Abstract
Stimulant drug use is associated with numerous health problems among men who have sex with men (MSM). This paper describes how stimulant drug use changes over a four and one-half year period from 2003 until 2008. Participants were 2,389 men (17,222 person-visits) from The Multicenter AIDS Cohort Study (MACS)—an ongoing, prospective study of HIV infection among MSM. Group-based trajectory analyses of data from these men over the study period yielded a four groups solution: consistent users (9.8%), men whose use increased (5.4%), men whose use declined (6.9%), and abstinent or rarely-using men (77.9%). There were significant differences between groups in terms of demographic, behavioral risk and HIV serostatus. Men who increased or decreased stimulant drug use over time reported congruent changes in sexual risk taking. The fact that sexual risk levels parallel stimulant drug use over time suggests that finding ways to lower rates of stimulant drug use among MSM could be a tool in HIV prevention.
Keywords: Drug use, Gay men’s health, HIV risk behavior, MSM, Stimulant use
Introduction
Stimulant drug use, including methamphetamine use, is associated with numerous health problems among men who have sex with men (MSM). Although research on the health outcomes of stimulant drug use among MSM has primarily focused on risks for HIV seroconversion [1–5], additional research has identified associations between stimulant drug use and infection with other sexually-transmitted infections [6–9], mood disorders [10, 11], violence victimization [12], tooth loss and other dental problems [13, 14], as well as poor social functioning and downward social mobility [10, 11]. The general recognition of the many serious health problems associated with the varying forms of stimulant drug use has been the source of ongoing calls for interventions to lower this form of drug use among MSM and other populations [15].
Although a cluster of health problems associated with stimulant drug use has been characterized, descriptive studies of how patterns of stimulant drug use may change over time among MSM have only rarely been attempted (see, for example, Colfax et al. [16]). This is somewhat surprising in that “natural history” descriptions of patterns of use of stimulant drug use over time could provide valuable guidance in efforts to prevent the harmful effects of drug use among MSM. For example, identification of the characteristics of men most vulnerable to heavy use would help in the construction of targeted community-based prevention campaigns. More rigorous description of the health problems associated with heavy stimulant drug use might help motivate men to carefully monitor their stimulant drug use, or even decide to forego drug use initiation. Furthermore, identification of whether men’s HIV risk profile lessens after discontinuance of use might motivate frequent users to end or reduce substance use. Conversely, the study of “resiliency” factors that prevent problematic use of drugs or predict recovery from abuse might provide insights important to improving the efficacy of interventions designed to lower drug-related health and social problems among MSM.
This paper will describe patterns of stimulant drug use among men participating in the Multicenter AIDS Cohort Study (MACS) over a four and a half year period of time from October 2003 through March 2008. The MACS is a large multi-center observational study of HIV risk among MSM that also administered a detailed battery of drug use questions. Notably, the study period for this analysis was one in which numerous alarms were raised about rising rates of stimulant drug use among MSM as well as harm associated with stimulant drug use [17–19]. We use data from the MACS to characterize patterns of stimulant drug use from 2003 to 2008, to identify the men who are most likely to initiate stimulant drug use over time as well as those who reduce or stop use and to determine whether changing patterns of use over time are associated with differential HIV risk outcomes.
Methods
MACS Background
The MACS is an ongoing, prospective study of the natural history of HIV infection among MSM in the United States. A total of 6,973 men were enrolled during the history of the project: 4,954 men in 1984–1985, 668 in 1987–1991, and 1,351 in 2001–2003 at four centers located in Baltimore, MD/Washington DC; Chicago, IL; Los Angeles, CA; and Pittsburgh, PA. The study design has been described previously [20–22] and only methods relevant to the present study are described here. The study questionnaires are available at http://www.statepi.jhsph.edu/macs/forms.html. The MACS study protocols were approved by institutional review boards of each of the participating centers, and their community affiliates, and informed consent was obtained from all participants. Data from the MACS cohort have been the source of numerous papers on the interconnections between substance use and high risk sexual behavior (see, for example, Ostrow et al. 2000 [23]) and the relationship between non-intravenous substance use and HIV seroconversion among MSM [5, 24].
Participants returned every 6 months for a detailed interview, physical examination, and collection of blood for laboratory testing and storage. The interview included questions about medical conditions, medical treatments, sexual behavior, and recreational drugs (e.g., marijuana, poppers, cocaine, crack, heroin, methamphetamine, ecstasy) as well as alcohol consumption. All questions concerning sexual and drug use behaviors were assessed using audio computer-assisted self interviewing (ACASI), a methodology shown to yield more accurate assessments of “sensitive behaviors” than interviewer-administered questionnaires [25].
