Abstract
Background
The feasibility of total laparoscopic pancreaticoduodenectomy (TLPD) has been established. Laparoscopic major venous resection during TLPD has not been reported. The aim of the present study was to describe the technique and outcomes of patients undergoing TLPD with major venous resection.
Methods
Retrospective review of all consecutive patients undergoing TLPD and major venous resection from July 2007 to December 2010 was performed. Patient demographics and peri-operative outcomes were retrieved. Data are presented as mean ± standard deviation (SD) or median with range.
Results
Out of 129 patients undergoing TLPD, major venous resection was performed in 11 patients with a mean age of 71 years. Median operative time and blood loss was 413 (301–666) min and 500 (75–2800) ml, respectively. Venous resection included tangential (n = 10) and segmental resection (n = 1). Venous reconstruction included patch (n = 4), suture (n = 4), stapled (n = 2) and a left renal vein interposition graft (n = 1). Median mesoportal clamp time was 35 (10–82) min. There was no 30-day or in-hospital mortality. Post-operative imaging was available in 10 patients with 100% patency at the venous reconstruction site.
Conclusions
Laparoscopic major venous resection during TLPD is feasible in selected patients. Extensive experience with complex laparoscopic pancreatic resection and reconstruction is advocated before attempting this procedure.
Keywords: adenocarcinoma, pancreatic neoplasia, resection, pancreatic neoplasia, outcomes, pancreatic neoplasia
Introduction
Enthusiasm for minimally invasive approaches in patients requiring a pancreaticoduodenectomy has recently gained momentum and has stemmed from excellent outcomes of laparoscopic distal pancreatectomy.1,2 Several single-institutional series have now reported the feasibility and safety of total laparoscopic pancreaticoduodenectomy (TLPD) and suggest advantages similar to those reported for minimally invasive approaches in other procedures.3–5 TLPD has been performed for malignant indications in 65% to 96% of reported patients and although comparative trials are lacking, initial outcomes are promising.
Advances in the surgical treatment of patients with pancreatic malignancy have also become apparent in traditional open approaches. Whereas patients with malignant involvement of the portal vein (PV) or superior mesenteric vein (SMV) were previously considered unresectable and were either excluded from operative treatment or underwent a pancreaticoduodenectomy with a high rate of margin positivity, several series now demonstrate the feasibility of concomitant major venous resection when necessary to achieve a macroscopic and microscopic negative (R0) resection. While randomized-controlled trials have not been performed, comparative studies have reported peri-operative and oncological outcomes that are similar to patients undergoing a pancreaticoduodenectomy without venous involvement.6–13
Currently, major venous involvement has been considered a relative contraindication for the laparoscopic approach to a pancreaticoduodenectomy given the limited experience with TLPD and the added complexity of vascular resection and reconstruction. We report the first series of TLPD with major venous resection for patients with suspected malignant involvement of the PV or SMV.
Methods
After institutional review board approval, a retrospective review of our prospectively maintained database was performed of all consecutive patients undergoing TLPD from July 2007 to December 2010, at Mayo Clinic in Rochester, MN, USA. Patients having undergone concomitant major venous resection and reconstruction were included in the present study. Indications for venous resection included expected malignant adherence or invasion of the PV or SMV. Consideration for the laparoscopic approach in patients requiring major venous resection and reconstruction occurred only after substantial experience with TLPD without venous resection (>60 cases) and significant experience in open pancreaticoduodenectomy with and without major venous resection and reconstruction.
