Abstract
Insomnia has become a major public health issue in recent times. Although quality of sleep is affected by environmental, psychophysiological, and pharmacological factors, diet and nutrient intake also contribute to sleep problems. This study investigated the association between nutrient intake and co-morbid symptoms associated with sleep status among selected adults. Subjects in this study included 87 men and women aged 21-45 years. Presence of insomnia was assessed using the Insomnia Screening Questionnaire, and dietary intake was measured over three consecutive days by dietary survey. Descriptive analysis, ANOVA, and Chi-Square tests were performed to compute and interpret the data. Approximately 60% of the participants were insomniacs. People with insomnia consumed significantly lesser quantities of nutrients as compared to normal sleepers. Differences in intakes of energy, carbohydrates, folic acid, and B12 were highly significant (P < 0.002). Further, intakes of protein, fat, and thiamine were significantly different (P < 0.021) between insomniacs and normal sleepers. The nutrient intake pattern of the insomniacs with co-morbid symptoms was quite different from that of the normal sleepers. Based on these results, it is probable that there is an association between nutrition deficiency, co-morbid symptoms, and sleep status. More studies are required to confirm these results.
Keywords: Sleep, insomnia, nutrient intake, sleep disturbances, public health
Introduction
Sleep is a physiological process that occurs in humans and animals and is defined as a recurrent state of reduced attention to the surrounding environment. The most important functions of sleep are the restoration of body functions, synthesis of proteins, and the prevention of lethargy. The number of sleep hours required varies from individual to individual. An adult person needs 7 to 9 hours of good sleep daily to be alert during the day [1]. Disturbances in sleep status generally described as difficulty in falling asleep, waking up frequently during the night with difficulty returning back to sleep, waking up too early in the morning, and un-refreshing sleep are collectively referred to as insomnia. Thus, insomnia is the perception or complaint of inadequate or poor sleep status [2]. Leg cramps, restless leg syndrome, and periodic limb movement are just some of the co-morbid symptoms associated with poor sleep status.
Insomnia is not defined by the number of hours of sleep a person gets or how long it takes to fall asleep, as individuals vary in their requirement for satisfactory sleep. The effect of nutrition on sleep status has been recognized recently [3]. Presently, the amount of knowledge related to nutrition and sleep status is scarce [4]. Although previous studies have shown an association between vitamins and sleep disorders, a direct link between vitamins and quality of sleep is not clear [5]. For example, vitamin B12 deficiency results in poor sleep status by shortening the length of the sleep-wake rhythm and affects the circadian aspect of sleep propensity [6,7]. Studies have demonstrated that supplementation with vitamin B-complex improves nocturnal leg cramps, suggesting a possible nutritional method for the management of certain types of sleep disorders [8]. Restless leg syndrome is often a complaint among anemic individuals. For this, iron supplementation and improvement in iron status have been reported to have reducing effects, indicating a relationship between sleep quality and nutritional deficiencies [9].
Based on case controlled studies, it could be stated that dietary deficiencies affect quality of sleep [10]. There are a limited number of studies regarding dietary intake and the sleep response in populations. Hence, the present study was carried out to investigate the association between nutrient intakes and sleep status in selected adults in Mysore, Karnataka, India.
Subjects and Methods
Selection of subjects
This study was conducted in Mysore city, a major city of Karnataka in south India, and it included 120 subjects from institutions such as software and IT companies as well as students and faculty members of various universities. The exclusion criteria included regular medication for any medical or psychiatric problem.
