Abstract
Objective
Epidemiological evidence suggests that infections may contribute to atherogenesis. However, with the exception of Chlamydophila pneumoniae, cultivable bacteria have not been recovered from atherosclerotic lesions. Therefore, we aimed at developing an approach to recover uncultivable bacteria from atherectomy tissues.
Methods
We cultured homogenates from atherectomy specimens from seven non-septic patients undergoing surgery for arterial obstruction either alone or together with THP-1 monocyte-like cells. We performed 16S rDNA analysis, biochemical tests, random amplification of polymorphic DNA PCR analysis, quantitative polymerase chain reaction (qPCR) and immunohistofluorescence to identify the cultivated bacteria. Wilcoxon Signed-Rank Tests were used to determine whether THP-1 treatment yielded a higher number of isolates than did the untreated controls.
Results
We recovered more bacteria from co-cultures of atherectomy specimens with THP-1 cells than atherectomy specimens cultured alone. On average, tissue homogenates incubated with THP-1 cells vs control yielded 124 vs 22 colony-forming units (CFUs), a median of 140 vs. 7, respectively (p = 0.02). We recovered 872 isolates of limited number of species, including Propionibacterium acnes, Staphylococcus epidermidis and Streptococcus infantis and the fastidious anaerobe Porphyromonas gingivalis, and confirmed its presence in tissue using double immunofluorescence imaging. qPCR demonstrated the presence of ≥3.5 × 103 P. gingivalis genomes/g of atheromatous tissue.
Conclusions
These results indicate that viable previously uncultivable bacterial species are present within atheromas. Our results suggest revisiting the hypothesis that infections may have a causative role in atherosclerotic inflammation and have implications for research regarding novel diagnostics and treatments for cardiovascular disease.
Keywords: atherosclerosis, monocytes, Porphyromonas gingivalis, periodontal disease, bacterial infection
INTRODUCTION
Atherosclerosis is a chronic inflammatory condition associated with hypercholesterolemia, hypertension, diabetes, smoking, and genetic factors. Although it has been shown that these pro-inflammatory risk factors are highly prevalent among individuals with cardiovascular disease (CVD), the incidence of atherosclerosis is not fully explained by them [1]. An abundance of serological and epidemiological evidence supports a bacterial and viral infectious contribution towards the initiation and/or progression of atherosclerosis [2]. For example, Chlamydophila pneumoniae was cultivated from atheromas [3], [4] and DNA data suggest that various pathogens are associated with atherosclerotic tissue [5], [6]. Until now, however, no other bacteria could be cultivated from atheromas [7].
It has been suggested that large randomized controlled clinical trials of antibiotics in patients with pre-existing CVD [8] may have failed, in part, because the tested antibiotics lacked activity against non-cultivable bacteria. Chronic infection diseases such as periodontitis may underlie the failure of antibiotics to prevent acute ischemias. In concordance, clarithromycin treatment reduced recurrent cardiovascular events only in subjects without periodontitis, but failed in subjects with periodontitis most likely since it is not functional for periodontal therapy, lacking effect on dental biofilm microbiota [9]. Moreover, the focus on one organism (C. pneumoniae) was likely insufficient given the mounting evidence that multiple species are likely to coexist in atherosclerotic tissue [5], [6].
We hypothesized that oral flora bacteria may become uncultivable when they reside in cells of atheromatous tissues. Indeed, monocytes/macrophages, which are prominent residents of atheromatous tissues, harbor many facultative intracellular pathogens (e.g. Legionella, M. tuberculosis). Moreover, uncultivable Legionella sp. have been made cultivable by co-incubation with amoeba [10], and Tropheryma whippelii has been grown in vitro by co-incubation with human monocytes [11]. Therefore, we examined whether the human monocytic cell line THP-1 can facilitate recovery of uncultivable bacterial species from human atherectomy tissues.
MATERIALS AND METHODS
Processing of atheromatous tissue
We obtained carotid and femoral atherectomy tissues at surgery from 7 patients (men and women aged 58–79 years, see Table 1), 4 female, 3 male, average age 67.5 years, undergoing this procedure to relieve vascular obstruction. The specimens were obtained at surgery according to a protocol approved by Columbia University’s Institutional Review Board. Carotid or femoral atherectomy specimens (~100 mg wet weight) were obtained and immediately washed in sterile saline (4°C) to remove contaminating blood, homogenized in 5 ml RPMI medium (4°C) using a glass homogenizer, and sonicated for 30 sec at 4°C until no intact nucleated cells were visible by phase microscopic examination. A 625 μl aliquot of the homogenate was added to 1.375 ml of medium containing 105 THP-1 cells (ATCC, Manassas, VA), the mixture was placed in a 15.6 mm diameter tissue culture treated 24 well plate and incubated for 3 hours at 37°C in a 95% air/5% CO2 atmosphere. The suspension was centrifuged for 7 minutes at 800 × g and after concentration via high-speed centrifugation, the entire supernatant was plated on fastidious anaerobic agar (FAA) plates for 14 days at 37°C under aerobic and anaerobic conditions. The pelleted THP-1 cells were re-suspended in 2 ml of PBS, washed with this volume of medium 2 times by centrifugation at 800 × g for 7 min, re-suspended in 1 ml of water to lyse the THP-1 cells, and after concentration via high-speed centrifugation, the entire lysate was plated. Mendonca [12] reported that non-cultivable Listeria could be recovered only under strictly anaerobic conditions. Accordingly, we plated the lysate on fastidious anaerobic agar (FAA) plates and incubated them under anaerobic conditions at 37°C for 14 days. As a control, a second 625 μl aliquot of the atherectomy specimen homogenate was added to 1.375 ml PBS, incubated for 3 hours at 37°C in a 95% air/5% CO2 and plated on FAA plates as described above. As an additional control, THP-1 cells not incubated with homogenized atherectomy tissue were processed in parallel in the same manner. All procedures were carried out in an alcohol and UV-light sterilized laminar flow hood. We used the Wilcoxon Signed-Rank Test to compare the numbers of colonies of bacteria recovered from co-culture of atherectomy homogenate with pelleted THP-1 cells, the supernatant of the pelleted THP-1 cells, and the homogenate mixed with PBS. The corresponding volumes are reported in the table below.