Procedure
The technique of TLPD has been described previously.3 Typically, assessment of the plane posterior to the pancreatic neck is performed early in the procedure to either confirm the extent of malignant mesoportal venous involvement demonstrated on pre-operative imaging or to identify unsuspected involvement. In the event that the tumour originates within or extends into the uncinate process, a posterior, superior mesenteric artery (SMA) approach is performed early to assess resectability and to facilitate the uncinate dissection when venous involvement is present. Combined with an anterior approach to the SMA and uncinate dissection, this facilitates isolation of the involved portion of vein to allow en-bloc resection. Exposure of the PV, SMV and distal splenic vein is accomplished for complete major venous control in anticipation of venous resection. To minimize mesoportal clamp time, the remainder of the pancreaticoduodenectomy dissection is completed reserving the venous transection as the final step in the resection.
Systemic intravenous unfractionated heparin (3000 to 5000 units) is given before clamping of the mesoportal system. Venous clamping is performed with atraumatic endo vessel clamps (Aesculap Inc., Center Valley, PA, USA) using a dedicated applier that facilitates control and precise placement. When feasible, a curved clamp is used for tangential occlusion, avoiding complete disruption of the mesoportal blood flow. For longer venous resection (>3 cm), circumferential involvement >25%, or segmental resections, individual clamping of the portal, superior mesenteric and splenic vein is performed. Venous resection is then performed sharply with scissors, leaving the involved vein en-bloc with the pancreaticoduodenectomy specimen.
The technique of venous resection and reconstruction is based on the extent and location of venous involvement. Where less than 50% of the circumference is involved, tangential resection with primary suture closure (<25% involvement) or patch venorrhaphy (25–50% involvement) is generally preferred. For patch reconstruction, we favour the use of a bovine pericardial graft (Synovis Life Technologies Inc, St. Paul, MN, USA) over an autologous vein. Segmental resection is performed when expected circumferential venous involvement is greater than 50%. A primary end-to-end reconstruction is performed when possible; otherwise an autologous left renal vein interposition graft is used. All methods of venous reconstruction utilize a 5–0 Prolene suture.
Post-operatively, low-dose (81 mg) aspirin is prescribed and is continued for 3 months. In patients with malignancy and a history of thrombosis, full anticoagulation with warfarin is generally instituted. Post-operative imaging was obtained to assess patency of venous reconstruction and to rule out thrombosis.
Data are presented as mean ± standard deviation (SD) or median with range.
Results
Out of the 129 patients undergoing TLPD, laparoscopic major venous resection was performed in 11 patients with a mean age of 71 years. Patient demographics and peri-operative characteristics are listed in Table 1. The median body mass index (BMI) (kg/m2) and American Society of Anesthesiologists (ASA) score were 24 (17–35) and 2 (2–4), respectively. Four patients had previous abdominal operations that included partial colectomy, ventral/umbilical hernia repair and appendectomy. Indication for a pancreaticoduodenectomy included pancreatic ductal adenocarcinoma (n = 9), neuroendocrine carcinoma (n = 1) and indeterminate pancreatic head mass (n = 1). One patient underwent conversion to open for anticipated difficult venous and pancreatic reconstruction early in the experience; the remaining patients underwent total laparoscopic resection and reconstruction. In two patients, robotic assistance was used for pancreaticobiliary reconstruction after pure laparoscopic resection and venous reconstruction.
Table 1.
Characteristics of 11 patients undergoing TLPD with major venous resection
| Patient | Age (years) | BMI (kg/m2) | Resection/reconstruction | Operative time (min) | EBL (ml) | T size (cm) | R0/R1 | LOS (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | 50 | 24 | T / Patch | 301 | 900 | 4.5 | R0 | 6 |
| 2 | 58 | 17 | T / Stapled | 371 | 450 | 3.7 | R0 | 5 |
| 3 | 68 | 23 | T / Suture | 422 | 600 | 4.4 | R0 | 4 |
| 4 | 58 | 28 | T / Stapled | 388 | 450 | 5 | R0 | 24 |
| 5 | 77 | 29 | T / Suture | 480 | 100 | 4.3 | R1 | 7 |
| 6 | 79 | 24 | T / Suture | 380 | 300 | 2 | R0 | 8 |
| 7 | 78 | 22 | T / Patch | 653 | 800 | 3.8 | R0 | 35 |
| 8 | 80 | 35 | T / Suture | 413 | 500 | 2 | R0 | 35 |
| 9 | 70 | 27 | T / Patch | 453 | 75 | 2.9 | R0 | 14 |
| 10 | 81 | 24 | T / Patch | 370 | 500 | 4 | R0 | 7 |
| 11 | 80 | 22 | S / RVIG | 666 | 2800 | 5.1 | R0 | 7 |
| Median | 71* | 24 | – | 413 | 500 | 4 | – | 7 |
Mean.
