Abstract
Purpose of review
Both arthritis and foot pain are major public health problems. Approximately 24% of adults have foot ailments, and the prevalence increases with age. Foot pain, particularly related to shoes, footwear and rheumatic disorders, may be an important modifiable factor. Surprisingly, this topic has received little attention in the rheumatology community.
Recent findings
Despite the major focus of structure and alignment in arthritis, remarkably little work has focused on the foot and non-surgical foot interventions that might affect lower extremity joint alignment, structure and pain in rheumatic diseases. Emerging research suggests that there may be a significant role for foot orthotics and footwear in the treatment of rheumatoid arthritis and osteoarthritis of the hip, knee and foot. This review highlights the current understanding on the topic of foot orthotics and footwear in adults with rheumatic diseases.
Summary
Biomechanical evidence indicates that foot orthotics and specialized footwear may change muscle activation and gait patterns to reduce joint loading. Emerging evidence suggests that orthotics, specific shoe types and footwear interventions may provide an effective non-surgical intervention in rheumatic diseases. Yet good data are sparse, and it is premature to recommend guidelines. As there are a limited number of studies that underpin the foot’s role in arthritis etiology and progression, clinical trials and prospective studies are of utmost importance to unravel the links between foot pain, foot conditions and interventions that lessen the impact of rheumatic diseases.
Keywords: arthritis, pain, feet, osteoarthritis, orthotics, footwear, shoes, shoe modifications
Introduction
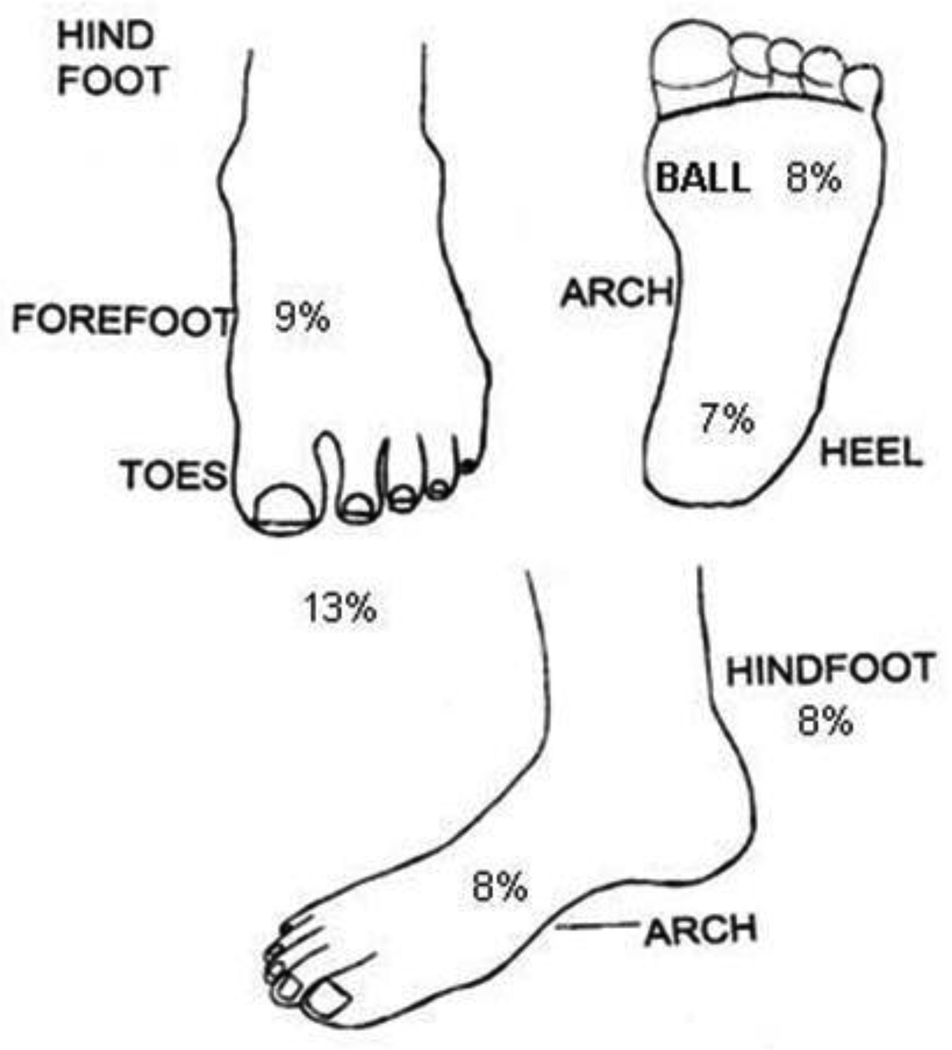
Both arthritis and foot pain are major public health problems with escalating trajectories. As the number of older adults in the population exponentially increase, so will the burden and proportions of society affected by these problems. A podiatric supplement to the US National Health Interview Survey estimated 24% of the population has at least one foot ailment, with older adults experiencing more troubles than younger adults[1]. Recent prevalence data from the Framingham Study reported that 19% of men and 29% of women reported foot pain on most days of the month, with prevalence of pain at specific foot locations ranging from 7% to 13% (figure 1) [2].
Figure 1.
Diagram of the foot and prevalence of pain in each location as reported by the 3,372 men and women in the Framingham Foot Study, 2002–2008 [2].