Table 1.
Impact of incubation of homogenates of atherectomy tissues with vs. without THP-1 cells on recovery of bacteria from atherectomy specimens from 7 different non-septic afebrile patients.
| Patient # | Age, gender | Source of atherectomy specimen | CFU bacteria from homogenates incubated with THP-1 cells | CFU bacteria from homogenates incubated without THP-1 cells |
|---|---|---|---|---|
| 1 | 58, male | carotid artery | 256 | 1 |
| 2 | 73, female | carotid artery | 7 | 11 |
| 3 | 79, male | carotid artery | 2 | 3 |
| 4 | 67, female | femoral artery | 140 | 6 |
| 5 | 66, female | femoral artery | 159 | 13 |
| 6 | 66, male | carotid artery | 132 | 115 |
| 7 | 64, female | femoral artery | 176 | 7 |
| Average or total | 67.5 years | 872 | 156 |
| Outline of the procedure described above |
|---|
|
Biochemical identification of the clinical isolates
Clinical microbiology analysis of bacterial strains was performed with Advanced Expert System software in conjunction with the VITEK 2 test system (BioMérieux, Inc., Hazelwood, MO) in Columbia University’s Clinical Microbiology Service.
Bacterial genomic DNA isolation, 16S rDNA gene amplification, GenBank and phylogenetic analysis
Genomic DNAs from twenty P. gingivalis and two P. acnes clinical isolates were isolated and 1,516 bp segments of 16S rDNAs were amplified using Platinum Blue PCR Supermix (Invitrogen, Carlsbad, CA) with universal 16S rDNA primers 9F (5′-GAGTTTGATYMTGGCTCAG-3′) and 1541R (5′-AAGGAGGTGWTCCARCC-3′)[13] using initial denaturation at 94°C for 2 minutes followed by 40 cycles (94°C/30 seconds, 52°C/30 seconds, 72°C/1 minute) with a final primer extension for 5 minutes at 72°C. The resulting 1.5 kb PCR fragments from two P. gingivalis isolates, CU1 and CU2 was sequenced on 3730xl DNA Analyzer (Applied Biosystems, Foster City, CA) with the same primers and with an additional internal primer 530R (5′-GTGCCAGCAGCCGCGG-3′). The complete sequences of the 16S rDNA segments were assembled and further analyzed using NCBI (http://blast.ncbi.nlm.nih.gov/Blast.cgi), Ribosomal Database Project (RDP) 16S RNA classifier [14] at the Ribosomal Database project website (http://rdp.cme.msu.edu/index.jsp) and Green Genes at Lawrence Berkeley National Laboratory (http://greengenes.lbl.gov/cgi-bin/nph-index.cgi). In addition, all P. gingivalis isolates were analyzed using species-specific 16S rDNA PCR, as described [6].
RAPD-PCR analysis
For genetic polymorphism analysis of the P. gingivalis isolates, random amplification of polymorphic DNA (RAPD) PCR analysis was carried out as described [15], with primer #01–05 and 100 ng DNA template (seven isolates, the lab strain W83, and five strains from the collection: 33277, 381, AJW2, AJW4 and A7436).
Isolation of total genomic DNA from the tissue
Genomic DNAs from atheromas were isolated as previously described [6].