T, tangential resection; S, segmental resection; RVIG, renal vein interposition graft; BMI, body mass index; EBL, estimated blood loss; LOS, length of stay.
Vascular resection was performed based on concerns of malignant adherence or invasion in all patients. Venous resection included the SMV (n = 6), PV (n = 3), or both (n = 2) and consisted of a tangential (n = 10) or segmental (n = 1) resection. Venous reconstruction included primary suture venorrhaphy in four patients, patch venorrhaphy in four (Fig. 1), tangential stapling in two and interposition graft using the left renal vein in one patient (Figs 2,3). The overall median mesoportal clamp time was 35 (10 to 82) min. In three patients, complete mesoportal occlusion was unnecessary (stapled technique in two and primary suture venorrhaphy in one). Median operative time and blood loss were 413 (301–666) min and 500 (75–2800) ml, respectively.
Figure 1.
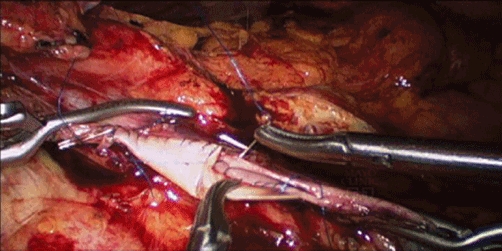
Intra-operative photo of patch venorrhaphy after tangential venous resection
Figure 2.
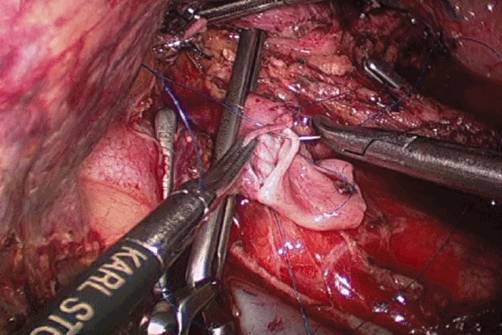
Intra-operative photo of distal venous anastomosis using an autologous left renal vein interposition graft after segmental venous resection
Figure 3.
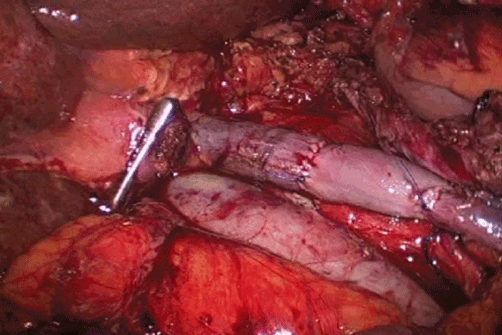
Intra-operative photo of completed venous reconstruction using autologous left renal vein interposition
Histopathology confirmed pancreatic ductal adenocarcinoma in nine patients, neuroendocrine carcinoma in one and mass-forming autoimmune pancreatitis in one. A complete macroscopic and microscopic margin negative resection (R0) was obtained in 9 out of 10 patients (90%) with malignant disease. In three patients, re-excision into the pancreatic body was necessary to achieve an R0 resection after initial pancreatic neck margins were microscopically positive on frozen section analysis. One patient underwent laparoscopic completion pancreatectomy because of poor quality of the pancreatic remnant. In the patient with neuroendocrine carcinoma, tumour thrombus was noted in an inferior pancreaticoduodenal venous tributary of the SMV with venous invasion confirmed on histopathology. One patient in this series had an R1 resection as a result of microscopic presence of ductal adenocarcinoma at the retroperitoneal (SMA) margin. Mass-forming autoimmune pancreatitis was demonstrated on the final histology of one patient who had initially presented with obstructive jaundice and was found to have a 2-cm pancreatic head mass with biliary and pancreatic ductal dilatation. Pre-operative endoscopic ultrasound-guided fine needle aspiration was performed and demonstrated atypical cells on cytology. Operative findings were that of considerable perivascular fibrosis and a dense, focal adherence to the lateral wall of the PV that prompted tangential venous resection.