For persons with rheumatoid arthritis (RA), these site-specific prevalence reports of foot pain are approximately double those seen in the general population[3]. Foot pain, particularly as it relates to shoes, footwear and arthritis-related disorders may be an important modifiable factor, yet this topic has received little attention in the rheumatology community. Over the past few decades, knee bracing for knee osteoarthritis has garnered significant attention for its role in correcting joint malalignment and possibly reducing progression of knee osteoarthritis. In comparison, very little work has focused on the foot and non-surgical foot intervention that might benefit foot pain and related rheumatic diseases. However, emerging research suggests that there may be a significant role for foot orthotics and footwear in the treatment of rheumatic disease. This review highlights the current understanding on the topic of foot orthotics and shoe wear in adult populations with rheumatoid arthritis and osteoarthritis.
Popular belief is that foot orthoses and therapeutic footwear cause changes in kinematic and skeletal alignment; however, systematic reviews suggest these changes may be minimal[4]. In contrast, research suggests that the benefit of foot orthotics and specialized shoe wear is in changing the shank and foot muscle activation[5] and gait[6] pattern to reduce joint loading. Nigg et al.[7] proposed the “preferred movement pathway model,” hypothesizing that altering afferent signaling with foot orthotics leads to changes in muscle activity to reduce lower extremity stress[8]. These data, when taken together, provide evidence that the foot provides the “micro control” of gait[9] and suggests orthotics and specific shoe wear may provide an effective non-surgical and non-pharmacologic intervention in rheumatic diseases.
The foot in rheumatoid arthritis
Over 85% of patients with rheumatoid arthritis (RA) have painful feet or ankles during the course of the disease, and within the first year of diagnosis up to 57% of patients report foot or ankle symptoms[10]. In patients with RA, inflammation and changes in bone and ligament integrity cause hindfoot instability leading to forefoot deformity[11–12]. The hindfoot instability can be insidious, leading the forefoot to present symptoms first. These ailments include hallux valgus, subluxation, dislocation or erosion of the metatarsophalangeal (MTP) joints as well as hammer toe or claw toe in the lesser toes. Both the hindfoot and forefoot adaptations lead to altered foot and ankle motion, higher forefoot plantar pressure loading, and increased pain during weight-bearing and locomotor activities [13–15].
Correcting plantar loading and stabilizing the foot and ankle may reduce the likelihood of foot deformities and walking disability for patients with RA[11, 15–16]. Commonly this is thought to be accomplished through orthotics or custom shoe wear. However, critical reviews of controlled studies in shoe wear and foot orthotics in persons with RA have shown limited evidence to support their use[17–18], leading a Cochrane review to report only a “silver level of evidence” for prescribing custom-made foot orthoses in patients with RA [19].
Foot orthotics for patients with RA
As the primary reason people use orthotics is to facilitate movement[20], understanding the effects of foot orthotics on gait is paramount. Kavlak et al.[21] noted that using a custom-made foot orthotic for three months reduced pain, increased step and stride length, and lowered energy expenditure during gait relative to the pre-orthotic condition in patients with RA. A similar study by Mejjad et al. [22] concurred that custom-made orthotics reduced pain, but they concluded that the orthotics were not adequate in improving gait as only step length improved. There was, however, a two month difference in acclimation periods, with participants in the Mejjad study only using the orthotics for one month prior to retesting. While persons without RA may have an acclimation period as short as two weeks[23], research in study participants with RA suggests six weeks with an average of 6 hours per day of use is needed to see a treatment effect[24–25]. The longer acclimation period in the clinical RA studies points to the need for further research to understand differences in orthotic use and gait adaptations in patients with RA.
In addition to treatment time, the type of orthotic (e.g., rigid or soft) relative to foot structure is important as well[25]. In general, rigid orthotics are used to control excessive pronation (pes planus or flat-footedness), reduce forefoot loading [24] and decrease forefoot and rearfoot pain[25]. Rigid orthotics may also reduce the risk of subsequent deformities such as hallux valgus[16]. In one of the few prospective studies, Budiman-Mak et al.[16] showed that using a custom-molded hard foot orthosis led to a 73% decrease in the incidence of hallux valgus over a three-year period. Conversely, soft orthotics are typically used in conjunction with rigid foot ailments, such as pes cavus[26], and reduce both forefoot and generalized foot pain in patients with RA [21–22, 27]. As both rigid and soft orthotics provided adequate comfort in these patients[24–25, 27], the recommendation is that foot orthotics should be custom-designed to meet the individual’s unique needs to reduce pain[19, 25].
Shoe wear for patients with RA
In persons with RA, shoes, like their orthotic counterparts, should reduce plantar pressure and stress while stabilizing the foot and ankle. Heat-moldable, customizable shoes or shoes with extra-depth may improve ambulation and reduce pain in patients with RA[28–29]. A study of 25 participants with RA reported that wearing heat-moldable shoes for three month increased walking ability for 80% of the participants[28]. To increase foot and ankle stabilization, extra-depth orthopaedic shoes, especially when aligned with a foot orthotic, may be effective[24].
While current evidence suggests that therapeutic and orthopaedic footwear can improve gait in persons with RA[24, 28–30], there tends to be large resistance in wearing these types of footwear[20, 31]. Many studies have reported that people with RA find the size, aesthetics, design, weight and comfort of orthopaedic shoes to be unacceptable [20, 30, 32].
As orthopaedic and therapeutic footwear tend to have increased bulk, running shoes may provide some of the comforts without the extra size and weight [33]. In a recent single-blind comparison with participants unable to see the type of shoe (control shoe, running shoe or orthopaedic shoe), the participants chose the running shoe over the others based on comfort and weight[33]. It is important to note that the running shoes also provided better attenuation of forefoot plantar pressure and foot loading relative to the orthopaedic and control shoe. These findings suggest that there is an increased need for exploring lightweight alternatives to the traditional therapeutic shoe.
