Abstract
Epidermolytic hyperkeratosis presents with perinuclear vacuolization of the keratinocytes in spinous and granular layers, keratinocytes with ill-defined limits, which leads to a reticulate appearance of the epidermis, an increased number of variously shaped and sized basophilic keratohyalin granules and the same sized eosinophilic trichohyalin granules, at any level of epidermis, mainly in the stratum granulosum, and compact hyperkeratosis. This minor reactive pathologic reaction pattern of skin is found in large variety of diseases. This paper is the first case report of such pattern in inflammatory linear verrucous epidermal nevus. Our case is of a 23-year-old man with pruritic verrucous lesions of trunk and extremities initiated since 13 years ago. Physical examination revealed white linear hyperkeratotic lesions, some of them on erythematous background and also classic epidermal nevus. No skeletal, ophthalmic, and nervous system involvement was detected. Microscopic study of pruritic verrucous lesions showed psoriasiform acanthosis, mild papillomatous, hyperkeratosis, and epidermolytic hyperkeratotic changes in hair follicles and acrosyrinx accompanied with moderate perivascular inflammation.
Keywords: Epidermolytic hyperkeratosis, epidermal nevus, inflammatory linear verrucous epidermal nevus
Introduction
Epidermolytic hyperkeratosis (EH) is a minor pathologic reaction pattern of skin, first described by Ackerman in 1970.[1,2] This pattern has been observed incidentally in a variety of benign and malignant skin lesions or hereditary disorders. EH has been found in tissue adjacent to and within melanocytic lesions,[3] progressive systemic sclerosis, squamous cell carcinoma, nevus comedonicus, acanthoma, follicular cyst, reactive erythema, basal cell carcinoma, melanoma, seborrheic keratoses, leukoplakia, scars, actinic keratoses, epidermoid cyst, epidermolytic acanthoma,[2] eczema nummular, solid hidradenoma, epidermal nevi, and normal epithelium of mouth and skin.[1,2,4] Accidental EH is not associated with bulla formation.[3]
Inflammatory linear verrucous epidermal nevus (ILVEN) is characterized by erythematous pruritic inflammatory lesions that occur as linear bands following Blaschko's lines. It is a clinical variant of verrucous epidermal nevus.[5]
This is the first case of follicular and acrosyringeal epidermolytic hyperkeratosis in association with ILVEN.
Case Report
Our case is a 23-year-old man referring to dermatology clinic with pruritic verrucous lesions initiated since 13 years ago.
Physical examinations revealed white linear scaly lesions; some of them were located on pruritic erythematous plaques. These lesions were on the left side of neck, shoulders, left upper and lower limbs, left axillary, back and abdominal surface, some sloughed off easily. In addition, brown linear verrucous lesions without any erythema and inflammation were detected on patient's back and left arm indicating classic epidermal nevus [Figure 1]. Family history for these lesions was negative.
Figure 1.

White linear hyperkeratotic lesions some of them on erythematosus background and brown linear verrucous lesions without any erythema and inflammation
There was no history of seizure and developmental psychomotor disorders. To assess skeletal, ophthalmic and neurologic co-morbidities, several consultations were performed which had no significant findings.
Microscopic studies showed psoriasiform acanthosis, mild papillomatosis, hyperkeratosis, and epidermolytic hyperkeratosis changes involving hair follicles and acrosyrinx with moderate dermal perivascular inflammation [Figures 2 and 3].
Figure 2.
