time 2. Age, education, and the protective composite score were centered to the mean.
*p < .05; **p < .01; ***p < .001.
Figure 1.
The estimated means of episodic memory (left panel) and executive functioning (right panel) as a function of the number of psychosocial and behavioral factors, while adjusting for sociodemographics, physical risk factors, health status, and cognitive activities.
Figure 2.
The predicted values for episodic memory by education and number of psychosocial and behavioral factors, while adjusting for sociodemographics, physical risk factors, health status, and cognitive activities; education: M years = 14.15 (approximately some college), SD = 2.64; M –1SD = approximately high school or less; M + 1SD = approximately a bachelor's degree or higher.
BOLOS
This subsample of MIDUS allowed us to look at change in cognitive functioning and analyze cognitive decline in relation to the number of protective factors. For the four cognitive factors, there were significant mean differences over time for short-term memory, speed of processing, and reasoning—stability coefficients and mean differences between Time 1 and Time 2: short-term memory r(144) = .72, p < .001; t(145) = 2.30, p = .023 (Time 1: M = 0, SD = 1; Time 2: M = –0.12, SD = 1); speed r(139) = .78, p < .001; t(140) = 2.90, p = .004 (Time 1: M = 0, SD = 1; Time 2: M = –0.20, SD = 1.27); reasoning r(138) = .84, p < .001; t(139) = 4.42, p < .001 (Time 1: M = 0; SD = 1; Time 2: M = –0.23; SD = 1.05); and vocabulary r(142) = .84, p < .001; t(143) = .51, p = .612 (Time 1: M = 0, SD = 1; Time 2: M = –0.03, SD = .82); for each set of analysis, the maximum number of longitudinal participants was used. There was considerable cross-occasion stability in all factors. Individual differences in change in short-term memory and reasoning were significantly associated with age. However, the Time 1 protective composite was positively associated with change only for reasoning (Table 4), beyond the role of sociodemographic variables, physical risk factors, and health status, β = .10, t(126) = 2.02, p = .045. Moreover, when the interaction terms between the protective composite and age and education were entered in the model, the number of factors reduced the association between level of education and reasoning abilities, β = –.09, t(124) = –2.03, p = .045. Regarding the effects of change in the protective composite between Time 1 and Time 2, increasing the number of protective factors did not lead to better maintenance of reasoning abilities over and above the Time 1 factors, β = –.01, t(117) = –.23, p = .823.
Table 4.
Hierarchical Multiple Regression With Reasoning at Time 2 as the Dependent Variable (Boston Longitudinal Study)
| Step 1 |
Step 2 |
Step 3 |
||||
| Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | Unstandardized (standardized) parameter estimate | SE | |
| Reasoning Time 1 | .73 (.69)*** | .059 | .74 (.70)*** | .058 | .74 (.70)*** | .058 |
| Age | –.02 (–.23)*** | .004 | –.02 (–.22)** | .004 | –.02 (–.22)** | .004 |
| Sex | –.04 (–.02) | .096 | .00 (.00) | .097 | –.02 (–.01) | .096 |
| Education | .03 (.08) | .020 | .03 (.06) | .020 | .02 (.04) | .021 |
| Race | –.15 (–.06) | .114 | –.11 (–.05) | .114 | –.09 (–.04) | .113 |
| Waist circumference | –.04 (–.03) | .051 | –.04 (–.04) | .050 | –.05 (–.04) | .050 |
| Smoking | .01 (.01) | .069 | .01 (.01) | .068 | .01 (.01) | .068 |
| Alcohol or drug problems | .05 (.02) | .147 | .06 (.02) | .145 | .05 (.01) | .145 |
| Health status | .01 (.01) | .083 | .03 (.02) | .082 | .02 (.01) | .082 |
| Protective composite | .10 (.10)* | .051 | .09 (.08) | .051 | ||
| Protective composite × age | .00 (–.02) | .004 | ||||
| Protective composite × education | –.04 (–.09)* | .018 | ||||
Notes: Step 1: R2 = .752, F(9, 127) = 42.85, p < .001; Step 2: R2 change = .008, F change (1, 126) = 4.10, p = .045; Step 3: R2 change = .008, F change (2, 124) = 2.15, p = .121. The outcome and all the predictors were measured at Time 2. Age, education, and the protective composite score were centered to the mean. The model did not adjust for cognitive activities because this was measured at Time 2, only.
