Abstract
Background:
The spinal metastasis occurs in up to 40% of cancer patient. We compared the Tokuhashi and Tomita scoring systems, two commonly used scoring systems for prognosis in spinal metastases. We also assessed the different variables separately with respect to their value in predicting postsurgical life expectancy. Finally, we suggest criteria for selecting patients for surgery based on the postoperative survival pattern.
Materials and Methods:
We retrospectively analyzed 102 patients who had been operated for metastatic disease of the spine. Predictive scoring was done according to the scoring systems proposed by Tokuhashi and Tomita. Overall survival was assessed using Kaplan–Meier survival analysis. Using the log rank test and Cox regression model we assessed the value of the individual components of each scoring system for predicting survival in these patients.
Result:
The factors that were most significantly associated with survival were the general condition score (Karnofsky Performance Scale) (P=.000, log rank test), metastasis to internal organs (P=.0002 log rank test), and number of extraspinal bone metastases (P=.0058). Type of primary tumor was not found to be significantly associated with survival according to the revised Tokuhashi scoring system (P=.9131, log rank test). Stepwise logistic regression revealed that the Tomita score correlated more closely with survival than the Tokuhashi score.
Conclusion:
The patient's performance status, extent of visceral metastasis, and extent of bone metastases are significant predictors of survival in patients with metastatic disease. Both revised Tokuhashi and Tomita scores were significantly correlated with survival. A revised Tokuhashi score of 7 or more and a Tomita score of 6 or less indicated >50% chance of surviving 6 months postoperatively. We recommend that the Tomita score be used for prognostication in patients who are contemplating surgery, as it is simpler to score and has a higher strength of correlation with survival than the Tokuhashi score.
Keywords: Spine metastasis, prognostic predictors, survival
INTRODUCTION
The skeletal metastasis in spine occurs in up to 40% of cancer patients.1,2 Surgery is indicated for radio-resistant tumors (e.g., sarcomas and lung, colon and renal cell carcinomas), spinal instability, neural compression, deformity, intractable pain, and failure of radiotherapy and for relief of symptoms.3–6 Only those patients who have a reasonable life expectancy after surgery should be exposed to the morbidity associated with surgery. Prediction of life expectancy is difficult due to the diverse range of factors that determine survival in patients with malignancies.7–11 Our study aimed to assess certain variables in patients with spinal metastases requiring surgery with regard to their value in predicting postsurgical life-expectancy. We also compared the revised Tokuhashi and the Tomita scoring systems, two commonly used prognostic scoring systems for spinal metastases and to suggest criteria for selecting patients for surgery based on the postoperative survival pattern.
MATERIALS AND METHODS
We retrospectively analyzed the data of 102 patients who underwent surgery for metastatic spine disease at our institute. There were 54 females (53%) and 48 males (47%). The median age at presentation was 58.5 years. The most common presenting symptoms for patients with spinal metastasis were pain and weakness [Figure 1]. The commonest malignancy was breast cancer (n=25, 24.51%), followed by lung cancer (n=16, 15.69%).
Figure 1.
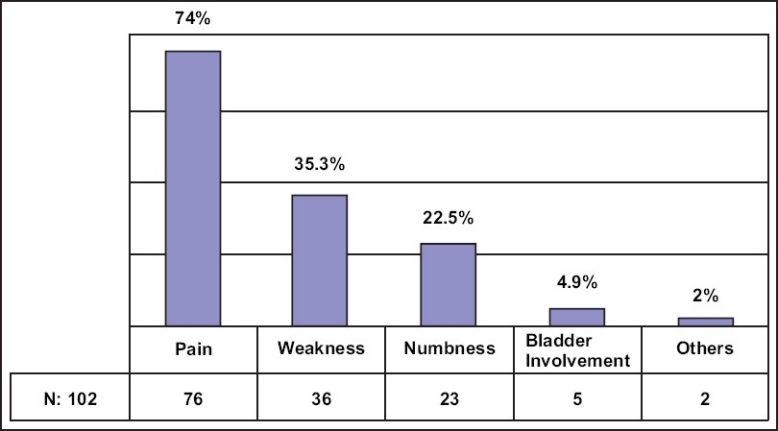
Bar diagram showing presenting symptoms
The indications for surgery included radiological cord compression, impending neurological problem, impending pathological fracture, and intractable pain. Posterior surgery was performed in morbid and high-risk patients. Conservative decompression laminectomy was performed if the spine was deemed stable, for example, when the thoracic spine was affected and there was involvement of less than 50% of the vertebral body. Instrumentation was added when the fracture was deemed unstable and in need of supplementation. Anterior surgery was chosen for the relatively less morbid and low-risk patients.