This analysis follows stimulant drug use from semiannual visits 40 (data collection starting in October 1, 2003) through visit 48 (data collection ending in March 31, 2008) of the MACS. We selected visit 40 as the baseline for this analysis since the sample size reached its maximum size at visit 40 after the most recent expansion of cohort between 2001 and 2003. To be included in the analysis, participants must have had at least one male sex partner during the study period and data about stimulant drug use for at least two visits during the study period. Of 2,750 men who participated in the MACS between visits 40 and 48, 2,389 responded to questions regarding stimulant drug use at least two times during study period and had at least one male sex partner. The study sample included 2,389 male participants contributing 17,222 person-visits. The median number of observations in our study period per participant was 8 (range 2–9).
Measurement of Key Variables
Stimulant Drug Use
Study participants reported considerable overlap in use of varying kinds of stimulant drugs over the study period. This analysis will describe patterns of use of stimulant drugs as a whole, since attribution of health or behavioral outcomes to any one drug category among a group of men who commonly use multiple forms of stimulant drugs would be beyond the scope of the available data. Participants were considered to be users of stimulant drugs if they reported the use of any of the following drugs in the previous 6 months during the 4½ year follow-up period: (1) crack cocaine, (2) other forms of cocaine, (3) methamphetamines (or speed, meth or ice), and (4) other recreational drugs such as “ecstasy” or MDMA (3,4-methylenedioxy-Af-methylamphetamine).
Sociodemographic Characteristics
Baseline data at visit 40 were used to define dichotomous analysis variables for race (white/non white) and education (college graduate/less than college graduate). Self-reported annual gross income in the past year was dichotomized as more than $50,000 or not, and a summary variable was created to indicate if a participant had earned more than $50,000 at any visit during the study period.
Sexual Risk-Taking
At each visit, the number of anal sexual partners with whom the participants reported always using a condom was subtracted from the total number of partners for each respective activity (receptive or insertive) to obtain the number of partners with whom the participant engaged in unprotected anal sex. Sexual risk-taking was measured by counting the number of unprotected anal intercourse insertive partners and the number of unprotected anal intercourse receptive partners over the past 6 months.
Alcohol Use
Alcohol use was measured using questions about frequency of drinking and average number of drinks the participant consumed during drinking occasions since the last visit. Binge drinking was defined as 5 or more drinks per occasion occurring at least monthly.
Tobacco Use
Participants were considered to be current smokers if they responded yes to a question asking about any cigarette consumption in the past 6 months.
HIV Serostatus
At each visit, HIV serostatus was determined using an enzyme-linked immunosorbent assay with confirmatory western blot tests on all participants not previously documented by the study to be HIV infected. By visit 48, 1,207 men (50.5%) remained HIV-negative and 1,182 (49.5%) were HIV seropositive. A total of 39 men seroconverted between visits 40 and 48; these men were included among the HIV seropositives for this analysis.
Approach to Data Analysis
Three data analytic procedures were used to accomplish the study goals: (A) group-based trajectory analyses; (B) analysis of variance (ANOVA) and χ2 tests to examine trajectory group differences in demographic and substantive variables; and (C) individual trajectory modeling to examine change in sexual risk-taking over time within and between trajectory groups. First, a semi-parametric, group-based approach was used to identify clusters of individual growth trajectories of stimulant drug use [26,27]. Trajectories were modeled as a function of visit by using the SAS PROC TRAJ software (SAS version 9.2, Cary, NC), available online at http://www.andrew.cmu.edu/user/bjones/index. Individuals with missing observations were included because PROC TRAJ uses all values available from each case to estimate an individual’s trajectory. A logistic model was used because stimulant use is a binary variable. Selection of optimal number of trajectory groups was guided by Nagin’s criteria: (1) substantive theory, (2) Bayesian Information Criteria (BIC), (3) Average Posterior Probabilities (AvePP), and (4) group size. After the optimum number of trajectory groups was selected, we determined the trend of each group (e.g., linear, quadratic, cubic). We tested models from two to five group solutions, in which the BIC continued to improve from the two group through to the four group solution. However, the five group solution did not converge. We therefore used the four group solution for this analysis.
