Abstract
A descriptive study was conducted to determine the information needs of American Indian (AI) and Alaska Native (AN) cancer survivors and assess satisfaction with and acceptability of telehealth support group services for cancer survivors in AI and AN rural communities. AI and AN cancer survivors were asked to complete the Telehealth Satisfaction Survey and two open-ended questions, one regarding information needs and one seeking comments and suggestions about cancer support group meetings. Thirty-two surveys were returned. Information about nutrition during treatment and treatment-related side effects were the most sought after topics. Participants valued the opportunity to interact with other AI and AN cancer survivors who also lived in remote locations and the usefulness of the information presented. The link with geographically distant survivors was valuable to participants as they felt they were no longer alone in their cancer experiences. Determining survivors’ information needs provides meaningful topics for future support group education. Telehealth is a viable way to facilitate cancer support groups to AI and AN cancer survivors in rural communities.
Support groups for people with cancer are a well-documented, evidence-based intervention for dealing with the psychological effects of a cancer diagnosis and treatment and for providing information for follow-up care (Andersen, 2002; Classen et al., 2001; Dolbeault et al., 2009; Fobair et al., 2002; Gottlieb & Wachala, 2007). Support group participants report gaining a sense of community and unconditional acceptance in addition to receiving information about their cancer, treatment, and self-care (Ussher, Kirsten, Butow, & Sandoval, 2006). However, support groups for people with cancer often are not available in rural areas, particularly in rural American Indian (AI) and Alaska Native (AN) communities (U.S. Department of Health and Social Services, 2006). The purpose of this program evaluation is to determine the information needs of AI and AN cancer survivors living in rural communities and to explore these survivors’ satisfaction with telehealth facilitation of support group meetings.
Access to Support Groups in Rural Communities
Rural residents usually travel great distances to receive cancer treatment. For example, residents in rural western Washington frequently obtain specialty and subspecialty health care in Seattle. Their trips often require two to five hours of travel by automobile and ferry or by small aircraft, with round-trip costs ranging from $50–$200 (Olson & Simmons, 2005). In Alaska, many rural communities are separated by vast mountain ranges, stretches of tundra, glaciers, impassable river systems, and open waters, with 80% of AN villages not linked by a road system. The distance from many Alaskan communities to the nearest medical facility is comparable to the distance from New York to Chicago. Travel costs for these rural patients to access services not available at rural tribal clinics are substantial, ranging from $100–$1,200 (U.S. Department of Health and Human Services, Indian Health Services, 2010). The combination of travel costs, loss of income from missed work, and childcare costs can create a large economic burden for rural patients receiving health care in an urban setting.
Telehealth holds promise as a new strategy to address follow-up care and quality-of-life needs for rural cancer survivors. This modality can bridge geographic distance and increase access to care in rural settings. Several studies have demonstrated high levels of participation and satisfaction with cancer support groups conducted over the telephone or Internet (O’Brien, Harris, King, & O’Brien, 2008; Winzelberg et al., 2003). In addition, the feasibility of using videoconferencing to facilitate support groups for people with cancer in rural areas has been studied with 27 women with breast cancer in north-eastern California (Collie et al., 2007). The women showed a clinically significant improvement in depression and in symptoms of post-traumatic stress disorder. In Lounsberry, Macrae, Angen, Hoeber, and Carlson (2009), videoconferencing was used to facilitate support groups for 19 allogeneic hematopoietic stem cell transplantation survivors across Canada. Participants reported positive reactions to the support group experience.
Cancer Prevalence
Cancer is the second-leading cause of death for AIs older than age 45 (U.S. Department of Health and Human Services, Indian Health Services, 2010) and the leading cause of death for ANs older than age 45 (Lanier, Kelly, Maxwell, McEvoy, & Homan, 2006). Based on data from the National Cancer Institute, the Centers for Disease Control and Prevention, and the North American Association of Central Cancer Registries, and mortality data from the National Center for Health Statistics, cancer incidence rates show a decrease in all races in both men and women except AI and AN women, for whom rates were stable (Jemal, Siegel, Xu, & Ward, 2010). Among AIs and ANs living in Indian Health Services Contract Health Service Delivery Areas, incidence and mortality rates decreased in men but remained stable in women from 1997–2006 (Edwards et al., 2010). Breast, colorectal, lung, and uterine cancer were among the top five cancers among AI and AN women (Wingo et al., 2008).