All the patients were operated at the same institution by a group of four fellowship-trained spine surgeons. Oncology physicians were also involved in the treatment for chemotherapy or radiotherapy, when indicated. All the patients in the study were followed up postoperatively up to death.
Mortality records were retrieved from the National Cancer Registry. Predictive scoring was done based on the scoring systems proposed by Tokuhashi et al.12 and Tomita et al.13 The prognostic values of the Tokuhashi and Tomita scores for predicting 6 month postoperative survival were compared. We also analyzed the effect of the time lapse between diagnosis of primary cancer and presentation of spinal secondary on postoperative life expectancy. Overall survival was analyzed using the Kaplan–Meier method. Individual components of each score were also assessed for significance as prognostic indicators using the log rank test and Cox regression model.
The revised Tokuhashi et al.12 scoring system takes into account those parameters that are expected to be significant in influencing the surgical outcome in patients with spinal metastases. These parameters include the Karnofsky Performance Scale (KPS), presence of extraspinal bone metastasis, number of vertebral levels involved, extension of metastasis to an internal organ, presence of spinal cord palsy, and type of primary tumor. Tomita et al.13 used three factors proven to be significant for prognostication, namely, the grade of malignancy, presence of visceral metastases, and presence of bone metastases. For both scoring systems, each parameter was assigned a weighted score and the total score was obtained by adding the scores of each component.
RESULTS
The thoracic spine was the most common site of involvement in our series of patients [Figure 2].
Figure 2.
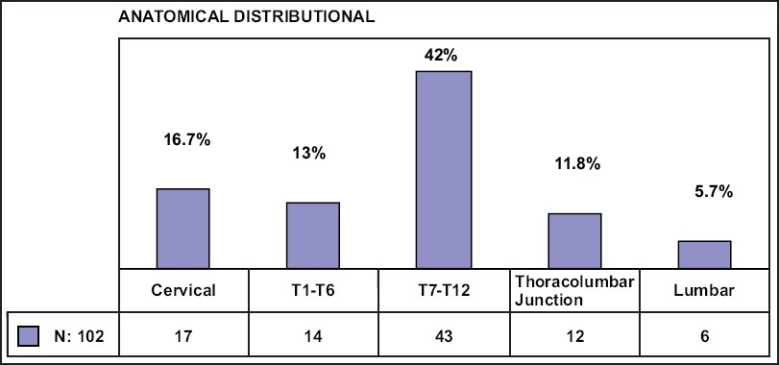
Bar diagram showing distribution of secondaries in the spine
Univariate analysis
Gender: The median survival time for males was 5 months and for female it was 9 months (95% CI: 1 to 9) (P<.05, log rank test).
Age: Patients aged 55 years and below had a median survival of 12 months and those aged above 55 years had a median survival of 9 months (P=.719, log rank test). There was a trend for longer survival in younger patients.
Time to presentation with spinal metastasis: The spinal metastasis was the first indication of the presence of malignant disease in 29 patients. The median postoperative survival in these patients was 4 months (95% CI: 0 to 8.6), while those with known history of cancer and presenting with symptoms of spinal metastasis lived a median period of 7 months (95% CI: 4.23 to 9.77) post surgery. The difference was not statistically significant (P=.296, log rank test).
Analysis of individual components of the revised Tokuhashi scoring system
The most significant factors associated with survival were the general condition score (KPS) (P=.000, log rank test), extent of metastasis to internal organs (P=.0002, log rank test), and number of extraspinal bone metastases (P=.0058, log rank test) [Table 1].