Chi-square tests and ANOVA were used to test group differences in demographic, behavioral, and psychosocial characteristics (see Table 2). To summarize results of the continuous variables across visits, mean scores of these measures of interest (e.g., number of drinks, number of male intercourse sexual partners) across visits were calculated. For dichotomous variables (e.g., current smoker, binge drinking), summary variables were created to denote whether participants ever reported such behaviors at any visit during the study period. Last, we used growth curve modeling (PROC MIXED, SAS version 9.2) to predict the longitudinal change in number of unprotected insertive anal sex partners (NUAII) and number of unprotected receptive anal sex partners (NUARI) over 4½ years using stimulant drug use trajectories as a predictor [28, 29].
Table 2.
Demographic characteristics at visit 40 (n = 2,270)
| No use N= 1604 | Increasing N = 108 | Decreasing N= 134 | Consistently high N = 189 | F | χ2 | P | |
|---|---|---|---|---|---|---|---|
| Age, mean (SD) | 48.7 (10.0) | 41.9 (10.5)a*** | 42.3 (9.1)b*** | 42.2 (9.5)c*** | 48.53 | - | <0.001 |
| Agea, n (%) | - | 131.75 | <0.001 | ||||
| 18–29 | 76 (4.7) | 16 (14.8) | 15 (11.2) | 19 (10.0) | |||
| 30–39 | 209 (13.0) | 20 (18.5) | 31 (23.1) | 57 (30.2) | |||
| 40–49 | 578 (36.0) | 45 (41.7) | 64 (47.8) | 70 (37.0) | |||
| 50–59 | 536 (33.4) | 25 (23.2) | 21 (15.7) | 40 (21.2) | |||
| 60–79 | 205 (12.8) | 2 (1.9) | 3 (2.2) | 3 (1.6) | |||
| White race (%) | 78.4 | 56.5 | 58.2 | 59.3 | - | 72.54 | <0.001 |
| Baseline college graduate or more (%) | 60.4 | 38.0 | 44.0 | 39.7 | - | 54.81 | <0.001 |
| >50K annual income (%) | 37.3 | 16.2 | 21.4 | 27.4 | - | 35.05 | <0.001 |
| HIV negative (%) | 55.7 | 38.0 | 33.6 | 39.7 | - | 46.85 | <0.001 |
| Binge drinking (%) | 7.2 | 7.6 | 17.6 | 14.5 | - | 25.75 | <0.001 |
| No. drinks per week, mean (SD) | 4.81 (8.18) | 4.88 (7.61) | 8.20 (11.57)b***, d* | 7.90 (10.94)c***, e* | 12.09 | - | <0.001 |
| Current smoker (%) | 23.4 | 47.6 | 56.8 | 50.5 | - | 131.67 | <0.001 |
| NUAII partner, mean (SD), truncate at 10 | 0.96 (6.62) | 1.55 (6.78) | 1.53 (4.31) | 3.30 (9.69)c*** | 6.40 | - | <0.001 |
| NUARI partner, mean (SD), truncate at 10 | 0.56 (2.74) | 1.06 (5.02) | 2.27 (10.38)b*** | 2.53 (7.29)c*** | 15.50 | - | <0.001 |
For continuous variables, besides Analysis of Variance (ANOVA), post-hoc pairwise comparisons were performed using Sheffé adjustment for P values 10.8% data missing
Comparison between the increasing and no use groups
Comparison between the decreasing and no use groups
Comparison between the consistently high and no use groups
Comparison between the decreasing and increasing groups
Comparison between the consistently high and increasing groups
P< 0.05
P < 0.01
P < 0.001
Results
At visit 40, the men included in this analysis of the MACS cohort had a mean age of 47, with 6% of the men 29 years of age or younger, 17% between the ages of 30 and 39, 38% between the ages of 40–49, 29% between the ages of 50 and 59 and 10% age 60 or older. The men were predominately Caucasian (64%), with the remainder identifying as an ethnic/racial minority (25.5% African American, 9.8% Latino/Hispanic and 1.4% mixed or other). Nearly half (48%) of the men were HIV seropositive by visit 40. The sample reported predominantly middle range incomes, with 46% reporting annual incomes of less than $30,000,20% reporting incomes between $30,000 and $50,000, with the remaining 34% reporting incomes greater than $50,000. The sample as a whole was highly educated, with only 6% reporting less than a high school education, 14% reporting a high school education, 27% reporting at least 1 year of college but no degree, and 52% reporting a college degree or post-graduate education.
