Abstract
Background/Aim:
Morbidly obese patients have a high prevalence of fatty liver disease and its serious complications, and high prevalence of abnormal liver function tests (LFT). The LFT can give a clue to the liver damage and correlate with activity. We aim to study the pattern of LFT in morbidly obese Saudi patients undergoing bariatric surgery in Eastern region.
Patients and Methods:
Medical records of patients undergoing bariatric surgery were reviewed. Demographic data, comorbid conditions, and medications taken were recorded. Intraoperative liver appearance was noted. Patients with alcohol intake or without LFT were excluded.
Results:
Out of 113 patients, 15 patients were excluded, and of the remaining 98 patients analyzed, 58.2% were females. Mean age was 33.1 ± 8.87 years. Mean body mass index (BMI) was 53.7 ± 1.27 kg/m2. Abnormal LFT (alanine aminotransaminase (ALT), aspartate aminotransaminase (AST) alkaline phosphatase (ALK), and Gamma glutamyl transpeptidase (GTT) were observed in 17.3%, with 1.5 to 2 times the upper limit of normal. ALT was most elevated in 12.2%. Abdominal ultrasonography was done in 67 (68.4%) patients, of whom 51 (76%) had fatty liver. Comorbid conditions including diabetes mellitus, hypertension, hyperlipidemia, bronchial asthma, and obstructive sleep apnea were observed in 51 (51.50%) patients, eight of them (16.3%) had abnormal LFT. No intraoperative changes of cirrhosis were observed.
Conclusion:
The prevalence of abnormal LFT is low in morbidly obese patients from the eastern region of Saudi Arabia. A prospective study with a larger sample and liver biopsy, is needed to clarify the findings.
Keywords: Bariatric surgery, liver function tests, morbidly obese
The biochemical tests that reflect liver cell damage or synthetic and excretion function are the main indicators of liver status and functions. These tests include liver enzymes: Alanine aminotransaminase (ALT), aspartate aminotransaminase (AST), alkaline phosphatase (ALK) and gamma glutamyl transpeptidase (GTT). The other important tests are serum bilirubin, albumin and international normalized ratio (INR). In clinical practice, these tests or parameters are used to guide the management of liver diseases. Uncommonly, abnormalities of liver enzymes are found in asymptomatic healthy individuals.[1] In obese subjects, the liver function tests (LFT) derangements have been noticed to be more frequent than in non obese ones due to the high prevalence of non alcoholic fatty liver disease (NALFD) and its consequences.[2–5] Numerous studies have shown higher prevalence of liver function derangements and high prevalence of liver damage as well in morbidly obese patients undergoing weight reduction surgery.[6–9]
In Saudi Arabia, despite the high prevalence of obesity,[10,11] we have not come across data that looked at the prevalence of liver function abnormalities in asymptomatic, obese or morbidly obese subjects undergoing bariatric surgery. Nowadays there are many centers in the country performing weight reduction surgery for morbid obesity. One of the rare complications of such surgery is liver cirrhosis and liver failure. In our center, we had two cases of liver cirrhosis (unreported) post-bariatric surgery; one died and the other had decompensated cirrhosis. There are conflicting reports on the correlation between LFT abnormalities and degree of liver damage, but most studies show a positive correlation.[7–9] In some chronic liver diseases, e.g., chronic hepatitis C, the prevalence of significant fibrosis with persistently normal liver function has been reported in around 25% of patients.[12,13]
The importance of the preoperative LFT abnormalities in predicting the presence and significance of pre-existing liver disease in morbidly obese patients going for weight reduction surgery, and the need for liver biopsies, are still open questions, the answers for which will require further studies.
The aim of this study is to assess the prevalence of abnormal LFTs in morbidly obese Saudi patients undergoing weight reduction surgery.
PATIENTS AND METHODS
The charts of morbidly obese patients who had undergone weight reduction surgery between November 2005 and July 2008 were reviewed. Demographic data, patients’ characteristics, comorbid conditions, medications, preoperative blood tests, including LFT, viral hepatitis serology, serum cholesterol and triglycerides, INR and platelets’ count, were all recorded. The LFT panel included ALT, AST, ALK, GTT, bilirubin and albumin. All blood tests were done in the same laboratory using the same standards, which is in compliance with internationally accepted figures for normal ranges of laboratory tests. Intraoperative findings of liver morphologies were also noted. Patients with history of alcohol consumption and those without preoperative LFT were excluded. All patients were included irrespective of the type of bariatric surgery they were subjected to. Laboratory test values above the upper limit of normal (ULN) were considered as abnormal. Liver ultrasound reports were recorded, and their findings were categorized as normal or indicative of fatty infiltration of the liver.
