Abstract
Unsedated colonoscopy has been an evolving subject ever since its initial description four decades ago. Failure in unsedated diagnostic cases due to patient pain led to the introduction of sedation. Extension to screening cases, albeit logical, created a sedation-related barrier to colonoscopy screening. In recent years a water method has been developed to combat the pain during unsedated colonoscopy in the US. In randomized controlled trials the water method decreases pain, increases cecal intubation success, and enhances the proportion of patients who complete unsedated colonoscopy. The salvage cleansing of suboptimal bowel preparation by the water method serendipitously may have increased the detection of adenoma in both unsedated and sedated patients. The state-of-the-art lecture concludes that unsedated colonoscopy is feasible. The hypothesis is that recent advances, such as the development of the water method, may contribute to reviving unsedated colonoscopy as a potentially attractive option for colon cancer screening and deserves to be tested.
Keywords: Adenoma detection, colonoscopy, colorectal cancer screening, sedation risk-free colonoscopy, unsedated colonoscopy, water method
Colonoscopy was developed as an unsedated procedure about 40 years ago. Failure in a minority of early cases was due to patient anxiety and discomfort. Subsequently, sedation was introduced as a solution.[1–2] In the US, sedation has become the standard of practice for all colonoscopies, including screening cases.[3] Unsedated colonoscopy carries a negative image, where patients are deprived of medications that ensure relief and amnesia of the discomfort.[4–6] To counter the stigma, supporters of unsedated colonoscopy proposed alternative descriptions. Sedation-free was used by Takahashi in Japan,[7,8] Park in Korea,[9] and Fennerty in US;[10] medication-free by Ylinen in Finland,[11] and sedationless by Rφsch in Germany.[12,13]
The term sedation risk-free (SRF) colonoscopy, a name proposed in a ‘think-outside-the-box’ editorial,[14] was used to emphasize its advantage in minimizing the burden of colorectal cancer screening. The reviewed data confirm that sedation risk-free colonoscopy continues to be practiced in many parts of the world.[15]
In the primary care literature in the US, sedation has been identified as a barrier to colonoscopy screening of colorectal cancer,[16] wherein, 14% of the patients cited the need for an escort and time-off after sedation as the reasons for non-adherence to the recommended screening. A US study, based on detailed patient diaries,[17] revealed that a median of 39.5 hours are spent for a colonoscopy. After colonoscopy, the median time to return to routine is 15.8 hours, and another 1.8 hours for recovery to normal. In a review of over 20 thousand reports in the Clinical Outcomes Research Initiative Database, sedation-related complications occurred in 1.3%.[18] The most common were respiratory suppression reflected by hypoxia (0.75%), and cardiovascular events such as hypotension and bradycardia (0.49%).
The various options of colonoscopy with or without routine sedation are summarized in a recent review.[19] The options can be divided into scheduled and unscheduled. The only unscheduled option is unsedated when patients present after completing bowel preparation, but without an escort. In the US, 1 – 2% of the patients fall into this category. The implication is that even non-advocates of unsedated colonoscopy have been willing to perform colonoscopy without sedation in about 1 to 2% of their patients. The scheduled options range from deep sedation, conscious sedation, to the unsedated. The advantage of deep sedation to the endoscopist is that productivity can be increased by about two-thirds. However, it is more expensive, and if an anesthesiologist is involved, the fee is more than that of the endoscopist. Conscious sedation can be divided into traditional, minimal sedation, as-needed, and on-demand sedation. Use of as-needed sedation is based on the decision of the colonoscopist. It carries a risk of coercion because endoscopists have been shown to be less accurate than nurses and patients in gauging discomfort during colonoscopy. In the use of as-needed sedation, patients are often told to bear the discomfort in order to complete the visualization process. On-demand sedation is decided by the patients. It is less coercive. The remaining discussion will focus on the scheduled unsedated and on-demand sedation options.
