Abstract
Tuberculosis has been a well-known affliction of human kind, since antiquity. Cutaneous tuberculosis constitutes only a small proportion of extra pulmonary tuberculosis and multifocal involvement of cutaneous tuberculosis is an even rarer manifestation. We report one such case of multifocal tuberculosis verrucosa cutis in a 17-year old male patient in the absence of any primary tuberculous focus.
Keywords: Multifocal, cutaneous, tuberculosis
Introduction
Tuberculosis is an ancient disease and Mycobacterium tuberculosis, the microorganism responsible for it, was identified over 100 years ago. Cutaneous tuberculosis constitutes only a small proportion of extra pulmonary tuberculosis.
Tuberculosis verrucosa cutis (TBVC), also known as warty tuberculosis,[1] anatomist's wart or prosector's wart is characterized by the presence of verrucous plaque-like lesions, due to direct inoculation of the organism into the skin of a previously infected patient. Hematogenous,[2] tumor-like,[3] and exuberant granulomatous[4] forms have also been described. In India, the incidence of cutaneous tuberculosis has fallen from 2% to 0.15% and is rare in developed countries.[5]
Case Report
A 17-year-old male cattleherd presented with multiple skin lesions of his left foot of 2 years duration. The lesion initially started in the instep of the left foot as an itchy papule, which later enlarged to form a painful verrucous plaque [Figure 1]. A year later, he noticed similar lesions in the lateral aspect of the same foot. On examination, multiple verrucous, oozy plaques were present on the inner dorsal and lateral aspect of left foot [Figure 2]. Size of foot lesions ranged from 2 × 2 cm to 7 × 3 cm. Linear lesions were present on the lateral aspect of the foot. Base of the lesion was not fixed to deeper structures and satellite papules were present around the plaques.
Figure 1.

Hypertrophic plaque in the instep of left foot
Figure 2.

Multiple hypertrophic verrucous plaques in the dorsum and lateral aspect of left foot
Routine blood investigations and chest radiographs were within normal limits. Mantoux test measured 17 × 15 mm in size. Ten percent potassium hydroxide smear preparation was negative for fungus. Radiographs of the foot showed only soft-tissue swelling without bony involvement. Biopsy from the foot lesion was consistent with TBVC, with marked hypertrophy of the epidermis and mid-dermal granulomata with Langhans giant cells [Figures 3 and 4]. Patient was diagnosed as having TBVC. He was started on isoniazid, rifampicin, ethambutol, and pyrizinamide, daily for 2 months, followed by isoniazid and rifampicin for 4 months. Within three months, lesions flattened out [Figures 5 and 6] and at the end of 6 months all the lesions completely resolved.
Figure 3.
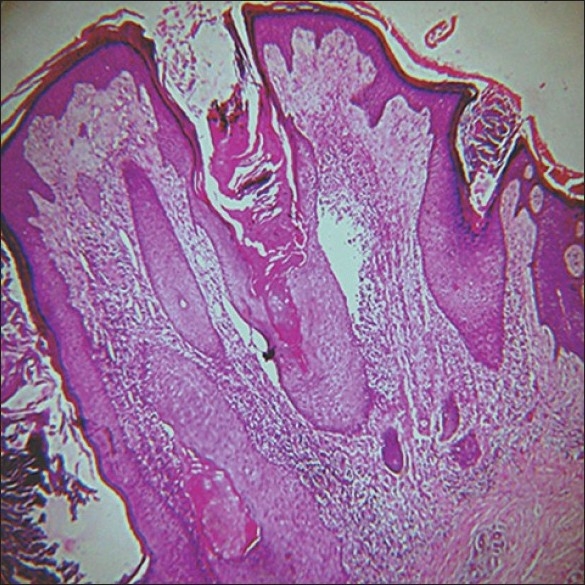
Section on 20× magnification showing hyperkeratosis, acanthosis, papillomatosis with mid dermal granulomata
Figure 4.
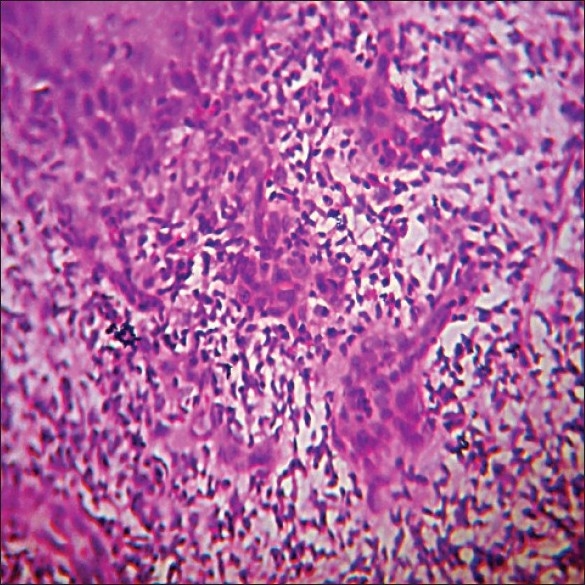
Section on 40× magnification showing epitheloid granuloma with lymphocytic infiltrate and dermal edema
Figure 5.