To What Extent Does Use of Varying Kinds of Stimulant Drugs Overlap Over Time Among MSM?
Table 1 illustrates the substantial overlap of various stimulant drugs reported by MACS participants between visits 40 and 48. For example, among the methamphetamine users, nearly half (45%) had used crack or powder cocaine and 40% reported using MDA/MDMA. Only 27% of the methamphetamine users were exclusive users of only that drug, while 73% of methamphetamine-using men used two or more stimulant drugs. Use of multiple kinds of stimulant drugs was even greater among men who reported any crack, cocaine or MDA use.
Table 1.
Participants who reported using specific stimulant drugs at any visit also reported using other stimulant drugs during the study period (visit 40–48, n = 2,389)
| Any crack (n = 373) | Any cocaine (n = 352) | Any meth (n = 310) | Any MDA (n = 215) | |
|---|---|---|---|---|
| Any crack (n = 373) | X | n = 219 (62.2%) | n = 139 (44.8%) | n = 90 (41.9%) |
| Any cocaine (n = 352) | X | n = 141 (45.5%) | n = 107 (49.8%) | |
| Any meth (n = 310) | X | n = 129 (60.0%) | ||
| Any MDA (n = 215) | X | |||
| Use of only one stimulant drug | n = 93 (24.9%) | n = 70 (19.9%) | n = 82 (26.5%) | n = 37 (17.2%) |
| Use of 2+ stimulant drugs | n = 280 (75.1%) | n = 282 (80.1%) | n = 228 (73.5%) | n = 178 (82.8%) |
How Do Patterns of Stimulant Drug Use Change Over Time Among MSM?
We next turned to the question of how patterns of use changed over the 4-year period. The group-based analysis yielded a solution that identified four groups (see Fig. 1). These groups include a group of men who were consistent users of stimulant drugs over time (9.8% of the cohort, n = 234), a group of men whose use increase over time (5.4% of the cohort, n = 129), a group of men whose use declined over time (6.9% of the cohort, n = 165) and a group of abstinent or rarely-using men (77.9% of the cohort, hereafter described as the “no use” pattern, n = 1861). The AvePP for the four-group model ranged from 0.79 to 0.99. These scores indicate that 79–99% of individuals were correctly assigned to different groups.
Fig. 1.
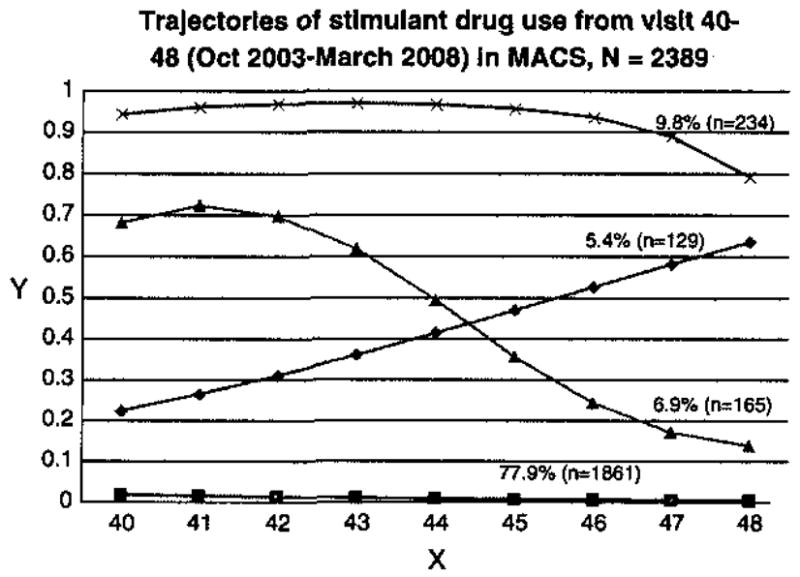
Trajectories of stimulant drug use MSM from 2003 to 2008 in the Multicenter AIDS Cohort Study. MACS Multicenter AIDS Cohort Study, Y probability of reporting stimulant drug use in the past 6 months at a particular visit, X visit
Are There Demographic or Behavioral Differences on Intake Between Men Who Subsequently Report Varying Drug Use Patterns Over Time?