The data were entered and analyzed using the Statistical Package for Social Sciences (SPSS-Version 16, Chicago, IL, USA). Frequency distributions were generated and comparisons between categorical data were done using Chi-squared test. A P value of 0.05 or less was considered as indicative of statistical significance.
RESULTS
This study was carried out in the year 2009, in King Abdulaziz Medical City, National Guard, at Al-Ahsa, Saudi Arabia.
The hospital records included 113 patients with morbid obesity who had undergone bariatric surgery. The sample involved in this study amounted to 98 patients forming (86.7%) of the initial sample included.
Male and female patients comprised 41.8% and 58.2% of the sample, respectively. The mean (± standard deviation) age of patients was 33.1 ± 8.87 years. The mean body mass index (BMI) was 53.7 ± 1.27 kg/m2.
Abnormal liver LFTs were observed in 17 patients (17.3%) [Table 1]. The most frequently elevated enzymes were ALT shown by 12 (12.2%) patients, followed by AST. The highest level of ALT amounted to up to four times the ULN [Figure 1].
Table 1.
Characteristics of 98 morbidly obese patients (n = 98)
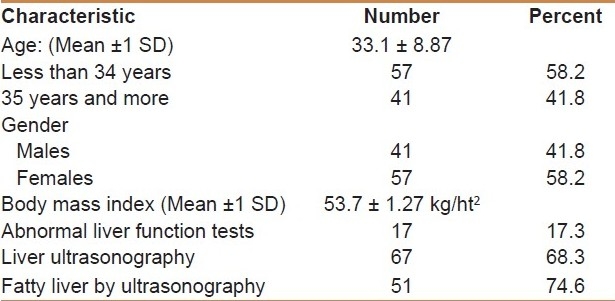
Figure 1.
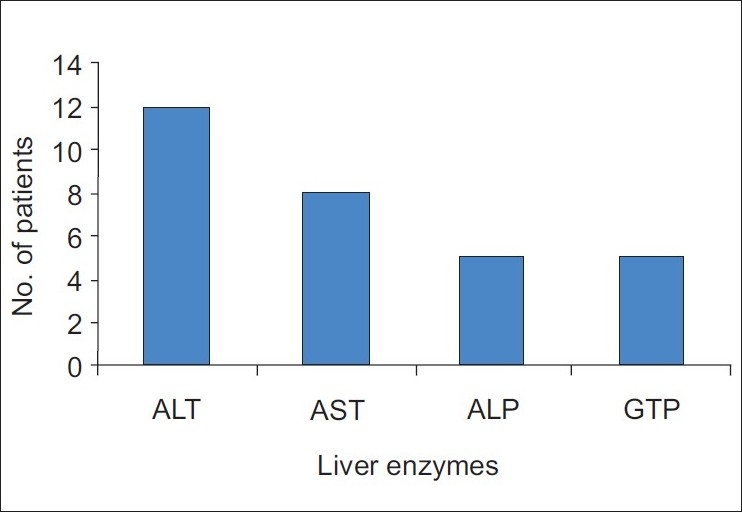
Liver function test abnormalities in the morbidly obese subjects undergoing bariatric surgery
Comorbid conditions were observed in 51 (52%) cases; the most frequently observed conditions were diabetes mellitus and hypertension. Of those patients, 9 (9.1%) had abnormal LFTs [Table 2].
Table 2.
Comorbid conditions among 51 morbidly obese patients out of (n = 98)
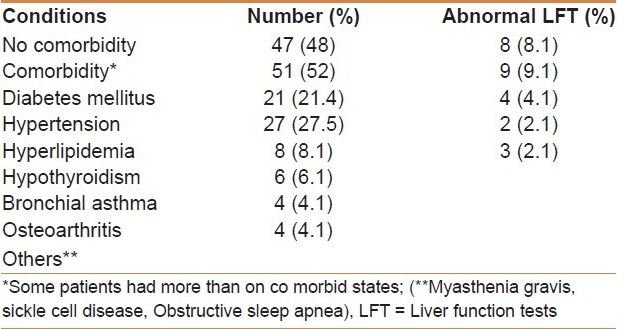
Lipid profiles were tested in 28 patients. Hypercholesterolemia or hypertriglycideremia were observed in eight patients and three patients had abnormal LFTs.
