Abstract
Background:
Anterior cruciate ligament (ACL) avulsion fracture is commonly associated with knee injuries and its management is controversial ranging from conservative treatment to arthroscopic fixation. The aim of our study was to assess the clinical and radiological results of arthroscopic staple fixation in the management of ACL avulsion fractures.
Materials and Methods:
Twenty-two patients (17 males and 5 females) who underwent arthroscopic staple fixation for displaced ACL avulsion fractures were analysed. The mean age was 32.2 years (15-55 years) with a mean followup of 21 months (6-36 months). All patients were assessed clinically by calculating their Lysholm and International Knee Documentation Committee (IKDC) scores and the radiological union was assessed in the followup radiographs.
Results:
The mean Lysholm score was 95.4(83-100) and the mean IKDC score was 91.1(77-100) at the final followup. In 20 patients anterior drawer's test was negative at the end of final followup while two patients had grade I laxity. Associated knee injuries were found in seven cases. The final outcome was not greatly influenced by the presence of associated injuries when treated simultaneously. At final followup all the patients were able to return to their pre-injury occupation
Conclusion:
Arthroscopic staple fixation is a safe and reliable method for producing clinical and radiological outcome in displaced ACL avulsion fractures.
Keywords: ACL avulsion, arthroscopy, staple
INTRODUCTION
Anterior cruciate ligament (ACL) avulsion fractures contribute most of the injuries around the knee joint and result in significant disability if left untreated. They are caused by forceful hyperextension of the knee or by a direct blow over distal end of femur with the knee flexed. In the past, non-operative method of treatment in the form of immobilization of the knee in full extension or in 20° of flexion1 the position in which ACL is most relaxed was followed. However, patients were immobilized for 4 to 6 weeks. Reduction is not achieved by manipulating the knee into hyperextension with the patient anesthetized, which can neither dislodge nor approximate the fragment to its bed1 since the fractured fragment is not between the articulating surface of tibia and femur, but lies in an empty non-articulating area of the joint. Open reduction and internal fixation of tibial spine fractures carries a risk of knee stiffness and infection.2 Arthroscopic fixation of ACL overcomes the complications of long-term immobilization, such as knee stiffness and DVT.
The aim of our study was to evaluate the clinical and radiological results of ACL avulsion fractures treated by arthroscopic staple fixation technique.
MATERIALS AND METHODS
Twenty-two patients (17 males and 5 females) who underwent arthroscopic staple fixation of displaced ACL avulsion fractures from January 2007 to June 2009 and had completed the minimum followup of six months and were available for final assessment were included in our study. The mean age of the patients was 32.2 years (range 15 to 55 years). The mode of injury was road traffic accident in 19 patients and secondary to twisting injury in 3 patients.
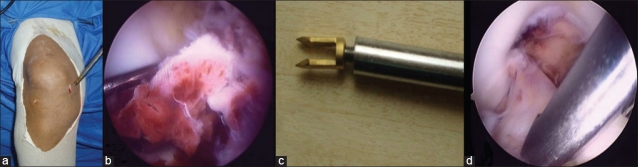
All patients were assessed in the casualty by a careful physical examination to rule out associated injuries and by a plain radiograph of the knee joint [Figure 1]. Thirteen patients had type II injury of the ACL (anterior third displacement of the avulsed fragment) and nine patients had type III injury of the ACL where the avulsed fragment was displaced completely. Patients with associated ipsilateral knee injuries were included, whereas patients with polytrauma and contra-lateral limb injuries were excluded from the analysis.
Figure 1.
Plain radiograph anteroposterior (a) and lateral view (b) of right knee of a 28 year old man with ACL avulsion fracture
Four patients with severe communition of the avulsed fragment underwent MRI of the knee to assess the size of the largest bony fragment attached to the ACL that might allow fixation with a staple and also to assess the integrity of the ACL fibers. Associated ipsilateral knee injuries were found in seven patients.