*p < .05; **p < .01; ***p < .001.
DISCUSSION
The present study revealed that a composite index of the number of adaptive psychosocial and behavioral factors was positively related to cognitive performance (episodic memory and executive functioning) and change (reasoning abilities), over and above the role of physical risk factors, health status, and cognitive activities (MIDUS). Whereas previous studies have examined these factors individually, the present study demonstrates the cumulative association and protective value for cognitive functioning. Interestingly, the effects of the protective factors were equally beneficial across adulthood and into old age. Another key promising finding was that education differences in episodic memory and declines in reasoning abilities were significantly attenuated as a function of the number of protective factors. In previous work, we had a similar finding in that engaging in frequent cognitive activity compensated for education differences in episodic memory (Lachman et al., 2010). In the current study, this mitigating role was extended to noncognitive protective factors. This suggests that the cognitive risks traditionally associated with low educational attainment can be attenuated by modifying a large spectrum of lifestyle factors. However, for executive functioning, the effects of education were not reduced by the protective factors as they were for episodic memory. Perhaps, one clue comes from the BOLOS analyses. In that case, changes in reasoning were attenuated by the protective factor, especially for those with lower education. Thus, it may be that education effects for those aspects of cognitive performance that depend on strategic behaviors are more likely to be attenuated with psychosocial and behavioral factors. In contrast, education differences involving speed and attentional processes may be less amenable to behavioral factors.
Engaging in a greater number of protective lifestyle factors was associated with better cognition both in the cross-sectional and longitudinal analyses. The patterns obtained in MIDUS also showed that those who adopted additional protective behaviors between the two occasions of measurement showed improved executive functioning. However, increases in protective behaviors did not improve episodic memory or reasoning beyond the protective effects at Time 1. Further work is needed to explore why only executive functioning was related to changes in protection.
To our knowledge, this is the first time that the combined contribution of psychosocial and behavioral factors to cognitive performance has been analyzed, and these results have valuable public health relevance. Importantly, the protective factors we examined are modifiable. Several studies have shown and reviewed the efficacy of interventions to change control beliefs (e.g., Lachman, Neupert, & Agrigoroaei, 2011), physical activity (e.g., Yan, Wilber, Aguirre, & Trejo, 2009), and social support (e.g., Berkman et al., 2003; Rains & Young, 2009). Therefore, these factors could be considered in the design of future multiple-behavior interventions or lifestyle programs (Small et al., 2006). Also, knowing someone's standing on the protective composite could allow the identification of the persons most at risk for cognitive decline. For example, those at retirement age are a vulnerable group, given their potential for decreases in social exchanges, control beliefs, and frequency of physical exercise. Thus, this group could be targeted and encouraged to engage in diverse activities providing a high sense of control, quality social support, and opportunities for physical activity.
We acknowledge that the obtained patterns must be considered in light of some inherent limitations. The generalizability of our findings is limited to some extent by the positive selection of the longitudinal participants in MIDUS and BOLOS and the relatively small sample size of BOLOS. Also, even though the data are from a large national probability-based sample, the median split approach used to compute the protective composite is sample dependent and cannot provide universal guidelines. Although it is a reasonable method given the lack of clinically meaningful criteria for dividing participants into high and low categories, future studies should consider different approaches for computing protective factors using different cutoffs, weighted scores, or continuous scales.
Although the design from the larger MIDUS study was cross-sectional, it is encouraging that the findings were essentially replicated with the longitudinal sample in which we found the protective factor related to change with one key cognitive dimension: reasoning. Also, the validity of some of our self-reported measures (e.g., waist circumference, physical exercise) could be optimized using multiple indicators. Furthermore, the amount of variance accounted for by the psychosocial and behavioral factors was in the small range. Along with the factors we considered in the current study, other variables can play a role in cognitive functioning (Hertzog et al., 2008) and should be considered as protective factors or covariates in the statistical models. For instance, level of stress (Neupert, Almeida, Mroczek, & Spiro, 2006), personality profiles (Pearman, 2009; Willis & Boron, 2008), and healthy nutrition (Del Parigi, Panza, Capurso, & Solfrizzi, 2006) also account for between-person heterogeneity in cognitive performance, directly or via physical health.