Screening for hepatitis B virus (HBV) was carried out in 19 patients and that for hepatitis C virus (HCV) in 20 patients, of whom two patients were positive for HCV antibodies, but none of them had abnormal LFTs.
Patients who had undergone abdominal ultrasound examination amounted to 67 (68.4%) of the studied sample. Fatty liver appearances were observed in 51 patients comprising 74.6% [Table 1].
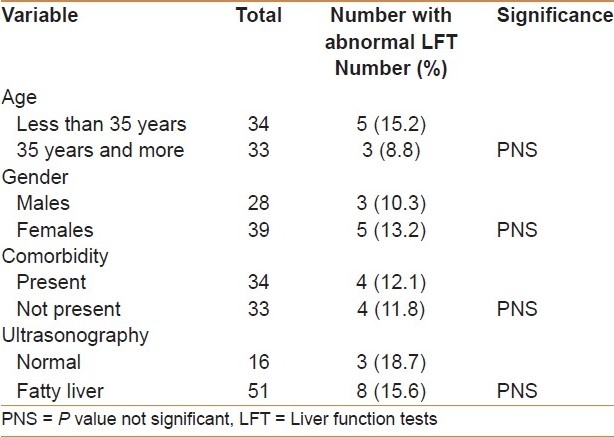
A sub-sample of patients who had undergone liver ultrasound examination was generated which included 67 patients. Abnormal LFTs were observed in 8 (11.9%) cases, compared with two patients with abnormal LFT in those with normal ultrasound.
There were more patients with abnormal LFT who were younger than 35 years than those who were older (15.2% and 8.8%, respectively), but the difference was not statistically significant. There was no significant gender difference in having abnormal LFT between patients who had comorbid conditions, or between patients who had or had no ultrasonographic fatty liver appearance [Table 3].
Table 3.
Relation of abnormal liver functions with age, gender, comorbidity status, in patients undergoing abdominal ultrasonography (n = 67)
DISCUSSION
In asymptomatic healthy adults, abnormal LFT has been found in around 7 to 9% of cases without identifiable cause.[1] In morbidly obese patients going for weight reduction surgery, the prevalence of abnormal LFT has been noticed to be much higher.[2–5] Several studies on such patients reported a prevalence of 19 to 24%.[2–5]
In our patients, abnormal LFT prevalence was rather lower than that reported in other studies, despite the similarity of patients’ characteristics, except in one study where it showed a similar result.[3] One possible explanation is that we might have slightly different or lower figures of normal values. The laboratory reference values used in our laboratory were of the same standard reference adopted worldwide, as there is no available baseline data exploring normal LFT values in our normal individuals.
Literature review reveals high prevalence of NAFLD in morbidly obese subjects (upto 96%), with a high prevalence of steatosis as well.[6–8,11,14,15]
There are also reports of advanced liver disease with fibrosis in 9 to 21% cases,[6–8,14,15] as well as cirrhosis in 4% cases.[2,7,11] Most of these findings were histologically proven.
Several studies have pointed to a positive correlation between liver enzyme elevations and the degree of liver damage, where patients with advanced liver disease had more LFT derangements, in particular AST and ALT.[6,8,16–19]
In view of these findings, around 17% of our study sample might have significant liver damage.
On the contrary, other reports have not shown any positive correlation between histological findings of NASH, fibrosis or cirrhosis, and LFT abnormalities.[15,20]
Whether there is positive or negative correlation, it is difficult to reflect this correlation to our patients and extrapolate a judgment of the degree of liver involvement.
Liver biopsy has been advocated routinely during bariatric surgery to determine the prevalence and natural history of NASH, which will have important implications in directing future therapeutics for obese patients with NASH, and for patients undergoing bariatric surgery.[2,21]
Our study was not supported by liver biopsy because it is retrospective, and there was no clinical indication for the operating surgeon to perform liver biopsy during surgery.