Tissue analysis for P. gingivalis DNA using quantitative polymerase chain reaction (qPCR)
We tested total DNA from the atheromatous tissue for P. gingivalis DNA using 16S rDNA and ragA gene amplification (http://cmr.jcvi.org/tigr-scripts/CMR/GenomePage.cgi?database=gpg). The primers (forward, 5′-CATAGATATCACGAGGAACTCCGATT-3′ and reverse, 5′-AAACTGTTAGCAACTACCGATGTGG-3′) [6] define a 436 bp amplicon of the 16S RNA sequence of P. gingivalis and the primers (forward, 5′-TTTGCCTGAACACAGAGTCG-3′ and reverse, 5′-GACTGCTTTTCCCACGAGAG-3′) define a 369 bp amplicon of the ragA gene. A series of 10X dilution calibration samples were used starting at 500 pg.μl−1 down to 0.5 fg.μl−1 or ~0.16 molar equivalents of target DNA per microliter. Three replicates containing 3 μl (100 ng) of the DNA isolated from the atheromatous samples were amplified in real-time PCR against three replicates of serially diluted P. gingivalis calibration samples and six template-free controls using 17 μl of 1x Platinum SYBR Green qPCR SuperMix-UDG (Invitrogen) and amplified for 40 cycles using an ABI 7000 Sequence analysis system with the default protocol. Upon the completion of the protocol, the levels of the positive signals obtained in the PCR with atheromatous samples were compared with tissue-free controls using Student’s t-test. The specificity of each amplicon was interrogated with melting curve analysis, amplicon size analysis using Agilent Bioanalyzer, and – finally - by sequencing.
Metagenomic screening of diseased and healthy control tissue pairs
As controls, five pairs of human diseased and matching adjacent healthy (D/H) post mortem tissue were analyzed for presence of eubacterial DNA. The specimens were obtained according to approved Institutional Review Board protocol. The analysis was performed using 16S rDNA amplification, as follows. A 1,516-bp segment of 16S rDNA was amplified from the genomic DNA templates using Advantage 2 Polymerase mix (Clontech) with universal 16S rDNA primers 9F (5′-GAGTTTGATYMTGGCTCAG-3′) and 1541R (5′-AAGGAGGTGWTCCARCC-3′) [16]. A “no template control” reaction was included in the experimental protocol to monitor for the external contamination of the samples.
Immunohistofluorescent detection of P. gingivalis in a plaque specimen
Carotid specimen #1 was embedded in OCT medium and frozen at −70° C. Blocks were cut to 5 μm thick pieces using a cryostat and the ribbon of tissue was put on a poly-L-lysine-coated slide and dried. The slides were fixed in acetone and blocked overnight at 4° C in 5% bovine serum albumin and 1% dry milk. For staining, mouse anti-P. gingivalis IgG1 antibody 61BG1.3 [17] (kindly provided by R. Gmur) was diluted 1:50. Slides were incubated at 37° C for 1.5 hours, washed in PBS, and treated with the secondary Alexa Fluor 456-conjugated goat anti-mouse antibody (Invitrogen, 4 μg.ml−1) for 1 hour. Unrelated mouse IgG1 isotype controls (Santa Cruz Biotechnology, Santa Cruz, CA) were also used. To confirm the P. gingivalis staining specificity, the specimens were double stained using a rabbit anti-P. gingivalis serum [18] diluted 1:50 for incubation at 37° C for 1.5 hours. The slides were washed in PBS, incubated in the secondary goat anti-rabbit Alexa Fluor 488-conjugated antibody (A11008, Invitrogen) (4 μg.ml−1) for 1 hour and viewed in a fluorescent microscope Nikon Eclipse 80i. As additional control, slides were processed without primary rabbit antibody.
In addition, immunohistochemical detection of P. gingivalis in the tissue was performed in a similar fashion using the monoclonal anti-P. gingivalis antibody as described above, with a goat anti-mouse AP-conjugated secondary antibody (Zymed, San Fransisco, US). The slides were further incubated with 5-Bromo-4-chloro-3-indolyl phosphate (Sigma, St Louis, US) for 1 hour, stained with Meyer’s Hematoxylin (Sigma, St Louis, US) for 3 minutes and washed for 3 minutes in running water. As control, same isotype unrelated antibody was used.
RESULTS
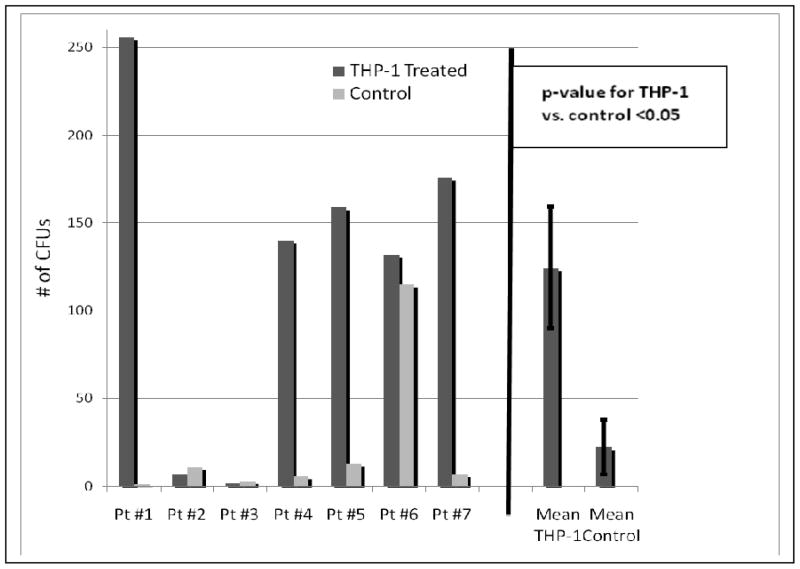
We recovered 5.6-fold more bacterial colonies from homogenates of the 7 atherectomy specimens incubated with THP-1 cells than from the same homogenates incubated in medium without THP-1 cells (872 vs. 156 colonies) (Table 1). Ninety eight percent of the recovered 872 bacterial colonies (from THP-1 cells that had been incubated with homogenates of atherectomy tissues) were from 5 of the 7 patients, and 74% of the 156 bacterial colonies recovered from controls (homogenates incubated in medium without THP-1 cells) were from 1 of the 7 patients (Fig. 1). This is consistent with previously observed inter-individual variation [5]. The ratio of bacterial colonies recovered from homogenates from 4 of the 7 patients incubated with vs. without THP-1 cells was 27:1 (Table 1).