Selection of the tools
Questionnaires
In order to select the subjects based on their sleep status, the Insomnia Screening Index of Clinical Practice Guideline of the Alberta Medical Association (English language) was used [11]. This is a simple questionnaire to assess insomnia among subjects. A pilot study was conducted to verify the suitability of the questionnaire, including the language in an Indian context, and was found to be appropriate for use without any modification; also, the selected subjects were educated and well versed in the English language. Presence of insomnia was assessed based on four questions enquiring subjects about their sleep status during the past four weeks: (i) difficulty in initiating sleep; (ii) nocturnal awakenings with difficulty returning to sleep; (ii) early involuntary awakening and too short sleep period (six hours or less); and (iv) non-restorative sleep with a feeling of tiredness upon awakening and negative consequences in terms of daytime alertness, fatigue, and irritability as a result. In addition, the questionnaire included self-reporting multiple assessment quarries for measuring co-morbid symptoms such as restless leg syndrome, circadian rhythm disorders, and hypersomnia, which are associated with sleep status.
Nutrient intake was also assessed based on dietary intake over 3 consecutive days using the daily record method [12,13]. Subjects were trained in recording their daily food intake by demonstrating the use of standard cups and spoons for serving food and beverages [14]. Nutrient intake based on dietary intake data was calculated using a dietary ready reckoner for cooked foods, which was developed by the Department of Studies in Food Science and Nutrition, University of Mysore based on Indian Council of Medical Research (ICMR) data [14-16]. Nutrient intakes were adjusted for energy intake using the Nutrient residual (energy-adjusted) model, as recommended by Willett [17].
Anthropometry
Height and weight measurements were carried out to assess nutritional status; height was measured to the nearest of 0.1 cm and weight to 0.1 kg, as suggested by Jelliffe [18]. A height measuring scale [19] and an electronic weighing machine were used. Based on the data, BMI was calculated according to the formula: (wt/kg)/(ht/m)2 [20].
Conducting the study
The proposed study involved human volunteers. Therefore, approval was sought from the Human Ethics Committee of the University of Mysore, and consent letters from all subjects were obtained.
A brief write-up about insomnia explaining its causes and consequences on quality of life was prepared and distributed to the authorities of selected institutions to solicit their cooperation. Convenient time was considered for each institute, and a preliminary meeting to explain the purpose and importance of the study was organized for the employees with due support provided by the authorities. A total number of 120 questionnaires titled 'Insomnia Screening Questionnaire' and 'food intake record' were distributed. Heights and weights of all the subjects were recorded by the investigator according to standard techniques.
Computation of results and statistical analysis
Eighty-seven questionnaires out of the 120 distributed were completed. The selected subjects comprised both males and females aged 21-45 years in an insomnia group (n = 53) and normal sleep group (n = 34). The data collected were tabulated, and suitable statistical tests were applied using Statistical Package XLSTAT 2007 and SPSS 15.0 to interpret the results.
Results
General information of the selected subjects
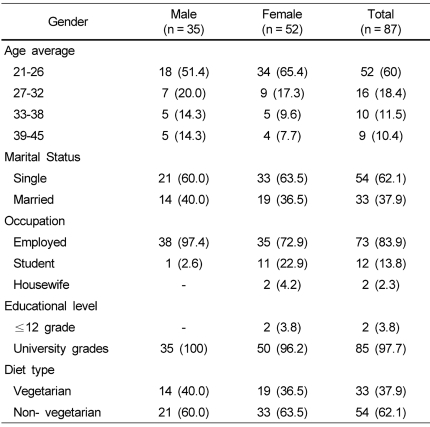
Table 1 presents the general profile of the participants. A higher percentage of subjects were aged 21-26 years, followed by those aged 27-32 years. Among the 87 subjects included in this study, 35 subjects were males and 52 females. Most of the subjects (62%) were unmarried. Almost all of the selected subjects were graduates or postgraduates; 84% were employed in different organizations and institutes, whereas a small proportion (13.8%) of the participants was comprised of students. A higher percentage of the subjects (65%) consisted of non-vegetarians.
Table 1.