Table 1.
Median survival for metastatic spine tumours (each Tokuhashi component)
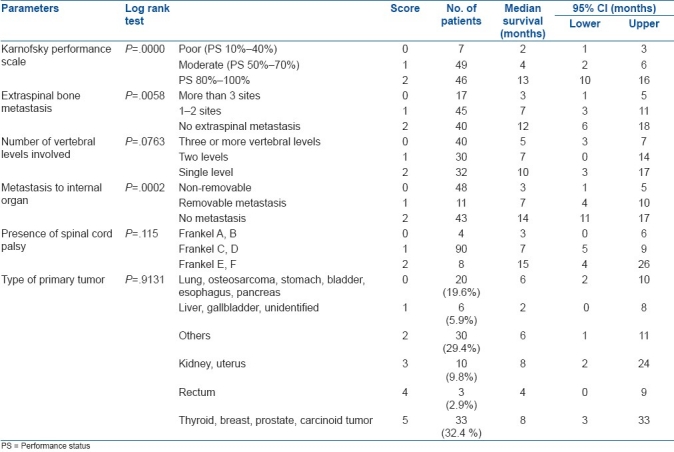
The type of primary cancer did not influence the postsurgical survival according to the revised Tokuhashi scoring system (P=.9131). However, applying the scoring system originally proposed by Tokuhashi et al.,17,14 we found significant correlation between the score and survival (P=.0027, log rank test) [Table 2 and Figure 3].
Table 2.
Median survival for primary cancer against the original Tokuhashi scoring
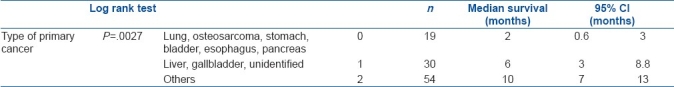
Figure 3.
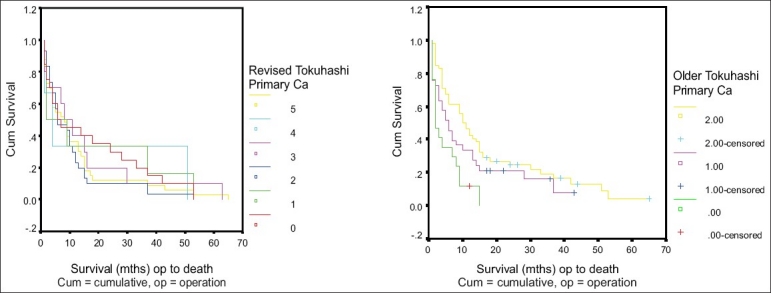
Survival function according to old and new Tokuhashi scoring systems
Analysis of the Tomita et al. scoring system
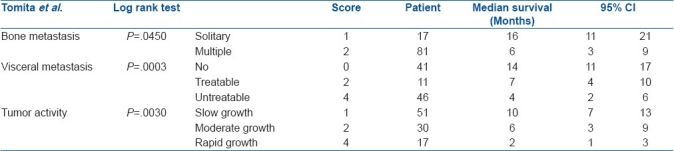
The Tomita score had significant correlation with survival in our series of patients. All three components of the Tomita scoring system were found to have significant influence on survival [Table 3].
Table 3.
Influence of individual components of the Tomita score on survival
Multivariate analysis
We used the Wald (forward stepwise) method to rank the different parameters in the revised Tokuhashi and the Tomita scoring systems to evaluate which correlates most closely with survival. This showed that Tokuhashi ‘general condition,’ Tokuhashi ‘metastasis to internal organs,’ and Tokuhashi (old) ‘type of primary’ were the most accurate predictors of survival (P=.000, P=.002, and P=.001, respectively; chi-square test). Cross tabulation used to correlate strength of equivalent parameters in Tomita scoring system. It had shown that, visceral metastasis and tumor activity in Tomita scoring system closely correlate with Tokuhashi metastasis to internal organ and older Tokuhashi primary tumor type respectively. There was significant correlation between these parameters (Spearman's ratio: –1.000) [Figure 4].