Figure 1.
Left, number of CFUs isolated from each of 7 surgical atherectomy specimens from 7 different patients. THP-1 treated = homogenates of atherectomy tissues incubated with THP-1 cells for 3 h at 37°C and then plated on FAA agar. Control = an equal volume of atherectomy tissue homogenate incubated without THP-1 cells for 3 h at 37°C and plated on FAA agar. Right, mean (+/−SEM) number of isolates recovered with THP-1 cells vs. without THP-1 cells (p for difference = 0.02 using Wilcoxon Signed-Rank Test). Pt, patient.
To determine whether the recovered bacteria were intracellular, a control experiment, with an additional step was carried out in parallel. Before lysis, the THP-1 cells were treated with antibiotics (gentamicin, 300 μg/ml and metronidazole, 200 μg/ml) for 1 hour to kill all bacteria that had not invaded. The resulting numbers of recovered intracellular bacteria were matching those of non-antibiotic treated specimen, indicating that all were intracellular.
We used the Wilcoxon Signed-Rank Test to determine whether the THP-1 co-cultivation method increased the recovery as compared to the PBS suspension method. On average atherectomy homogenates incubated with THP-1 cells vs in PBS without THP-1 cells yielded 124 vs 22 colony-forming units (CFUs), a median of 140 vs. 7, respectively (p = 0.02) (Fig. 1). THP-1 cells alone did not produce any bacterial colonies. THP-1 incubation with atherectomy homogenate from patient 1 followed by lysis and incubation in anaerobic environment produced 20 black-pigmenting colonies in addition to 236 other colonies of different morphologies. Rapid illumination of the black-pigmented colonies with long-wave UV demonstrated no fluorescence, suggesting the species was P. gingivalis.
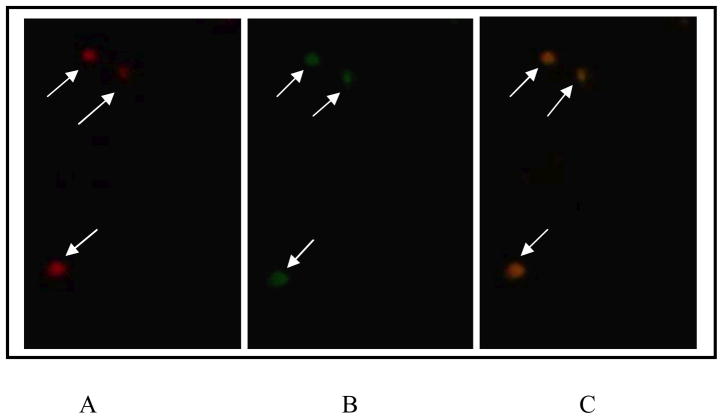
Indirect immunofluorescence with both mouse and rabbit anti-P. gingivalis antibodies further confirmed the presence of P. gingivalis in sections of atherosclerotic plaque from patient 1 (Fig. 2). The preservation of the specimens was not of sufficient quality to determine whether these bacteria were contained within human cells within the plaques.
Fig. 2.
Detection of P. gingivalis in carotid atheromatous tissue sections using double immunohistofluorescence and two different antibodies. Images are representative; three separate slides yielded similar results.
A, Primary antibody, mouse anti-P. gingivalis IgG1 monoclonal antibody 61BG1.3; secondary antibody, Alexa Fluor 456-conjugated goat anti-mouse antibody (red).
B, Primary antibody, rabbit anti-P. gingivalis serum; secondary antibody, goat anti-rabbit Alexa Fluor 488-conjugated antibody (green).
C, Colocalization of both stains is represented as overlap of the preceding images.
Negative controls (not shown): primary mouse unrelated IgG1 isotype control antibody and primary rabbit antibody (omitted). Scale bar, 10 μm.
