Abstract
Objective
Patellar bracing is a mechanical treatment strategy for patellofemoral osteoarthritis (OA) that aims to unload the lateral compartment of the joint by translating the patella medially. Our objective was to determine whether a patellar brace can correct patellar kinematics in patients with patellofemoral OA.
Design
We assessed the effect of a patellar brace on three-dimensional patellar kinematics (flexion, spin and tilt; proximal, lateral and anterior translation) at sequential, static knee postures, using a validated MRI-based method, in 19 patients with radiographic lateral patellofemoral OA. Differences in kinematics between un-braced and braced conditions were assessed in the unloaded and loaded knee (15% bodyweight load) using hierarchical linear random-effects models. Random slope and quadratic terms were included in the model when significant (p<0.05).
Results
Bracing with load caused the patellae to translate 0.46 mm medially (p<0.001), tilt 1.17° medially (p<0.001), spin 0.62° externally (p=0.012) and translate 1.09 mm distally (p<0.001) and 0.47 mm anteriorly (p<0.001) over the range of knee flexion angles studied. Bracing also caused the patellae to extend in early angles of knee flexion (p<0.001). The brace caused similar trends for the unloaded condition, though magnitudes of the changes varied.
Conclusion
Bracing changed patellar kinematics, but these changes did not appear large enough to be clinically meaningful because no reduction in pain was observed in the parent study.
Keywords: Patella, patellofemoral, osteoarthritis, brace, kinematics, MRI
Introduction
Knee osteoarthritis (OA) is symptomatic in 12.1% of Americans over 60 years of age1, and the patellofemoral joint is involved in 50% of all radiographic knee osteoarthritis cases in either an isolated form or combined with tibiofemoral OA2. Despite the prevalence of patellofemoral OA, the patellofemoral joint has received relatively little attention in the OA literature and there are few treatment options for individuals with patellofemoral OA. Patellar malalignment is associated with radiographic patellofemoral OA progression and symptoms3 and with magnetic resonance imaging (MRI) measures of cartilage loss and bone marrow lesions4. It is hypothesized that correcting patellar malalignment using strategies such as bracing or taping may arrest OA symptoms and progression. Patellar taping has reduced pain in patients with symptomatic generalized knee OA5,6 and with clinical and radiographic patellofemoral OA7,8. Taping also reduced lateral patellar tilt and displacement in the latter group8.
The mechanical aim of a patellofemoral brace is to change patellofemoral kinematics, specifically to cause a medial translation of the patella thereby unloading the lateral compartment. Bracing is considered suitable for individuals with lateral patellar tracking, isolated lateral patellofemoral OA or bi-compartmental patellofemoral OA. Bracing is a commonly used treatment strategy because of its relatively low cost and ease of implementation. Further, it does not have some of the limitations of taping including loosening, skin irritation due to the adhesive and the technical skill requirement for application. However, it is unclear whether a patellar brace is capable of changing patellofemoral joint kinematics in subjects with patellofemoral OA.
Patellar kinematics have been assessed in vivo using computed tomography9,10, fluoroscopy11–13 and MRI14–20. The advantage of MRI-based methods is that no ionizing radiation is used and therefore kinematics can be assessed longitudinally or under multiple test conditions. Two-dimensional MRI-based methods have been developed15,18,20, however, they are limited because patellar tracking is only evaluated in one plane (usually axial). Three-dimensional patellar kinematics assessments with MRI provide a more complete description of patellar tracking, including translations and rotations in all three planes. The range of knee flexion can be studied by measuring patellar position in sequential static postures of the loaded knee16,17. In these methods, subjects lie supine in the MRI scanner and load the knee in a simulation of weightbearing by pressing the foot against a custom designed pedal system. These methods have been used to study individuals with knee OA21, ACL injury22 and patellofemoral pain syndrome23,24 but they have not been applied to a population of individuals with patellofemoral OA.
Although patellar kinematics have not been assessed in the patellofemoral OA population, the effect of a patellofemoral brace has been assessed in individuals with patellofemoral pain. One study of two-dimensional patellar kinematics in loaded, sequential static postures reported that lateral translation was reduced when the brace was applied in subjects with patellofemoral pain25. In a more recent study of two-dimensional patellar kinematics, assessed during continuous flexion in weightbearing using an open-bore MRI scanner, the brace reduced lateral tilt and translation in subjects with patellofemoral pain26. It is not clear whether the same changes in kinematics observed in the patellofemoral pain population would also be observed in the patellofemoral OA population with its attendant structural changes, such as the degeneration of articular cartilage or presence of osteophytes which may constrain patellar motion. It is also unclear how a patellar brace affects patellar kinematics in three dimensions. The aim of the current study was to assess the effect of a patellofemoral brace on three-dimensional patellar kinematics in individuals with radiographic lateral patellofemoral OA.
Methods
Subjects
Twenty subjects with symptomatic radiographic lateral patellofemoral OA were recruited to participate in this study. This group was a subset of participants enrolled in a randomized crossover trial examining the efficacy of an intervention brace and a control brace for reducing knee pain27. There was a 6 week washout period between treatment phases. The kinematic assessment for the current study took place approximately 2 weeks into the phase of the study where the experimental brace was worn. Subjects were included in this study if they had knee pain on most days of the past month and either isolated patellofemoral OA or patellofemoral OA with concomitant tibiofemoral OA. Radiographic patellofemoral OA was defined as a grade 2 or above osteophyte (0–3 scale) or joint space narrowing of greater than 1 (0–3 scale) with a concurrent grade 1 osteophyte on a skyline radiograph in accordance with the OARSI atlas. Tibiofemoral OA was defined as a Kellgren/Lawrence grade 2 or above from a posteroanterior radiograph. Subjects with concomitant tibiofemoral OA were only included if the symptoms of pain location or physical examination findings were consistent with patellofemoral disease as the predominant source of symptoms. The study was approved by the Boston University Medical Center and University of British Columbia institutional review board and all subjects gave informed consent.
Patellar Brace
The patellar brace used in this study was a standard sleeve with a T-strap (Bio Skin Q, Cropper Medical Inc., Ashland, OR, USA) (Figure 1). The T-strap was positioned to create a medial translation of the patella. A trained research assistant (KH) instructed participants on correctly donning and doffing the brace.
Figure 1.
The patellar brace (Bio Skin Q, Cropper Medical Inc., Ashland, OR, USA) evaluated in this study.
Three-Dimensional Patellar Kinematics
We assessed three-dimensional patellar kinematics in each subject using a validated, noninvasive, sequential static, MRI-based method16,28. Kinematics were assessed under 4 different conditions: 1) no load, no brace 2) 15% BW load, no brace 3) no load, brace 4) 15% BW, brace. We chose a load of 15% BW because we found previously that this load is achievable by study participants with knee OA21 and because a 30% load was difficult for some healthy participants29. We tested a no load condition in the study to determine whether kinematic changes created by the brace were consistent at different loads.