Similar to the running shoe shape is the toe rocker-soled shoe. The toe rocker-soled shoe is thought to reduce pain by decreasing forefoot loading and promoting a normal heel-toe motion during gait[34–35]. With disease progression, patients with RA move from a heel-toe rolling gait to a more shuffled step with a delayed heel lift[10, 36], and the toe rocker-soled shoe may slow this progression[37]. A randomized controlled trial of patients with RA examined the effects of extra deep forefoot-rocker shoe with either a custom-made semi-rigid insole or a ready-made simple soft insole [37]. Pain was found to decrease in both treated and untreated groups, and between groups there were no clinically identifiable differences. Cho et al.[37] concluded that rocker-soled shoes with comfortable insoles may be enough to reduce foot pain and increase foot function for patients with RA.
The foot in lower extremity osteoarthritis
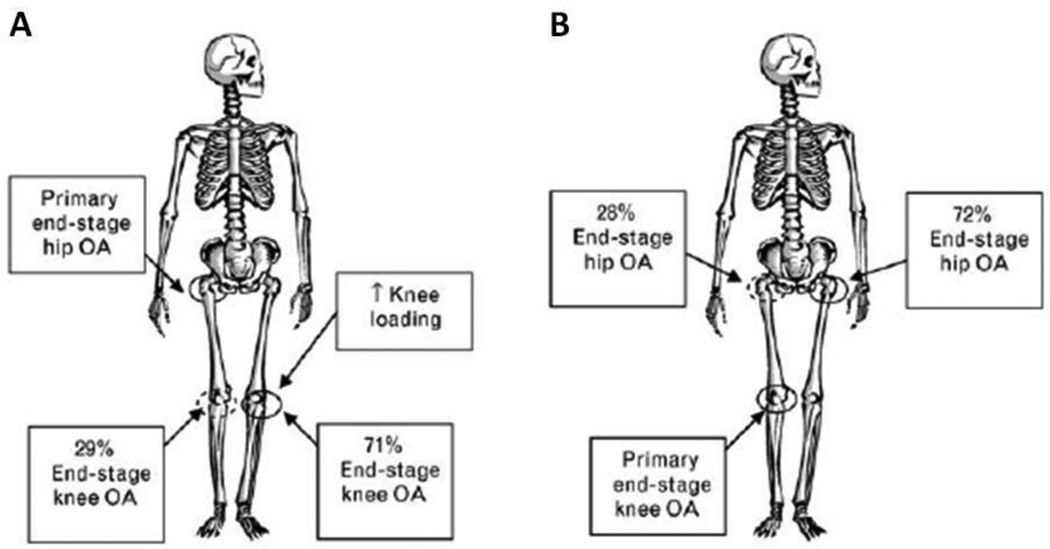
The role of the foot has been limitedly explored with regard to lower extremity osteoarthritis (OA). While there are no prospective studies available, cross-sectional studies show a strong and notable association between foot alignment and hip and knee OA[38–40]. These findings suggest that patients with hip OA are more likely to have a high-arched foot, whereas patients with knee OA are more likely to be flat-footed[38–40]. These studies do not provide a causative mechanism between foot structure and OA development, but they do provide justification for exploring the role of the foot in lower extremity OA. Further, the known progression between primary hip and knee OA to subsequent joint OA development (see Figure 2) necessitates research exploring the role of the foot in lower extremity OA.
Figure 2.
There is a known relationship between hip and knee osteoarthritis (OA) progression [41]. Diagram A shows the progression of end-stage hip OA to the contralateral knee, and diagram B shows progression of primary knee OA to contralateral hip OA. Notably missing from these schematics is the foot’s role in OA etiology and/or progression.
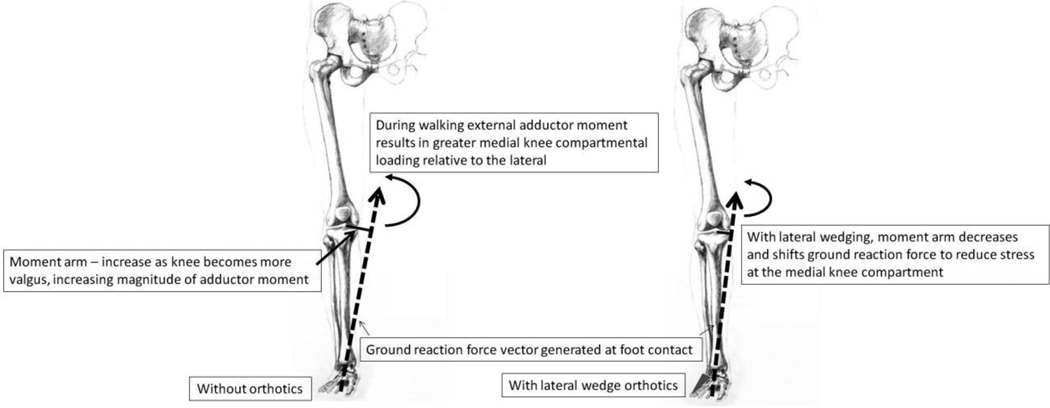
Foot orthotics and shoe wear in knee OA
The most common knee osteoarthritis is medial compartmental knee OA[42]. Though the cause non-traumatic medial knee OA is unknown, two mechanisms of disease are thought to be a high rate of loading and a high external adductor moment during walking. As such, studies often focus on the effects of shoe wear and foot orthotics on these biomechanical markers in medial compartmental knee OA. Most research on foot orthotics focuses on lateral wedge orthotics in this population as lateral wedge orthotics are thought to reduce the knee adductor moment to reduce medial-compartmental knee stress (see Figure 3).