Biochemical analysis of the isolates was performed with Advanced Expert System software in conjunction with the VITEK 2 test system (BioMerieux Inc., Hazelwood, MO) in the Columbia University Clinical Microbiology Service. Further, 16S rDNA sequencing of an additional 32 amplicons from non-pigmenting isolates from different phenotypes identified them as P. acnes, S. epidermidis and S. infantis. Amplification with universal primers of genomic DNA from 6 black-pigmenting isolates followed by sequencing and nucleotide database analysis confirmed they were P. gingivalis (see Methods). To assess the genetic relatedness between the recovered P. gingivalis isolates, we used RAPD PCR analysis [15] (Fig. 3). The analyzed P. gingivalis isolates gave identical patterns and displayed on 1% agarose gel a pattern different from that of the W83 strain used in our laboratory, and from the other strains in the tested collection (not shown). All 20 black-pigmenting isolates from patient #1 were positively identified as P. gingivalis with species-specific 16S rDNA PCR (data not shown).
Figure 3.
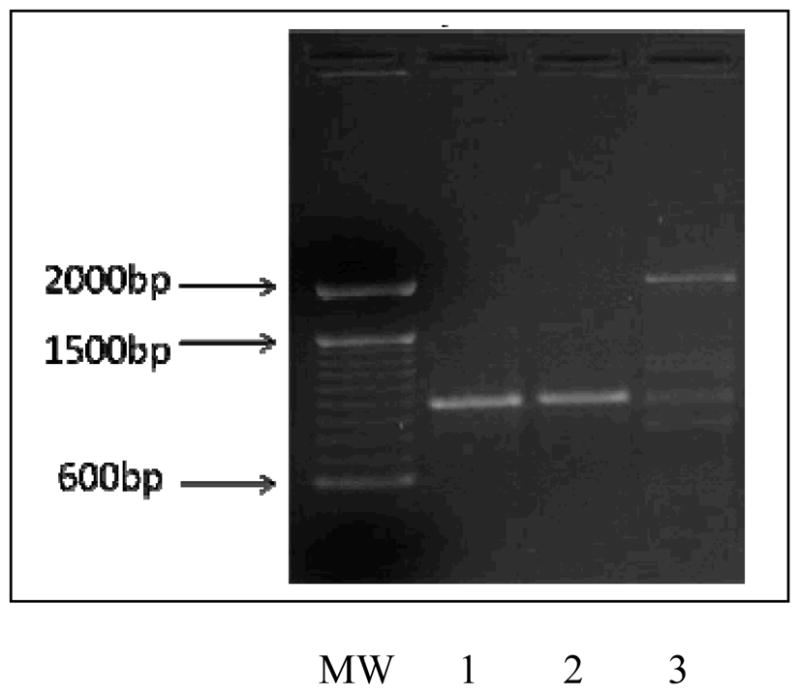
RAPD-PCR profiles of amplification using DNA template from P. gingivalis isolates recovered form atheromatous tissue.
Lanes 1 and 2, profile of P. gingivalis clinical isolates CU1 and CU2. Lane 3, control P. gingivalis W83. MW, molecular mass marker with major bands indicated.
Quantitative PCR analysis of total atheromatous tissue DNA of patient 1 demonstrated the presence of at least 3.5 × 103 P. gingivalis genomes/gm tissue. We were unable to process for cultivation non-diseased tissue samples controls from patients for ethical reasons. We have, however, analyzed arterial tissues from atherosclerotic lesions and normal arteries of non-survivors (obtained 24–48 hrs after death) using 16S rDNA PCR. The metagenomic analysis of the 16S amplicons from atheromatous tissue and matching healthy control from the same patient identified a higher presence of bacterial species in diseased tissues, as compared to healthy controls (15 vs. 7). These data are in line with the reported prevalence of bacterial DNA in diseased tissues compared to healthy control material from 26 individuals [5].
DISCUSSION
A large body of evidence links chronic infections in to CVD [19], [20], Nevertheless, the evidence for causality is still lacking [21]. This has led to two hypotheses regarding the role of periodontal bacteria in atherogenesis. Our current findings advance this science considerably by informing a direct infection hypothesis. It posits that periodontal bacteria (e.g., P. gingivalis), are phagocytosed by monocytes in oral tissues and carried within them via the blood to atheromatous lesions (the “Trojan horse” model). According to this hypothesis, these bacteria persist within lesional monocytes/macrophages and stimulate them to secrete pro-inflammatory substances (e.g., TNFα). Phagocytic cells have been shown to harbor viable C. pneumoniae while at the same time protecting the intracellular bacteria from antibiotic treatment [22]. A variant of the direct invasion hypothesis is that periodontal bacteria invade the bloodstream and metastasize without the aid of monocytes to atheromatous lesions.
The second, or indirect hypothesis, posits that chronic low-grade “systemic” inflammation, induced by persistent periodontal bacterial infection, can cause endothelial dysfunction and initiate and perpetuate atherogenesis. Consistent with both hypotheses, a recent randomized clinical trial demonstrated sustained reductions in endothelial dysfunction after periodontal therapy despite limited long-term effects on systemic inflammatory markers [23].
The most direct way to distinguish between the direct and indirect hypotheses is to determine whether bacteria from the oral flora are present within atheromatous tissues and whether they remain viable and/or grow within cells that participate in atherogenesis. Accordingly, using quantitative PCR analysis, we [24], [25], [26], [27], [6], and others [5], [28], [29] have identified bacteria or bacterial DNA in the atheromas, shown bacteria can persist in vascular cells for extended periods of time, and demonstrated they directly initiate and/or exacerbate atherogenesis. Bacterial DNA was mainly found in diseased vascular tissues but not in healthy tissues [5]. Serum IgA antibody titers to Aggregatibacter actinomycetemcomitans or to C. pneumoniae heat shock protein 60 were associated with coronary obstruction [30]. While these studies provide support for the direct hypothesis, they provide no insight into the underlying mechanisms.