In spite of these limitations and the fact that the current design does not provide a final answer concerning causality, the present study provides a plausible examination of the role of the synergistic effects of high control beliefs, frequent physical activity, and high-quality social support, on cognitive functioning and long-term change. However, future work is needed to examine this set of protective factors in relation to long-term changes in multiple aspects of cognition, including the risk of dementia, and to explore the individual and shared mechanisms (e.g., stress hormones, McEwen, 2008; inflammation processes, Ferrucci et al., 1999; allostatic load, Gruenewald et al., 2009) that may be involved in linking the combined psychosocial and behavioral factors to cognitive functioning.
FUNDING
This work was supported by the National Institute on Aging (RO1 AG 032271, RO1 AG17920, PO1 AG20166) and the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development.
SUPPLEMENTARY MATERIAL
Supplementary tables can be found at: http://psychsocgerontology.oxfordjournals.org/.
Acknowledgments
The article was written while the second author was a fellow at the Center for Advanced Study in the Behavioral Sciences at Stanford University and a member of the working group sponsored by the Stanford Center on Longevity.
References
- Albert MS, Jones K, Savage CR, Berkman L, Seeman T, Blazer D, Rowe JW. Predictors of cognitive change in older persons: MacArthur Studies of Successful Aging. Psychology and Aging. 1995;10:578–589. doi: 10.1037//0882-7974.10.4.578. doi:10.1037/0882-7974.10.4.578. [DOI] [PubMed] [Google Scholar]
- Alley D, Suthers K, Crimmins E. Education and cognitive decline in older Americans: Results from the AHEAD sample. Research on Aging. 2007;29:73–94. doi: 10.1177/0164027506294245. doi:10.1177/0164027506294245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anstey KJ, von Sanden C, Salim A, O’Kearney R. Smoking as a risk factor for dementia and cognitive decline: A meta-analysis of prospective studies. American Journal of Epidemiology. 2007;166:367–378. doi: 10.1093/aje/kwm116. doi:10.1093/aje/kwm116. [DOI] [PubMed] [Google Scholar]
- Béland F, Zunzunegui M, Alvarado B, Otero A, del Ser T. Trajectories of cognitive decline and social relations. Journal of Gerontology: Psychological Sciences. 2005;60B:P320–P330. doi: 10.1093/geronb/60.6.p320. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Schneiderman N. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Journal of the American Medical Association. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. doi:10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. doi:10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bielak AAM, Hultsch DF, Levy-Ajzenkopf J, MacDonald SWS, Hunter MA, Strauss E. Short-term changes in general and memory-specific control beliefs and their relationship to cognition in younger and older adults. International Journal of Aging and Human Development. 2007;65:53–71. doi: 10.2190/G458-X101-0338-746X. doi:10.2190/G458-X101-0338-746X. [DOI] [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC. How healthy are we? A national study of well-being at midlife. Chicago: University of Chicago Press; 2004. [Google Scholar]
- Caplan LJ, Schooler C. The roles of fatalism, self-confidence, and intellectual resources in the disablement process in older adults. Psychology and Aging. 2003;18:551–561. doi: 10.1037/0882-7974.18.3.551. doi:10.1037/0882-7974.18.3.551. [DOI] [PubMed] [Google Scholar]
- Chen H, Guo X. Obesity and functional disability in elderly Americans. Journal of the American Geriatrics Society. 2008;56:689–694. doi: 10.1111/j.1532-5415.2007.01624.x. doi:10.1111/j.1532-5415.2007.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. London: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychological Science. 2003;14:125–130. doi: 10.1111/1467-9280.t01-1-01430. doi:10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- Cotter KA, Lachman ME. Psychosocial and behavioural contributors to health: Age-related increases in physical disability are reduced by physical fitness. Psychology and Health. 2010;25:805–820. doi: 10.1080/08870440902883212. doi:10.1080/08870440902883212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Parigi A, Panza F, Capurso C, Solfrizzi V. Nutritional factors, cognitive decline, and dementia. Brain Research Bulletin. 2006;69:1–19. doi: 10.1016/j.brainresbull.2005.09.020. doi:10.1016/j.brainresbull.2005.09.020. [DOI] [PubMed] [Google Scholar]