Describing the characteristics of men who subsequently reported varying patterns of stimulant drug use is useful because it identifies those men who are most vulnerable to frequent use of stimulant drugs. The characteristics of men who reported varying patterns of stimulant drug use over an ensuing 4 year period are give in Table 2. Men who exhibited any use of stimulant drugs were significantly younger than men who reported no use of stimulant drugs (t = 8.51, P < 0.001). There were significant differences across the different drug-using groups in terms of racial background (χ2 = 72.54, P < 0.001), educational attainment (χ2 = 54.81, P<0.001), income (χ2 = 35.05, P < 0.001), and HIV serostatus (χ2 = 46.85, P < 0.001).
Men who reported decreasing stimulant drug use patterns reported greater numbers of alcoholic drinks per week than did men who reported no stimulant drug use (t = 4.28, P< 0.001) and men who increased stimulant drug use (t = 2.91, P = 0.037). Men in the consistently high use group reported higher drinking levels than did men in the no use (t = 4.58, P < 0.001) and increasing use categories (t = 2.85, P = 0.044). Men in the consistently high group reported significantly greater numbers of unprotected insertive and receptive partners than the no use group (t = 4.33, P< 0.001 and t = 5.70, P< 0.001, respectively).
Do Men with Different Substance Use Patterns Over Time Report Differences in Sexual Risk-Taking Over Time?
Table 3 gives intercept estimates for measures of sexual risk-taking at visit 40 as well as slope estimates for how these behaviors changed over time. Thus, the intercept estimates give health profiles of the men at intake; the slope values provide estimates of how health profiles changed over time among men in the varying drug use groups. Table 3 reports whether the average intercept and slope values for men in the “Increasing”, “Decreasing” and “Consistently high” groups were significantly different from men in the “No Use” reference group.
Table 3.
Random effect parameters with 95% confidence intervals for models of changes in sexual risk measures from visit 40 to visit 48 in the MACS using trajectory groups (n = 2,389)
| No use N = 1,604 | Increasing N = 108 | Decreasing 134 | Consistently high N = 189 | |
|---|---|---|---|---|
| NUAH | ||||
| ntercept | 0.807 [0.563, 1.051] | 0.782 [−0.179, 1.743] | 0.704 [−0.163, 1.571] | 2.633*** [1.890, 3.375] |
| Slope | −0.033 [−0.076, 0.011] | 0.056 [−0.112, 0.224] | −0.006 [−0.160, 0.148] | −0.062 [−0.196, 0.072] |
| NUARI | ||||
| ntercept | 0.615 [0.419, 0.812] | 0.270 [−0.504, 1.043] | 2.012*** [1.317, 2.707] | 1.895*** [1.297, 2.490] |
| Slope | −0.019 [−0.045, 0.008] | 0.130* [0.028, 0.233] | −0.236*** [−0.329, −0.142] | −0.023 [−0.104, 0.059] |
Note: The significance values in these columns reflect tests between each group and the no use comparison group
P < 0.05
P< 0.01
P < 0.001
Consistently high users of stimulant drugs reported 2.63 greater number of unprotected insertive anal sex partners than non-users at visit 40 (t = 6.95, P < 0.001). There were no significant differences in NUAII between the other groups compared to non-users at visit 40. Men in the decreasing group and the consistently high group reported 2.01 and 1.89 more NUARI partners respectively compared to non-users (t = 5.68, P < 0.001 and t = 6.23, P < 0.001, respectively). In terms of change in risky sexual behavior over time, men who were classified as decreasing use of stimulant drugs over time reported a significant reduction in unprotected receptive partners over time compared to the men who were not using stimulant drugs (reduction of 0.24 partner compared to the no use group, t = 4.93, P < 0.001). Similarly, men in the increasing group reported significantly greater numbers of unprotected receptive partners over time compared to the men who did not use stimulant drugs (t = 2.49, P = 0.013). There was a very small, non-significant reduction of NUAR1 among the consistently high users compared to non-users over time (t = 0.55, P = 0.583). Thus, in terms of sexual risk taking, men who increased or decreased stimulant drug use over time reported congruent changes in sexual risk taking over the same time period. There was minimal reduction of sexual risk-taking behaviors among those men who reported consistently high stimulant drug use over this same time period.