The cultivation and identification of a number of bacterial species in diseased vascular tissue is a necessary advancement of the direct biological hypothesis in addition to fulfilling the Koch’s postulate. Admittedly, Koch’s postulates might not be entirely appropriate in the context of a hypothesis that allows for multiple causative agents and suggests that infections alone are unlikely to be either sufficient or necessary causes of CVD. Chronic respiratory, urinary tract, dental, and other infections increased the risk of carotid atherosclerosis according to a large epidemiological study [31]. No single infectious organism has so far been identified as causative agent of atherosclerosis, therefore summary measures of multiple chronic infectious exposures, or “infectious burden,” have been associated with the risk of stroke and atherosclerosis affecting the carotid arteries [32]. This burden includes C. pneumoniae or viral infections such as herpes simplex virus, hepatitis virus and influenza [33], [30]. Nevertheless, the isolation from diseased human vascular tissue of a microbial species a priori hypothesized to have atherogenic potential is an important step forward. Moreover, the specific periodontal organisms identified are noteworthy. Accumulating evidence has implicated specific infectious agents in the progression of atherosclerosis, including the oral pathogen P. gingivalis [34]. Accordingly, P. gingivalis is also strongly associated with periodontal inflammation, but not with healthy state [35]. P. acnes, also a member of the periodontal microbiota [36], is the most prevalent species in apical periodontitis lesions [37] and has been recovered from root canals and from blood samples taken during and after endodontic treatment [38], [39].
Five of the seven studied specimens yielded most isolates, which reflects previously observed inter-individual variation and the dynamic composition of human microbiota [5], [40]. Ott et al. reported high bacterial diversity in atheromas with a range of 5 to 22. This may also mean low bacterial survival or indirect infection as cause of atherosclerotic inflammation in two of the patients.
However, unlike the findings with DNA-based detection methods, here we report the recovery of only a small number of bacterial species. This indicates that the inflammation may be associated with limited spectrum of organisms; therefore an additional benefit of our approach may be a reduction in false positive findings. Importantly, the present study, first of its kind, defines the possibility to design qualitative and quantitative studies of the association of specific bacteria with clinical measures of disease.
While P. acnes, S. epidermidis and S. infantis could have originated from many bodily sites, including periodontium, the presence of P. gingivalis is consistent with systemic periodontal infection. Whatever their site of origin, these findings support the direct invasion hypothesis. They are consistent with our finding that “infectious burden” is associated with stroke risk and carotid plaque thickness [41], with the report that systemic exposure to P. gingivalis increases the risk of stroke[42] and with reports that oral colonization with periodontal bacterial pathogens is associated with increased carotid artery intima-media thickness [43].
Acknowledgments
This work was supported by the Columbia University College of Dental Medicine, Section of Oral and Diagnostic Sciences and National Heart, Lung and Blood Institute, HL72002. We thank Dr. Samuel C. Silverstein for critical analysis of these results and for editorial assistance in preparation of this manuscript.
Footnotes
Conflict of interest: Authors have no conflict of interest to declare.
References
- 1.Katz JT, Shannon RP. Bacteria and coronary atheroma: more fingerprints but no smoking gun. Circulation. 2006;113:920–2. doi: 10.1161/CIRCULATIONAHA.105.607358. [DOI] [PubMed] [Google Scholar]
- 2.Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340:115–26. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 3.Jackson LA, Campbell LA, Kuo CC, Rodriguez DI, Lee A, Grayston JT. Isolation of Chlamydia pneumoniae from a carotid endarterectomy specimen. J Infect Dis. 1997;176:292–5. doi: 10.1086/517270. [DOI] [PubMed] [Google Scholar]
- 4.Saikku P. Chlamydia pneumoniae in atherosclerosis. J Intern Med. 2000;247:391–6. doi: 10.1046/j.1365-2796.2000.00659.x. [DOI] [PubMed] [Google Scholar]
- 5.Ott SJ, El Mokhtari NE, Musfeldt M, et al. Detection of diverse bacterial signatures in atherosclerotic lesions of patients with coronary heart disease. Circulation. 2006;113:929–37. doi: 10.1161/CIRCULATIONAHA.105.579979. [DOI] [PubMed] [Google Scholar]