Figure 3.
During walking a ground reaction force (GRF) and an associated external adductor moment is generated. The external adductor moment is related to the GRF and the moment arm, defined as the distance from the knee joint axis to the GRF. With malalignment, either at the foot or knee, there is a higher external adductor moment at the knee joint. Lateral wedge orthotics is thought to decrease moment arm to reduce the external adductor moment and stress at the medial knee compartment. (Adapted from [43].)
Butler et al.[44] reported 12 of 20 participants with medial knee OA had a 10% reduction in the first peak knee adduction moment and five of the 20 exhibited a 10% reduction in the second peak knee adduction moment when using lateral wedged insoles during walking. A long-term study confirmed these results, showing that using lateral wedged insoles for two years showed decreased adductor moments during gait with and without the insoles (i.e., when walking barefoot)[6]. These latter results suggest that transient effects of foot orthotics can lead to long-term gait adaptations that reduce adductor moments. The researchers concluded that “as excess loading of the knee is associated with OA progression, these sustained reductions may have a beneficial impact on the disease course”[6].
Though this conclusion may be valid, a similar two-year prospective randomized controlled trial of lateral wedge orthotics for patients with knee OA showed no structural radiographic difference between patients who used the lateral wedge insoles relative to neutral insoles[45]. They did find, however, patients who used lateral wedged orthotics had lower NSAID (nonsteroidal anti-inflammatory drug) usage and better compliance compared to those with the neutral-wedged insole. The authors concluded that the decreased NSAID use and better compliance provide evidence of beneficial effect of lateral wedge insoles in patients with knee OA. A subsequent 1-year randomized controlled trial by Barrios et al.[46] confirmed these results, while also noting that patients in the lateral wedge orthotic group showed earlier improvements relative to the neutral orthotic.
By convention, lateral wedged orthotics are typically placed in the shoe, but a 2007 study examined the effectiveness of this practice. In this study Kuroyanagi et al.[47] assessed the short-term effects of insole orthotics versus subtalar strapped orthotics. They found that while both reduced loading relative to walking barefoot, the subtalar strapping had a greater reduction in medial knee loading in patients with moderate, but not severe, knee OA.
In addition to orthotics, shoes may play a role in the treatment of knee OA. Erhart et al.[48–49] explored variable-stiffness shoes in patients with medial knee OA. In this work, the variable-stiffness shoe reduced pain during walking while lowering the knee adductor moment. With six months of use patients improved function and had less pain with the variable-stiffness shoe. Other studies corroborate these findings, as Shakoor et al.[50] reported that patients with knee OA showed a decreased knee adductor moment when walking with the “mobility shoe” relative to both the control and the patient’s self-selected shoes.
Interestingly, Shakoor et al.[51] also found that when comparing clogs, stability shoes, flat walking shoes, and flip-flops, in patients with knee OA peak knee loads were greatest in the clogs and stability shoes and least in the flat walking shoes and flip-flops, as well as when walking barefoot. These data suggest that footwear is an important treatment consideration in patients with knee OA. They concluded that shoe flexibility and heel height (small height is better) may be important differentiating characteristics of shoes that affect knee loads. Together these studies suggest that footwear can affect knee joint loads and that clinicians should evaluate the patient’s shoes when exploring treatment strategies in patients with knee OA.
Foot orthotics and shoe wear in hip OA
Few studies have attempted to evaluate shoe and orthotic treatment for hip OA. Overall, the evidence for or against the orthotics is weak and no randomized controlled trials have evaluated their efficacy.
Gélis et al. [52] aimed to develop clinical practice guidelines for the use of foot orthotics in the treatment of knee and hip OA but found weak evidence for the use of foot orthotics. Lee et al. [53] agreed, stating that with the lack of controlled trials on foot orthotics their effectiveness is unknown. Despite this lack of evidence, particularly with regard to hip OA, the OARSI (Osteoarthritis Research Society International) recommendations state that “Every patient with hip or knee OA should receive advice concerning appropriate footwear” [54]. It is stated, however, that this recommendation concerning footwear is based on expert opinion given the lack of controlled trials in patients with hip OA.
Foot orthotics in midfoot OA
A lesser-known osteoarthritis is that of the midfoot. The etiology of midfoot OA is poorly understood. It has been linked to trauma, inflammatory arthropathy, mechanical stress and idiopathic osteoarthritis. Like other forms of non-traumatic OA, midfoot OA may be a result of abnormally high mechanical stress. Davitt et al.[55] hypothesized that aberrant loading may be the result of toe length abnormalities, as patients with idiopathic midfoot OA were more likely to have a second toe longer than the great toe. Yu et al.[56] suggested that the aberrant loading may be a result of past shoe use or footwear, noting that chronic high-heel use increased the risk of midfoot OA.
Promising non-invasive treatment of midfoot OA is a full-length orthotic, which decreases pain and increases foot function by reducing both the magnitude and duration of medial midfoot loading[57] as pointed out by Rao and colleagues. The orthotic intervention may promote a “stiffening” strategy[58], which may increase the mechanical advantage of the great toe and reduce the stress at the medial midfoot. However, future work is needed to understand the mechanical effects of orthotics on this population and the optimal time needed for treatment effect.