At the Sepulveda Ambulatory Care Center, colonoscopy was routinely performed with conscious sedation prior to 2002. Since 2002, scheduled unsedated colonoscopy has been offered as an option.[20–23] This began as a performance improvement project, to restore the discontinued sedated colonoscopy service as a result of nursing shortage.[21] The information in the literature was summarized and discussed with the patients in the clinic during a pre-colonoscopy visit, which is standard practice.[22] Without sedation, there is no risk of sedation-related complications, no escort requirement, no need for time spent in recovery, and no activity restrictions after the examination. The endoscopist minimizes the amount of air used and the procedure time to decrease patient discomfort. During the examination, the endoscopist verbally interacts with the patient about abdominal discomfort in order to obtain a head-start on the implementing maneuvers to avert the upcoming discomfort. The patients are asked to choose either the sedated or unsedated option. About one-third of the patients chose the SRF option,[20,21] and the main reasons include the ability to communicate and the lack of escort requirement.[21]
Overall, the average success rate of cecal intubation with unsedated colonoscopy is about 80%.[15] The major limiting factor is discomfort, in part because air lengthens the colon and exaggerates angulations at all the flexures and redundant segments making it more difficult to perform unsedated colonoscopy. In developing a modern method we combined the maneuvers described in several water-related methods,[24] with turning the air pump off to avoid colon elongation.[25,26] Residual air was removed by suction to minimize angulations well-illustrated by diagrams provided by Mizukami.[27] We then used water to open the lumen to assist insertion and water exchange to clear the view. Details of the modern water method can be described as follows:[19] When the colonoscope is inserted into the rectum, air is removed by suction to collapse the rectal lumen. The tip of the colonoscope is then pushed up against the slit-like opening or the convergence of folds leading to the lumen proximal to the rectum. The lumen proximal to the rectum opens up with water infusion. Whenever air pockets are encountered, the air is removed by suction. Residual feces suspended in the water in the lumen are removed by suction and water is infused to clear the view. Infused water removed by suction produces turbulence in the vicinity of the tip of the colonoscope to dislodge feces adherent to the adjacent mucosa. The process is repeated followed by insertion of the colonoscope further into the colon. Water exchange may be necessary in the cecum, before the appendix opening can be clearly identified. The appendix opening may appear as ‘concentric rings’ in a collapsed, but water-filled cecum. Recognition of diverticular openings is important to avoid inappropriate attempts to distend the diverticulum with water.
The uncontrolled, non-randomized, consecutive group experience on cecal intubation in the scheduled unsedated patients[28] was as follows: When the traditional air method was used, the cecal intubation rate was only 76%, with the main limiting factor being patient discomfort. When we switched to the water method, the cecal intubation rate significantly increased to 97%. Willingness to repeat unsedated colonoscopy in the future significantly improved from 69 to 90%. The proportion of patients with significant pain during insertion decreased from 12 to 1.6%. This could be due to the cleansing of the water exchange. The proportion of patients with poor bowel preparation during withdrawal decreased from 12 to 1.6%.
We then performed two proof-of-concept randomized controlled trials (RCTs).[29,30] One RCT focused on scheduled unsedated colonoscopy.[29] The primary outcomes were discomfort during and after unsedated colonoscopy. Maximum discomfort during colonoscopy was scored as follows: 0 = none, 10 = most severe; verbal scale. Overall discomfort after colonoscopy was scored as follows: 0 = none, 10 = most severe; visual analog scale. The second RCT focused on sedation on demand.[30] The primary outcome was the completion of unsedated examination. Colonoscopy was started without premedication. When the patient reported a pain score of 2, the nurse offered medications to the patient who could either accept or decline. The colonoscopist did not influence the decision. The data of the scheduled unsedated patients[29] showed that the median maximum discomfort score during colonoscopy was significantly lower in the water group (3 vs. 6). The median overall discomfort score after colonoscopy (2 vs. 3) was lower in the water group, and the difference approached significance. The proportion with severe overall discomfort score of ≥ 5 after colonoscopy was significantly lower in the water group (12 vs. 33%). The cecal intubation rate (98 vs. 78%) and willingness to repeat unsedated colonoscopy (93 vs. 78%) were both significantly higher in the water group. The results of the on-demand sedation study[30] showed that combined with the option of sedation on demand, the water method permitted a significantly higher proportion of patients to complete colonoscopy without sedation (78 vs. 54%). The 50 patients examined by the water method collectively spent less time in recovery on-site (162 minutes) and at home (303 hours).
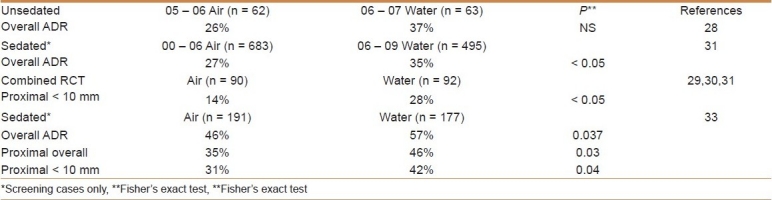
When attention was focused on adenoma detection, a fascinating pattern emerged [Table 1]. The consecutive group data in one study showed a trend toward a higher adenoma detection rate (ADR) in the water-method group.[28] With a large number of patients whose data were stored in an endoscopic database at the Sacramento VAMC, from 2000 to 2006 (air method) and 2006 to 2009 (water method), a significantly higher ADR in the water group was revealed.[31] When we assessed the pooled data in the two proof-of-concept RCTs,[29,30] we found a significantly higher diminutive ADR in the proximal colon.[32] A third quasi RCT was recently completed at a third site. Preliminary analysis showed a significantly higher overall ADR, ADR in the proximal colon, and ADR of proximal < 10 mm adenoma, with the water method.[33] These data suggested that the water method had other beneficial effects.