The cancer-related health disparities experienced by AI and AN communities are among the most striking of any minority group in the United States and are largely attributable to poverty, economic oppression, lack of access to continuous high-quality care, and lack of opportunities for health-promoting behaviors (Burhansstipanov, 2005; Burhansstipanov & Hollow, 2001; Institute of Medicine, 2002; Warne, 2006). Many AIs and ANs live on reservation lands or in remote rural areas and their primary health care is provided either by a tribe-operated health program or by the Indian Health Service (Wiggins et al., 2008). After receiving cancer treatment in an urban center, many AIs and ANs return to their home communities and reenter healthcare systems that are overburdened and severely underfunded (President’s Cancer Panel, 2003). As AI and AN cancer survivors transition from active treatment to follow-up care in rural home communities, the need for local support arises. The Institute of Medicine concluded that comprehensive, coordinated, long-term support of cancer survivors was the exception rather than the norm in the United States, particularly for rural AI and AN cancer survivors (Hewitt, Greenfield, & Stovall, 2006).
American Indian and Alaska Native Cancer Survivor Issues
In Native American Cancer Survivors’ Support Circles, a California-based project, survivors selected topics to be presented at support circles to ensure that the topics were relevant to urban- and rural-based AI survivors (Weiner, Burhansstipanov, Krebs, & Restivo, 2005). The topics selected included providing an overview of cancer among AIs; sharing personal reactions to cancer treatments; discussing cancer with providers; talking with family about the cancer experience; discussing dreams; and learning about diet, nutrition, and exercise. The survivors also chose the format for a ceremony at the end of each circle meeting. Survivors attending the National Native American Cancer Survivors’/Thrivers’ Conference (Pelusi & Krebs, 2005) identified other pertinent issues for support group topics, including palliative care, common drug side effects, peripheral neuropathy, the ability to concentrate and comprehend, how to obtain second opinions, and how to access screening, treatment, and education.
In summary, among AIs and ANs, a number of cancer health disparities exist. One of the disparities is a lack of access to culturally congruent cancer support groups for rural AIs and ANs. Understanding the information needs of AIs and ANs would provide valuable information about what topics are relevant for AI and AN cancer survivors. In addition, videoconferencing has been used with success to facilitate support groups; however, the satisfaction with videoconferencing has yet to be explored among rural AI and AN cancer survivors. Therefore, the authors also wanted to evaluate the satisfaction with facilitation of support group meetings via videoconferencing.
Methods
The authors used a cross-sectional, descriptive study design to survey AI and AN cancer survivors living in rural communities to provide an evaluation of support group programs, the survivors’ information needs, and the use of telehealth to facilitate support group meetings. Approval was granted from the appropriate tribal bodies and the human subjects committee of the participating university.
Support Group Sites
Twelve support group meetings were conducted from February 2008 to September 2009. The groups took breaks for winter holidays and summer activities. Altogether, 25 rural tribal sites in Washington and Alaska participated, with a mean of six sites participating in each meeting. Attendance from several sites ranged from 6–57 survivors per support group meeting, with a mean of 36 survivors joining each meeting. Survivor attendance at each site ranged from 2–11 individuals. The distance from each remote site to the nearest available in-person support group ranged from 39–1,190 miles. Three sites were not linked by a road system and air travel was the only way to reach the nearest in-person support group. Four additional sites had connecting roads, but they were passable for only a few months out of the year. From these sites, travel by road to the nearest in-person support group would take more than 24 hours.
The remote sites were hosted by individual AI and AN communities. Each support group meeting was led by a facilitator located at one of three different urban sites: the Alaska Native Tribal Health Consortium in Anchorage, the University of Washington in Seattle, and the Fred Hutchinson Cancer Research Center in Seattle. Videoconference equipment was most commonly set up in a rural tribal clinic conference room where participants could join group meetings. Some of the local support group coordinators were trained to use the videoconferencing equipment while other sites had information technology staff available to help set up the equipment. A technical expert at the university site also was available to help with technologic issues. Ethical considerations (i.e., patient confidentiality in regard to being viewed on a television screen) regarding the use of telehealth technology are addressed in Demiris, Doorenbos, and Towle (2009).