MRI scans for each subject were collected according to the previously described and validated protocol using a 3T MRI scanner (Intera, Phillips, Best, The Netherlands)16. Briefly, high resolution scans were acquired while the subject lay in a supine position with the knee in a relaxed position (Table 1). Next, six static, low-resolution scans were acquired at six different flexion angles between full extension and approximately 50° flexion (Table 1) for each of the four conditions described above. For these scans, the subject’s foot was positioned on a MRI-safe loading plate (Figure 2) with the knee flexed to the prescribed angle (approximately 0°, 10°, 20°, 30°, 40° and 50°, using a standard goniometer). A scan was acquired at the first flexion angle with no applied load (condition 1) and then with 15% BW load (condition 2). The process was repeated at each of the 5 other prescribed flexion angles. The subject then donned the patellar brace and the process of acquiring the low-resolution scans at no load (condition 3) and 15% BW load (condition 4) was repeated for the six knee flexion angles.
Table 1.
MRI parameters for high- and low-resolution images.
| Parameter | High-resolution | Low-Resolution |
|---|---|---|
| Coil | Knee | Body |
| In-plane resolution | 0.586 mm | 1.25 mm |
| Slice thickness | 2 mm | 2 mm |
| Slice separation | 2 mm | 7 mm |
| Matrix size | 512 × 512 | 256 × 256 |
| Repetition Time | 360 ms | 307 ms |
| Echo Time | 10.0 ms | 6.2 ms |
| Flip Angle | 90° | 90° |
| Field of view | 300 mm | 320 mm |
| Scan time | 9 min 10 s | 34 s |
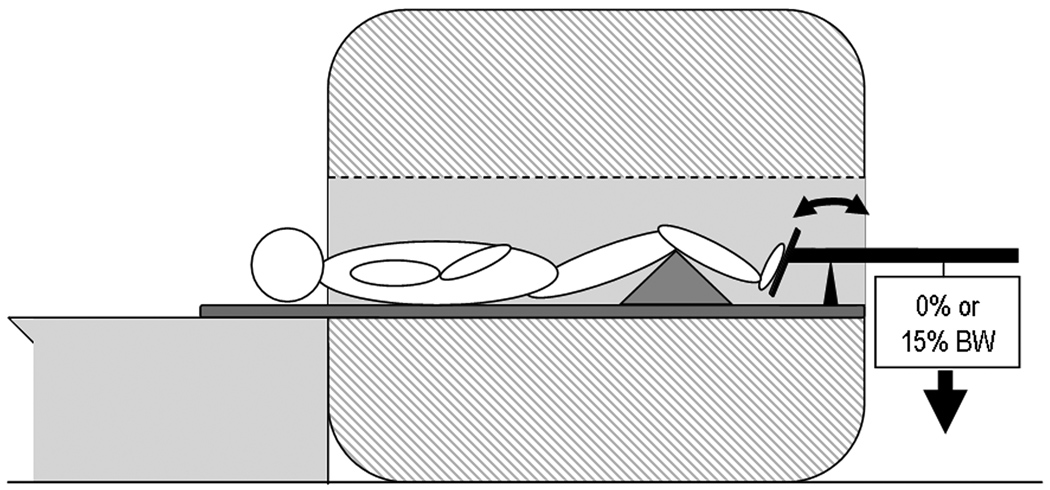
Figure 2.
Schematic of the patient lying supine in the MRI scanner. The patient’s foot is positioned on the MR-safe loading rig and the knee is supported by triangular foam padding. The weight is released against the patient’s foot thereby applying an axial load.
To calculate three-dimensional patellar kinematics, the images were processed using commercial (Analyze, Analyze Direct, Overland Park, KS, USA) and custom written software (Matlab, the Mathworks, Natick, MA, USA) according to the previously described method16. The patella, femur and tibia were segmented in a slice-by-slice manner from the high-resolution scan and each set of low-resolution scans. Bone models were created from the high-resolution scans and bone contours were created from the low-resolution scans. Orthogonal anatomical coordinate systems (flexion, long and anterior) were assigned to each bone in the model29. The origins of the patellar, femoral and tibial coordinate systems were the most posterior point on the axial midslice, the most distal point on the sagittal slice containing the most proximal point of the trochlear notch and the most proximal point of the medial tibial eminence, respectively. The positive directions for all coordinate systems were proximal, lateral and anterior. Next, each set of contours (six per condition) was registered to the bone models using an Iterative Closest Points algorithm30. A modified Joint Coordinate System, defined as the flexion axis of the femur, the long axis of the patella and a third, anteriorly directed axis which was orthogonal to the other two16,31, was used to determine the orientation of the patella with respect to the femur at each angle of knee flexion for each condition. Translations were defined using the position of the origin of the patellar coordinate system expressed in the femoral coordinate system at each knee flexion angle for each condition. Therefore the attitude and position of the patella with respect to the femur were described using the following three-dimensional patellar kinematic parameters: patellar flexion (rotation about the flexion axis of the femur), patellar spin (rotation about the third, anteriorly directed axis of the modified Joint Coordinate System), patellar tilt (rotation about the long axis of the patella), proximal-distal translation (position of the patellar origin along the long axis of the femur), medial-lateral translation (position of the patellar origin along the flexion axis of the femur) and anterior-posterior translation (position of the patellar origin along the anterior axis of the femur) (Figure 3). Similarly, tibiofemoral flexion was calculated. Error in the method is less than 1.02° for spin and tilt and less than 0.88 mm for translations, assessed using Roentgen stereophotogrammetric analysis (RSA) as a standard16. The intra-subject repeatability of the method is less than 1.04° for spin and tilt and less than 0.81 mm for translations, assessed as the mean standard deviation of 4 trials in 3 subjects28.
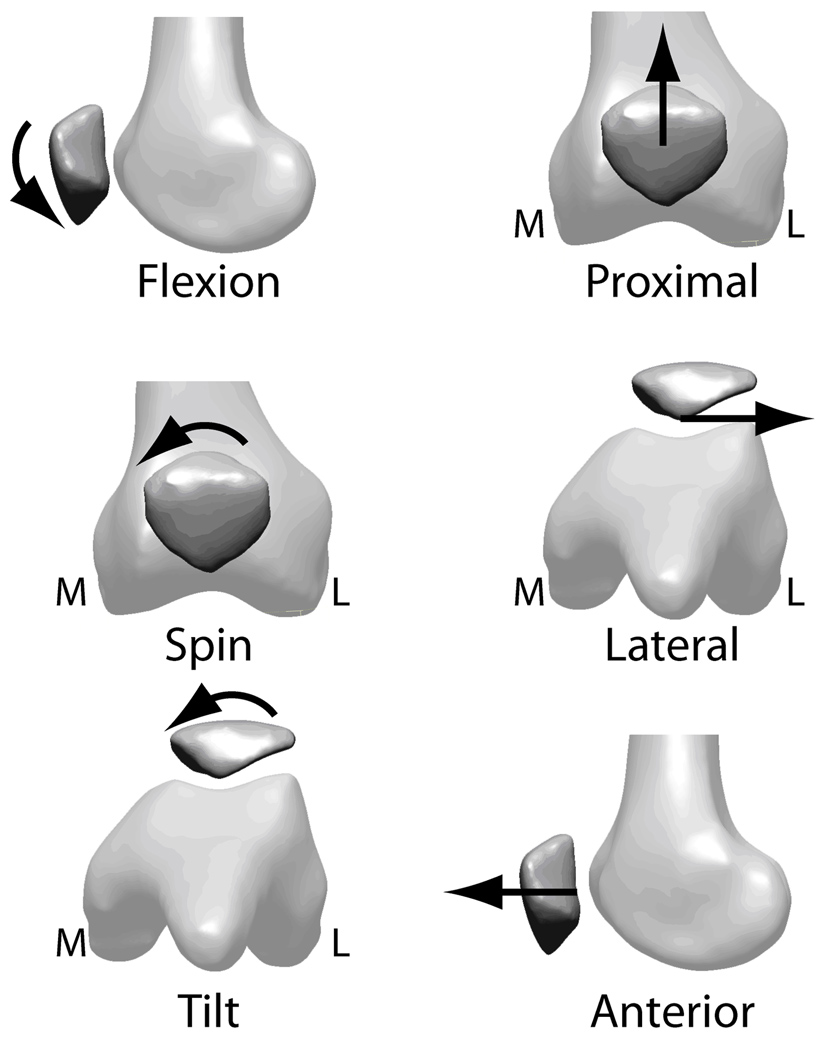
Figure 3.