The median number of lymph nodes harvested for this cohort was 19 (9–45) with 50% of patients with a malignant histology demonstrating regional lymph node metastases.
Post-operative complications occurred in six patients and included a pancreatic anastomotic leak in three, post-operative anaemia/haemorrhage requiring a transfusion in three, arrhythmia in two, transient renal failure in one and delayed gastric emptying in one. Median length of hospital stay was 7 days (4–35). There was no 30-day or in-hospital mortality. The median follow-up for this cohort was 7.2 (1.5–19) months. Computed tomography imaging was available in 10 patients greater than 1 month post-operatively which demonstrated patency of the mesoportal venous system without evidence of thrombosis in all patients. The single patient with no imaging at follow-up was alive and well 6 months post-operatively, but had refused adjuvant treatment or imaging after R0 resection of stage IB, pancreatic adenocarcinoma.
Discussion
Total laparoscopic pancreaticoduodenectomy has been established as feasible and safe in several centres with two series reporting experience in more than 60 patients.3,4 While adequate comparative trials are still lacking, peri-operative outcomes of TLPD are favourable and appear comparable to those reported for open approaches.3,4,14 Given the relatively short follow-up and small numbers of patients, adequate disease-free and overall survival outcomes are not established for TLPD in patients with pancreatic malignancy. Surrogates of the adequacy of oncological resection such as the number of lymph nodes harvested, margin status and short-term outcomes appear comparable, albeit, potential selection and reporting bias preclude a valid interpretation of these initial results.
Advances in the surgical treatment of pancreatic malignancy have also included a more aggressive operative approach for patients with malignant major venous involvement. Previously considered unresectable, many centres now perform en-bloc major venous resection with pancreaticoduodenectomy in these patients. The rationale for this approach has been to increase the number of candidates for resection and to improve the margin negative resection rate for those with venous involvement. While randomized-controlled trials have not been performed, several retrospective comparative trials have reported similar outcomes for patients requiring venous resection as a result of malignant involvement compared with those that do not.6,9 Performed predominantly in high-volume centres specializing in pancreatic disease, this approach has been limited to open approaches owing to the limited experience of TLPD and the added complexity of major venous resection and reconstruction.
The present study is the first to describe the technique and outcomes of a series of patients undergoing laparoscopic major venous resection and reconstruction. Caution should be apparent in review of the course of events that led to the application of laparoscopic approaches to major venous resection at our institution. In our early experience with TLPD, possible malignant involvement of the PV or SMV was considered a contraindication for the laparoscopic approach and these patients underwent open pancreaticoduodenectomy with major venous resection.3 However, after considerable experience with TLPD, it became evident that laparoscopic venous resection and reconstruction could also be performed. With the advantages afforded by laparoscopy including excellent exposure, magnification and positive intra-abdominal pressure (limiting low pressure venous bleeding), we felt that a laparoscopic approach to major venous resection may be safe and even beneficial. Before attempting the first laparoscopic major venous resection, extensive experience and planning were ensured. First, sufficient experience with an open pancreaticoduodenectomy, with and without major venous resection, in over 100 patients was obtained. Second, TLPD was performed in over 60 patients without venous resection. Finally, techniques of laparoscopic major vascular resection and reconstruction were investigated in a swine model. In the author's opinion, this preparation cannot be overemphasized as fatigue (long-operative times) and frustration (procedure complexity) with TLPD alone in the early experience is the inappropriate time for application of the added complexity and risk of major vascular resection and reconstruction.