Table 1.
Beneficial effects of the water method on adenoma detection
As such, in unsedated patients the water method minimizes discomfort during and after colonoscopy and enhances the willingness to repeat the unsedated option. With on-demand sedation the water method increases the proportion completing unsedated colonoscopy and reduces patient recovery time and the burdens on-site and at home. The higher ADR may translate into fewer adenomas being ‘missed’ when patients are examined with the water method.
In conclusion, unsedated colonoscopy certainly appears feasible. It may provide profound benefits, especially when it is integrated into the various options to minimize patient burden in screening. The feasibility is enhanced by the water method.[34] The water method may have other benefits such as increasing adenoma detection. A report on colon cancer in the Kingdom of Saudi Arabia noted that between 1994 and 2003, age-standardized rates for colorectal cancer in the Kingdom of Saudi Arabia almost doubled,[35] as compared to a decline in US. Between 2001 and 2003, while the annual percent change of colorectal cancer incidence in the US showed a decrease in females, the annual percent change in Saudi females showed a rise of 6%. On the other hand, the rising incidence among Saudi males, during the years 1999 to 2003, was significant, with an annual percent change of 20.5%. The projection model suggested that the incidence of colorectal cancer in the Kingdom of Saudi Arabia could increase four-fold in both genders by the year 2030. The authors speculated that the progressively increasing exposure to risk factors, lack of nationwide screening programs, along with aging and growing population, probably explained the rising colorectal cancer rates.[35] There is an urgent needs to make the population aware of the possible relation between diet and colorectal cancer.[35] Improved food supply policy and screening for colorectal cancer are important measures.[35] The latter can be considered for implementation with or without[36] sedation in the Kingdom of Saudi Arabia. We hypothesize that the unsedated colonoscopy combined with the water method may be an attractive option for a newly inaugurated colorectal cancer screening program, and this approach should be prospectively evaluated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wolff WI, Shinya H. Colonofiberoscopy. JAMA. 1971;217:1509–12. [PubMed] [Google Scholar]
- 2.Waye JD. Colonoscopy. Surg Clin N Am. 1972;52:1013–24. doi: 10.1016/s0039-6109(16)39799-7. [DOI] [PubMed] [Google Scholar]
- 3.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162–8. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 4.Leo RA. Unsedated endoscopy: you don’t get a medal for it! South Med J. 2004;97:797–8. doi: 10.1097/01.SMJ.0000136287.03289.3D. [DOI] [PubMed] [Google Scholar]
- 5.Madan A, Minocha A. Who is willing to undergo endoscopy without sedation: patients, nurses, or the physicians? South Med J. 2004;97:800–5. doi: 10.1097/01.SMJ.0000129794.97798.A5. [DOI] [PubMed] [Google Scholar]
- 6.Levenson D. Health quality organization criticizes colonoscopies given without pain medication. Rep Med Guidel Outcomes Res. 2001;12:9-10–12. [PubMed] [Google Scholar]
- 7.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295–300. doi: 10.1007/s10350-004-0940-1. [DOI] [PubMed] [Google Scholar]
- 8.Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Sedation-free colonoscopy. Dis Colon Rectum. 2005;48:855–9. doi: 10.1007/s10350-004-0860-0. [DOI] [PubMed] [Google Scholar]
- 9.Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, et al. Sedation-free colonoscopy using an upper endoscope is tolerable and effective in patients with low body mass index: A prospective randomized study. Am J Gastroenterol. 2006;101:2504–10. doi: 10.1111/j.1572-0241.2006.00790.x. [DOI] [PubMed] [Google Scholar]
- 10.Fennerty B. [Last accessed on 2010 Jan 11]. Available from: http://blogs.jwatch.org/gastroenterology/index.php/sedation-free-colonoscopy why-isnt-it-the standard/2009/0218/
- 11.Ylinen ER, Vehviläinen-Julkunen K, Pietilä AM, Hannila ML, Heikkinen M. Medication-free colonoscopy – factors related to pain and its assessment. J Adv Nurs. 2009;65:2597–607. doi: 10.1111/j.1365-2648.2009.05119.x. [DOI] [PubMed] [Google Scholar]
- 12.Rösch T. A Prospective pilot study to assess technical performance of a new single use colonoscope with inverted sleeve technology. Digestive Disease Week. 2007 Abstract W1344. [Google Scholar]