- 6.Kozarov E, Sweier D, Shelburne C, Progulske-Fox A, Lopatin D. Detection of bacterial DNA in atheromatous plaques by quantitative PCR. Microbes Infect. 2006;8:687–93. doi: 10.1016/j.micinf.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Fiehn NE, Larsen T, Christiansen N, Holmstrup P, Schroeder TV. Identification of periodontal pathogens in atherosclerotic vessels. J Periodontol. 2005;76:731–6. doi: 10.1902/jop.2005.76.5.731. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JL. Infection, antibiotics, and atherothrombosis--end of the road or new beginnings? N Engl J Med. 2005;352:1706–9. doi: 10.1056/NEJMe058019. [DOI] [PubMed] [Google Scholar]
- 9.Paju S, Sinisalo J, Pussinen PJ, Valtonen V, Nieminen MS. Is periodontal infection behind the failure of antibiotics to prevent coronary events? Atherosclerosis. 2007;193:193–5. doi: 10.1016/j.atherosclerosis.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Steinert M, Emody L, Amann R, Hacker J. Resuscitation of viable but nonculturable Legionella pneumophila Philadelphia JR32 by Acanthamoeba castellanii. Appl Environ Microbiol. 1997;63:2047–53. doi: 10.1128/aem.63.5.2047-2053.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoedon G, Goldenberger D, Forrer R, et al. Deactivation of macrophages with interleukin-4 is the key to the isolation of Tropheryma whippelii. J Infect Dis. 1997;176:672–7. doi: 10.1086/514089. [DOI] [PubMed] [Google Scholar]
- 12.Mendonca AF, Knabel SJ. A novel strictly anaerobic recovery and enrichment system incorporating lithium for detection of heat-injured Listeria monocytogenes in pasteurized milk containing background microflora. Appl Environ Microbiol. 1994;60:4001–8. doi: 10.1128/aem.60.11.4001-4008.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bahrani-Mougeot FK, Paster BJ, Coleman S, Ashar J, Barbuto S, Lockhart PB. Diverse and novel oral bacterial species in blood following dental procedures. J Clin Microbiol. 2008;46:2129–32. doi: 10.1128/JCM.02004-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cole JR, Wang Q, Cardenas E, et al. The Ribosomal Database Project: improved alignments and new tools for rRNA analysis. Nucleic Acids Res. 2009;37:D141–5. doi: 10.1093/nar/gkn879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshino T, Laine ML, van Winkelhoff AJ, Dahlen G. Genotypic characterization of Porphyromonas gingivalis isolated from Swedish patients with periodontitis and from periodontal abscesses. Oral Microbiol Immunol. 2007;22:195–200. doi: 10.1111/j.1399-302X.2007.00350.x. [DOI] [PubMed] [Google Scholar]
- 16.Bahrani-Mougeot FK, Paster BJ, Coleman S, et al. Molecular analysis of oral and respiratory bacterial species associated with ventilator-associated pneumonia. J Clin Microbiol. 2007;45:1588–93. doi: 10.1128/JCM.01963-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gmur R, Werner-Felmayer G, Guggenheim B. Production and characterization of monoclonal antibodies specific for Bacteroides gingivalis. Oral Microbiol Immunol. 1988;3:181–6. doi: 10.1111/j.1399-302x.1988.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 18.Progulske-Fox A, Tumwarson S, Holt SC. The expression and function of Bacteroides gingivalis hemagglutinin gene in Escherichia coli. Oral Microbiol Immunol. 1989;4:121–31. doi: 10.1111/j.1399-302x.1989.tb00238.x. [DOI] [PubMed] [Google Scholar]
- 19.Offenbacher S, Beck JD. A perspective on the potential cardioprotective benefits of periodontal therapy. Am Heart J. 2005;149:950–4. doi: 10.1016/j.ahj.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 20.Gibson FC, 3rd, Yumoto H, Takahashi Y, Chou HH, Genco CA. Innate Immune Signaling and Porphyromonas gingivalis-accelerated Atherosclerosis. J Dent Res. 2006;85:106–21. doi: 10.1177/154405910608500202. [DOI] [PubMed] [Google Scholar]
- 21.Friedewald VE, Kornman KS, Beck JD, et al. The American Journal of Cardiology and Journal of Periodontology Editors’ Consensus: periodontitis and atherosclerotic cardiovascular disease. Am J Cardiol. 2009;104:59–68. doi: 10.1016/j.amjcard.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Gieffers J, Fullgraf H, Jahn J, et al. Chlamydia pneumoniae infection in circulating human monocytes is refractory to antibiotic treatment. Circulation. 2001;103:351–6. doi: 10.1161/01.cir.103.3.351. [DOI] [PubMed] [Google Scholar]
- 23.Tonetti MS. Periodontitis and risk for atherosclerosis: an update on intervention trials. J Clin Periodontol. 2009;36 (Suppl 10):15–9. doi: 10.1111/j.1600-051X.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 24.Kozarov E, Dorn B, Shelburne C, Dunn W, Progulske-Fox A. Human atherosclerotic plaque contains viable invasive Porphyromonas gingivalis and Actinobacillus actinomycetemcomitans. Arterioscler Thromb Vasc Biol. 2005;25:e17–8. doi: 10.1161/01.ATV.0000155018.67835.1a. [DOI] [PubMed] [Google Scholar]