General information of the subjects
Relationship of sleep status with age, gender, and BMI of selected subjects
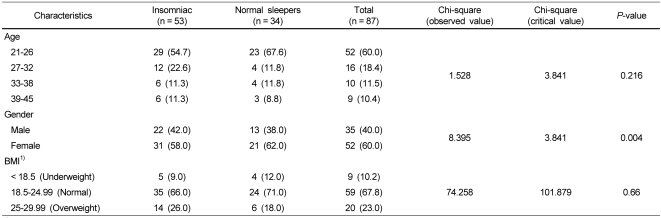
A perusal of Table 2 indicates the occurrence of insomnia with relation to age, gender, and BMI. Sixty-three percent of subjects exhibited symptoms of insomnia. Insomnia was more prevalent (55%) in the 21-32 age group as compared to the older age (33-45) group. Although both men and women displayed symptoms of insomnia, occurrence was higher (58%) among women. According to Chi-Square analysis, a significant association was observed between gender and sleep status.
Table 2.
Association of sleep status with age, gender, and BMI of selected subjects [N (%)]
1)BMI: Body mass index
The association between BMI and sleep status can also be seen in Table 2. A higher percentage of subjects with BMI values in the normal range as well as those in the underweight category were normal sleepers compared to those in the overweight category.
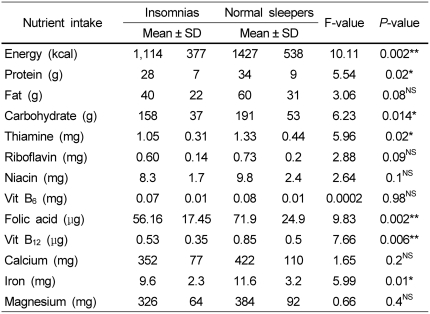
Association between nutrient intake and sleep status
Information concerning nutrient intake among subjects with sleep disturbances must be obtained to understand the influence of diet on sleep status. A perusal of Table 3 illustrates the mean intake of energy, three macro and nine micro nutrients by insomniacs as compared to subjects in the normal sleep group. Significant differences (1%) were noted in the mean intakes of energy, folic acid, B12, and iron between the two groups. The normal sleepers consumed a significantly higher quantity of energy as well as certain nutrients, namely carbohydrates, folic acid, and vitamin B12, compared to the insomniacs. In addition to these, protein and thiamine intakes also exhibited significant differences (at 5%). Nevertheless, intakes of all nutrients, regardless of statistical significance, were found to be markedly lower among insomniacs as compared to normal sleepers. These results are similar to studies performed by other investigators that reported deficient energy and nutrient intakes among insomniacs [4,21].
Table 3.
Comparison of mean nutrient intake/day between normal sleepers and insomniac subjects
*Statistical test (ANOVA) was done after adjustment with energy intake using residual method
*P < 0.05, **P < 0.01
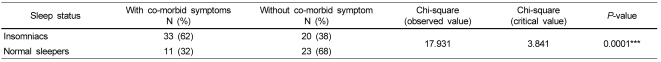
Occurrence of insomnia and co-morbid symptoms
Co-morbid symptoms are considered to be precipitating factors that worsen insomnia; different symptoms are known to coexist with sleep status [22]. It is evident from Table 4 that 38% of the insomniacs did not experience clinical symptoms, whereas a higher percentage of the participants suffered co-morbid symptoms (62%). Surprisingly, 32% of the normal sleepers experienced co-morbid symptoms; however, the result of the Chi-Square test revealed a highly significant association between sleep status (insomniacs and normal sleepers) and presence of co-morbid symptoms.
Table 4.