Three-dimensional patellar kinematic parameters. Rotations: flexion/extension, internal/external spin, medial/lateral tilt. Translations: proximal/distal, lateral/medial, anterior/posterior. Arrowheads indicate the positive directions. M=medial, L=lateral.
Each kinematic parameter was plotted as a function of tibiofemoral knee flexion (calculated from the kinematic analysis) for each of the 4 conditions. The calculated knee flexion data were scaled so that the calculated and goniometer measures of knee flexion at the second loaded position of the no brace, no load condition (approximately 10°) were equal (i.e. the data were centered at 10° of knee flexion). This centering step was required because of difficulties in consistently identifying the origin of the tibial anatomical coordinate system on the MRI images, likely due to osteoarthritic changes.
Statistical Analysis
We tested the null hypothesis that there was no difference between the bracing conditions at no load and 15% BW load for each patellar kinematic parameter using hierarchical linear random-effects models and packaged software (Stata 10, StataCorp LP, College Station, TX, USA). The model is a weighted average of each subject’s kinematic data that takes into consideration any missing data and the variance from the mean. The models in this study took the following form:
where ‘y’ was the kinematic parameter, ‘knee_angle’ was the knee flexion angle and ‘condition’ was 1) no load, no brace 2) 15% BW load, no brace 3) no load, with brace, and 4) 15% BW, with brace. The random intercept term (β3) was always included in the model while the quadratic (β2) and random slope (β4) terms were included only when significant (p<0.05). Statistically significant differences were defined as p<0.05.
Results
Nineteen subjects (14 female, 5 male, 62.4 ± 9.9 years, 86.6 ± 18.9 kg) with lateral patellofemoral OA participated in this study. The twentieth subject was excluded from the analysis due to motion artifact in the high-resolution MRI scan which made patellar kinematic assessment impossible. Of the 19 remaining subjects, 6 had concomitant tibiofemoral OA and 6 had concomitant medial patellofemoral OA and tibiofemoral OA. The subjects had been wearing the brace for 16.0 ± 6.8 (mean ± standard deviation) days when the study was carried out. The subjects wore the brace for an average of 5.1 ± 1.9 hours per day.
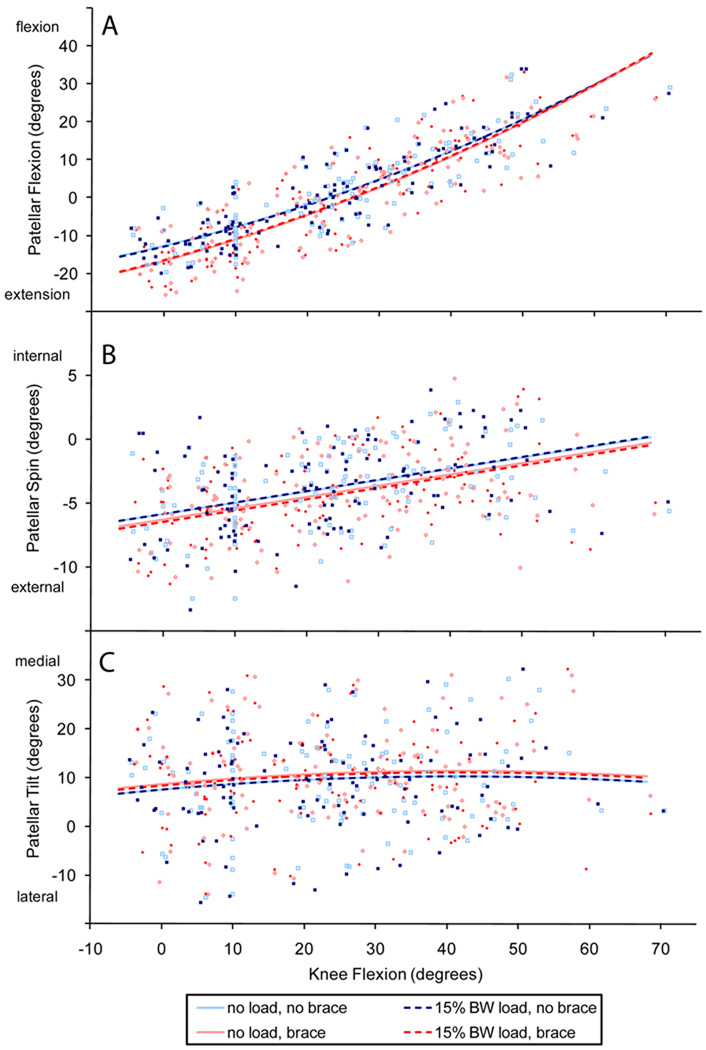
The brace caused the patellae to extend in early angles of knee flexion but the difference was not maintained in greater angles of knee flexion (Figure 4a, Table 2). The slope (β4) varied between conditions for flexion; the braced condition had greater slopes than the no brace condition at both load levels (both p<0.001) (Table 2). The brace caused the patellae to spin externally by 0.62° for the loaded condition (p=0.012) throughout the range of knee flexion studied (Figure 4b, Table 2). The trend was similar for the unloaded condition but the results were not statistically significant. The brace caused a medial tilt of the patella of 1.11° for the unloaded condition (p<0.001) and 0.85° for the loaded condition (p=0.004) throughout the range of knee flexion studied (Figure 4c, Table 2).
Figure 4.
Rotational results as a function of knee flexion for patellar a) flexion, b) spin and c) tilt. The lines indicate the results of the hierarchical linear random-effects model for each condition 1) no load, no brace, 2) 15% BW load, no brace, 3) no load, with brace, 4) 15% BW load, with brace. The raw data points are included and are colored according to condition. The data were scaled to 10° of knee flexion.
Table 2.