Figure 4.
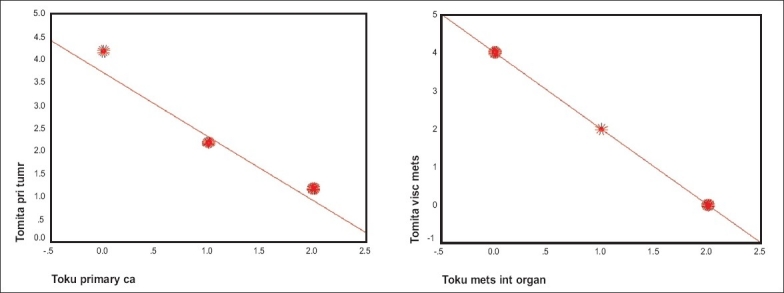
Cross-tabulation of Tomita and Tokuhashi metastasis
To summarize, the parameters that influenced survival were: Tokuhashi general condition, Tokuhashi metastasis to internal organs, Tokuhashi (old) type of primary cancer, Tomita visceral metastasis, Tomita tumor activity
Parameters that not influenced survivals: Age, sex, Tokuhashi (revised) type of primary tumor, spinal cord palsy, Tokuhashi vertebral metastasis, Tokuhashi bone metastasis, Tomita bone metastasis
Six-month survival
The total Tokuhashi score can range from 0–15. We grouped the scores in our study into five groups and examined the likelihood of 6-month survival in each group [Table 4]. There is significant difference in survival among the five Tokuhashi score groups (P=.0038, log rank test), with higher median survival in the groups with higher scores. The median survival time (and the 95% CI) are summarized in the following tables.
Table 4.
Revised Tokuhashi scores and the likelihood of 6-month survival
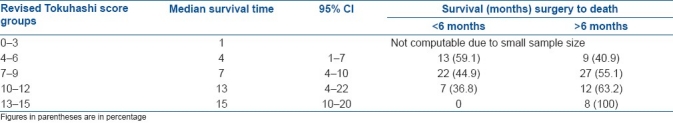
The 6-month survival rate was 55.1% for the group with score 7–9, 63.2% for those with score 10–12, and 100% for those with score 13–15; these differences were statistically significant (P<.05, log rank test).
There is significant difference in survival between the four Tomita score groups (P<.00005, log rank test). Lower scores were correlated with higher median survival [Table 5].
Table 5.
Tomita scores and the likelihood of 6-month survival
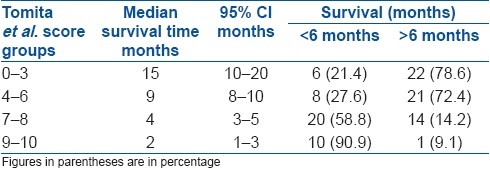
With a Tokuhashi score of 7 or more and a Tomita score of 6 or less there is more than 50% chance that the patient will survive beyond 6 months after surgery. The assurance that there is a good chance of survival after surgery can be useful for surgeons as it will give them the confidence to proceed with surgery. This knowledge will also be useful when counseling patients on various treatment options.
Survival logistic analysis at 6 months: Tomita vs Tokuhashi score
Stepwise logistic regression analysis was used to evaluate the strength of correlation between the Tokuhashi and Tomita scores and 3-month and 6-month survival. The Tomita score (P=.001) was shown to be a significant independent predictor for 3-month as well as 6-month survival. The Tokuhashi score was not used as it was not a significant predictor in comparison with the Tomita score for 3- and 6-month survival.
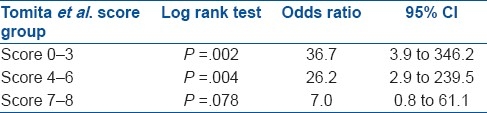
We examined survival in the different score groups, with the Tomita 9–10 score group (i.e., poorest prognosis) as the reference group; the 6-month survival in the groups is shown in the Table 6.
Table 6.