Resolved lesions at 3 months
Figure 6.

Resolved lesions at 3 months
Discussion
The symptoms of mycobacterial infections depend mainly on the route of transmission, the pathogenicity and drug resistance of the bacteria, the immune status of the host and various local factors. Percutaneous transmission leading to cutaneous tubercular manifestations is becoming very common.[6,7] Cutaneous tuberculosis, is perceived to form a continuous spectrum, with lupus vulgaris and TBVC at one end and scrofu-loderma and tuberculosis cutis orificialis at the other, corresponding to a declining cell-mediated immunity across the spectrum.
TBVC, a verrucous form of cutaneous tuberculosis results from inoculation of tubercle bacilli into the skin of a previously infected patient with moderate to high degree of immunity.[8] The diagnosis of TBVC is based on history, evolution of the disease, cardinal morphological features and histopathological characteristics. Pulmonary tuberculosis can spread to distant or contiguous sites. The most common site of occurrence is the lower limbs and this can be substantiated by a clinico-pathological and epidemiological study conducted by Padmavathy et al. on 71 patients.[9] However, multifocal cutaneous lesions without any other tubercular focus in the body are quite rare. Prasad et al. in 2002 reported a similar case with multifocal involvement.[10] Such a case is even more unusual as there was no evidence of immune competence. The multifocal pattern of the disease in this patient may be attributed to multiple sites of entry of the organism, without a pulmonary focus. Moreover, patient tends cattle; this may explain the anthropo-zoonotic[11] transmission of the organism, due to unnoticed microtrauma.
Combination of different types of cutaneous TB has been reported, but this multifocal involvement of the same limb is a rare entity. Such rare occurrences should prompt the dermatologist to look for other associations and should be reported.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Grange JM, Noble WC, Yates MD, Collins CH. Inoculation mycobacterioses. Clin Exp Dermatol. 1988;13:211–20. doi: 10.1111/j.1365-2230.1988.tb00682.x. [DOI] [PubMed] [Google Scholar]
- 2.Irgang S. Ulcerative cutaneous lesions in sarcoidosis. Br J Dermatol. 1955;67:255–60. doi: 10.1111/j.1365-2133.1955.tb12731.x. [DOI] [PubMed] [Google Scholar]
- 3.Iizwa O, Aiba S, Tagami H. Tuberculosis verrucosa cutis in a tumour like form. Br J Dermatol. 1991;125:79–80. doi: 10.1111/j.1365-2133.1991.tb06047.x. [DOI] [PubMed] [Google Scholar]
- 4.Wong KO, Lee KP, Chin SF. Tuberculosis of the skin in Hong kong. Br J Dermatol. 1968;80:424–9. doi: 10.1111/j.1365-2133.1968.tb11977.x. [DOI] [PubMed] [Google Scholar]
- 5.Gopinathan R, Pandit D, Joshi J, Jerajani H, Mathur M. Clinical and morphological variants of cutaneous tuberculosis and its relation to mycobacterium species. Indian J Med Microbiol. 2001;19:193–6. [PubMed] [Google Scholar]
- 6.Chowdhury MM, Varma S, Howell S, Holt PJ, Statham BN. Facial cutaneous tuberculosis: an unusual presentation. Clin Exp Dermatol. 2000;25:48–50. doi: 10.1046/j.1365-2230.2000.00572.x. [DOI] [PubMed] [Google Scholar]
- 7.De Jong JW, van Altena R. Non-respiratory tuberculosis with Mycobacterium tuberculosis after penetrating lesions of the skin: five case histories. Int J Tuberc Lung Dis. 2000;4:1184–87. [PubMed] [Google Scholar]
- 8.Sehgal VN, Wagh SA. Cutaneous tuberculosis: Current concepts. Int J Dermatol. 1990;29:237–52. doi: 10.1111/j.1365-4362.1990.tb02554.x. [DOI] [PubMed] [Google Scholar]
- 9.Padmavathy L, Lakshmana Rao L, Pari T, Ethirajan N, Krishnaswamy B. Lupus vulgaris and tuberculosis verrucosa cutis: Clinicopathological study of 71 patients. Indian J Tub. 2008;55:203–9. [PubMed] [Google Scholar]
- 10.Prasad P.V.S, Ambujam S, Paul Elizebeth K, Krishnasamy B, Veliath A J. Multifocal tuberculosis verrucosa cutis: An unusual presentation. Indian J Tub. 2002;49:229. [Google Scholar]
- 11.Montali RJ, Mikota SK, Cheng LI. Mycobacterium tuberculosis in zoo and wildlife species. Rev Sci Tech. 2001;20:291–303. doi: 10.20506/rst.20.1.1268. [DOI] [PubMed] [Google Scholar]