- 13.Rösch T, Adler A, Pohl H, Wettschureck E, Koch M, Wiedenmann B, et al. A motor-driven single-use colonoscope controlled with a hand-held device: A feasibility study in volunteers. Gastrointest Endosc. 2008;67:1139–46. doi: 10.1016/j.gie.2007.10.065. [DOI] [PubMed] [Google Scholar]
- 14.Leung FW. Thinking outside the box – the case of unsedated screening colonoscopy in the U.S. Gastrointest Endosc. 2009;69:1354–6. doi: 10.1016/j.gie.2008.12.234. [DOI] [PubMed] [Google Scholar]
- 15.Leung FW, Aljebreen AM, Brocchi E, Chang EB, Liao WC, Mizukami T, et al. Sedation risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc. 2010;2:81–9. doi: 10.4253/wjge.v2.i3.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Denberg TD, Melhado TV, Coombes JM, Beaty BL, Berman K, Byers TE, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med. 2005;20:989–95. doi: 10.1111/j.1525-1497.2005.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Patient time requirements for screening colonoscopy. Am J Gastroenterol. 2007;102:2401–10. doi: 10.1111/j.1572-0241.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- 18.Ko CW, Riffle S, Michaels L, Holub J, Shapiro JA, Ciol MA, et al. Serious complications within 30 days of screening and surveillance colonoscopy are uncommon. Clin Gastro Hepatol. 2010;8:166–73. doi: 10.1016/j.cgh.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung FW, Aharonian HS, Guth PH, Chu SK, Nguyen BD, Simpson P. Involvement of trainees in routine unsedated colonoscopy - review of pilot experience. Gastrointest Endosc. 2008;67:718–22. doi: 10.1016/j.gie.2007.11.040. [DOI] [PubMed] [Google Scholar]
- 21.Leung FW. Unsedated colonoscopy introduced as a routine option to ensure access is acceptable to a subgroup of US veterans. Dig Dis Sci. 2008;53:2719–22. doi: 10.1007/s10620-007-0192-8. [DOI] [PubMed] [Google Scholar]
- 22.Leung FW. Promoting informed choice of unsedated colonoscopy - patient-centered care for a subgroup of U.S. veterans. Dig Dis Sci. 2008;53:2955–9. doi: 10.1007/s10620-008-0253-7. [DOI] [PubMed] [Google Scholar]
- 23.Leung FW, Aharonian HS, Guth PH, Jackson G, Chu SK, Nguyen BD, et al. Unsedated colonoscopy: Time to revisit this option? J Fam Pract. 2008;57:E1–4. [PubMed] [Google Scholar]
- 24.Leung FW. Water-related method for performance of colonoscopy. Dig Dis Sci. 2008;53:2847–50. doi: 10.1007/s10620-008-0259-1. [DOI] [PubMed] [Google Scholar]
- 25.Leung JW, Mann S, Leung FW. Option for screening colonoscopy without sedation – a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–31. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 26.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. A pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 27.Mizukami T, Yokoyama A, Imaeda H, Kumai K. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Dig Endosc. 2007;19:43–7. [Google Scholar]
- 28.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–50. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 29.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized controlled trial (RCT) demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 30.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–10. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 31.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective data showing the water method increased adenoma detection rate – a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramirez FC, Leung FW. The water method is associated with higher adenoma detection rate (ADR) – a head-to-head comparative study. Abstract presented at the 2011 DDW meeting. 2011 May 8th and May 10th. [Google Scholar]
- 34.Leung FW, Leung JW, Mann SK, Friedland S, Ramirez FC. Innovation Forum - The water method significantly enhances the outcome of colonoscopy in sedated and unsedated patient. Endoscopy. 2011 doi: 10.1055/s-0030-1256407. [In Press] [DOI] [PubMed] [Google Scholar]
- 35.Ibrahim EM, Zeeneldin AA, El-Khodary TR, Al-Gahmi AM, Bin Sadiq BM. Past, present and future of colorectal cancer in the Kingdom of Saudi Arabia. Saudi J Gastroenterol. 2008;14:178–82. doi: 10.4103/1319-3767.43275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aljebreen AM. The completeness rate of colonoscopy in a cohort of unsedated patients. Saudi J Gastroenterol. 2004;10:150–4. [PubMed] [Google Scholar]