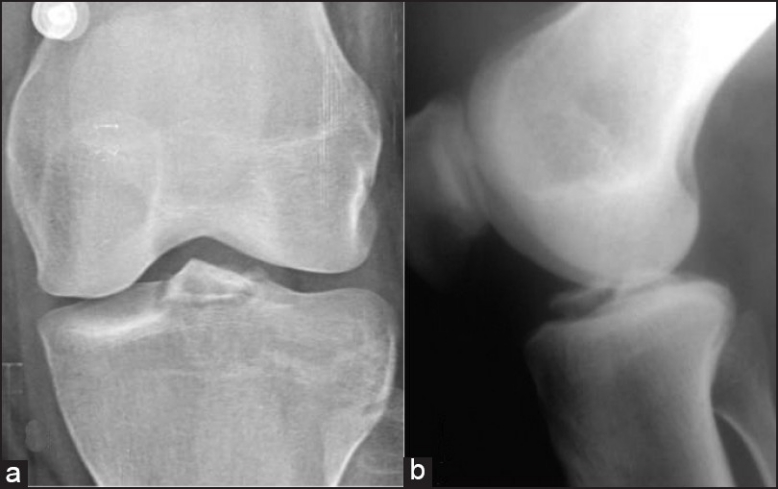
All patients underwent arthroscopic staple fixation. Under tourniquet control knee joint was examined by standard medial and lateral para patellar arthroscopic portals. The medial portal was higher than the lateral portal and in a more vertical position to facilitate the staple fixation [Figure 2]. Sometimes an additional higher lateral portal was needed to fix the fragment from lateral side. Thorough wash was given to drain the hematoma and the avulsed ACL fragment was visualized [Figure 2b] and it was made sure that there was no meniscal interposition. The titanium staple [Figure 2c] is of 2 centimeters length and has two “v”-shaped fangs. It was threaded to the introducer and inserted through the high medial portal and placed over the avulsed fragment. The fragment was reduced to its insertion bed arthroscopically by utilizing the staple as a joystick [Figure 2d]. Then the staple was driven through the avulsed fragment and into the tibial plateau by hammering on to the introducer gently. Then the introducer was unscrewed from the staple head. The avulsed fragment was fixed with either one or two staples depending on the size of the fragment [Figure 3]. In comminuted fractures, the largest fragment containing most of the ACL fibers was fixed with the staple and the remaining loose small fragments were removed, as it might lead to locking resulting in a fixed flexion deformity later. Intra operatively, the stability of the fixation was checked by pulling the ACL with a probe and full range of motion of the knee was performed.
Figure 2.
(a) Arthroscopic high medial portal used to fix ACL avulsion fracture. (b) Arthroscopic view of ACL avulsion fracture. (c) Titanium staple used to fix ACL avulsion fracture (d) Staple aiding in reduction of the avulsed fragment.
Figure 3.
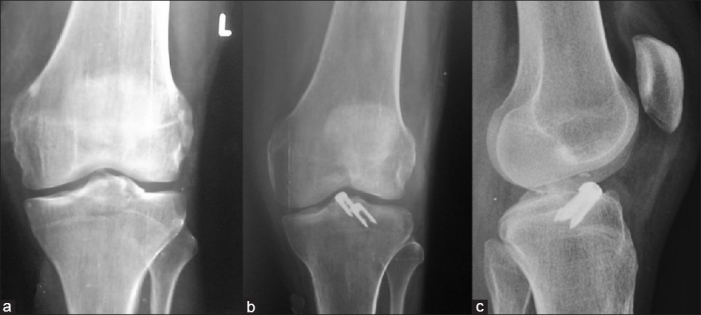
(a) Anteroposterior X-ray of left knee of a 39 years old male shows large ACL avulsion; (b) postoperative anteroposterior and (c) lateral view of the same patient shows ACL fixed with 2 staples
The associated ipsilateral injuries of the knee were managed simultaneously. In our series, seven patients had associated knee injuries. Three patients had tibial condyle fractures which were fixed percutaneously with screws before ACL avulsion fracture fixation for better purchase of the staple [Figure 4]. Two patients had meniscal injuries which were treated by partial menisectomies and two patients had PCL avulsion fractures which were fixed with cancellous screws by a posterior approach [Figure 5].