Odds of 6-month survival according to Tomita score (with score group 9–10 as reference group)
DISCUSSION
In patients with metastatic spinal tumors surgery can provide symptomatic relief of pain and nerve palsy and improve quality of life.7,13–15 However, because of the morbidity associated with surgery and the recuperation period required, patients considered for surgical intervention should have a reasonable life-expectancy (of at least 3–6 months) postoperatively.16
According to the revised Tokuhashi preoperative prognostic scoring system, total scores of 0–8, 9–11, and 12–15 predict life-expectancy of <6 months, >6 months, and ≥1 year, respectively. Tokuhashi et al. found that with this scoring system the survival period after surgery could be predicted consistently. The accuracy rate was 86.4% in a prospective series of 118 patients and 82.5% in a retrospective series of 246 patients.12
Tomita et al.13 used three factors for estimating survival prognosis: the grade of malignancy, extent of visceral metastases, and extent of bone metastases. Each factor was assigned a weighted score, which was determined retrospectively. Visceral metastases have twice the weightage as bony metastases, reflecting the relatively stronger correlation of the former with prognosis (which was apparent in our study also). Tomita et al. applied this scoring system prospectively to a series of 61 patients with spinal metastases between 1993 and 1996. In 43 of 52 patients (83%) who had been treated surgically they achieved local control for more than 80% of the survival period (the life span of the patient). The results suggested that this classification was simple to use, had prognostic value, and was reliably accurate in the management of spinal metastases.
The KPS has been used in oncology since 1948 to assess performance status of patients.19 It is generally regarded as the gold standard measurement of performance status in cancer patients.17,18 Our study showed that the KPS had the highest correlation with survival (P=.000, log rank test). Being a general score, it takes into account many comorbidities that determine survival. There is higher median survival time for the female population in our study [P<.05, log rank test]. Of females with breast cancer, 93% had KPS of more than 60%.
The efficacy and accuracy of the Tokuhashi and Tomita scoring systems has been studied by many authors in the past in different population groups. Grainger et al.20 retrospectively reviewed 169 patients operated for spinal metastasis and calculated prognostic scores according to the systems of Tokuhashi and Tomita. They found that patients with Tokuhashi scores of 9–12 had 50% survival of 23 months compared to 5 months and 2 months survival in those with scores of 5–8 and 1–4, respectively (P<.05). The Tomita scoring method showed a similar trend, with 50% survival of 15 and 5 months for predicted long and medium term groups (P<.05). The authors concluded that both systems are potentially useful when deciding the suitability for surgery of patients with metastatic spinal disease. They had concluded that the Tomita system was less sensitive for early mortality.
Ulmar et al.21 retrospectively analyzed 37 patients surgically treated for vertebral metastases secondary to renal cancer. The Tokuhashi and Tomita scores were calculated for each patient. They found that the Tokuhashi score was very reliable for the estimation of life-expectancy of renal cancer patients with vertebral metastases, with a statistically high significance. However, they found no correlation between predicted and real survival with the Tomita score.
Zeng et al.,22 in their retrospective review, used the revised Tokuhashi system to score 447 patients operated for spinal metastases. The relationship between survival time and the Tokuhashi score was analyzed. They concluded that the Tokuhashi score was positively correlated with survival time (r=0.833; P<.001). Thus, with a revised Tokuhashi score of 12–15 points, surgery would be a good option for extending lifespan in a patient with a solitary spinal metastasis of a slow-growth primary tumor.
Katagiri et al.23 did a multivariate analysis of data from 350 patients operated for spinal metastases. They identified five significant prognostic factors for survival, namely, the site of the primary lesion, the performance status, the presence of visceral or cerebral metastases, any previous chemotherapy, and presence of multiple skeletal metastases. The score for each significant factor was derived from the corresponding estimated regression coefficients (natural logarithm of the hazard ratio). The prognostic score was calculated by adding up the scores for the individual factors. The rate of survival was 31% at 6 months and 11% at 1 year for patients with a prognostic score of 6 or more. By contrast, patients with a prognostic score of 2 or less had a rate of survival of 98% at 6 months and 89% at 1 year. This scoring system can be used to determine the optimal treatment for patients with pathological fractures or epidural compression.