In our study, 74.6% of the 67 patients who had ultrasonographic examination of the liver had features of fatty liver, and almost 25% had abnormal LFT. Similar figures have been reported.[22] There has been a study which has shown a correlation between ultrasonographic findings of fatty liver and histological derangements.[23]
In many of the previous studies, elevated liver enzymes were found to be more frequent in patients with comorbid conditions such as diabetes mellitus and hyperlipidemia. However, this was not observed in our patients.
ALT has been found to be the most elevated liver enzyme in our patients. This finding is in agreement with previous reports.[3,18,20]
We had two patients (not included in the study, and not reported) who developed decompensated liver cirrhosis post-bariatric surgery, of whom one died later. We could not tell whether they had preoperative significant liver disease, or complication of bariatric surgery.
Our study has the limitation that it is retrospective and lacked liver biopsy results. However, it highlights important information of a low prevalence of LFTs abnormalities in this group of patients.
Further prospective studies incorporating liver biopsies are warranted in order to reliably identify the prevalence and degree of liver damage of these patients.
CONCLUSIONS
This study demonstrates a low prevalence of abnormal LFT in our morbidly obese patients who underwent bariatric surgery. This may serve as an indirect indication of a lower prevalence of significant liver damage in these subjects. It is the first study in our area, and could serve as baseline information in these subjects. A prospective study with a larger sample incorporating liver biopsy will be needed to make the issue clearer and to assess the correlation between LFTSs and histological activity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ioannou GN, Boyko EJ, Lee SP. The prevalence of predictors of elevated serum aminotransferase activity in the United States in 1999-2002. Am J Gastroenterol. 2006;101:76–82. doi: 10.1111/j.1572-0241.2005.00341.x. [DOI] [PubMed] [Google Scholar]
- 2.Del Gaudio A, Boschi L, Del Gaudio GA, Mastrangelo L, Munari D. Liver damage in obese patients. Obes Surg. 2002;12:802–4. doi: 10.1381/096089202320995592. [DOI] [PubMed] [Google Scholar]
- 3.Albert S, Borovicka J, Thurnheer M, Lange J, Meyenberger C. Pre- and postoperative transaminase changes within the scope of gastric banding in morbid obesity. Praxis. 2001;90:1459–64. [PubMed] [Google Scholar]
- 4.Wolf AM, Busch B, Kuhlmann HW, Beisiegel U. Histological changes in the liver of morbidly obese patients: Correlation with metabolic parameters. Obes Surg. 2005;15:228–37. doi: 10.1381/0960892053268408. [DOI] [PubMed] [Google Scholar]
- 5.Nomura F, Ohnishi K, Satomura Y, Ohtsuki T, Fukunaga K, Honda M, et al. Liver function test in moderate obesity-study in534 moderately obese subjects among 4613 male company employees. Int J Obes. 1986;10:349–54. [PubMed] [Google Scholar]
- 6.Boza C, Riquelme A, Ibanz L, Durate I, Norero E, ViViani P, et al. Predictors of nonalcoholic steatohepatitis (NASH) in obese patients undergoing gastric bypass. Obes Surg. 2005;15:1148–53. doi: 10.1381/0960892055002347. [DOI] [PubMed] [Google Scholar]
- 7.Beymer C, Kowdley KV, Larson A, Edmonson P, Dellinger EP, Flum DR. Prevalence and predictors of asymptomatic liver disease in patients undergoing gastric bypass surgery. Arch Surg. 2003;138:1240–4. doi: 10.1001/archsurg.138.11.1240. [DOI] [PubMed] [Google Scholar]
- 8.Ong JP, Elariny H, Collantes R, Younoszai A, Chandhoke V, Reines HD, et al. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Obes Surg. 2005;15:310–5. doi: 10.1381/0960892053576820. [DOI] [PubMed] [Google Scholar]