Frequency of occurrence of co-morbid symptoms in relation to sleep status
***P < 0.0001
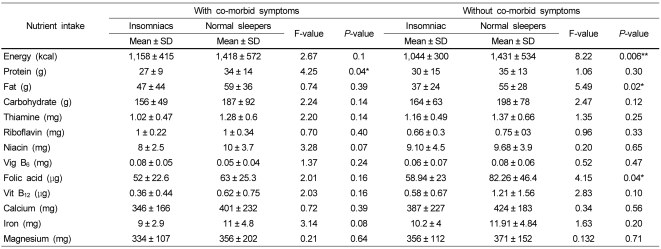
Influence of co-morbidity on nutrient intake
Table 5 presents the mean and standard deviation of nutrient intake among normal sleepers and insomniacs with and without co-morbid symptoms. Mean energy intakes among the insomniacs with symptoms were considerably lower in comparison with corresponding normal sleepers. However, the differences were not statistically significant. Further comparison of energy intake between normal sleepers and insomniacs without co-morbid symptoms revealed a significant difference (P < 0.006), wherein insomniacs consumed significantly less energy. Similarly, the intakes of fat and folic acid were also significantly lower among the insomniacs without co-morbid symptoms. On the other hand, protein intake was significantly lower among the insomniacs with co-morbid symptoms. Intakes of other nutrients were not found to be different statistically significant between the insomniacs and normal sleepers with and without co-morbid symptoms.
Table 5.
Nutrient intake in insomniacs and normal sleepers based on presence of co-morbid symptoms
*P < 0.05, **P < 0.01
Discussion
Very few research studies have demonstrated associations between food and nutrient deficiencies and sleep disturbances; however, confirmatory data has yet to be established for effective nutritional management of insomnia. Several foods and nutrients have traditionally been associated with sleep status [23]. Researchers have recently begun to investigate the effectiveness of such foods as substitutes for pharmacological interventions. The effects of food and food constituents on sleep disturbances are not fully known. It is noteworthy to mention that sleep-related health problems are associated with specific food consumption behaviors. Consumption of tea, coffee, or alcohol as well as dining just before bedtime is reported to have negative effect on sleep [24]. The need to develop a database regarding food and nutrient intakes by insomniacs is well recognized by public health nutritionists [25]. The available literature strongly points to the ability of certain nutrients to affect sleep by altering neural responses; especially, B group vitamins are known to cause psychological distress, leading to sleep disturbances [26,27]. Further, iron deficiency anemia is a putative cause for restless leg syndrome (RLS), a human sensorimotor reflector that appears to intensify during the evening hours [10,28,29]. Though the mechanism of RLS development is uncertain, there is circumstantial evidence that the dopaminergic system and iron status play roles in the pathophysiology of the syndrome [30]. However, it is well documented that iron absorption is counteracted by a variety of dietary factors. The level of iron consumed indicates the possibility of low bioavailability and anemia among insomniacs [31]. The other macro nutrient that is important with respect to sleep disturbance is carbohydrates [25]. Studies have reported that dietary carbohydrates promote good sleep through the secretion of serotonin, a hormone that directly influences sleep [25]. Deficiency of carbohydrates evidently induces midnight waking and food cravings, which disturb sleep [32]. These earlier findings correspond with our current results. Protein intakes were low among the insomniacs in this study. Information about the effects of protein on sleep is less available; hence, it is difficult to explain the influence of low consumption of dietary protein on sleep. However, there is the possibility that amino acids such as tryptophan and tyrosine are potent promoters of sleep, and protein deficiency could lead to lower availability of these amino acids and reduced sleep quality [33].
Intakes of the B vitamins riboflavin, niacin, B6, and folic acid were drastically decreased in all of the subjects included in this study; however, the deficiencies were markedly higher in the insomniacs. Vitamin B12 is reported to affect the body's biological rhythm, clinically; B12 supplementation improves the symptoms of sleep-wake rhythm disorders [7]. Experimental studies on humans and clinical evidence suggest that vitamin B12 plays a role in the entraining mechanism of the biological clock [6]. Evidently, intake of B12 by insomniacs with and without co-morbid symptoms was lower compared to normal sleepers. It can thus be assumed that poor sleep status affects food intake in several ways, possibly by lowering the appetite and also the desire to eat well. This can be explained on the basis of hormonal changes occurring during the night, which affect daytime eating behavior [34].