Support Group Content
Support group meetings lasted two hours and usually were held monthly. Participants included survivors, their caregivers, and family members. At each site, a local support group coordinator participated in the meeting; some of the coordinators were trained professionals (e.g., nurses, social workers) and others were local tribal members who were cancer survivors. The content of the meetings varied and included group counseling, education programs such as modules from Cancer 101: A Cancer Education and Training Program for American Indians and Alaska Natives (Hill et al., 2010), and other educational presentations by content experts.
Developed in 2002, Cancer 101 was the result of collaborations among the Northwest Portland Area Indian Health Board, Spirit of EAGLES (Education, Advocacy, Grants, Leadership, Elders, and Survivors) and the National Cancer Institute-sponsored Cancer Information Service—Northwest Region (Hill et al., 2010). Cancer 101 can be adapted to meet an individual survivor’s needs and is targeted at community members and staff and community health representatives of the Indian Health Service. The curriculum includes seven learning modules that cover (a) an overview of cancer concerns among AI and AN populations, (b) a basic explanation of cancer, (c) cancer screening and early detection, (d) cancer diagnosis and staging, (e) cancer risks and risk reduction, (f) the basics of cancer treatment, and (g) support for patients and caregivers. Each learning module can be presented in 30–40 minutes.
Other topics for the program’s support group meetings were determined by asking participants at the first meeting to identify desired education offerings. Responses included presentations by content experts about pain management, psychological support, and clinical and legal end-of-life issues.
At each site, a video teleconferencing system was used to join the support group meetings. All sites dialed into a video teleconferencing bridge, which connected all of the sites together simultaneously to create a multipoint conference. At each site, the video teleconferencing equipment, which includes a camera to capture the images of the participants in the room, is connected to a television monitor through which participants could watch and listen to the presentation and discussion. A voice-activated system was used so that the bridge automatically captured the image from the site where a participant was speaking. So, for example, during the didactic portion of the meeting, all sites and participants could see the speaker as he or she presented from the host site. However, during the discussion portion of the meeting, the bridge automatically switched to capture the image of whomever spoke, no matter if that individual was at the host site or one of the participant sites. Participating sites connected to the bridge either via ISDN lines or an Internet connection. Through interactions over a course of several months, participants from western Washington and throughout Alaska began to develop a level of comfort and trust with each other.
Procedures
After the fifth support group meeting, support group coordinators approached a convenience sample of the 50 survivors who attended that meeting and asked if they would complete a survey. The survey was administrated online, by telephone, in person, or by mail to allow for maximum participation and to accommodate varying literacy levels. The survey consisted of demographic questions, the Telehealth Satisfaction Survey (Health Canada, 2007), and two open-ended questions. The Telehealth Satisfaction Survey consists of six Likert-type items with a range from lowest (1) to highest (5) satisfaction with telehealth. Two additional items asked about the distance and time needed to attend a support group meeting not conducted via telehealth. Of the two open-ended questions, one asked participants what topics they would like to learn more about and the other asked for comments or suggestions about the support group meetings.
Analysis
The authors used descriptive statistics, including counts and percentages for binary and categorically scored data, and means and standard deviations for continuously scored data. All analyses were conducted using SPSS® Statistics, version 18.0. The authors analyzed responses to the open-ended questions using a topical data analysis technique (Sandelowski & Barroso, 2003). Atlas/ti®, version 6.0, was used for data management and analysis, to develop an initial coding scheme, and to augment the scheme with additional codes identified from responses. Responses were independently coded by two investigators who met to discuss the codes and differences in application. Discrepancies were resolved through discussion and agreement between the coders. After the initial round of coding was completed, two investigators generated reports on the broad domains of interest and then read the coded responses to identify the range of responses within each domain (Ayres, Kavanaugh, & Knafl, 2003). To ensure the trustworthiness of the analysis, the authors shared interpretations of the responses with the participants, obtained feedback, and adjusted the summary to include participants’ comments and recommendations.