- 9.Al Nuaim AR, AL-Rubeaan K, AL-Mazrou Y, AL-Doghari N, Khoja T. High prevalence of overweight and obesity in Saudi Arabia. Int J of Obes Relat Metab Disord. 1996;20:547–52. [PubMed] [Google Scholar]
- 10.Al-Nozha MM, AL-Mazrou YY, AL-Maatouq MA, Arafah MR, Khalil MZ, Khan NB, et al. Obesity in Saudi Arabia. Saudi Med J. 2005;26:825–29. [PubMed] [Google Scholar]
- 11.Luykx FH, Desaive C, Thiry A, Dewe W, Scheen AJ, Gielen JE, et al. Liver abnormality in severely obese patients: Effect of drastic weight loss after gastroplasty. Int J Obes Relat Metab Disord. 1998;22:222–6. doi: 10.1038/sj.ijo.0800571. [DOI] [PubMed] [Google Scholar]
- 12.de Santana NP, de Freitas LA, Lyra AC, Parana R, Santan G, Trepo C, et al. Liver histological alterations in patients with chronic hepatitis C and normal ALT levels in the city of Salvador, Northeast-Brazil. Braz J Infect Dis. 2005;9:134–41. doi: 10.1590/s1413-86702005000200003. [DOI] [PubMed] [Google Scholar]
- 13.Sanai FM, Benmousa A, Al-Hussaini H, Ashraf S, Alhafi O, Abdo AA, et al. Is serum alanine aminotransaminase level a reliable marker of histological disease in chronic hepatitis C infection? Liver Int. 2008;28:1011–8. doi: 10.1111/j.1478-3231.2008.01733.x. Epub 2008 Apr 1. [DOI] [PubMed] [Google Scholar]
- 14.Albert S, Brovicka J, Thurnheer M, Lange J, Meyenberger C. Pre- and postoperative transaminase changes within the scope of gastric banding in morbid obesity. Praxis. 2001;90:1459–64. [PubMed] [Google Scholar]
- 15.Silverman JF, O’brien KF, Long S, Leggett N, Khazanie PG, Pories WJ, et al. Liver pathology in morbidly obese patients with and without diabetes. Am J Gastroenterol. 1990;85:1349–55. [PubMed] [Google Scholar]
- 16.Chavarria-Areiniega S, Lopez-alvarenga JC, Uribe-Uribe NO, Herrera-Hernandez M, Gonzalez-Barranco J. Relationship between morphological diagnosis of NASH and liver function tests in a group of patients with morbid obesity. Rev Invest Clin. 2005;57:505–12. [PubMed] [Google Scholar]
- 17.Dixon JB, Bahthal PS, O’brien BE. Nonalcoholic fatty liver disease: Predictors of nonalcoholic steatohepatitis and liver fibrosis in Severely Obese Subjects. Am J Gastroenterol. 2001;121:91–100. doi: 10.1053/gast.2001.25540. [DOI] [PubMed] [Google Scholar]
- 18.Gholam PM, Flancbaum L, Machan JT, Charney DA, Kolter DP. Nonalcoholic fatty liver disease in severely obese subjects. Am J Gastroenterol. 2007;102:399–408. doi: 10.1111/j.1572-0241.2006.01041.x. [DOI] [PubMed] [Google Scholar]
- 19.Suzuki A, Lymp J, Sauver JS, Angulo P, Lindor K. Values and limitations of serum aminotransferases in clinical trials of nonalcoholic steatohepatitis. Liver Int. 2006;26:1209–16. doi: 10.1111/j.1478-3231.2006.01362.x. [DOI] [PubMed] [Google Scholar]
- 20.Silverman EM, Sapala JA, Appelman HD. Regression of hepatic fibrosis in morbidly obese persons after gastric bypass. Am J Clin Pathol. 1995;104:23–31. doi: 10.1093/ajcp/104.1.23. [DOI] [PubMed] [Google Scholar]
- 21.Shalhub S, Parsee A, Gallagher SF, Haines KL, Wiliikomm C, Brantly SG, et al. The importance of routine liver biopsy in diagnosing nonalcoholic steatohepatitis in bariatric patients. Obes Surg. 2004;14:54–9. doi: 10.1381/096089204772787293. [DOI] [PubMed] [Google Scholar]
- 22.Teivelis MP, Faintuch J, Ishadia R, Sakai P, Bresser A, Gama-Rodrigues J. Endoscopic and ultrasonographic evaluation before and after Roux-en-Y gastric bypass for morbid obesity. Arg Gastroenterol. 2007;44:8–13. doi: 10.1590/s0004-28032007000100003. [DOI] [PubMed] [Google Scholar]
- 23.Liang RJ, Wang HH, Lee WJ, Liew PL, Lin JT, Wu MS. Diagnostic value of ultrasonic examination for nonalcoholic steatohepatitis in morbidly obese patients undergoing laproscopic bariatric surgery. Obes Surg. 2007;17:45–56. doi: 10.1007/s11695-007-9005-6. [DOI] [PubMed] [Google Scholar]