Figure 4.
Anteroposterior (a) and lateral (b) radiograph of the right knee of a 35 year old female shows ACL avulsion and posterior tibial condyle fracture fixed respectively with staples (c,d) and percutaneous cancellous screws
Figure 5(a-c).
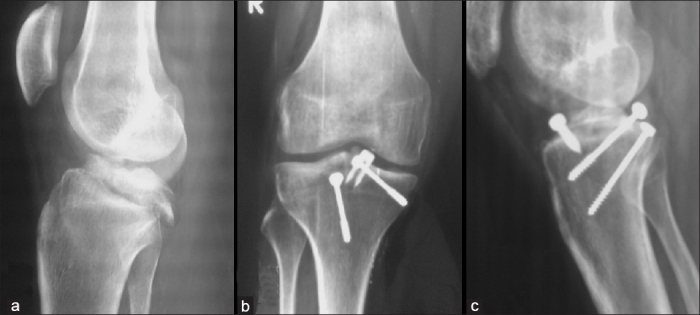
ACL and PCL avulsion fracture of the right knee in a 47 year old male fixed with screws for PCL and staples for ACL
All patients were mobilized partial weight bearing for the first 4 weeks with a knee brace followed by full weight bearing along with knee bending exercises from 4 weeks postoperatively. Then an active rehabilitation program was started to gradually attain the full range of movements. Patients were evaluated functionally by examining for clinical signs of laxity and assessed by the Lysholm score and the International Knee Documentation Committee (IKDC) score at end of third and sixth month and at final followup. The radiological healing was assessed by followup radiographs.
RESULTS
Twenty-two patients were analyzed post-operatively and followed up for a mean period of 21 months (range 6-36 months). Complete range of motion of the knee joint at final follow up was achieved in 20 patients. Two patients had a fixed flexion deformity of 5° and restricted 15° terminal flexion. At the end of final followup, Anterior drawer's test was negative in 20 patients, while 2 patients revealed grade I laxity. None of the patients had symptoms of giving away of the knee joint on daily routine activities and all patients returned to their pre-injury activity level. There were no surgical site infections in our series. The mean IKDC score was 91.1 (range 77-100) and the mean Lysholm score was 95.4 (range 83-100). The mean time to union was 8 weeks (range 6-10 weeks) radiologically and all cases united.
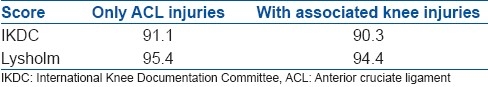
In our series double staple fixation was done for large avulsed fragment in 7 patients and single staple fixation in 15 patients with small fragment [Figure 3]. There was no difference in the functional outcome of the patients at final followup based on the number of the staples. Patients with associated injuries returned back to their pre-injury occupation at time of final followup and the Lysholm and IKDC scores of these patients were comparable to those of the other patients with only ACL injuries [Table 1].
Table 1.
IKDC and Lysholm scores in only ACL injuries and ACL with associated knee injuries
One patient had back out of one staple 8 months after surgery in which two staples were used [Figure 6]. The backed out staple was removed arthroscopically and the patient was able to return to his pre-injury activity level. Routine removal of the staple is not advocated. However we recommend removal of the staple if there is lossening or backing out radiologically. Otherwise the backed out staple can cause impingement and articular cartilage damage.
Figure 6.

Anteroposterior X-ray of the right knee showing back out of the staple in a 26 year old male
DISCUSSION
The ACL is attached on the tibia to a wide depressed area in front of and lateral to the anterior tibial spine.3 ACL avulsion fractures account for a majority of knee injuries when compared to PCL avulsions. Avulsion fractures were classified into three types by Meyers and McKeever1 as Type I-undisplaced, Type II-anterior third displacement, and Type III completely displaced. Type I injuries are best treated conservatively.