Results
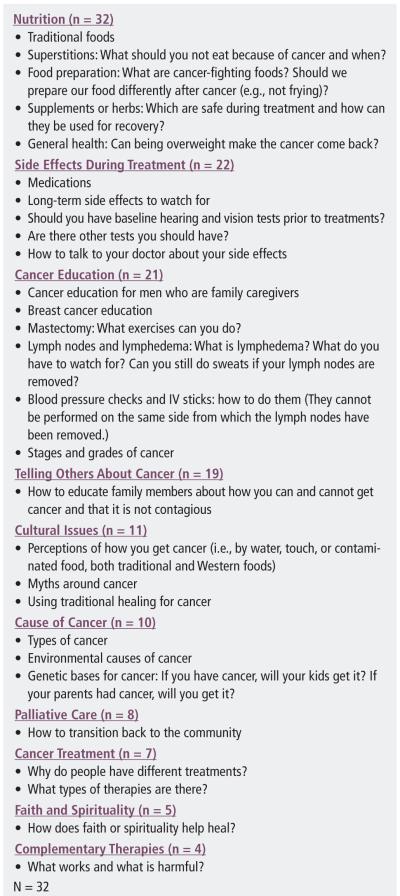
Thirty-two out of 50 (64%) AI and AN cancer survivors returned the survey. The mean age of respondents was 53 ± 11 years. All of the respondents in this program evaluation were women, 20 (63%) were married, and 27 (84%) had completed high school. Twenty-seven survey participants (84%) had a diagnosis of latestage cancer, with 11 (34%) reporting breast and 9 (28%) lung cancer. Various other types of cancer also were reported (38%; n = 12). Figure 1 shows the top 10 informational needs identified by the survey. Nutrition, identified by 100% of survey participants, was the information need of greatest interest. Related topics included food preparation, food superstitions, and foods to eat during cancer treatment. Other top informational needs were side effects during treatment, general cancer education, and cultural issues related to cancer. Responses to items on the Telehealth Satisfaction Survey are shown in Table 1. Participants reported a high level of satisfaction with the facilitation of support group meetings by videoconference. Participants reported greatest satisfaction with the ability to interact with AI and AN cancer survivors from other rural tribal communities in Washington and Alaska.
Figure 1.
Top Informational Needs and Sample Responses of American Indian and Alaska Native Cancer Survivors
Table 1.
Telehealth Satisfaction Survey Responses
| VARIABLE | X̄ | SD |
|---|---|---|
| Sound quality | 3.97 | 0.47 |
| Comfort with asking questions via telehealth (N = 20) | 4 | 0 |
| Picture quality | 4.03 | 0.78 |
| Satisfaction with telehealth | 4.59 | 0.5 |
| Usefulness of information presented | 4.75 | 0.44 |
| Value of opportunity to interact with American Indian and Alaska Native cancer survivors from other communities |
4.97 | 0.18 |
N = 32 unless otherwise indicated
Note. Scores range from 1 (lowest) to 5 (highest).
Discussion
Information Needs
Determining the information needs of AI and AN cancer survivors is important for planning support groups that will be relevant and useful. The Cancer 101 curriculum covers most of the top 10 information needs identified by participants, including general cancer education, causes of cancer, cancer treatment, and side effects during treatment. Additional education topics requested by participants included nutrition, cultural issues, faith and spirituality, telling others about cancer, palliative care, and complementary therapies. Nutrition was the top information need identified by the participants as well as by previous research with support group participants (Weiner et al., 2005). Support group participants from Weiner et al. (2005) also identified a need for information on talking with family about the cancer experience, which matches the current study’s participants’ request for information on how to tell others about cancer. The findings suggest that developing Cancer 101 learning modules on nutrition and on communicating about cancer may benefit AI and AN support groups who use the program. Another topic that may benefit AI and AN cancer survivors is palliative care, which also was identified as an information need by survivors attending the national Native American Cancer Survivors’/Thrivers’ Conference (Pelusi & Krebs, 2005). The participants in the current study identified additional information needs around culture, complementary therapies, and faith and spirituality.
Satisfaction With Telehealth
Overall, program participants were satisfied with the telehealth facilitation of support groups. Connecting with other cancer survivors was very valuable to the participants, perhaps because in small, isolated rural communities, survivors typically are few in number. By seeing and hearing other AI and AN cancer survivors, participants realized they were not alone. The results are consistent with those reported for other cancer support groups facilitated by videoconference (Collie et al., 2007; Lounsberry et al., 2009). In addition, participants were satisfied with the audiovisual quality of the videoconferences. The presence of an on-site support group coordinator who was knowledgeable about the technology may have enhanced satisfaction.