Discussion
This analysis of data from the MACS cohort shows that MSM exhibit remarkably different patterns of stimulant drug use over time. By far the modal pattern of “use” of these drugs is no use at all, with 78% of the sample reporting no or rare use of stimulant drugs over a four and a half year period, 5.4% reporting increasing use and an additional 6.9% reporting decreasing use, and 9.8% consistently reporting consistent high use. The dominance of abstinence (or near abstinence) from all of these forms of stimulant drug use was evident even during an historical period in which a widespread epidemic of stimulant drug use, and particularly methamphetamine use, was reported to be in force among MSM [17–19]. Despite the dominant patterns of abstinence from stimulant drug use within the entire MACS cohort, it is nonetheless true that prevalence of stimulant use among men in the MACS cohort appears to be far greater than that found in the general population of men in the United States [30] and that stimulant drug use has been associated with important health problems among gay men and other at-risk populations.
Among men who reported use of these drugs, those who used any one stimulant drug were highly likely to use other stimulant drugs, so that there are relatively few men who are exclusive users of, say, cocaine or methamphetamines alone. Furthermore, among the men who used stimulant drugs over this 4 year period, men were only somewhat more likely to report levels of consistent frequent use or increasing use over time 15% of the men in the cohort) as declining use over time (~7% of the men in the cohort). Men who discontinued stimulant drug use reported a statistically significant attenuation of risky sexual practices over time and men who increased stimulant drug use reported increasing levels of sexual risk-taking, compared to men who did not use stimulant drugs at all. The fact that men who reported any stimulant drug use were only somewhat less likely to report declining use as they were to report frequent or increasing use suggests that there may be strong tendencies toward self-control of stimulant drug use among MSM. The fact that sexual risk levels parallel stimulant drug use over time suggests that finding ways to lower rates of stimulant drug use among MSM could be a potent tool in HIV prevention efforts, as well as in the prevention of other health problems associated with stimulant drug use. It is also important to remember that while ongoing analyses of cohort studies using biological end-points report that stimulant drug use is closely associated with a sizeable proportion of HIV seroconversions [4, 24], other important phenomena are also in play to drive HIV risk among MSM that are probably independent of substance use [31], Addressing prevention needs that are associated with substance use and those that are largely independent of substance use will be important to forging effective prevention models for MSM. In addition, the fact that the men in this analysis who were most likely to be stimulant drug users were younger suggests that prevention and treatment programs should be designed to be especially welcoming to younger men.
The data described here were all collected as part of the ongoing MACS cohort study, and so are susceptible to biases that result from participation in ongoing cohort studies as well as possible self-report biases. Furthermore, this analysis reports data for a four and a half year period of time in these men’s lives. Longer periods of measurement of stimulant drug use in the cohort, or measuring stimulant use during a different four and a half year period might reveal different trajectories of drug use. These design properties of the MACS might be expected to bias estimates of varying rates of distinct drug use patterns over time. That is, cohort, aging, mortality, drop-out, self-report and long term measurement effects might work to produce low-end estimates of long-term heavy drug use over long periods of time, although cohort, aging and mortality effects would be observed among any group of people followed over time. In addition, the measurement approaches used in this study do not allow us to demonstrate that stimulant drug use preceded risky sexual behavior. However, if the trends reported here represent broader drug use patterns found among MSM over time, it seems clear that important tendencies toward moderate or abstinent drug use exist among MSM, and that further study of patterns of resilience against frequent drug use might inform the design of intervention programs to reduce substance abuse-related harm among gay men in important ways.
To expand on this last point, while a classical analysis of drug use patterns within a high risk population might be to focus on the men who report heavy drug use or initiate heavy drug use over time, in the MACS, such men account for only about 15% of the cohort. Thus, an analysis that focuses exclusively on describing patterns of heavy or problematic use of stimulant drugs would work, in practice, to relegate 85% of the sample that either never used these drugs frequently, used them infrequently or moved towards discontinuance of use to that of a comparison group used to highlight the characteristics of men given to problematic substance use. Marginalizing the experiences of men who do not manifest heavy drug use patterns over time to that of a comparison group function may blind us to the discovery of useful self-regulation strategies that work to prevent the onset of problematic drug use careers. The dominant patterns of abstinence and the important tendency towards discontinuance of use may suggest that, in a social context where there may be strong pressure and ample opportunities to use stimulants, MSM have developed strong monitoring skills to resist not only uptake but also frequent use of stimulant drugs. However, factors that promote successful self-monitoring or even discontinuance of stimulant drug use are typically understudied in descriptions of substance abuse careers among MSM.