The role of footwear in arthritis and foot pain
As footwear is an important treatment strategy for reducing pain and improving function in population with arthritis, it is plausible to believe that footwear may be implicated in the disease etiology (as is the case with midfoot OA[56]).
As women tend to be at a greater risk of hip and knee OA, differences in shoe wear have been implicated, particularly with regard to high heel use. However, a retrospective analysis of factors affecting knee OA reported that wearing high heels did not increase the risk for developing this OA[59], dispelling the belief that high-heeled shoes are a major factor that promotes joint degeneration in women.
Moreover, wearing high heels has shown mixed results with the development of foot pain. A 2009 study by Dufour et al.[2] examined factors associated with foot pain, including current and past shoe wear. They found that women who regularly wore “poor shoes” (e.g., high heels, sandals, slippers) in their past were more likely to experience foot pain in their later years compared to those who wore average shoes.
Contrary to these results, a 2010 study by Paiva de Castro et al.[60] examined the prevalence of current pain among older Brazilian men and women when wearing shoes, and the relations between foot pain and high-heeled shoes. Women had a higher prevalence of foot pain compared to men. Approximately 50% of women and 30% of men reported foot pain when wearing shoes, and in this study current high-heeled shoe use was not associated with pain.
Though the long-term effects of wearing high heels are inconclusive, research has implicated shoes in general with poor foot development and alignment. A study investigating the current[61] and past[62] shoe wear in over 4000 adults and children in India concluded that wearing shoes, particularly during the “critical age in the development of the medial longitudinal arch” (up to 6 years of age), may increase the incidence of flat-footedness. In their sample, the longer a child waited before regularly wearing shoes, the less likely he or she was to have flat feet and foot ligament laxity as an adult[62]. They concluded that prospective long-term studies are needed to evaluate the possible link between shoe use and development of flat footedness. Further, with the known associations between foot structure and OA development[38–40], the role of past footwear and foot structure will certainly be an important component in understanding the etiology of joint degenerative diseases.
Conclusion
This review presented our current understanding of musculoskeletal research that has focused on preventing or relieving foot pain and the effect of footwear and orthotics in adults. Non-surgical interventions may be important modifiable factors for the prevention of foot pain and slowing the foot-related progression of RA, osteoarthritis and perhaps other rheumatic diseases. Emerging evidence indicates that orthotics and perhaps footwear interventions play an important role in rheumatology-related foot health. Study design will be of utmost importance in unraveling the links between foot pain, foot conditions and interventions that lessen the impact of rheumatic diseases, as far too few prospective studies have been performed and more randomized clinical trials are needed. There is insufficient evidence to conclusively link footwear interventions with improvement in persons with RA and OA of various sites. Recent studies of interventions have been inconsistent.
Given the current status of arthritis, foot pain and footwear in the literature, good data are sparse and it is premature to recommend guidelines. More data focusing on rheumatic conditions and specific foot conditions and possible interventions are desperately needed. In addition, there are massive holes in our current knowledge, particularly around pediatric foot issues as well as the biomechanical pathways. Both non-surgical and surgical interventions require more evaluation to add to our meager understanding of possible interventions to improve foot-related pain and dysfunction in rheumatologic conditions. Further studies of the etiology of foot pain and foot biomechanics are essential. Prospective studies are needed to explore the mechanisms by which foot conditions and foot pain operate and to make recommendations for those persons with rheumatic diseases. Longer-term prospective controlled intervention studies are needed to determine whether treatment with specific foot interventions or alterations in biomechanics can improve physical functioning, lessen the burden of disease or reduce severity of rheumatic diseases affecting the feet.
KEY BULLET POINTS.
Foot pain, particularly as it relates to shoes, footwear and arthritis-related disorders may be an important modifiable factor, yet this topic has received little attention in the rheumatology community.
Emerging research suggests that there may be a significant role for foot orthotics and footwear in the treatment of rheumatoid arthritis and osteoarthritis of the hip, knee and foot.
Biomechanical evidence indicates that foot orthotics and specialized footwear may change muscle activation and gait patterns to reduce joint loading.
Clinical trials and prospective studies are needed to unravel the links between foot pain, foot conditions and interventions that lessen the impact of rheumatic diseases.
Acknowledgements
The authors acknowledge the helpful critiques and comments from Thomas Hagedorn, Virginia Casey and the Musculoskeletal Research Center at Hebrew SeniorLife. The authors are supported by National Institutes of Health grants, including AR047853, AG026316 and T32-AG023480.