Participants
All of the support group participants were women. This program’s lack of male participants may be related to cultural differences in self-expression or to discomfort with mixed-gender groups. Based on participant feedback, the Native American Cancer Survivors’ Support Circles convened circles of men and women separately to protect modesty and privacy (Weiner et al., 2005). Other studies have found that female AI cancer survivors relied on more expressive types of social support than did male AI cancer survivors (Bauer, Englert, Michalek, Canfield, & Mahoney, 2005). However, gender differences in support group participation also have been reported in studies among predominantly Caucasian, middle-class, educated, and younger participants (Gottlieb & Wachala, 2007; Sherman et al., 2008).
The types of cancer reported by survivors participating in the support groups appeared to represent those of the greater AI and AN population. The most common diagnoses, breast and lung cancer, also are among the most common cancers in AI women in all regions of the United States except the Southwest (Wiggins et al., 2008). The late stage of diagnosis prevalent among participants reflects national statistics that AI and AN women are commonly diagnosed with late-stage cancers.
Limitations
This program evaluation has several notable limitations. First, the survey sample was small and included AI and AN cancer survivors from only two states, so findings may not be applicable to the broader AI cancer survivor community. In addition, the well-known shortcomings of self-reported data can result in biases from the ordering of questions, questions being misunderstood, and inaccurate responses; self-reported survey data may not capture the essence of complex experiences or issues (Polit & Beck, 2008). Also, the participating support group participants were self-selected and, therefore, not representative of national AI and AN populations. Research on self-selected cancer support group participants has found that participants tend to be more optimistic and, therefore, more likely to benefit from a group experience than patients with cancer who do not participate in support groups (Shou, Ekeberg, Karesen, & Sorensen, 2008). Self-selected participants also may be more comfortable with technology than those who choose not to participate (Lounsberry et al., 2009). Lastly, this program evaluation reflects only female AI and AN cancer survivors’ information needs and satisfaction with telehealth; therefore, the authors’ findings are applicable only to women’s support groups. Future research should address the information needs of male AI and AN cancer survivors and their level of satisfaction with support groups facilitated by videoconference.
Conclusions
An important role of the oncology nurse is to provide patients suffering from cancer with pertinent information and assistance with coping. The authors’ program evaluation identified the information needs of female AI and AN cancer survivors who participated in support group meetings. Information needs such as nutrition and telling others about cancer, which was found to be frequently endorsed by the participants, had not been included in the original list of topics selected for meetings. Assessing participants’ information needs is a key first step to planning and delivering effective AI and AN cancer support group services. Videoconferencing was found to be a viable method for facilitating support group meetings to rural AI and AN communities. Telehealth should be considered when planning support groups for AI and AN cancer survivors who cannot easily access in-person support groups because of geographic isolation. Results suggest that AI and AN cancer survivors were satisfied with support groups convened by videoconferencing. The ability to interact with other cancer survivors helped participants feel that they were not alone.
At a Glance.
-
✦
Support groups delivered by videoconferencing bridge geographical distances and increase access to support groups in rural communities.
-
✦
Assessing information needs of participants is essential in providing a culturally congruent support group.
-
✦
Rural American Indian and Alaska Native women with cancer express satisfaction with support groups delivered by videoconference.
Acknowledgments
The authors take full responsibility for the content of the article but acknowledge that the Native People for Cancer Control Telehealth network is supported by a grant (# H2ATH07752) from the Office for the Advancement of Telehealth, Health Resources and Services Administration, U.S. Department of Health and Human Services, and by a grant (# CA141875) from the National Cancer Institute. The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the independent peer reviewers or editorial staff.
Footnotes
Receive free continuing nursing education credit for reading this article and taking a brief quiz online. To access the test for this and other articles, visit http://evaluationcenter.ons.org/Login.aspx. After entering your Oncology Nursing Society profile username and password, select CNE Tests and Evals from the left-hand menu. Scroll down to Clinical Journal of Oncology Nursing and choose the test(s) you would like to take.