This latter point is important in terms of examining the logic of intervention design to prevent substance abuse within communities of high risk individuals. One path to intervention design would be to identify the characteristics of individuals who manifest substance abuse careers, find ways to address the factors that make such individuals vulnerable to the development of substance abuse careers, and then test interventions that are based on a vulnerability analysis. However, another approach to intervention design might be to understand the factors that underlie resilience among the men who never used stimulants, moderated their use or never used the drugs frequently, find ways to incorporate these strengths into intervention design for high risk men, and then test these interventions. Put another way, should the design of interventions to prevent problematic substance abuse be based on the experiences of the small proportion of men who manifest problematic drug abuse careers (in the case of the MACS cohort, approximately 15% over a 4 year period) or on the far larger group of men who do not manifest these problems at all over an extended period of time? Would interventions be most effective if they are based on an analysis of vulnerability or of resilience?
This last question, of course, may present a false dichotomy in terms of the logic of intervention design. Although important interventions have been developed to promote gay men’s health, and a growing number of these programs yield efficacious effects in randomized controlled trials, the dominant approach to these intervention designs has been based on vulnerability analyses. Research that is designed to identify strengths that gay men exhibit in the face of drug abuse epidemics may yield insights that would be central to the design of interventions with increased potency to control harm associated with substance abuse epidemics among MSM. To the extent that HIV risk and stimulant drug use are linked among MSM, these interventions would also serve an important function in reducing HIV transmission among MSM. Such research might include qualitative research to understand how men themselves manage their risk for problematic drug use, work that would turn these insights into theoretical statements, and thus provide a blueprint to explain both resilience and vulnerability to substance abuse careers among MSM. Testing of new theory to explain resilience against the development of a substance abuse career might in turn result in new methods to support resolution of these careers. While this approach may seem quite novel, the analysis of the MACS data presented here would suggest that strength-based approaches to substance abuse prevention efforts might well be a useful addition to the more classical vulnerability-based approaches to intervention design for MSM.
Acknowledgments
Support for this study was provided by National Institute of Drug Abuse grant R01 DA022936. We would also sincerely like to thank the men who have participated in the MACS since its inception for their immense contribution to HIV research. This article is dedicated to the memory of Keith Bussy, a man whose tireless advocacy for HIV infected men improved the lives of countless people. His dedication and constant smile were an inspiration to all who knew him.
Contributor Information
Sin How Lim, Department of Behavioral and Community Health Sciences, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, USA.
David Ostrow, Ogburn-Stouffer Center for Social Organization Research at the National Opinion, Research Center, University of Chicago, Chicago, IL, USA.
Ron Stall, Email: rstall@pitt.edu, Department of Behavioral and Community Health Sciences, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, USA.
Joan Chmiel, Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Amy Herrick, Department of Behavioral and Community Health Sciences, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, USA.
Steve Shoptaw, Department of Family Medicine and Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA.
Uyen Kao, Department of Family Medicine, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA.
Adam Carrico, Department of Medicine, Center for AIDS Prevention Studies, University of California, San Francisco, CA, USA.
Michael Plankey, Department of Medicine, Georgetown University Medical Center, Washington, DC, USA.
References
- 1.Page-Shafer K, Veugelers PJ, Moss AR, Strathdee S, Kaldor JM, van Griensven GJ. Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982–1994. Am J Epidemiol. 1997;146(7):531–42. doi: 10.1093/oxfordjournals.aje.a009311. [DOI] [PubMed] [Google Scholar]
- 2.Chesney MA, Barrett DC, Stall R. Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health. 1998;88(l):113–6. doi: 10.2105/ajph.88.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchacz K, McFarland W, Kellogg TA, et al. Amphetamine use is associated with increased HIV incidence among men who have sex with men in San Francisco. AIDS. 2005;19(13):1423–4. doi: 10.1097/01.aids.0000180794.27896.fb. [DOI] [PubMed] [Google Scholar]