Coefficients (95% confidence interval) and p-values for the hierarchical random-effects models for rotations. The quadratic and random slope terms (β2 and β4, respectively) were included in the model when significant. NS = not significant.
| Coefficients | Flexion | Spin | Tilt |
|---|---|---|---|
|
β0 (y-intercept, °) |
−12.83 (−15.43, −10.23) p < 0.001 |
−5.83 (−7.03, −4.63) p < 0.001 |
7.60 (2.72, 12.48) p = 0.002 |
|
β1 (slope, ° / ° knee flexion) |
0.459 (0.385, 0.534) p < 0.001 |
0.089 (0.072, 0.105) p < 0.001 |
0.131 (0.052, 0.211) p = 0.001 |
|
β2 (quadratic, ° / ° knee flexion2) |
0.0041(0.0033, 0.0050) p < 0.001 |
NS | −0.0016 (−0.0025, −0.0006) p = 0.001 |
|
β3: (random intercept by condition, °) |
|||
| 0% load: no brace vs brace | −3.88 (−4.82, −2.94) p<0.001 |
−0.43 (−0.90, 0.04) p = 0.071 |
1.11 (0.54, 1.68) p < 0.001 |
| 15% load: no brace vs brace | −3.60 (−4.51, −2.68) p<0.001 |
−0.62 (−1.10, −0.15) p = 0.010 |
0.85 (0.27, 1.43) p = 0.004 |
| No brace: 0% load vs 15% load | −0.23 (−1.15, 0.69) p=0.626 |
0.02 (−0.46, 0.49) p = 0.944 |
−0.06 (−0.64, 0.51) p = 0.832 |
| Brace: 0% load vs 15% load | 0.05 (0.98, −0.88) p=0.913 |
−0.18 (−0.65, 0.29) p = 0.460 |
−0.32 (−0.89, 0.25) p = 0.274 |
|
β4: (random slope by condition, ° / ° knee flexion) |
|||
| 0% load: no brace vs brace | 0.062 (0.030, 0.094) p < 0.001 |
NS | NS |
| 15% load: no brace vs brace | 0.060 (0.028, 0.092) p<0.001 |
NS | NS |
| No brace: 0% load vs 15% load | 0.004 (−0.029, 0.036) p = 0.834 |
NS | NS |
| Brace: 0% load vs 15% load | 0.002 (−0.030, 0.033) p = 0.907 |
NS | NS |
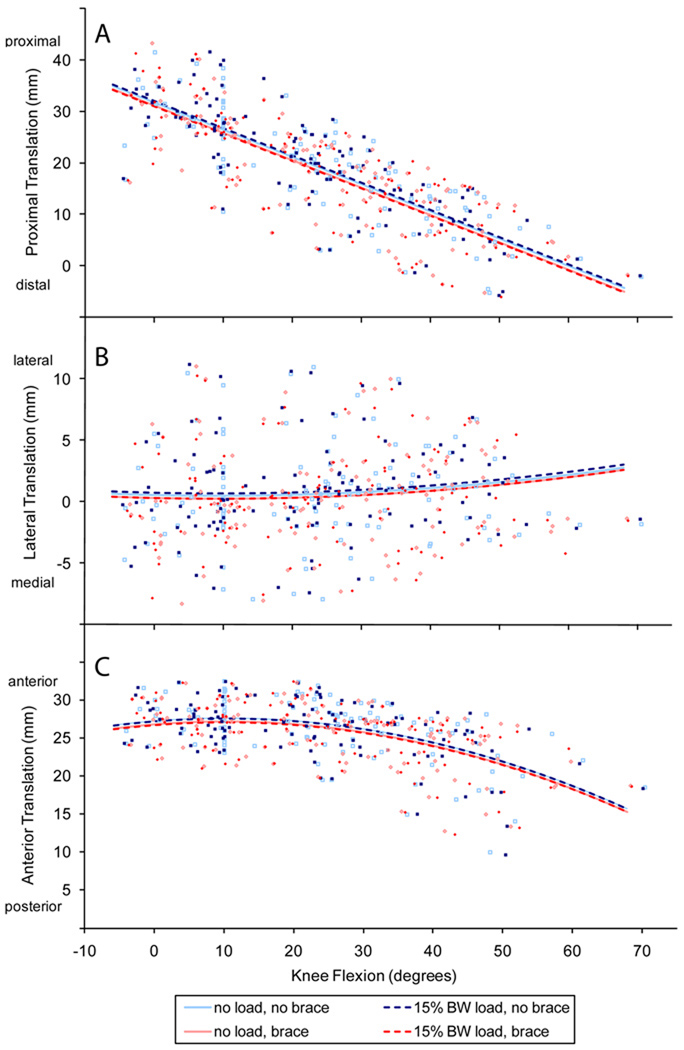
The brace caused the patellae to translate distally by 0.67 mm for the unloaded condition (p=0.001) and 1.09 mm for the loaded condition (p<0.001) throughout the range of knee flexion studied (Figure 5a, Table 3). Medial translations of 0.23 mm for the unloaded condition (p<0.001) and 0.46 mm for the loaded condition (p<0.001) were also found throughout the range of knee flexion studied (Figure 5b, Table 3). Finally, the brace caused a posterior translation of 0.51 mm for the unloaded condition (p<0.001) and 0.47 mm for the loaded condition (p<0.001) throughout the range of knee flexion studied (Figure 5c, Table 3).
Figure 5.
Translation results as a function of knee flexion for a) proximal, b) lateral and c) anterior translation. The lines indicate the results of the hierarchical linear random-effects model for each condition 1) no load, no brace, 2) 15% BW load, no brace, 3) no load, with brace, 4) 15% BW load, with brace. The raw data points are included and are colored according to condition. The data were scaled to 10° of knee flexion.
Table 3.
Coefficients (95% confidence interval) and p-values for the hierarchical random-effects models for translations. The quadratic term (β2) was included in the model when significant. The random slope term (β4) was not significant for any translation and therefore not included. NS = not significant.
| Coefficients | Proximal | Lateral | Anterior |
|---|---|---|---|
|
β0 (y-intercept, mm) |
31.77 (28.64, 34.90) p < 0.001 |
0.54 (−1.37, 2.45) p = 0.579 |
27.50 (26.21, 28.78) p < 0.001 |
|
β1 (slope, mm / ° knee flexion) |
−0.531 (−0.574, −0.489) p < 0.001 |
−0.013 (−0.047, 0.022) p = 0.468 |
0.072 (0.034, 0.11) p < 0.001 |
|
β2 (quadratic, mm / ° knee flexion2) |
NS | 0.0007 (0.0003, 0.0010) p < 0.001 |
−0.0036 (−0.0039, −0.0033) p < 0.001 |
|
β3: (random intercept by condition, mm) |
|||
| 0% load: no brace vs brace | −0.67 (−1.05, 0.29) p = 0.001 |
−0.23 (−0.44, −0.02) p = 0.031 |
−0.51 (−0.68, −0.33) p < 0.001 |
| 15% load: no brace vs brace | −1.09 (−1.48, −0.69) p < 0.001 |
−0.46 (−0.68, −0.25) p < 0.001 |
−0.47 (−0.64, −0.29) p<0.001 |
| No brace: 0% load vs 15% load | 0.31 (−0.07, 0.69) p = 0.114 |
0.22 (0.01, 0.44) p = 0.042 |
−0.06 (−0.23, 0.12) p = 0.525 |
| Brace: 0% load vs 15% load | −0.11 (−0.49, 0.28) p = 0.586 |
−0.01 (−0.22, 0.20) p = 0.937 |
−0.02 (−0.16, 0.19) p = 0.866 |
The quadratic coefficient (β2) was significant for patellar flexion, tilt, lateral translation and anterior translation and therefore included in those models. The random slope coefficient (β4) was significant for patellar flexion therefore included in that model.
Loading did not effect kinematics for any parameter except lateral translation in which the patella translated laterally by 0.22 mm (p=0.42) with applied load for the no brace condition (Figure 5b, Table 3).