References
- 1.Greenberg L, Davis H. Foot problems in the US. The 1990 National Health Interview Survey. J Am Podiatr Med Assoc. 1993;83(8):475–483. doi: 10.7547/87507315-83-8-475. [DOI] [PubMed] [Google Scholar]
- 2.Dufour AB, Broe KE, Nguyen US, et al. Foot pain: is current or past shoewear a factor? Arthritis Rheum. 2009;61(10):1352–1358. doi: 10.1002/art.24733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Otter SJ, Lucas K, Springett K, et al. Foot pain in rheumatoid arthritis prevalence, risk factors and management: an epidemiological study. Clin Rheumatol. 2010;29(3):255–271. doi: 10.1007/s10067-009-1312-y. [DOI] [PubMed] [Google Scholar]
- 4.Ball KA, Afheldt MJ. Evolution of foot orthotics--part 2: research reshapes long-standing theory. J Manipulative Physiol Ther. 2002;25(2):125–134. doi: 10.1067/mmt.2002.121416. [DOI] [PubMed] [Google Scholar]
- 5.Nurse MA, Hulliger M, Wakeling JM, et al. Changing the texture of footwear can alter gait patterns. J Electromyogr Kinesiol. 2005;15(5):496–506. doi: 10.1016/j.jelekin.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Thorp LE, Wimmer MA, Sumner DR, et al. Custom shoe inserts induce beneficial long-term gait adaptations in medial knee osteoarthritis. Arthritis Rheum. 2007;56:S120. [Google Scholar]
- 7.Nigg BM, Nurse MA, Stefanyshyn DJ. Shoe inserts and orthotics for sport and physical activities. Med Sci Sports Exerc. 1999;31(7 Suppl):S421–S428. doi: 10.1097/00005768-199907001-00003. [DOI] [PubMed] [Google Scholar]
- 8.Nigg BM. The role of impact forces and foot pronation: a new paradigm. Clin J Sport Med. 2001;11(1):2–9. doi: 10.1097/00042752-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Cavanagh PR, Perry JE, Ulbrecht JS, et al. Neuropathic diabetic patients do not have reduced variability of plantar loading during gait. Gait Posture. 1998;7(3):191–199. doi: 10.1016/s0966-6362(98)00011-3. [DOI] [PubMed] [Google Scholar]
- 10. van der Leeden M, Steultjens MP, Ursum J, et al. Prevalence and course of forefoot impairments and walking disability in the first eight years of rheumatoid arthritis. Arthritis Rheum. 2008;59(11):1596–1602. doi: 10.1002/art.24188. ** This work showed longitudinal data to describe prevalence and severity of foot impairment throughout the first 8 years of an RA diagnosis.
- 11.Dimonte P, Light H. Pathomechanics, gait deviations, and treatment of the rheumatoid foot: a clinical report. Phys Ther. 1982;62(8):1148–1156. doi: 10.1093/ptj/62.8.1148. [DOI] [PubMed] [Google Scholar]
- 12.Coughlin MJ. Common causes of pain in the forefoot in adults. J Bone Joint Surg Br. 2000;82(6):781–790. doi: 10.1302/0301-620x.82b6.11422. [DOI] [PubMed] [Google Scholar]
- 13.Laroche D, Ornetti P, Thomas E, et al. Kinematic adaptation of locomotor pattern in rheumatoid arthritis patients with forefoot impairment. Exp Brain Res. 2007;176(1):85–97. doi: 10.1007/s00221-006-0597-1. [DOI] [PubMed] [Google Scholar]
- 14.Semple R, Turner DE, Helliwell PS, Woodburn J. Regionalised centre of pressure analysis in patients with rheumatoid arthritis. Clin Biomech (Bristol, Avon) 2007;22(1):127–129. doi: 10.1016/j.clinbiomech.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Grondal L, Tengstrand B, Nordmark B, et al. The foot: still the most important reason for walking incapacity in rheumatoid arthritis: distribution of symptomatic joints in 1,000 RA patients. Acta Orthop. 2008;79(2):257–261. doi: 10.1080/17453670710015067. [DOI] [PubMed] [Google Scholar]
- 16. Budiman-Mak E, Conrad KJ, Roach KE, et al. Can Foot Orthoses Prevent Hallux Valgus Deformity in Rheumatoid Arthritis? A Randomized Clinical Trial. J Clin Rheumatol. 1995;1(6):313–322. doi: 10.1097/00124743-199512000-00001. ** This citation is one of the few prospective clinical trials of interventions to prevent foot disorders in persons with RA and showed that custom-molded hard foot orthoses decreased the incidence of hallux valgus by 73% in treated RA patients over a 3-year period.
- 17.Clark H, Rome K, Plant M, et al. A critical review of foot orthoses in the rheumatoid arthritic foot. Rheumatology (Oxford) 2006;45(2):139–145. doi: 10.1093/rheumatology/kei177. [DOI] [PubMed] [Google Scholar]
- 18.Egan M, Brosseau L, Farmer M, et al. Splints/orthoses in the treatment of rheumatoid arthritis. Cochrane Database Syst Rev. 2003;1 doi: 10.1002/14651858.CD004018. CD004018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hawke F, Burns J, Radford JA, du Toit V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008;3 doi: 10.1002/14651858.CD006801.pub2. CD006801. ** This citation contains important references of the relativelyl few clinical trials in RA leading the authors to note the only a 'silver' level of evidence currently is available in support of prescribing custom-made foot orthoses in patients with RA.
- 20. de Boer IG, Peeters AJ, Ronday HK, et al. Assistive devices: usage in patients with rheumatoid arthritis. Clin Rheumatol. 2009;28(2):119–128. doi: 10.1007/s10067-008-0989-7. * This study notes the extreme poor adherence for orthopedic supportive shoe wear by persons with RA based on fit, aesthetics, design and even comfort in wearing.
- 21.Kavlak Y, Uygur F, Korkmaz C, Bek N. Outcome of orthoses intervention in the rheumatoid foot. Foot Ankle Int. 2003;24(6):494–499. doi: 10.1177/107110070302400608. [DOI] [PubMed] [Google Scholar]
- 22.Mejjad O, Vittecoq O, Pouplin S, et al. Foot orthotics decrease pain but do not improve gait in rheumatoid arthritis patients. Joint Bone Spine. 2004;71(6):542–545. doi: 10.1016/j.jbspin.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Mattacola CG, Dwyer MK, Miller AK, et al. Effect of orthoses on postural stability in asymptomatic subjects with rearfoot malalignment during a 6-week acclimation period. Arch Phys Med Rehabil. 2007;88(5):653–660. doi: 10.1016/j.apmr.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 24. Chalmers AC, Busby C, Goyert J, et al. Metatarsalgia and rheumatoid arthritis--a randomized, single blind, sequential trial comparing 2 types of foot orthoses and supportive shoes. J Rheumatol. 2000;27(7):1643–1647. * This work is one of the first studies to emphasize that RA patients may need a longer run-in or acclimation period for orthotics in order to see a treatement effect.