- 4.Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20(5):731–9. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- 5.Plankey MW, Ostrow DG, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2007;45(l):85–92. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168(2):93–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Diamond C, Thiede H, Perdue T, et al. Seroepidemiology of human herpesvirus 8 among young men who have sex with men. Sex Transm Dis. 2001;28(3):176–83. doi: 10.1097/00007435-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case- control study. J Med Internet Res. 2004;6(4):e41. doi: 10.2196/jmir.6.4.e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32(7):458–63. doi: 10.1097/01.olq.0000168280.34424.58. [DOI] [PubMed] [Google Scholar]
- 10.Reback CJ, Kamien JB, Amass L. Characteristics and HIV risk behaviors of homeless, substance-using men who have sex with men. Addict Behav. 2007;32(3):647–54. doi: 10.1016/j.addbeh.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Semple SJ, Patterson TL, Grant I. Binge use of methamphetamine among HIV-positive men who have sex with men: pilot data and HIV prevention implications. AIDS Educ Prev. 2003;15(2):133–47. doi: 10.1521/aeap.15.3.133.23835. [DOI] [PubMed] [Google Scholar]
- 12.Klitzman RL, Greenberg JD, Pollack LM, et al. MDMA (‘ecstasy’) use, and its association with high risk behaviors, mental health, and other factors among gay/bisexual men in New York City. Drug Alcohol Depend. 2002;66(2):115–25. doi: 10.1016/s0376-8716(01)00189-2. [DOI] [PubMed] [Google Scholar]
- 13.Redfeam PJ, Agrawal N, Mair LH. An association between the regular use of 3,4 methylenedioxy-methamphetamine (ecstasy) and excessive wear of the teeth. Addiction. 1998;93(5):745–8. doi: 10.1046/j.1360-0443.1998.93574510.x. [DOI] [PubMed] [Google Scholar]
- 14.Richards JR, Brofeldt BT. Patterns of tooth wear associated with methamphetamine use. J Periodontol. 2000;71(8):1371–4. doi: 10.1902/jop.2000.71.8.1371. [DOI] [PubMed] [Google Scholar]
- 15.Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121(2):127–32. doi: 10.1177/003335490612100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(11):62–70. doi: 10.1093/jurban/jti025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobs A. The New York Times. Sect Bl 2002. Jan 29, In clubs, a potent drug stirs fear of an epidemic. [Google Scholar]
- 18.Kurtz SP. Post-circuit blues: motivations and consequences of crystal meth use among gay men in Miami. AIDS Behav. 2005;9(l):63–72. doi: 10.1007/s10461-005-1682-3. [DOI] [PubMed] [Google Scholar]
- 19.O’Bryan W. Crystal and the community: a grassroots alliance gains momentum in its fight against methamphetamines. Metro Weekly-Washington. 2005 http://www.metroweekly.com/feature/?ak=1672. Cited Oct 25 2009.
- 20.Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR., Jr The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am J Epidemiol. 1987;126(2):310–8. doi: 10.1093/aje/126.2.310. [DOI] [PubMed] [Google Scholar]
- 21.Detels R, Phair JP, Saah AJ, et al. Recent scientific contributions to understanding HIV/AIDS from the Multicenter AIDS Cohort Study. J Epidemiol. 1992;2:S11–9. [Google Scholar]
- 22.Dudley J, Jin S, Hoover D, Metz S, Thackeray R, Chmiel J. The Multicenter AIDS Cohort Study: retention after 9 1/2 years. Am J Epidemiol. 1995;142(3):323–30. doi: 10.1093/oxfordjournals.aje.a117638. [DOI] [PubMed] [Google Scholar]
- 23.Ostrow DG. The role of drugs in the sexual lives of men who have sex with men: continuing barriers to researching this question. AIDS Behav. 2000;4(2):205–19. [Google Scholar]
- 24.Ostrow DG, Plankey MW, Cox C, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51(3):349–55. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gribble JN, Miller HG, Cooley PC, et al. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35(6–8):869–90. doi: 10.3109/10826080009148425. [DOI] [PubMed] [Google Scholar]
- 26.Nagin D. Analyzing developmental trajectories: a semi-parametric group-based approach. Psychol Methods. 1999;4:139–57. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 27.Nagin D. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 28.Raudenbush SW, Bryk AS. Advanced quantitative techniques in the social sciences series 1. 2. Thousand Oaks, CA: Sage Publications; 2002. Hierarchical linear models: applications and data analysis methods. [Google Scholar]
- 29.Singer JD. Using SAS proc mixed to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23(4):323–55. [Google Scholar]
- 30.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. National Household Survey on Drug Abuse: summary of findings from 1999. Department of Health and Human Services; Rockville, MD: 2000. [Google Scholar]
- 31.Grov C, Parsons JT, Bimbi DS. In the shadows of a prevention campaign: sexual risk behavior in the absence of crystal methamphetamine. AIDS Educ Prev. 2008;20(1):42–55. doi: 10.1521/aeap.2008.20.1.42. [DOI] [PubMed] [Google Scholar]