Peri-operative outcomes in this series appear similar to those reported in recent series using the open approaches6–9 (Table 2). In spite of the potential limitations of a small series and potential selection bias, these data suggest that laparoscopic major venous resection with pancreaticoduodenectomy is feasible and safe in selected patients.
Table 2.
Peri-operative outcomes of pancreaticoduodenectomy with major venous resection in recent series and the present study
| Study | n | Approach | Clamp time (min) | Operative time (min) | EBL (ml) | R0 (%) | Morbidity (%) | Mortality (%) |
|---|---|---|---|---|---|---|---|---|
| Yekebas et al. 20086 | 136 | Open | NR | 360 | NR | 87.5 | 40 | 3.7 |
| Muller et al. 20097 | 110 | Open | NR | 421 | 1182 | 49 | 42 | 3.6 |
| Kaneoka et al. 20098 | 42 | Open | 26* | 342 | 1280 | 76 | 33 | 4.8 |
| Martin et al. 20099 | 36 | Open | 12.5 | 210 | 700 | 78 | 35 | 0 |
| Present study | 11 | Lap | 35 | 413 | 500 | 90 | 54 | 0 |
For patients reconstructed with graft.
EBL, estimated blood loss.
Various techniques of venous resection (tangential vs. segmental) and reconstruction (suture vs. patch or end-to-end vs. interposition graft) and have been reported without clear advantages of one particular technique over another.6–8 In the present series, all but one patient (91%) underwent tangential resection and reconstruction as opposed to a more predominant use of segmental resection reported by others.6–12 Whether this difference is as a result of patient selection bias or to the author's criteria for selecting the reconstruction method is unclear. We did not change our approach to vascular resection based on the laparoscopic approach. For open cases, the author uses the same criteria of extent of circumferential involvement to determine whether tangential or segmental resection is performed. Our preferred technique for reconstruction after segmental resection is a primary end-to-end anastomosis after sufficient mobilization, reserving interposition grafting for those circumstances where end-to-end is not feasible. The patient undergoing segmental resection in the present series had a 4-cm segment of PV/SMV resected and therefore underwent a left renal vein interposition graft for reconstruction as previously described.15
The median total venous clamp time (35 min) in this early series may be longer than is typically reported in open procedures and may represent the learning curve of laparoscopic venous resection. In spite of this, we observed no complications that could be directly attributed to a prolonged clamp time, and overall complication rates are similar to those reported for open approaches.16
This series cannot establish definitive outcomes of laparoscopic major venous resection with pancreaticoduodenectomy, but does suggest the feasibility and safety in selected patients. The unique exposure, magnification and positive pressure afforded by the laparoscopic approach may demonstrate advantages of this approach in larger series and comparative trials. The authors recommend the acquisition of considerable experience in both open PD with and without vascular resection, and TLPD without vascular resection before attempting laparoscopic major venous resection and reconstruction.
Acknowledgments
Funding was provided by the Mayo Clinic.
Conflicts of interest
None declared.