- 25. Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J Rheumatol. 2002;29(7):1377–1383. ** This citation is one of the few randomized trials of foot orthotics in a RA population. It showed that custom-designed foot orthoses used continuously for 30 months resulted in an appoximate 20% reduction in foot pain and 30% reduction in foot disability.
- 26.Jackson L, Binning J, Potter J. Plantar pressures in rheumatoid arthritis using prefabricated metatarsal padding. J Am Podiatr Med Assoc. 2004;94(3):239–245. doi: 10.7547/0940239. [DOI] [PubMed] [Google Scholar]
- 27.Hodge MC, Bach TM, Carter GM. novel Award First Prize Paper. Orthotic management of plantar pressure and pain in rheumatoid arthritis. Clin Biomech (Bristol, Avon) 1999;14(8):567–575. doi: 10.1016/s0268-0033(99)00034-0. [DOI] [PubMed] [Google Scholar]
- 28.Moncur C, Ward JR. Heat-moldable shoes for management of forefoot problems in rheumatoid arthritis. Arthritis & Rheumatism. 1990;3(4):222–226. [Google Scholar]
- 29.Fransen M, Edmonds J. Off-the-shelf orthopedic footwear for people with rheumatoid arthritis. Arthritis Care Res. 1997;10(4):250–256. doi: 10.1002/art.1790100406. [DOI] [PubMed] [Google Scholar]
- 30.Williams AE, Rome K, Nester CJ. A clinical trial of specialist footwear for patients with rheumatoid arthritis. Rheumatology (Oxford) 2007;46(2):302–307. doi: 10.1093/rheumatology/kel234. [DOI] [PubMed] [Google Scholar]
- 31.Williams A, Meacher K. Shoes in the cupboard: the fate of prescribed footwear? Prosthet Orthot Int. 2001;25(1):53–59. doi: 10.1080/03093640108726569. [DOI] [PubMed] [Google Scholar]
- 32.Williams AE, Nester CJ. Patient perceptions of stock footwear design features. Prosthet Orthot Int. 2006;30(1):61–71. doi: 10.1080/03093640600574425. [DOI] [PubMed] [Google Scholar]
- 33.Hennessy K, Burns J, Penkala S. Reducing plantar pressure in rheumatoid arthritis: a comparison of running versus off-the-shelf orthopaedic footwear. Clin Biomech (Bristol, Avon) 2007;22(8):917–923. doi: 10.1016/j.clinbiomech.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Nawoczenski DA, Saltzman CL, Cook TM. The effect of foot structure on the three-dimensional kinematic coupling behavior of the leg and rear foot. Phys Ther. 1998;78(4):404–416. doi: 10.1093/ptj/78.4.404. [DOI] [PubMed] [Google Scholar]
- 35.Brown D, Wertsch JJ, Harris GF, et al. Effect of rocker soles on plantar pressures. Arch Phys Med Rehabil. 2004;85(1):81–86. doi: 10.1016/s0003-9993(03)00374-5. [DOI] [PubMed] [Google Scholar]
- 36.van der Leeden M, Steultjens M, Dekker JH, et al. The relationship of disease duration to foot function, pain and disability in rheumatoid arthritis patients with foot complaints. Clin Exp Rheumatol. 2007;25(2):275–280. [PubMed] [Google Scholar]
- 37.Cho NS, Hwang JH, Chang HJ, et al. Randomized controlled trial for clinical effects of varying types of insoles combined with specialized shoes in patients with rheumatoid arthritis of the foot. Clin Rehabil. 2009;23(6):512–521. doi: 10.1177/0269215508101737. [DOI] [PubMed] [Google Scholar]
- 38.Reilly K, Barker K, Shamley D, Sandall S. Influence of foot characteristics on the site of lower limb osteoarthritis. Foot Ankle Int. 2006;27:206–211. doi: 10.1177/107110070602700310. [DOI] [PubMed] [Google Scholar]
- 39.Hillstrom H, Brower D, Whitney K, et al. Lower extremity conservative realignment therapies for knee osteoarthritis. Philadelphia: Hanley and Belfus. 2002 [Google Scholar]
- 40.Reilly K, Barker K, Shamley D, et al. The role of foot and ankle assessment of patients with lower limb osteoarthritis. Physiotherapy. 2009;95(3):164–169. doi: 10.1016/j.physio.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 41.Block JA, Shakoor N. Lower limb osteoarthritis: biomechanical alterations and implications for therapy. Curr Opin Rheumatol. 2010;22(5):544–550. doi: 10.1097/BOR.0b013e32833bd81f. [DOI] [PubMed] [Google Scholar]
- 42.Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis. 1993;52:520–526. doi: 10.1136/ard.52.7.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hinman RS, Bennell KL. Advances in insoles and shoes for knee osteoarthritis. Curr Opin Rheumatol. 2009;21(2):164–170. doi: 10.1097/BOR.0b013e32832496c2. [DOI] [PubMed] [Google Scholar]
- 44.Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res. 2007;25(9):1121–1127. doi: 10.1002/jor.20423. [DOI] [PubMed] [Google Scholar]
- 45. Pham T, Maillefert JF, Hudry C, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis. A two-year prospective randomized controlled study. Osteoarthritis Cartilage. 2004;12(1):46–55. doi: 10.1016/j.joca.2003.08.011. ** This randomized control study demonstrated the patients were more compliant and had reduced pain medications when using lateral wedge orthotics, but after the 2-year trial there was limited radiographic evidece to suggest that orthotics effected the joint structure.