- Dik MG, Deeg DJH, Visser M, Jonker C. Early life physical activity and cognition at old age. Journal of Clinical and Experimental Neuropsychology. 2003;25:643–653. doi: 10.1076/jcen.25.5.643.14583. doi:10.1076/jcen.25.5.643.14583. [DOI] [PubMed] [Google Scholar]
- Ferrucci L, Harris TB, Guralnik JM, Tracy RP, Corti MC, Cohen HJ, Havlik RJ. Serum IL-6 level and the development of disability in older persons. Journal of the American Geriatrics Society. 1999;47:639–646. doi: 10.1111/j.1532-5415.1999.tb01583.x. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. doi:10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Seeman TE, Karlamangla AS, Sarkisian CA. Allostatic load and frailty in older adults. Journal of the American Geriatrics Society. 2009;57:1525–1531. doi: 10.1111/j.1532-5415.2009.02389.x. doi:10.1111/j.1532-5415.2009.02389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall CD, Smith AL, Keele SW. The impact of aerobic activity on cognitive function in older adults: A new synthesis based on the concept of executive control. European Journal of Cognitive Psychology. 2001;13:279–300. doi:10.1080/09541440042000313. [Google Scholar]
- Hertzog C. Use it or lose it: An old hypothesis, new evidence, and an ongoing controversy. In: Bosworth HB, Hertzog C, editors. Aging and cognition: Research methodologies and empirical advances. Washington, DC: American Psychological Association; 2009. pp. 161–179. [Google Scholar]
- Hertzog C, Kramer AF, Wilson RS, Lindenberger U. Enrichment effects on adult cognitive development: Can the functional capacity of older adults be preserved and enhanced? Psychological Science in the Public Interest. 2008;9:1–65. doi: 10.1111/j.1539-6053.2009.01034.x. [DOI] [PubMed] [Google Scholar]
- Hertzog C, McGuire CL, Lineweaver TT. Aging, attributions, perceived control, and strategy use in a free recall task. Aging, Neuropsychology, and Cognition. 1998;5:85–106. doi:10.1076/anec.5.2.85.601. [Google Scholar]
- Hofer SM, Alwin DF. Handbook of cognitive aging: Interdisciplinary perspectives. Los Angeles: Sage Publications; 2008. [Google Scholar]
- Jedrziewski MK, Lee VM, Trojanowski JQ. Physical activity and cognitive health. Alzheimer's & Dementia. 2007;3:98–108. doi: 10.1016/j.jalz.2007.01.009. doi:10.1016/j.jalz.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp A, Paillard-Borg S, Wang H, Silverstein M, Winblad B, Fratiglioni L. Mental, physical and social components in leisure activities equally contribute to decrease dementia risk. Dementia and Geriatric Cognitive Disorders. 2006;21:65–73. doi: 10.1159/000089919. doi:10.1159/000089919. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Prüssner JC, Stone AA, Federenko I, Gaab J, Lintz D, Hellhammer DH. Persistent high cortisol responses to repeated psychological stress in a subpopulation of healthy men. Psychosomatic Medicine. 1995;57:468–474. doi: 10.1097/00006842-199509000-00009. [DOI] [PubMed] [Google Scholar]
- Kramer AF, Hahn S, Cohen NJ, Banich MT, McAuley E, Harrison CR, Colcombe A. Ageing, fitness and neurocognitive function. Nature. 1999;400:418–419. doi: 10.1038/22682. doi:10.1038/22682. [DOI] [PubMed] [Google Scholar]
- Lachman ME. Perceived control over aging-related declines: Adaptive beliefs and behaviors. Current Directions in Psychological Science. 2006;15:282–286. doi:10.1111/j.1467-8721.2006.00453.x. [Google Scholar]
- Lachman ME, Agrigoroaei S, Murphy C, Tun PA. Frequent cognitive activity compensates for education differences in episodic memory. The American Journal of Geriatric Psychiatry. 2010;18:4–10. doi: 10.1097/JGP.0b013e3181ab8b62. doi:10.1097/JGP.0b013e3181ab8b62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Andreoletti C. Strategy use mediates the relationship between control beliefs and memory performance for middle-aged and older adults. Journal of Gerontology: Psychological Sciences. 2006;61B:P88–P94. doi: 10.1093/geronb/61.2.p88. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Neupert SD, Agrigoroaei S. The relevance of control beliefs for health and aging. In: Schaie KW, Willis SL, editors. Handbook of the psychology of aging. San Diego, CA: Academic; 2011. Press. [Google Scholar]