Discussion
We assessed whether wearing a patellofemoral brace altered three-dimensional patellar kinematics in subjects with lateral radiographic patellofemoral OA. Donning the brace caused an average pattern of consistent external spin, medial tilt, proximal translation, medial translation and posterior translation of the patellae over the range of knee flexion studied, as described by the hierarchical random-effects models. It also caused the patellae to extend in early angles of knee flexion, but this difference was not maintained in greater flexion. These findings were consistent for the unloaded and loaded conditions, although the magnitudes of the differences varied slightly. The brace accomplished its mechanical aim of translating the patellae medially, however the magnitude of this translation was, on average, quite small (0.46 mm for 15% BW load condition). It is important to note that relatively large variability existed in patterns of kinematics between individuals, in particular for spin, tilt and lateral translation.
Since this is the first study to examine the effect of bracing in subjects with patellofemoral OA, there are no directly comparable results in the literature. However, our results are generally consistent with studies of patellofemoral bracing in subjects with patellofemoral pain and patellar subluxation and dislocation. In these studies, two-dimensional assessments in the axial plane were made using a measure of medial translation termed the bisect offset (the percentage of the width of the patella that is lateral to the deepest part of the trochlear groove32) and mediolateral patellar tilt angle (the angle between the line across the maximum width of the patella and the line joining the posterior femoral condyles18) or patellar tilt angle (the angle between the line parallel with the lateral patellar facet and a line joining the posterior femoral condyles33). In a study of patellofemoral pain, two different braces caused medial translations of 0.9 and 1.4 mm, respectively, (bisect offset decrease of 2.4% and 3.6%, standardized to mean patellar width of 38.8mm) when assessing kinematics with MRI at loaded sequential static postures25. In a second study of patellofemoral pain the brace caused a 1.6 mm medial translation (bisect offset 4%) when assessing kinematics in weightbearing flexion in an upright, open-bore MRI scanner26. In the study of patellar subluxation and dislocation the brace caused a medial translation of 0.4 mm (bisect offset approximately 1%) when assessing kinematics during continuous flexion with MRI (resisting the weight of the shank)33. Medial translations were smaller in the present study (0.23 to 0.46 mm) which may be due to differences in the OA joint anatomy, the age and strength of the patients and the definition of patellar translation. In these same studies the brace caused the patellae to tilt medially by approximately 1.5°25 and 3°26 (mediolateral patellar tilt angle) and 1.5°33 (the patellar tilt angle). The magnitude of medial tilt was smaller in the present study (between 0.79 and 1.17°). Some of the differences are likely the result of differences in the definition of tilt. In the present study, tilt was based on a coordinate system defined in three dimensions, in contrast with the two-dimensional assessments used in the other studies. Differences could also be due to variations in the design of the patellofemoral brace itself.
The patellofemoral brace also caused changes in patellar flexion, spin and distal translation, which is not its intended purpose. Our finding that bracing extended the patella in early knee flexion may be the result of the patellae translating proximally in early flexion, which may have shifted the proximal end of the patella above the brace’s patellar cutout and caused the patella to extend. Further, the brace caused the patellae to translate distally and spin externally, which may be due to the restriction of patellar motion that the cutout imposes. Finally, although small, the trend of posterior translation when the knee brace was worn was not surprising because, as others have speculated, the brace may cause the patella to be located more firmly in the trochlear groove, which is supported by the finding that bracing increases cartilage contact area25. Because this is the first three-dimensional assessment of bracing, comparison to the patellofemoral pain literature is not possible for these parameters.
Patellofemoral bracing produces similar kinematic results as patellar taping. A study of the effect of taping on patellar malalignment in patients with patellofemoral OA found that the tape caused the patellae to tilt medially by 3.57° but did not change the bisect offset8. It also found a decrease of 2.94% (or 1.1 mm, again using the comparative patellar width of 38.8 mm) in lateral displacement, which in this case was defined as the percentage of the patella lateral to the most anterior portion of the lateral condyle. The tape caused much greater tilt than observed in the present study and our measure of medial translation falls between the two measures used in the taping study. This highlights the difficulty in comparing results for medial translation between methods of assessment and this may be because they are sensitive to patellar type34 and coordinate system assignment35. Differences may be due to differing aims of the tape and the brace. The tape was positioned to translate and tilt the patella medially, tilt the patella superior and unload the infrapatellar fat pad. This aim is more complex than the medial translation applied by the brace. Differences may also be due to the cross-sectional design of the taping study; alignment was assessed immediately after tape application therefore the effect of loosening was not considered.
There were no differences in kinematics between the two load levels for the braced condition and only for lateral translation for the no brace condition, however this difference was very small. We have previously shown that there was no difference in kinematics between no load and 15% BW loads in normal subjects29; in the present study we have shown that this finding is also true in individuals with lateral patellofemoral OA. The small but statistically significant increase in lateral translation (0.22 mm) may be due to a laterally directed line of action of the active quadriceps muscles. It is possible that individuals with lateral patellofemoral OA display a more lateral patellar tracking than normal individuals and it appears that the quadriceps muscle contraction contributes to this pattern.
It is not clear whether the small changes in kinematics caused by the brace in this study reflect changes to the mechanical environment sufficient to produce clinical benefits. Patellar taping reduced pain in individuals with knee and patellofemoral OA5–8, however kinematics were not assessed in those studies. Therefore, it remains uncertain what magnitude of correction is required to reduce pain. The results from the parent cross-over study from which this subset was drawn found that the patellar brace did not reduce pain in this lateral patellofemoral OA population27. It is possible that the brace is not able to apply the same amount of mechanical correction as taping which may explain the difference in pain results. However, the subject groups differed between these two studies; the subjects taping study had bilateral patellofemoral OA. The kinematic differences for medial tilt and translation in the present study are smaller than those in the patellofemoral pain studies25,26,33, which is another indication that bracing affects the patellofemoral OA and pain populations differently. It is possible that the degenerative joint changes associated with OA impede the performance of the brace.
The differences observed when the brace was donned were, for the most part, smaller than the measurement error in the method and unlikely to be clinically meaningful. One possible reason that statistically significant differences were observed, even though they were smaller than the measurement error, is because the error is random rather than systematic16,28. The differences between the brace and no-brace conditions likely do not represent a clinically meaningful change in kinematics since no reduction in pain was observed in the parent study27. From previous two-dimensional bracing data in the patellofemoral pain population25,26 and taping data in the patellofemoral OA population8 we might expect clinically meaningful differences in medial translation to be at least 1 to 1.5 mm and in medial tilt to be at least 1.5 to 3.5°. There are no reference data available for the other four kinematics parameters.
This study was the first to assess the effect of a patellofemoral brace on three-dimensional patellar kinematics in subjects with patellofemoral OA. Strengths of this study include the carefully defined radiographic lateral patellofemoral OA population studied and the use of a validated method to assess three-dimensional patellar kinematics. A limitation of the study is that a sequential static method for assessing kinematics was used. Ideally we would assess patellar kinematics in normal activity, but to date no such method of assessment exists. Differences have been observed in two-dimensional patellar kinematics between unloaded, sequential static positions and continuous movement in resisted extension (open-chain)36, and between continuous resisted extension and continuous weightbearing flexion37. Further, the 15% BW load used in this study appears to be less than that experienced during dynamic activity; however, a force equilibrium analysis of the rig and lower limb has shown that the external extension moments (which vary with knee flexion) range from 25–200% of that experienced during the stance phase of gait (Appendix A). This load was chosen because all the participants with knee pain could tolerate and maintain throughout MRI scanning. It is likely that differences exist between sequential static and continuous methods and between resisted extension and simulated or actual weightbearing in three dimensions. Another limitation is that the patients wore the brace on average for 16 days prior to the kinematic assessment and as a result there may have been a learning effect, in particular for the no brace condition. Finally, we did not randomize the order in which each condition was studied because of the additional time that would have been required for the kinematic assessment. However, we chose to study the no brace condition prior to the brace condition because this order is aligned with the application of this treatment strategy.