- 46.Barrios JA, Crenshaw JR, Royer TD, Davis IS. Walking shoes and laterally wedged orthoses in the clinical management of medial tibiofemoral osteoarthritis: a one-year prospective controlled trial. Knee. 2009;16(2):136–142. doi: 10.1016/j.knee.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 47.Kuroyanagi Y, Nagura T, Matsumoto H, et al. The lateral wedged insole with subtalar strapping significantly reduces dynamic knee load in the medial compartment gait analysis on patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2007;15(8):932–936. doi: 10.1016/j.joca.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 48.Erhart JC, Mundermann A, Elspas B, et al. Changes in knee adduction moment, pain, and functionality with a variable-stiffness walking shoe after 6 months. J Orthop Res. 2010;28(7):873–879. doi: 10.1002/jor.21077. [DOI] [PubMed] [Google Scholar]
- 49.Erhart JC, Mundermann A, Elspas B, et al. A variable-stiffness shoe lowers the knee adduction moment in subjects with symptoms of medial compartment knee osteoarthritis. J Biomech. 2008;41(12):2720–2725. doi: 10.1016/j.jbiomech.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 50.Shakoor N, Lidtke RH, Sengupta M, et al. Effects of specialized footwear on joint loads in osteoarthritis of the knee. Arthritis Rheum. 2008;59(9):1214–1220. doi: 10.1002/art.24017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Shakoor N, Sengupta M, Foucher KC, et al. Effects of common footwear on joint loading in osteoarthritis of the knee. Arthritis Care Res (Hoboken) 2010;62(7):917–923. doi: 10.1002/acr.20165. ** The work by Shakoor and colleagues continues to show important connections between joint loading and shoe types. In this paper they compare joint loading in 5 types of footwear, and their data suggest that footwear is an important consideration in patients with knee OA.
- 52.Gelis A, Coudeyre E, Hudry C, et al. Is there an evidence-based efficacy for the use of foot orthotics in knee and hip osteoarthritis? Elaboration of French clinical practice guidelines. Joint Bone Spine. 2008;75(6):714–720. doi: 10.1016/j.jbspin.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 53.Lee YC, Shmerling RH. The benefit of nonpharmacologic therapy to treat symptomatic osteoarthritis. Curr Rheumatol Rep. 2008;10(1):5–10. doi: 10.1007/s11926-008-0002-0. [DOI] [PubMed] [Google Scholar]
- 54. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137–162. doi: 10.1016/j.joca.2007.12.013. * Using the full measure of the 'silver' level of evidence from foot wear studies, they recommend that patients with lower extremity OA receive advice regarding appropriate footwear.
- 55.Davitt JS, Kadel N, Sangeorzan BJ, et al. An association between functional second metatarsal length and midfoot arthrosis. J Bone Joint Surg Am. 2005;87(4):795–800. doi: 10.2106/JBJS.C.01238. [DOI] [PubMed] [Google Scholar]
- 56.Yu J, Cheung JT, Fan Y, et al. Development of a finite element model of female foot for high-heeled shoe design. Clin Biomech (Bristol, Avon) 2008;23:S31–S38. doi: 10.1016/j.clinbiomech.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 57.Rao S, Baumhauer JF, Becica L, Nawoczenski DA. Shoe inserts alter plantar loading and function in patients with midfoot arthritis. J Orthop Sports Phys Ther. 2009;39(7):522–531. doi: 10.2519/jospt.2009.2900. [DOI] [PubMed] [Google Scholar]
- 58. Rao S, Baumhauer JF, Tome J, Nawoczenski DA. Orthoses alter in vivo segmental foot kinematics during walking in patients with midfoot arthritis. Arch Phys Med Rehabil. 2010;91(4):608–614. doi: 10.1016/j.apmr.2009.11.027. * This important work is starting to unravel the complexities of midfoot arthritis and foot kinematics that may have implications for other conditions related to foot pain.
- 59.Dawson J, Juszczak E, Thorogood M, et al. An investigation of risk factors for symptomatic osteoarthritis of the knee in women using a life course approach. J Epidemiol Community Health. 2003;57(10):823–830. doi: 10.1136/jech.57.10.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paiva de Castro A, Rebelatto JR, Aurichio TR. The relationship between foot pain, anthropometric variables and footwear among older people. Appl Ergon. 2010;41(1):93–97. doi: 10.1016/j.apergo.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 61. Rao UB, Joseph B. The influence of footwear on the prevalence of flat foot. A survey of 2300 children. J Bone Joint Surg Br. 1992;74(4):525–527. doi: 10.1302/0301-620X.74B4.1624509. ** This study along with Sachithanandam and Joseph (1995) suggested that shoe wear in young children may effect the development of the longitudinal arch and foot structure.
- 62. Sachithanandam V, Joseph B. The influence of footwear on the prevalence of flat foot. A survey of 1846 skeletally mature persons. J Bone Joint Surg Br. 1995;77(2):254–257. ** This study along with Rao and Joseph (1992) suggested that shoe wear in young children may effect the development of the longitudinal arch and foot structure.