- Lachman ME, Neupert SD, Bertrand R, Jette AM. The effects of strength training on memory in older adults. Journal of Aging and Physical Activity. 2006;14:59–73. doi: 10.1123/japa.14.1.59. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Röcke C, Rosnick C, Ryff CD. Realism and illusion in Americans’ temporal views of their life satisfaction: Age differences in reconstructing the past and anticipating the future. Psychological Science. 2008;19:889–897. doi: 10.1111/j.1467-9280.2008.02173.x. doi:10.1111/j.1467-9280.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Tun PA. Cognitive testing in large-scale surveys: Assessment by telephone. In: Hofer SM, Alwin DF, editors. Handbook of cognitive aging: Interdisciplinary perspectives. Los Angeles: Sage Publications; 2008. pp. 506–523. [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. doi:10.1037/0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lopes MA, Furtado EF, Ferrioli E, Litvoc J, de Campos Bottino CM. Prevalence of alcohol-related problems in an elderly population and their association with cognitive impairment and dementia. Alcoholism: Clinical and Experimental Research. 2010;34:726–733. doi: 10.1111/j.1530-0277.2009.01142.x. doi:10.1111/j.1530-0277.2009.01142.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. European Journal of Pharmacology. 2008;583:174–185. doi: 10.1016/j.ejphar.2007.11.071. doi:10.1016/j.ejphar.2007.11.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMorris T, Collard K, Corbett J, Dicks M, Swain JP. A test of the catecholamines hypothesis for an acute exercise-cognition interaction. Pharmacology Biochemistry and Behavior. 2008;89:106–115. doi: 10.1016/j.pbb.2007.11.007. doi:10.1016/j.pbb.2007.11.007. [DOI] [PubMed] [Google Scholar]
- Miller LMS, Lachman ME. Cognitive performance and the role of control beliefs in midlife. Aging, Neuropsychology, and Cognition. 2000;7:69–85. doi:10.1076/1382-5585(200006)7:2;1-U;FT069. [Google Scholar]
- Neupert SD, Almeida DM, Mroczek DK, Spiro A., III Daily stressors and memory failures in a naturalistic setting: Findings from the VA Normative Aging Study. Psychology and Aging. 2006;21:424–429. doi: 10.1037/0882-7974.21.2.424. doi:10.1037/0882-7974.21.2.424. [DOI] [PubMed] [Google Scholar]
- Newson RS, Kemps EB. The influence of physical and cognitive activities on simple and complex cognitive tasks in older adults. Experimental Aging Research. 2006;32:341–362. doi: 10.1080/03610730600699134. doi:10.1080/03610730600699134. [DOI] [PubMed] [Google Scholar]
- Nilsson L, Nilsson E. Overweight and cognition. Scandinavian Journal of Psychology. 2009;50:660–667. doi: 10.1111/j.1467-9450.2009.00777.x. doi:10.1111/j.1467-9450.2009.00777.x. [DOI] [PubMed] [Google Scholar]
- Pearman A. Basic cognition in adulthood: Combined effects of sex and personality. Personality and Individual Differences. 2009;47:357–362. doi:10.1016/j.paid.2009.04.003. [Google Scholar]
- Poortiga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Preventive Medicine. 2007;44:124–128. doi: 10.1016/j.ypmed.2006.10.006. doi:10.1016/j.ypmed.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Rains SA, Young V. A meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Human Communication Research. 2009;35:309–336. doi:10.1111/j.1468-2958.2009.01353.x. [Google Scholar]
- Raven J, Raven JC, Court JH. Manual for Raven's progressive matrices and vocabulary scales: Section 1. Oxford: Oxford Psychologists; 1991. [Google Scholar]
- Rogers RL, Meyer JS, Mortel KF. After reaching retirement age physical activity sustains cerebral perfusion and cognition. Journal of the American Geriatrics Society. 1990;38:123–128. doi: 10.1111/j.1532-5415.1990.tb03472.x. [DOI] [PubMed] [Google Scholar]