Our study analyzed all six components of the Tokuhashi scoring system and found that the three parameters that significantly influence survival without controlling the other variables were the individual performance score, extent of metastasis to visceral organs, and extent of extraspinal bone metastases.
The type of primary tumor was not found to be statistically significant in the revised Tokuhashi scoring system, which had five grades (P=.9131 log rank), but it was found to be significant with the original scoring system where the score was categorized to three grades (P=.027). This may be explained by the lack of power of the study when the categories were expanded from three possibilities to six in the revised score.
Similar to previous studies that have proved the efficacy of both the Tokuhashi and the Tomita scoring systems, we too found that both scores correlated well with survival. Stepwise logistic regression for 3 and 6 months survival revealed that the Tomita score correlated more closely with survival than the Tokuhashi score, which is in contrast to findings of the earlier studies. The Tokuhashi scoring system takes into account parameters that do not significantly influence survival (e.g., presence of spinal cord palsy and number of vertebral levels involved) and this may confound the final score. Satoshi et al. found that, in patients with lung cancer, among the components of the Tokuhashi score only the patient's performance status correlated with survival, and that the Tokuhashi score as a whole did not correlate with survival.24
CONCLUSION
The individual performance status, extent of visceral metastasis, extent of bone metastases, and tumor activity are significant predictors of survival in patients with metastatic disease of the spine and requiring surgery. Both the revised Tokuhashi score and the Tomita score were significantly correlated with survival. A revised Tokuhashi score of 7 or more and a Tomita score of 6 or less indicated more than 50% chance of surviving 6 months postoperatively. We recommend that the Tomita score be used for prognostication in patients who are contemplating surgery as it is simpler to score and has a higher strength of correlation with survival than the Tokuhashi score.
ACKNOWLEDGEMENT
Stephanie Fook, Departments of Statistics, Singapore General Hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Abrams HL, Spiro R, Goldstein N. Metastases in carcinoma: Analysis of 1000 autopsied cases. Cancer. 1950;3:74–85. doi: 10.1002/1097-0142(1950)3:1<74::aid-cncr2820030111>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 2.Fornasier VL, Horne JG. Metastases to the vertebral column. Cancer. 1975;36:590–4. doi: 10.1002/1097-0142(197508)36:2<590::aid-cncr2820360240>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 3.Gerszten PC, Welch WC. Current surgical management of metastatic spinal disease. Oncology (Williston Park) 2000;14:1013–24. [PubMed] [Google Scholar]
- 4.Hatrick NC, Lucas JD, Timothy AR, Smith MA. The surgical treatment of metastatic disease of the spine. Radiother Oncol. 2000;56:335–9. doi: 10.1016/s0167-8140(00)00199-7. [DOI] [PubMed] [Google Scholar]
- 5.Klimo P, Jr, Kestle JR, Schmidt MH. Clinical trials and evidence-based medicine for metastatic spine disease. Neurosurg Clin N Am. 2004;15:549–64. doi: 10.1016/j.nec.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Maranzano E, Trippa F, Chirico L, Basagni ML, Rossi R. Management of metastatic spinal cord compression. Tumori. 2003;89:469–71. doi: 10.1177/030089160308900502. [DOI] [PubMed] [Google Scholar]