References
- 1.Vijan SS, Ahmed KA, Harmsen WS, Que FG, Reid-Lombardo KM, Nagorney DM, et al. Laparoscopic vs open distal pancreatectomy: a single-institution comparative study. Arch Surg. 2010;145:616–621. doi: 10.1001/archsurg.2010.120. [DOI] [PubMed] [Google Scholar]
- 2.Kooby DA, Hawkin WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg. 2010;210:779–785. doi: 10.1016/j.jamcollsurg.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 3.Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg. 2010;145:19–23. doi: 10.1001/archsurg.2009.243. [DOI] [PubMed] [Google Scholar]
- 4.Palanivelu C, Rajan PS, Rangarajan M, Vaithiswaran V, Senthilnathan P, Parthasarathi R, et al. Evolution in techniques of laparoscopic pancreaticoduodenectomy: a decade long experience from a tertiary center. J Hepatobiliary Pancreat Surg. 2009;16:731–740. doi: 10.1007/s00534-009-0157-8. [DOI] [PubMed] [Google Scholar]
- 5.Dulucq JL, Wintringer P, Mahajna A. Laparoscopic pancreaticoduodenectomy for benign and malignant diseases. Surg Endosc. 2006;20:1045–1050. doi: 10.1007/s00464-005-0474-1. [DOI] [PubMed] [Google Scholar]
- 6.Yekebas EF, Bogoevski D, Cataldegirmen G, Kunze C, Marx A, Vashist YK, et al. En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg. 2008;247:300–309. doi: 10.1097/SLA.0b013e31815aab22. [DOI] [PubMed] [Google Scholar]
- 7.Muller SA, Hartel M, Mehrabi A, Welsh T, Martin DJ, Hinz U, et al. Vascular resection in pancreatic cancer surgery: survival determinates. J Gastrointest Surg. 2009;13:784–792. doi: 10.1007/s11605-008-0791-5. [DOI] [PubMed] [Google Scholar]
- 8.Kaneoka Y, Yamaguchi A, Isogai M. Portal or superior mesenteric vein resection for pancreatic head adenocarcinoma: prognostic value of the length of venous resection. Surgery. 2009;145:417–425. doi: 10.1016/j.surg.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Martin RCG, Scoggins CR, Egnatashvili V, Staley CA, McMasters KM, Kooby DA. Arterial and venous resection for pancreatic adenocarcinoma: operative and long-term outcomes. Arch Surg. 2009;144:154–159. doi: 10.1001/archsurg.2008.547. [DOI] [PubMed] [Google Scholar]
- 10.Nakao A, Takeda S, Inoue S, Nomoto S, Kanazumi N, Sugimoto H, et al. Indications and techniques of extended resection for pancreatic cancer. World J Surg. 2006;30:976–982. doi: 10.1007/s00268-005-0438-6. [DOI] [PubMed] [Google Scholar]
- 11.Tseng JF, Raut CP, Lee JE, Pisters PW, Vauthey JN, Abdalla EK, et al. Pancreaticoduodenectomy with vascular resection: margin status and survival duration. J Gastrointest Surg. 2004;8:935–949. doi: 10.1016/j.gassur.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 12.Riedeger H, Makowiec F, Fischer E, Adam U, Hopt UT. Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg. 2006;10:1106–1115. doi: 10.1016/j.gassur.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Chu CK, Farnell MB, Nguyen JH, Stauffer JA, Kooby DA, Sclabas GM, et al. Prosthetic graft reconstruction after portal vein resection in pancreaticoduodenectomy: a multicenter analysis. J Am Coll Surg. 2010;211:316–324. doi: 10.1016/j.jamcollsurg.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Winter JM, Cameron JL, Campbell KA, Arnold JA, Chang DC, Coleman J, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single institutional experience. J Gastrointest Surg. 2006;10:1199–1211. doi: 10.1016/j.gassur.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Smoot RL, Christein JD, Farnell MB. An innovative option for venous reconstruction after pancreaticoduodenectomy: the left renal vein. J Gastrointest Surg. 2007;11:425–431. doi: 10.1007/s11605-007-0131-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramacciato G, Mercantini P, Peterucciani N, Giaccaglia B, Nigri G, Ravaioli M, et al. Does portal-superior mesenteric vein invasion still indicate irresectability for pancreatic carcinoma? Ann Surg Oncol. 2009;16:817–825. doi: 10.1245/s10434-008-0281-8. [DOI] [PubMed] [Google Scholar]