We found that bracing produced small but statistically significant differences in three-dimensional patellar kinematics in subjects with radiographic lateral patellofemoral OA. The brace caused the patellae to spin externally, tilt medially and translate distally, medially and posteriorly through the entire range of knee flexion studied. The brace also extended the patellae in early angles of knee flexion. These trends were similar for both loading conditions. Although the brace achieved the mechanical aim of translating the patellae medially it does not appear that this small medial translation is able to adequately correct patellar kinematics in patients with radiographic lateral patellofemoral OA.
Acknowledgements
The authors would like to acknowledge Kelley Erb and Kevin Hallock for acquiring the MRI scans, James D. Johnston for writing a portion of the Matlab program and Cropper Medical Inc. for donating the braces.
Role of Funding Sources
This project was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS 2P60 AR047785-06) (DH), the National Institute of Health (AR47785) (DF), the Canadian Arthritis Network/The Arthritis Society of Canada Training Program (EM), Natural Sciences and Engineering Research Council of Canada (EM), Michael Smith Foundation for Health Research (EM) and Canadian Institutes of Health Research (DW). The study sponsors had no role in study design, collection, analysis and interpretation of data; in manuscript writing; and in the decision to submit the manuscript for publication.
Appendix A
Rig and External Joint Loads
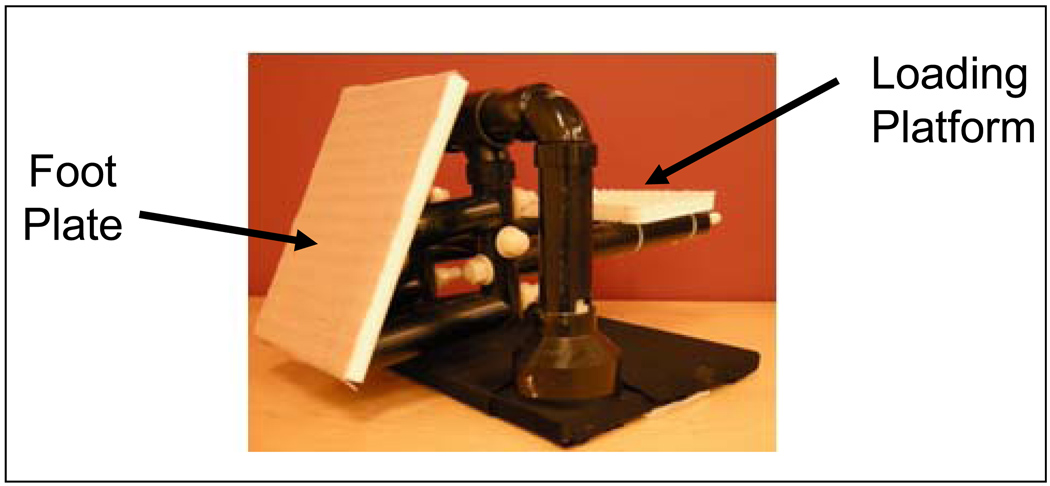
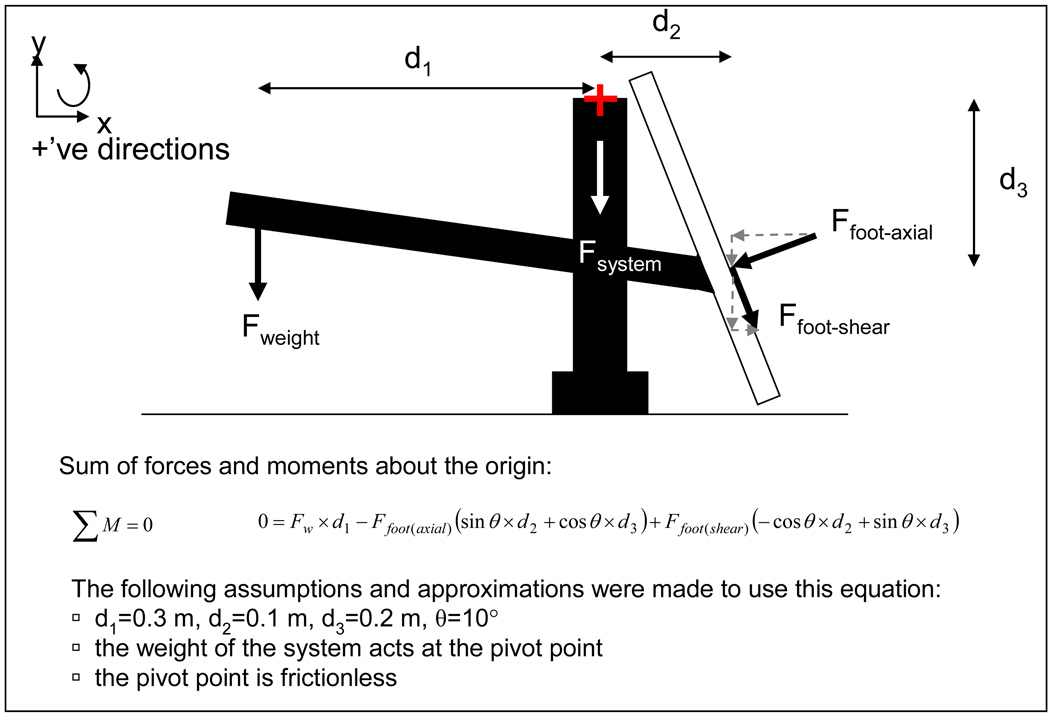
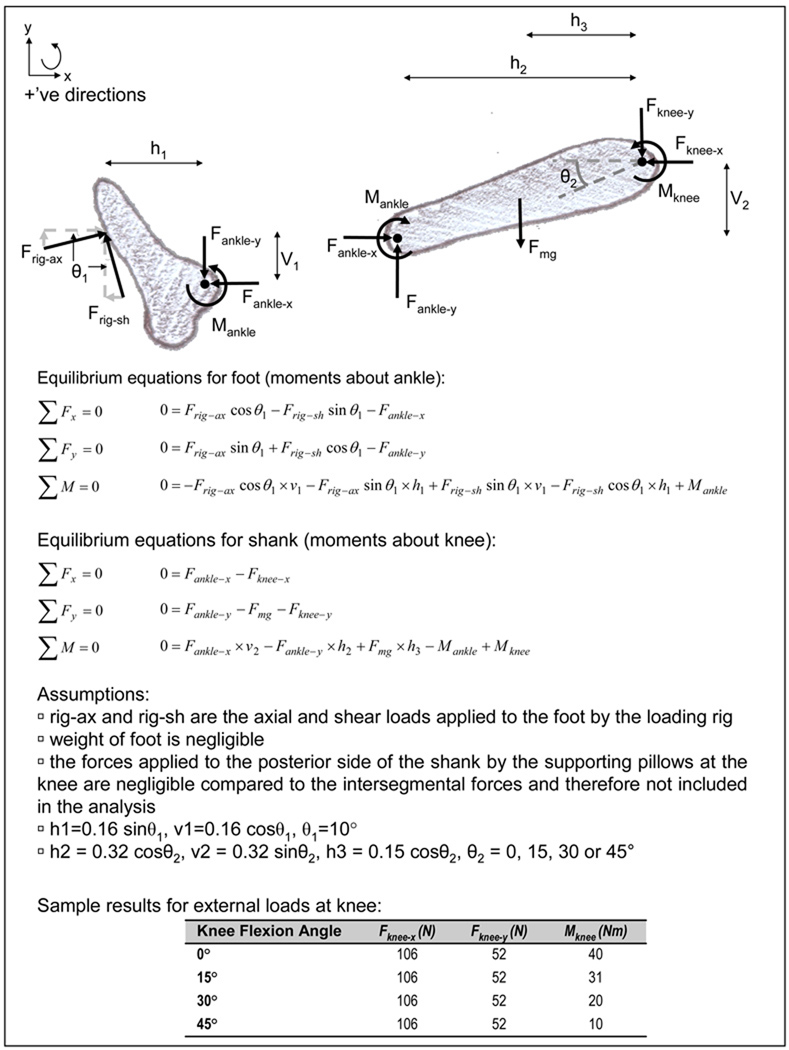
The loading rig consisted of a foot plate attached to a loading platform that hinges on an inversed U-shaped frame (Figure A1); therefore, the foot plate system was free to rotate about the crossbar of the frame. When in use the participant’s foot was placed on the loading plate, which was positioned at approximately 10° from vertical, and the prescribed load was placed on the loading platform. The load was then released and the participant was instructed to maintain his or her leg position so that the angle of the pedal did not change. The magnitude of the applied load required to create the prescribed axial load at the pedal (ie 15% BW load) was determined experimentally using a single axis load cell. The load was assumed to act at 15 cm from the bottom of the pedal, which is approximately at the centre of the foot. From this an estimate of shear load could be determined using a static equilibrium analysis of the rig (Figure A2). For example, for an individual who weighs 80 kg, the shear loads associated with an axial load of approximately 15% BW (118 N) was approximately 60 N and for 30% BW (236 N) was approximately 120 N.
Figure A1.
Photograph of loading rig.
Figure A2.
Free body diagram of loading rig (side view).