References
- Andersen BL. Biobehavioral outcomes following psychological interventions for cancer patients. Journal of Consulting and Clinical Psychology. 2002;70:590–610. doi: 10.1037//0022-006X.70.3.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres L, Kavanaugh K, Knafl KA. Within-case and across-case approaches to qualitative data analysis. Qualitative Health Research. 2003;13:871–883. doi: 10.1177/1049732303013006008. doi: 10.1177/1049732303013006008. [DOI] [PubMed] [Google Scholar]
- Bauer JE, Englert JJ, Michalek AM, Canfield P, Mahoney MC. American Indian cancer survivors. Journal of Cancer Education. 2005;20(Suppl.):23–27. doi: 10.1207/s15430154jce2001s_06. doi: 10.1207/s15430154jce2001s_06. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L. Community-driven Native American cancer survivors’ quality of life research priorities. Journal of Cancer Education. 2005;20:7–11. doi: 10.1207/s15430154jce2001s_03. doi: 10.1207/s15430154jce2001s_03. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Hollow W. Native American cultural aspects of oncology nursing care. Seminars in Oncology Nursing. 2001;17:206–219. doi: 10.1053/sonu.2001.25950. doi: 10.1053/sonu.2001.25950. [DOI] [PubMed] [Google Scholar]
- Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese-Davis J, Spiegel D. Supportive-expressive group therapy and distress in patients with metastatic breast cancer: A randomized clinical intervention trial. Archives of General Psychiatry. 2001;58:494–501. doi: 10.1001/archpsyc.58.5.494. doi: 10.1001/archpsyc.58.5.494. [DOI] [PubMed] [Google Scholar]
- Collie K, Kreshka MA, Ferrier S, Parsons R, Graddy K, Avram S, Koopman C. Videoconferencing for delivery of breast cancer support groups to women living in rural communities: A pilot study. Psycho-Oncology. 2007;16:778–782. doi: 10.1002/pon.1145. doi: 10.1002/pon.1145. [DOI] [PubMed] [Google Scholar]
- Demiris G, Doorenbos AZ, Towle C. Ethical considerations regarding the use of technology for older adults: The case of telehealth. Research in Gerontological Nursing. 2009;2(2):128–136. doi: 10.3928/19404921-20090401-02. doi: 10.3928/19404921-20090401-02. [DOI] [PubMed] [Google Scholar]
- Dolbeault S, Cayrou S, Bredart A, Viala AL, Desclaux B, Saltel P, Dickes P. The effectiveness of a psychoeducational group after early-stage breast cancer treatment. Psycho-Oncology. 2009;18:647–656. doi: 10.1002/pon.1440. doi: 10.1002/pon.1440. [DOI] [PubMed] [Google Scholar]
- Edwards BK, Ward E, Kohler BA, Dheman C, Zauber AG, Anderson RN, Ries LAG. Annual report to the nation on the status of cancer, 1975-2006. Cancer. 2010;116:544–573. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fobair P, Koopman C, DiMiceli S, O’Hanlan K, Butler LD, Classen C, Spiegel D. Psychosocial intervention for lesbians with primary breast cancer. Psycho-Oncology. 2002;11:427–438. doi: 10.1002/pon.624. [DOI] [PubMed] [Google Scholar]
- Gottlieb BH, Wachala ED. Cancer support groups: A critical review of empirical studies. Psycho-Oncology. 2007;16:379–400. doi: 10.1002/pon.1078. [DOI] [PubMed] [Google Scholar]
- Health Canada Telehealth Satisfaction Survey. First Nations, Inuit and Aboriginal Health. 2007 Retrieved from http://www.hc-sc.gc.ca/fniah-spnia/index-eng.php.