It can be concluded that although sleep is influenced by a variety of factors, sleep status and nutrient intakes are interdependent, since poor sleep may cause reduced food intake, and nutrient deficiency in turn could deteriorate sleep. Information about sleep status is essential, especially among productive age groups in a population. Lower intake of nutrients was observed more among insomniacs as compared to normal sleepers and this could be explanations of poor sleep status. Co-morbid symptoms sleep status and nutrient intake can influence each other. Further studies are required to confirm the association between nutrition and sleep.
References
- 1.Australasian Sleep Association [Internet] Available from: http://www.sleepaus.on.net/insomnia.insomniasig.html.
- 2.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18:257–261. doi: 10.3122/jabfm.18.4.257. [DOI] [PubMed] [Google Scholar]
- 3.Crisp AH, Stonehill E, Fenton GW. The relationship between sleep, nutrition and mood: a study of patients with anorexia nervosa. Postgrad Med J. 1971;47:207–213. doi: 10.1136/pgmj.47.546.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meolie AL, Rosen C, Kristo D, Kohrman M, Gooneratne N, Aguillard RN, Fayle R, Troell R, Townsend D, Claman D, Hoban T, Mahowald M Clinical Practice Review Committee; American Academy of Sleep Medicine. Oral nonprescription treatment for insomnia: an evaluation of products with limited evidence. J Clin Sleep Med. 2005;1:173–187. [PubMed] [Google Scholar]
- 5.Halson SL. Nutrition, sleep and recovery. Eur J Sport Sci. 2008;8:119–126. [Google Scholar]
- 6.Okawa M, Mishima K, Nanami T, Shimizu T, Iijima S, Hishikawa Y, Takahashi K. Vitamin B12 treatment for sleep-wake rhythm disorders. Sleep. 1990;13:15–23. doi: 10.1093/sleep/13.1.15. [DOI] [PubMed] [Google Scholar]
- 7.Ohta T, Ando K, Iwata T, Ozaki N, Kayukawa Y, Terashima M, Okada T, Kasahara Y. Treatment of persistent sleep-wake schedule disorders in adolescents with methylcobalamin (vitamin B12) Sleep. 1991;14:414–418. [PubMed] [Google Scholar]
- 8.Chan P, Huang TY, Chen YJ, Huang WP, Liu YC. Randomized, double-blind, placebo-controlled study of the safety and efficacy of vitamin B complex in the treatment of nocturnal leg cramps in elderly patients with hypertension. J Clin Pharmacol. 1998;38:1151–1154. [PubMed] [Google Scholar]
- 9.Earley CJ, Allen RP, Beard JL, Connor JR. Insight into the pathophysiology of restless legs syndrome. J Neurosci Res. 2000;62:623–628. doi: 10.1002/1097-4547(20001201)62:5<623::AID-JNR1>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 10.Lichstein KL, Payne KL, Soeffing JP, Heith Durrence H, Taylor DJ, Riedel BW, Bush AJ. Vitamins and sleep: an exploratory study. Sleep Med. 2007;9:27–32. doi: 10.1016/j.sleep.2006.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buscemi N, Vandermeer B, Friesen C, Bialy L, Tubman M, Ospina M, Klassen TP, Witmans M. Manifestations and Management of Chronic Insomnia in Adults. Evidence Reports/Technology Assessments. 2005. pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marr JW. Dietary survey methods: individual and group aspects. Proc R Soc Med. 1973;66:639–641. doi: 10.1177/003591577306600718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr. 1997;65(4 Suppl):1203S–1209S. doi: 10.1093/ajcn/65.4.1203S. [DOI] [PubMed] [Google Scholar]
- 14.Gopalan C, Rama Sastri BV, Balasubramanian SC, et al. Nutritive Value of Indian Foods. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 1980. [Google Scholar]
- 15.Rao Sowmya G, Puttaraj S. Nutrient intake and energy balance of adult women. Stud Home Comm Sci. 2007;1:31–37. [Google Scholar]