These loads applied by the rig can then be used to estimate the intersegmental forces and moments at the knee joint (external forces and moments). The segment lengths and the weight of the shank in the sample calculation were based on an example of a sagittal plane kinetic gait analysis found in a prominent textbook chapter1; this allows for direct comparison of intersegmental forces and moments at the knee. In the section on intersegmental loads below, a schematic of the system, free-body diagrams of the foot and the shank and equilibrium equations are shown (Figure A3). These equations can be used to estimate intersegmental forces and moments at the different load levels for different knee flexion angles (Figure A3). The external moments at the knee ranged from 10 Nm at 45° of knee flexion to 40 Nm at full extension. In the textbook example, the external moment at the knee was 43 Nm when ground reaction forces of 700 N in the vertical direction and 150 N in the horizontal direction were applied (textbook Figure 3–6 and Table 3–1)1. Therefore, the external moments at the knee during the MRI scan are similar to those experienced during gait; however, it must be noted that this is a measure of resultant external moment only and does not tell us about internal contact or muscle loads which can only be estimated using assumptions, simplifications and reduction or optimization algorithms.
Figure A3.
Sagittal plane intersegmental force analysis.
1 Andriacchi TP, Johnson TS, Hurwitz DE, Natarajan RN. Musculoskeletal Dynamics, Locomotion, and Clinical Applications. In: Basic Orthopaedic Biomechanics and Mechano-biology, Mow VC, Huiskes R, 3rd Edition, Philadelphia, Lippincott Williams & Wilkins 2005.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributions
The authors contributed to this manuscript in the following ways: Conception and design (EJM, DJH, WFH, DTF, DRW); Collection and assembly of data (PM, KAH, DJH, WFH); Analysis of data (EJM, DJH, WFH); Interpretation of data (EJM, DJH, WFH, DTF, DRW); Drafting the article (EJM, DRW); Revision of the article for important intellectual content (DJH, WFH, PM, KAH, DTF); Final approval of the submitted version (EJM, DJH, WFH, PM, KAH, DTF, DRW). EJM and DRW take responsibility for the integrity of the manuscript as a whole (dawilson@interchange.ubc.ca).
Competing Interests Statement
The authors have no conflicts to declare.
Contributor Information
Emily J. McWalter, PhD Candidate, Department of Mechanical Engineering, University of British Columbia 828 West 10th Avenue, Room 590, Vancouver, BC, Canada, V5Z 1L8, Phone: 604 875 4111 x 66314; Fax: 604 875 4851 emilymc@interchange.ubc.ca.
David J. Hunter, Chief of Research, New England Baptist Hospital.
William F. Harvey, Division of Research, New England Baptist Hospital.
Paula McCree, Director of Clinical Research, New England Baptist Hospital.
Kelly A. Hirko, Research Assistant, Boston University
David T. Felson, Professor of Medicine and Epidemiology and Chief, Clinical Epidemiology Research and Training Unit, Boston University School of Medicine.
David R. Wilson, Associate Professor, Department of Orthopaedics, University of British Columbia and Vancouver Coastal Health Research Institute.