- Sabia S, Nabi H, Kivimaki M, Shipley MJ, Marmot MG, Singh-Manoux A. Health behaviors from early to late midlife as predictors of cognitive function: The Whitehall II study. American Journal of Epidemiology. 2009;170:428–437. doi: 10.1093/aje/kwp161. doi:10.1093/aje/kwp161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA. When does age-related cognitive decline begin? Neurobiology of Aging. 2009;30:507–514. doi: 10.1016/j.neurobiolaging.2008.09.023. doi:10.1016/j.neurobiolaging.2008.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA, Kausler DH, Saults JS. Age, self-assessed health status, and cognition. Journal of Gerontology. 1990;45:P156–P160. doi: 10.1093/geronj/45.4.p156. [DOI] [PubMed] [Google Scholar]
- Schaie KW. Manual for the Schaie-Thurstone Adult Mental Abilities Test (STAMAT) Palo Alto, CA: Consulting Psychologists Press; 1985. [Google Scholar]
- Seeman TE, Crimmins E, Huang M, Singer B, Bucur A, Gruenewald T, Reuben DB. Cumulative biological risk and socio-economic differences in mortality: MacArthur Studies of Successful Aging. Social Science & Medicine. 2004;58:1985–1997. doi: 10.1016/S0277-9536(03)00402-7. doi:10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur Studies of Successful Aging. Health Psychology. 2001;20:243–255. doi: 10.1037//0278-6133.20.4.243. doi:10.1037//0278-6133.20.4.243. [DOI] [PubMed] [Google Scholar]
- Small BJ, McEvoy CL. Does participation in cognitive activities buffer age-related cognitive decline? In: Hofer SM, Alwin DF, editors. Handbook of cognitive aging: Interdisciplinary perspectives. Los Angeles: Sage Publications; 2008. pp. 575–586. [Google Scholar]
- Small GW, Silverman DHS, Siddarth P, Ercoli LM, Miller KJ, Lavretsky H, Phelps ME. Effects of a 14-day healthy longevity lifestyle program on cognition and brain function. American Journal of Geriatric Psychiatry. 2006;14:538–545. doi: 10.1097/01.JGP.0000219279.72210.ca. doi:10.1097/01.JGP.0000219279.72210.ca. [DOI] [PubMed] [Google Scholar]
- Spiro A, Brady CB, et al. Integrating health into cognitive aging research and theory: Quo vadis? In: Hofer SM, Alwin DF, editors. Handbook of cognitive aging: Interdisciplinary perspectives. Los Angeles: Sage Publications; 2008. pp. 260–283. [Google Scholar]
- StataCorp. Stata Statistical Software (Version 11) College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Sturman MT, Morris MC, Mendes de Leon CF, Bienias JL, Wilson RS, Evans DA. Physical activity, cognitive activity, and cognitive decline in a biracial community population. Archives of Neurology. 2005;62:1750–1754. doi: 10.1001/archneur.62.11.1750. doi:10.1001/archneur.62.11.1750. [DOI] [PubMed] [Google Scholar]
- Tun PA, Lachman ME. Age differences in reaction time and attention in a national telephone sample of adults: Education, sex, and task complexity matter. Developmental Psychology. 2008;44:1421–1429. doi: 10.1037/a0012845. doi:10.1037/a0012845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen HR, Lachman ME. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships. 2000;17:5–30. doi:10.1177/0265407500171001. [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale—Third Edition (WAIS) New York: Psychological Corporation; 1997. [Google Scholar]
- West RL, Yassuda MS. Aging and memory control beliefs: Performance in relation to goal setting and memory self-evaluation. Journal of Gerontology: Psychological Sciences. 2004;59B:P56–P65. doi: 10.1093/geronb/59.2.p56. [DOI] [PubMed] [Google Scholar]
- Willis SL, Boron JB. Midlife cognition: The association of personality with cognition and risk of cognitive impairment. In: Hofer SM, Alwin DF, editors. Handbook of cognitive aging: Interdisciplinary perspectives. Los Angeles: Sage Publications; 2008. pp. 647–660. [Google Scholar]
- Yaffe K, Fiocco AJ, Lindquist K, Vittinghoff E, Simonsick EM, Newman AB, Harris TB. Predictors of maintaining cognitive function in older adults: The Health ABC Study. Neurology. 2009;72:2029–2035. doi: 10.1212/WNL.0b013e3181a92c36. doi:10.1212/WNL.0b013e3181a92c36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan T, Wilber KH, Aguirre R, Trejo L. Do sedentary older adults benefit from community-based exercise? Results from the Active Start program. The Gerontologist. 2009;49:847–855. doi: 10.1093/geront/gnp113. doi:10.1093/geront/gnp113. [DOI] [PubMed] [Google Scholar]