- 25.Demmer RT, Desvarieux M. Periodontal infections and cardiovascular disease: the heart of the matter. J Am Dent Assoc. 2006;137(Suppl):14S–20S. doi: 10.14219/jada.archive.2006.0402. quiz 38S. [DOI] [PubMed] [Google Scholar]
- 26.Li L, Michel R, Cohen J, DeCarlo A, Kozarov E. Intracellular survival and vascular cell-to-cell transmission of Porphyromonas gingivalis. BMC Microbiol. 2008 Feb 6;8:26–36. doi: 10.1186/1471-2180-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rafferty B, Dolgilevich S, Kalachikov S, et al. Cultivation of Enterobacter hormaechei from human atherosclerotic tissue. J Atherosclerosis Thrombosis. 2011;18:72–81. doi: 10.5551/jat.5207. [2010, Oct 20 Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Lalla E, Lamster IB, Hofmann MA, et al. Oral infection with a periodontal pathogen accelerates early atherosclerosis in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2003;23:1405–11. doi: 10.1161/01.ATV.0000082462.26258.FE. [DOI] [PubMed] [Google Scholar]
- 29.Amar S, Wu SC, Madan M. Is Porphyromonas gingivalis cell invasion required for atherogenesis? Pharmacotherapeutic implications. J Immunol. 2009;182:1584–92. doi: 10.4049/jimmunol.182.3.1584. [DOI] [PubMed] [Google Scholar]
- 30.Pesonen E, El-Segaier M, Persson K, Puolakkainen M, Sarna S, Ohlin H, Pussinen PJ. Infections as a stimulus for coronary occlusion, obstruction, or acute coronary syndromes. Ther Adv Cardiovasc Dis. 2009;3:447–54. doi: 10.1177/1753944709345598. [DOI] [PubMed] [Google Scholar]
- 31.Kiechl S, Egger G, Mayr M, et al. Chronic infections and the risk of carotid atherosclerosis: prospective results from a large population study. Circulation. 2001;103:1064–70. doi: 10.1161/01.cir.103.8.1064. [DOI] [PubMed] [Google Scholar]
- 32.Elkind MS. Inflammatory mechanisms of stroke. Stroke. 2010;41:S3–8. doi: 10.1161/STROKEAHA.110.594945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huittinen T, Leinonen M, Tenkanen L, et al. Synergistic effect of persistent Chlamydia pneumoniae infection, autoimmunity, and inflammation on coronary risk. Circulation. 2003;107:2566–70. doi: 10.1161/01.CIR.0000068338.17948.22. [DOI] [PubMed] [Google Scholar]
- 34.Gibson FC, 3rd, Genco CA. Porphyromonas gingivalis mediated periodontal disease and atherosclerosis: disparate diseases with commonalities in pathogenesis through TLRs. Curr Pharm Des. 2007;13:3665–75. doi: 10.2174/138161207783018554. [DOI] [PubMed] [Google Scholar]
- 35.Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL., Jr Microbial complexes in subgingival plaque. J Clin Periodontol. 1998;25:134–44. doi: 10.1111/j.1600-051x.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 36.Fritschi BZ, Albert-Kiszely A, Persson GR. Staphylococcus aureus and other bacteria in untreated periodontitis. J Dent Res. 2008;87:589–93. doi: 10.1177/154405910808700605. [DOI] [PubMed] [Google Scholar]
- 37.Fujii R, Saito Y, Tokura Y, Nakagawa KI, Okuda K, Ishihara K. Characterization of bacterial flora in persistent apical periodontitis lesions. Oral Microbiol Immunol. 2009;24:502–5. doi: 10.1111/j.1399-302X.2009.00534.x. [DOI] [PubMed] [Google Scholar]
- 38.Debelian GJ, Olsen I, Tronstad L. Profiling of Propionibacterium acnes recovered from root canal and blood during and after endodontic treatment. Dental Traumatology. 1992;8:248–54. doi: 10.1111/j.1600-9657.1992.tb00253.x. [DOI] [PubMed] [Google Scholar]
- 39.Debelian GJ, Olsen I, Tronstad L. Anaerobic bacteremia and fungemia in patients undergoing endodontic therapy: an overview. Ann Periodontol. 1998;3:281–7. doi: 10.1902/annals.1998.3.1.281. [DOI] [PubMed] [Google Scholar]
- 40.Lipkin WI. Microbe hunting. Microbiol Molec Biol Reviews. 2010;74:1–16. doi: 10.1128/MMBR.00007-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elkind MS, Luna JM, Moon YP, et al. Infectious burden and carotid plaque thickness: the northern Manhattan study. Stroke. 2010;41:e117–22. doi: 10.1161/STROKEAHA.109.571299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pussinen PJ, Alfthan G, Jousilahti P, Paju S, Tuomilehto J. Systemic exposure to Porphyromonas gingivalis predicts incident stroke. Atherosclerosis. 2007;193:222–8. doi: 10.1016/j.atherosclerosis.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 43.Desvarieux M, Demmer RT, Rundek T, Boden-Albala B, Jacobs DR, Jr, Sacco RL, Papapanou PN. Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST) Circulation. 2005;111:576–82. doi: 10.1161/01.CIR.0000154582.37101.15. [DOI] [PMC free article] [PubMed] [Google Scholar]