- 16.Gopalan C, Rama Sastri BV, Balasubramanian SC. Nutritive Value of Indian Foods. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 1993. [Google Scholar]
- 17.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4 Suppl):1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. discussion 1229S-1231S. [DOI] [PubMed] [Google Scholar]
- 18.Jelliffe DB. The assessment of the nutritional status of the community (with special reference to field surveys in developing regions of the world) Monogr Ser World Health Organ. 1966;53:3–271. [PubMed] [Google Scholar]
- 19.Wheeler L, inventor. Height measuring scale. Google Patents. 1946
- 20.Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr. 1991;65:105–114. doi: 10.1079/bjn19910073. [DOI] [PubMed] [Google Scholar]
- 21.Wells AS, Read NW, Uvnas-Moberg K, Alster P. Influences of fat and carbohydrate on postprandial sleepiness, mood, and hormones. Physiol Behav. 1997;61:679–686. doi: 10.1016/s0031-9384(96)00519-7. [DOI] [PubMed] [Google Scholar]
- 22.Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23:243–308. [PubMed] [Google Scholar]
- 23.Porter JM, Horne JA. Bed-time food supplements and sleep: effects of different carbohydrate levels. Electroencephalogr Clin Neurophysiol. 1981;51:426–433. doi: 10.1016/0013-4694(81)90106-1. [DOI] [PubMed] [Google Scholar]
- 24.Wells AS, Read NW, Idzikowski C, Jones J. Effects of meals on objective and subjective measures of daytime sleepiness. J Appl Physiol. 1998;84:507–515. doi: 10.1152/jappl.1998.84.2.507. [DOI] [PubMed] [Google Scholar]
- 25.Afaghi A, O'Connor H, Chow CM. High-glycemic-index carbohydrate meals shorten sleep onset. Am J Clin Nutr. 2007;85:426–430. doi: 10.1093/ajcn/85.2.426. [DOI] [PubMed] [Google Scholar]
- 26.Abraham GE, Hargrove JT. Effect of vitamin B-6 on premenstrual symptomatology in women with premenstrual tension syndromes: a double blind crossover study. Obstet Gynecol Surv. 1981;36:259–261. [Google Scholar]
- 27.Bernstein AL. Vitamin B6 in clinical neurology. Ann N Y Acad Sci. 1990;585:250–260. doi: 10.1111/j.1749-6632.1990.tb28058.x. [DOI] [PubMed] [Google Scholar]
- 28.Dean T, Jr, Allen RP, O'Donnell CP, Earley CJ. The effects of dietary iron deprivation on murine circadian sleep architecture. Sleep Med. 2006;7:634–640. doi: 10.1016/j.sleep.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 29.O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–203. doi: 10.1093/ageing/23.3.200. [DOI] [PubMed] [Google Scholar]
- 30.Allen RP, Earley CJ. Restless legs syndrome: a review of clinical and pathophysiologic features. J Clin Neurophysiol. 2001;18:128–147. doi: 10.1097/00004691-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Nutrient Requirement and Recommended Dietary Allowances. Hyderabad: National Institute of Nutrition; 1990. pp. 65–69. [Google Scholar]
- 32.Hajak G, Rodenbeck A, Staedt J, Bandelow B, Huether G, Rüther E. Nocturnal plasma melatonin levels in patients suffering from chronic primary insomnia. J Pineal Res. 1995;19:116–122. doi: 10.1111/j.1600-079x.1995.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 33.Hudson C, Hudson SP, Hecht T, MacKenzie J. Protein source tryptophan versus pharmaceutical grade tryptophan as an efficacious treatment for chronic insomnia. Nutr Neurosci. 2005;8:121–127. doi: 10.1080/10284150500069561. [DOI] [PubMed] [Google Scholar]
- 34.Van Cauter E, Holmback U, Knutson K, Leproult R, Miller A, Nedeltcheva A, Pannain S, Penev P, Tasali E, Spiegel K. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67(Suppl 1):2–9. doi: 10.1159/000097543. [DOI] [PubMed] [Google Scholar]