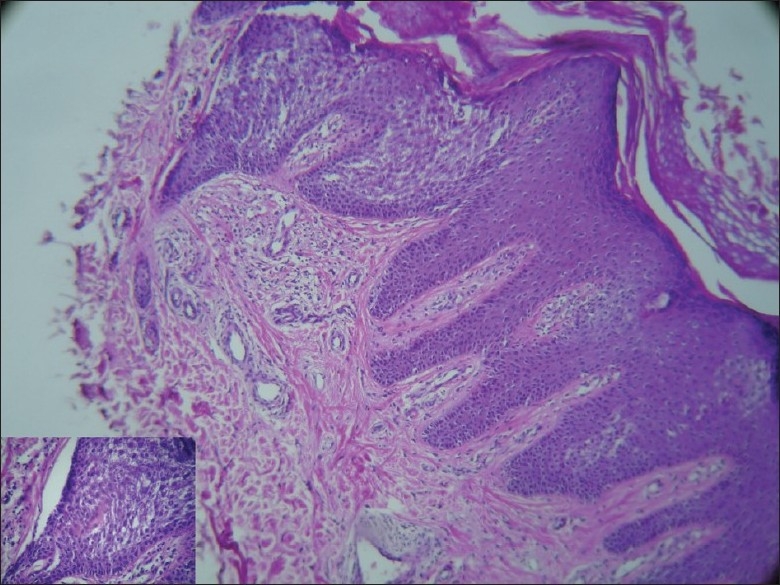
Psoriasiform acanthosis, mild papillomatosis, hyperkeratosis with foci of parakeratosis and epidermolytic hyperkeratosis change in acrosyrinx and moderate perivascular lymphohistiocytes infiltrate
Figure 3.

Epidermolytic hyperkeratosis: vacuolization of the upper and mid spinous layer in acrotrichia
Discussion
Inflammatory linear verrucous epidermal nevus (ILVEN) is an uncommon cutaneous lesion described in 1971 by Altman and Mehregan as a distinct clinical type of linear verrucous nevus.[5] About 6% of all epidermal nevi are ILVEN.[6,7] The lesions consisted of pruritic, erythematous, hyperkeratotic, linear plaques, distributed unilaterally with greater involvement of the left side.[4,6,8,9]
It is often present at birth or develops within the first 6 months of life.[8,9] Also, it can be initiated in adulthood.[10] It is more common in females (male to female ratio is 1:4)[5,6] and may be familial in some cases.[5,8,11]
The distribution is almost exclusively on the lower half of the body, and the buttock is the most frequently involved area.[7,12] Only 16% of lesions were found on the upper half of the body, including the axillae, arm, and hand.[7] A case of ILVEN was also reported on the head.[7]
The cause and pathogenesis of ILVEN are unknown. ILVEN is thought to be associated with upregulation of interleukin 1, interleukin 6, tumor necrosis factor-[alpha], and intercellular adhesion molecule 1.[5] Infection may be a trigger for the clonal inflammation in both ILVEN. The linear arrangement possibly reflects somatic mosaicism for a gene.[9] Epidermal verrucous nevi represent a proliferation of keratinocytes or adnexal epithelium that arise from the pluripotent cells in the germinal layer of the embryonic ectoderm.[5] In a few cases, the association of ILVEN with arthritis and with autoimmune lymphocytic thyroiditis makes also an immune involvement seem probable.[8–10]
Sotiriadis et al. proposed that ILVEN might be a form of linear psoriasis.[9] But, its resistance to standard treatment, and severe pruritus, may help to distinguish it clinically from psoriasis.[6] Patients with ILVEN are susceptible to psoriasis or have a family history of it.[9] A skin biopsy may be necessary to distinguish ILVEN from psoriasis.[6]
The classic clinical criteria for the diagnosis of ILVEN are: (1) unilateral, pruritic linear verrucous eruption; (2) early age of onset; and (3) resistance to treatment.[13,14] A typical presentations include widespread, bilateral distribution, and relatively late onset in adulthood.[5,15]
There are two different histopathological features for ILVEN: nonspecific and specific. Areas of depressed hypergranulosis and overlying orthokeratosis alternating sharply with areas of agranulosis and overlying parakeratosis are specific features. They are not always evident in biopsy specimens, and therefore, are not pathognomonic.[5,15] The nonspecific findings includes an inflammatory dermal infiltrate, acanthosis, and papillomatosis of the psoriasis type with elongation of the epidermal ridges.[5] Microabscesses of Munro, typically found in psoriasis, can be found in ILVEN as well.[9]
EH and focal acantholytic dyskeratosis may be prominent features of epidermal nevi. Five to ten percent of verrucous epidermal nevi show EH,[16] which may be observed clinically with skin fragility and sloughed off areas.[17] This type tends to be more warty.[6]
The characteristic histologic features of EH include: (1) perinuclear vacuolization of the keratinocytes in spinous and granular layers, (2) keratinocytes with ill-defined limits which leads to a reticulate appearance of the epidermis, (3) an increased number of variously shaped and sized basophilic keratohyalin granules and the same sized eosinophilic trichohyalin granules, at any level of epidermis, mainly in the stratum granulosum and sparing the basal layer, and (4) compact hyperkeratosis.[3,16]
Electron microscopic examination of EH shows (1) endoplasmic reticulum, ribonucleoprotein particles and keratinosomes in the perinuclear areas of the granular and spinous layers of the epidermis, (2) prominent mitochondria in the upper stratum granulosum, and (3) binucleated cells in the spinous and granular layers.[2]
Different types of epidermal nevi may occur simultaneously in a patient. As mentioned above, our case showed classic epidermal nevi and ILVEN at the same time.