- 7.Tokuhashi Y, Kawano H, Ohsaka S, Matsuzaki H, Toriyama S. A scoring system for preoperative evaluation of the prognosis of metastatic spine tumor prognosis. J Jpn Orthop Assoc. 1989;63:482–9. [PubMed] [Google Scholar]
- 8.Karnofsky DA. Clinical evaluation of anticancer drugs: Cancer chemotherapy. GANN Monogr. 1967;2:223–31. [Google Scholar]
- 9.Citrin DL, Hougen C, Zweibei W, Schlise S, Pruitt B, Ershler W. The use of serial bone scans inassessing response of bone metastases to systemic treatment. Cancer. 1981;47:680–5. doi: 10.1002/1097-0142(19810215)47:4<680::aid-cncr2820470410>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 10.Swenerton KD, Legha SS, Smith T, Hortobagyi GN, Gehan EA, Yap HY. Prognostic factors in metastaticbreast cancer treated with combination chemotherapy. Cancer Res. 1979;39:1552–62. [PubMed] [Google Scholar]
- 11.Yamashita K, Yonenobu S, Fuji T. Staging of metastatic spinal tumor. Rinsho Seikei Geka. 1986;21:445–50. [Google Scholar]
- 12.Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine. 2005;30:2186–91. doi: 10.1097/01.brs.0000180401.06919.a5. [DOI] [PubMed] [Google Scholar]
- 13.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine. 2001;26:298–306. doi: 10.1097/00007632-200102010-00016. [DOI] [PubMed] [Google Scholar]
- 14.Tokuhashi, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005;30:2186–91. doi: 10.1097/01.brs.0000180401.06919.a5. [DOI] [PubMed] [Google Scholar]
- 15.Enkaoua EA, Doursounian L, Chatellier G, Mabesoone F, Aimard T, Saillant G. Vertebral metastases: A critical appreciation of the preoperative prognostic Tokuhashi score in a series of 71 cases. Spine. 1987;22:2293–8. doi: 10.1097/00007632-199710010-00020. [DOI] [PubMed] [Google Scholar]
- 16.Walker MP, Yaszemski MJ, Kim CW, Talac R, Currier BL. Metastatic disease of the spine: Evaluation and treatment. Clin Orthop Relat Res. 2003;415:S165–75. doi: 10.1097/01.blo.0000092977.12414.f9. [DOI] [PubMed] [Google Scholar]
- 17.Kaasa T, Wessel J. The Edmonton Functional Assessment Tool: Further development and validation for use in palliative care. J Palliat Care. 2001;17:5–11. [PubMed] [Google Scholar]
- 18.Nikoletti S, Porock D, Kristjanson LJ, Medigovich K, Pedler P, Smith M. Performance status assessment in home hospice patients using a modified form of the Karnofsky Performance Status scale. J Palliat Med. 2000;3:301–11. doi: 10.1089/jpm.2000.3.301. [DOI] [PubMed] [Google Scholar]
- 19.Karnofsky D, Abelmann W, Craver L, Burchenal J. The use of nitrogen mustard in the palliative treatment of cancer. Cancer. 1948;1:634–56. [Google Scholar]
- 20.Grainger M, Stirling A, Marks D. validation of Tokuhashi and Tomita prognostic scoring systems in spinal metastases. JBJS(Br) 2004;86-B(SUPP_III):293. [Google Scholar]
- 21.Ulmar B, Naumann U, Catalkaya S, Muche R, Cakir B, Schmidt R, et al. Prognosis scores of Tokuhashi and Tomita for patients with spinal metastases of renal cancer. Ann Surg Oncol. 2007;14:998–1004. doi: 10.1245/s10434-006-9000-5. [DOI] [PubMed] [Google Scholar]
- 22.Zeng JC, Song YM, Liu H, Gong Q, Li T, Liu LM, et al. The predictive value of the Tokuhashi revised scoring system for the survival time of patients with spinal metastases. Sichuan Da Xue Xue Bao Yi Xue Ban. 2007;38:488–91. [PubMed] [Google Scholar]
- 23.Katagiri H, Takahashi M, Wakai K, Sugiura H, Kataoka T, Nakanishi K. Prognostic factors and a scoring system for patients with skeletal metastasis. J Bone Joint Surg Br. 2005;87:698–703. doi: 10.1302/0301-620X.87B5.15185. [DOI] [PubMed] [Google Scholar]
- 24.Ogihara S, Seichi A, Hozumi T, Oka H, Ieki R, Nakamura K, et al. Prognostic factors for patients with spinal metastases from lung cancer. Spine. 2006;31:1585–90. doi: 10.1097/01.brs.0000222146.91398.c9. [DOI] [PubMed] [Google Scholar]