References
- 1.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 2.McAlindon T, Zhang Y, Hannan M, Naimark A, Weissman B, Castelli W, et al. Are risk factors for patellofemoral and tibiofemoral knee osteoarthritis different? J Rheumatol. 1996;23:332–337. [PubMed] [Google Scholar]
- 3.Hunter DJ, Zhang YQ, Niu JB, Felson DT, Kwoh K, Newman A, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study. Osteoarthritis and Cartilage. 2007;15:1120–1127. doi: 10.1016/j.joca.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Felson DT, et al. The association between patellar alignment and patellofemoral joint osteoarthritis features--an MRI study. Rheumatology (Oxford) 2007;46:1303–1308. doi: 10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- 5.Hinman RS, Bennell KL, Crossley KM, McConnell J. Immediate effects of adhesive tape on pain and disability in individuals with knee osteoarthritis. Rheumatology (Oxford) 2003;42:865–869. doi: 10.1093/rheumatology/keg233. [DOI] [PubMed] [Google Scholar]
- 6.Hinman RS, Crossley KM, McConnell J, Bennell KL. Efficacy of knee tape in the management of osteoarthritis of the knee: blinded randomised controlled trial. BMJ. 2003;327:135. doi: 10.1136/bmj.327.7407.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: a new treatment for osteoarthritis of the knee joint? BMJ. 1994;308:753–755. doi: 10.1136/bmj.308.6931.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crossley KM, Marino GP, Macilquham MD, Schache AG, Hinman RS. Can patellar tape reduce the patellar malalignment and pain associated with patellofemoral osteoarthritis? Arthritis Rheum. 2009;61:1719–1725. doi: 10.1002/art.24872. [DOI] [PubMed] [Google Scholar]
- 9.Pinar H, Akseki D, Genc I, Karaoglan O. Kinematic and dynamic axial computerized tomography of the normal patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 1994;2:27–30. doi: 10.1007/BF01552650. [DOI] [PubMed] [Google Scholar]
- 10.Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography. A preliminary study. Clin Orthop Relat Res. 1986:286–293. [PubMed] [Google Scholar]
- 11.Bey MJ, Kline SK, Tashman S, Zauel R. Accuracy of biplane x-ray imaging combined with model-based tracking for measuring in-vivo patellofemoral joint motion. J Orthop Surg Res. 2008;3:38. doi: 10.1186/1749-799X-3-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fregly BJ, Rahman HA, Banks SA. Theoretical accuracy of model-based shape matching for measuring natural knee kinematics with single-plane fluoroscopy. J Biomech Eng. 2005;127:692–699. doi: 10.1115/1.1933949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stein LA, Endicott AN, Sampalis JS, Kaplow MA, Patel MD, Mitchell NS. Motion of the patella during walking: a video digital-fluoroscopic study in healthy volunteers. AJR Am J Roentgenol. 1993;161:617–620. doi: 10.2214/ajr.161.3.8352119. [DOI] [PubMed] [Google Scholar]
- 14.Barrance PJ, Williams GN, Novotny JE, Buchanan TS. A method for measurement of joint kinematics in vivo by registration of 3-D geometric models with cine phase contrast magnetic resonance imaging data. J Biomech Eng. 2005;127:829–837. doi: 10.1115/1.1992524. [DOI] [PubMed] [Google Scholar]
- 15.Draper CE, Santos JM, Kourtis LC, Besier TF, Fredericson M, Beaupre GS, et al. Feasibility of using real-time MRI to measure joint kinematics in 1.5T and open-bore 0.5T systems. J Magn Reson Imaging. 2008;28:158–166. doi: 10.1002/jmri.21413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fellows RA, Hill NA, Gill HS, MacIntyre NJ, Harrison MM, Ellis RE, et al. Magnetic resonance imaging for in vivo assessment of three-dimensional patellar tracking. J Biomech. 2005;38:1643–1652. doi: 10.1016/j.jbiomech.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Patel VV, Hall K, Ries M, Lindsey C, Ozhinsky E, Lu Y, et al. Magnetic resonance imaging of patellofemoral kinematics with weight-bearing. J Bone Joint Surg Am. 2003;85-A:2419–2424. doi: 10.2106/00004623-200312000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Powers CM, Shellock FG, Pfaff M. Quantification of patellar tracking using kinematic MRI. J Magn Reson Imaging. 1998;8:724–732. doi: 10.1002/jmri.1880080332. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan FT, Zajac FE, Drace JE. In vivo tracking of the human patella using cine phase contrast magnetic resonance imaging. J Biomech Eng. 1999;121:650–656. doi: 10.1115/1.2800868. [DOI] [PubMed] [Google Scholar]
- 20.von Eisenhart-Rothe R, Siebert M, Bringmann C, Vogl T, Englmeier KH, Graichen H. A new in vivo technique for determination of 3D kinematics and contact areas of the patello-femoral and tibio-femoral joint. J Biomech. 2004;37:927–934. doi: 10.1016/j.jbiomech.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 21.McWalter EJ, Cibere J, MacIntyre NJ, Nicolaou S, Schulzer M, Wilson DR. Relationship between varus-valgus alignment and patellar kinematics in individuals with knee osteoarthritis. J Bone Joint Surg Am. 2007;89:2723–2731. doi: 10.2106/JBJS.F.01016. [DOI] [PubMed] [Google Scholar]
- 22.Shin CS, Carpenter RD, Majumdar S, Ma CB. Three-dimensional in vivo patellofemoral kinematics and contact area of anterior cruciate ligament-deficient and -reconstructed subjects using magnetic resonance imaging. Arthroscopy. 2009;25:1214–1223. doi: 10.1016/j.arthro.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 23.MacIntyre NJ, Hill NA, Fellows RA, Ellis RE, Wilson DR. Patellofemoral joint kinematics in individuals with and without patellofemoral pain syndrome. J Bone Joint Surg Am. 2006;88:2596–2605. doi: 10.2106/JBJS.E.00674. [DOI] [PubMed] [Google Scholar]
- 24.Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res. 2009;27:561–570. doi: 10.1002/jor.20783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Powers CM, Ward SR, Chan LD, Chen YJ, Terk MR. The effect of bracing on patella alignment and patellofemoral joint contact area. Med Sci Sports Exerc. 2004;36:1226–1232. doi: 10.1249/01.mss.0000132376.50984.27. [DOI] [PubMed] [Google Scholar]
- 26.Draper CE, Besier TF, Santos JM, Jennings F, Fredericson M, Gold GE, et al. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J Orthop Res. 2009;27:571–577. doi: 10.1002/jor.20790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hunter DJ, Harvey W, Gross KD, Felson D, McCree P, Li L, et al. A randomized trial of patellofemoral bracing for treatment of patellofemoral osteoarthritis. Osteoarthritis and Cartilage. 2011 doi: 10.1016/j.joca.2010.12.010. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fellows RA, Hill NA, Macintyre NJ, Harrison MM, Ellis RE, Wilson DR. Repeatability of a novel technique for in vivo measurement of three-dimensional patellar tracking using magnetic resonance imaging. J Magn Reson Imaging. 2005;22:145–153. doi: 10.1002/jmri.20360. [DOI] [PubMed] [Google Scholar]
- 29.McWalter EJ, Hunter DJ, Wilson DR. The effect of load magnitude on three-dimensional patellar kinematics in vivo. J Biomech. 2010;43:1890–1897. doi: 10.1016/j.jbiomech.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 30.Besl PJ, McKay ND. A method for registration of 3-D shapes. IEEE Transaction on Pattern Analysis and Machine Intelligence. 1992;14:239–255. [Google Scholar]
- 31.Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115:344–349. doi: 10.1115/1.2895496. [DOI] [PubMed] [Google Scholar]
- 32.Stanford W, Phelan J, Kathol MH, Rooholamini SA, el-Khoury GY, Palutsis GR, et al. Patellofemoral joint motion: evaluation by ultrafast computed tomography. Skeletal Radiol. 1988;17:487–492. doi: 10.1007/BF00364042. [DOI] [PubMed] [Google Scholar]
- 33.Muhle C, Brinkmann G, Skaf A, Heller M, Resnick D. Effect of a patellar realignment brace on patients with patellar subluxation and dislocation. Evaluation with kinematic magnetic resonance imaging. Am J Sports Med. 1999;27:350–353. doi: 10.1177/03635465990270031401. [DOI] [PubMed] [Google Scholar]
- 34.Wiberg G. Roentgenographic and anatomic studies on the femoropatellar joint, with special reference to chondromalacia patellae. Acta Orthop Scand. 1941;12:319–340. [Google Scholar]
- 35.Bull AM, Katchburian MV, Shih YF, Amis AA. Standardisation of the description of patellofemoral motion and comparison between different techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10:184–193. doi: 10.1007/s00167-001-0276-5. [DOI] [PubMed] [Google Scholar]
- 36.Brossmann J, Muhle C, Schroder C, Melchert UH, Bull CC, Spielmann RP, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology. 1993;187:205–212. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 37.Draper CE, Besier TF, Fredericson M, Santos JM, Beaupre GS, Delp SL, et al. Differences in patellofemoral kinematics between weight-bearing and non-weightbearing conditions in patients with patellofemoral pain. J Orthop Res. 2010 doi: 10.1002/jor.21253. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]