Erythema and pruritus in clinic, and inflammation and parakeratosis in microscopy differentiate ILVEN from classic epidermal nevi. Although the dermis is not typically involved in epidermal nevi, lichenoid or superficial perivascular lymphocytic inflammation may be present.[18]
Our case presented with perivascular inflammation in addition to parakeratosis, papillomatous and psoriasiform changes, all indicating ILVEN. Epidermolytic changes were found around the hair infundibula and acrosyrinx. Epidermolytic hyperkeratosis with involvement of the follicular epithelium and the sebaceous duct is reported in patients with linear comedonicus nevus and nevoid follicular epidermolytic hyperkeratosis.[4,19,20]
Although lymphohistiocytic infiltration was seen in the dermis, but absence of histiocytes with foamy cytoplasm or Munro microabscess, and clinical presentations such as pruritus and lack of limb defects ruled out CHILD syndrome.[18]
ILVEN should be clinically and histologically distinguished from linear nevoid psoriasis, seborrheic keratoses, verruca vulgaris, verruciform acrokeratosis, lichen striatus, and ichthyosis.
Linear nevoid psoriasis is an uncommon type of psoriasis presenting with mild pruritus, which is often effectively treated. Although reports about congenital cases are available,[5,6] but it is thought that most young individuals previously diagnosed with “linear psoriasis” may actually have ILVEN.[8,9] There are cases of coexisting ILVEN and psoriasis and also ILVEN may predispose to the development of psoriasis.[8]
Elevated foci of parakeratosis with agranulosis alternating with depressed foci of orthokeratosis with hypergranulosis and increased expression of involucrin only of the orthokeratotic areas of the epidermis are findings that in some cases can be helpful in the differential diagnosis. However, they are not absolute diagnostic criteria.[9] Vissers et al. have mentioned that increased expression of cytokeratin 10 (CK10) is suggestive for ILVEN.[11] Nonetheless, the age of onset, pruritus, chronicity of the lesions, and resistance to anti psoriatic drugs help to distinguish the two conditions.[8]
The main suggested treatments for ILVEN include topical agents such as calcipotriol,[21] 5-fluorouracil, tretinoin, dermabrasion, cryotherapy, laser, and partial thickness excision.[5]
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Hutcheson AC, Nietert PJ, Maize JC. Incidental epidermolytic hyperkeratosis and focal acantholytic dyskeratosis in common acquired melanocytic nevi and atypical melanocytic lesions. J Am Acad Dermatol. 2004;50:388–90. doi: 10.1016/s0190-9622(03)02736-1. [DOI] [PubMed] [Google Scholar]
- 2.Steele CL, Shea CR, Petronic-Rosic V. Epidermolytic hyperkeratosis within infundibular cysts. J Cutan Pathol. 2007;34:360–2. doi: 10.1111/j.1600-0560.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 3.Conlin PA, Rapini RP. Epidermolytic hyperkeratosis associated with melanocytic nevi. Am J Dermatopathol. 2002;24:23–5. doi: 10.1097/00000372-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Ross R, DiGiovanna JJ, Capaldi L, Argenyi Z, Fleckman P, Robinson-Bostom L. Histopathologic characterization of epidermolytic hyperkeratosis: A systematic review of histology from the National Registry for Ichthyosis and Related Skin Disorders. J Am Acad Dermatol. 2008;59:86–90. doi: 10.1016/j.jaad.2008.