- Hewitt M, Greenfield S, Stovall S, editors. From cancer patient to cancer survivor: Lost in transition. National Academies Press; Washington, DC: 2006. [Google Scholar]
- Hill TG, Briant KJ, Bowen D, Boerner V, Vu T, Lopez K, Vinson E. Evaluation of Cancer 101: An educational program for native settings. Journal of Cancer Education. 2010;25:329–336. doi: 10.1007/s13187-010-0046-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: A Cancer Journal for Clinicians. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- Lanier AP, Kelly JJ, Maxwell J, McEvoy T, Homan C. Cancer in Alaska natives 1969-2003: 35-year report. 2006. Retrieved from http://www.anthc.org/chs/epicenter/upload/Cancer_Incidence_35-Year_Report.pdf. [PubMed] [Google Scholar]
- Lounsberry JJ, Macrae H, Angen M, Hoeber M, Carlson LE. Feasibility study of a telehealth delivered, psychoeducational support group for allogenic hematopoietic stem cell patients. Psycho-Oncology. 2009;19:777–781. doi: 10.1002/pon.1617. doi: 10.1002/pon.1617. [DOI] [PubMed] [Google Scholar]
- O’Brien M, Harris J, King R, O’Brien T. Supportive-expressive group therapy for women with metastatic breast cancer: Improving access for Australian women through use of teleconference. Counseling and Psychotherapy Research. 2008;8:28–35. doi: 10.1080/14733140801889071. [Google Scholar]
- Olson J, Simmons J. South Puget Intertribal Planning Agency’s comprehensive cancer control planning project: Cancer control information for the Five Tribes. South Puget Intertribal Planning Agency; Shelton, WA: 2005. [Google Scholar]
- Pelusi J, Krebs L. Understanding cancer—Understanding the stories of life and living. Journal of Cancer Education. 2005;20(Suppl.):12–16. doi: 10.1207/s15430154jce2001s_04. doi: 10.1207/s15430154jce2001s_04. [DOI] [PubMed] [Google Scholar]
- Polit D, Beck CT. Nursing research. Lippincott Williams and Wilkins; Philadelphia, PA: 2008. [Google Scholar]
- President’s Cancer Panel . Facing cancer in Indian country: The Yakama Nation and Pacific Northwest Tribes. U.S. Department of Health and Human Services, National Institute of Health, National Cancer Institute; Washington, DC: 2003. [Google Scholar]
- Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qualitative Health Research. 2003;13:905–923. doi: 10.1177/1049732303253488. [DOI] [PubMed] [Google Scholar]
- Sherman AC, Pennington J, Simonton S, Latif U, Arent L, Farley H. Determinants of participation in cancer support groups. International Journal of Behavioral Medicine. 2008;15:92–100. doi: 10.1080/10705500801929601. [DOI] [PubMed] [Google Scholar]
- Shou I, Ekeberg O, Karesen R, Sorensen E. Psychosocial intervention as a component of routine breast cancer care—Who participates and does it help? Psycho-Oncology. 2008;17:716–720. doi: 10.1002/pon.1264. doi: 10.1002/pon.1264. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Indian Health Services . Alaska area: Division of planning, evaluation and health statistics. Author; Anchorage, AK: 2010. [Google Scholar]
- U.S. Department of Health and Social Services . Alaska comprehensive cancer control plan 2005-2010. Author; Anchorage, AK: 2006. [Google Scholar]
- Ussher J, Kirsten L, Butow P, Sandoval M. What do cancer support groups provide which other supportive relationships do not? The experience of peer support groups for people with cancer. Social Science and Medicine. 2006;62:2565–2576. doi: 10.1016/j.socscimed.2005.10.034. [DOI] [PubMed] [Google Scholar]
- Warne D. Research and educational approaches to reducing health disparities among American Indians and Alaska Natives. Journal of Transcultural Nursing. 2006;17:266–271. doi: 10.1177/1043659606288381. [DOI] [PubMed] [Google Scholar]
- Weiner D, Burhansstipanov L, Krebs LU, Restivo T. From survivorship to thrivership: Native peoples weaving a healthy life from cancer. Journal of Cancer Education. 2005;20(Suppl.):28–32. doi: 10.1207/s15430154jce2001s_07. [DOI] [PubMed] [Google Scholar]
- Wiggins CL, Espey DK, Wingo PA, Kaur JS, Wilson RT, Swan J, Lanier AP. Cancer among American Indians and Alaska Natives in the United States, 1999-2004. Cancer. 2008;113:1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- Wingo PA, King J, Swan J, Coughlin SS, Kaur JS, Erb-Alvarez JA, Arambula Solomon TG. Breast cancer incidence among American Indian and Alaska Native women: US, 1999-2004. Cancer. 2008;113:1191–1202. doi: 10.1002/cncr.23725. [DOI] [PubMed] [Google Scholar]
- Winzelberg AJ, Classen C, Alpers GW, Roberts H, Koopman C, Adams RE, Taylor CB. Evaluation of an internet support group with primary breast cancer. Cancer. 2003;97:1164–1173. doi: 10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]