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee BJ, Mancini AJ, Renucci J, Paller AS, Bauer BS. Full-thickness surgical excision for the treatment of inflammatory linear verrucous epidermal nevus. Ann Plast Surg. 2001;47:285–92. doi: 10.1097/00000637-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Sugarman JL. Epidermal nevus syndromes. Semin Cutan Med Surg. 2007;26:221–30. doi: 10.1016/j.sder.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Chatproedprai S, Wananukul S, Prasarnnaem T, Noppakun N. Epidermal nevus syndrome. Int J Dermatol. 2007;46:858–60. doi: 10.1111/j.1365-4632.2007.03085.x. [DOI] [PubMed] [Google Scholar]
- 8.Al-Enezi S, Huber AM, Krafchik BR, Laxer RM. Inflammatory linear verrucous epidermal nevus and arthritis: A new association. J Pediatr. 2001;138:602–4. doi: 10.1067/mpd.2001.112173. [DOI] [PubMed] [Google Scholar]
- 9.Sotiriadis D, Patsatsi A, Lazaridou E, Kastanis A, Devliotou-Panagiotidou D. Is inflammatory linear verrucous epidermal naevus a form of linear naevoid psoriasis? J Eur Acad Dermatol Venereol. 2006;20:483–4. doi: 10.1111/j.1468-3083.2006.01481.x. [DOI] [PubMed] [Google Scholar]
- 10.Kosann MK. Inflammatory linear verrucous epidermal nevus. Dermatol Online J. 2002;9:15. [PubMed] [Google Scholar]
- 11.Mazereeuw-Hautier J, Marty C, Bonafé JL. Familial inflammatory linear verrucous epidermal naevus in a father and daughter. Clin Exp Dermatol. 2008;33:679–80. doi: 10.1111/j.1365-2230.2007.02666.x. [DOI] [PubMed] [Google Scholar]
- 12.Lee SH, Rogers M. Inflammatory linear verrucous epidermal naevi: A review of 23 cases. Astralas J Dermatol. 2001;42:252–6. doi: 10.1046/j.1440-0960.2001.00530.x. [DOI] [PubMed] [Google Scholar]
- 13.Altman J, Mehregan AH. Inflammatory linear verrucose epidermal nevus. Arch Dermatol. 1971;104:385–9. [PubMed] [Google Scholar]
- 14.Morag C, Metzker A. Inflammatory linear verrucous epidermal nevus: Report of seven new cases and review of the literature. Pediatr Dermatol. 1985;3:15–8. doi: 10.1111/j.1525-1470.1985.tb00479.x. [DOI] [PubMed] [Google Scholar]
- 15.Vissers WH, Muys L, Van Erp PE, de Jong EM, van de Kerkhof PC. Immunohistochemical differentiation between inflammatory linear verrucous epidermal nevus (ILVEN) and psoriasis. Eur J Dermatol. 2004;14:216–20. [PubMed] [Google Scholar]
- 16.Sarifakioglu E, Yenidunya S. Linear epidermolytic verrucous epidermal nevus of the male genitalia. Pediatr Dermatol. 2007;24:447–8. doi: 10.1111/j.1525-1470.2007.00481.x. [DOI] [PubMed] [Google Scholar]
- 17.Ogunbiyi AO, Ogunbiyi JO. Nevus depigmentosus and inflammatory linear epidermal nevus-an unusual combination with a note on histology. Int J Dermatol. 1998;37:600–2. doi: 10.1046/j.1365-4362.1998.00057.x. [DOI] [PubMed] [Google Scholar]
- 18.Brenn T, McKee PH. Tumors of the surface epithelium. In: Mckee PH, Calonje E, Granter SR, editors. Pathology of the skin with clinical correlations. 3th ed. China: Mosby Elsevier; 2005. pp. 1153–6. [Google Scholar]
- 19.Schecter AK, Lester B, Pan TD, Robinson-Bostom L. Linear nevus comedonicus with epidermolytic hyperkeratosis. J Cutan Pathol. 2004;31:502–5. doi: 10.1111/j.0303-6987.2004.00206.x. [DOI] [PubMed] [Google Scholar]
- 20.Plewig G, Christophers E. Nevoid follicular epidermolytic hyperkeratosis. Arch Dermatol. 1975;111:223–6. [PubMed] [Google Scholar]
- 21.Böhm I, Bieber T, Bauer R. Successful therapy of an ILVEN in a 7-year-old girl with calcipotriol Hautarzt. 1999;50:812–4. doi: 10.1007/s001050050990. [DOI] [PubMed] [Google Scholar]