Treatment of displaced fractures is controversial and multiple methods have been described. Different types of fixation for ACL avulsions include cancellous screws, staples, sutures, K wires to bio- absorbable suture anchors.12 The conservative method carries its complications of prolonged immobilization, knee stiffness, and residual instability. Open methods of fixation produce variable degree of knee stiffness due to the extensive dissection done and require long period of immobilization. Arthroscopic staple fixations overcomes these drawbacks.
ACL avulsions were more common in the age group of 15-30 years (n=12) in our series. Kendall et al found the incidence of injury in adults higher than that in children.4 Song EK et al found that there is no significant difference between adults and children in terms of final range of motion in avulsion fractures that were treated surgically.5 Wilfinger et al6 showed a good outcome at 1 year follow up in his study of 38 pediatric cases managed conservatively; however, there are no studies regarding conservative management in adults.
Huang et al7 reported good results with high functional scores with arthroscopic suture fixation. However, technically it is a difficult procedure when compared to staple fixation. Mc Lennan in his series showed that lack of extension, persistence of ligamentous instability, and quadriceps wasting are side effects seen in patients treated by arthroscopic reduction and percutaneous pin fixation of ACL avulsions when compared to arthroscopic staple fixation8. Ahn et al9 showed that arthroscopic reduction with modified pull-out suturing technique in displaced tibial spine ACL avulsion fractures showed excellent union rate for both acute and chronic cases. In our series, five patients were operated after 72 hours and they had slightly lower scores when compared to others. However, it does not affect the final outcome.
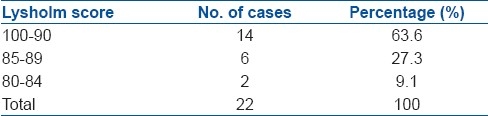
In our study the mean IKDC score was 91.1(77 to 100) and the mean Lysholm score was 95.4 (83 to 100) which is comparable to other series in the literature [Tables 2 and 3]. The mean IKDC score in the seven patients with associated injuries was 90.3 which was comparable to the total series mean score of 91.1 and a mean Lysholm score of 94.4 which was comparable to the total series mean score of 95.4 [Table 1] predicting that presence of associated knee injuries when treated simultaneously does not affect the final outcome of the ACL surgery.
Table 2.
IKDC score
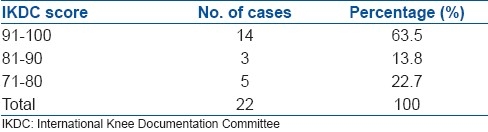
Table 3.
Lysholm score
No difference in the functional outcome was found of the patients at a final follow up based on the number of the staples used to fix the fragment and indirectly the size of the avulsed fragment.
Song et al5 using sutures and anchors for ACL avulsion obtained a Lysholm score of 89.5. Ahn et al9 produced a result of 95.6 Lysholm score using suture fixation. Robert et al published a Lysholm score of 94.2 using screws and suture alone. A satisfactory Lysholm score of 95.4 was obtained in our series with arthroscopic staple fixation. Seon et al10 compared screw and suture fixation and reported a Lysholm score of 91.7 and 92.7, respectively. In Medler series, avulsion fractures were fixed using ACL tibial drill guide and arthroscopy and have had good results.11 Good results were reported with bio absorbable suture anchors by Kim et al12 in five cases.
Arthroscopic staple fixation facilitates earlier knee mobilization decreasing the chances of knee stiffness when compared to open techniques of fixation. It also reduces the surgical time and the length of hospitalization. Arthroscopic staple fixation is a technically simple procedure when compared to the screw fixation or suturing techniques. Staple fixation obviates the need for drilling or tapping and also the difficulties in insertion of long screws can be avoided. The rare chances of the screw slipping from the driver during introduction and falling into the joint cavity do exist, whereas the staple pre-threaded to the driver avoids such problems. The suture techniques described in the literature require surgical expertise in performing them and are difficult when compared to the staple fixation which can be easily reproduced.
Common problems encountered in this technique are communition of the avulsed fragment, interposition of menisci or the transverse inter-meniscal ligament between fracture fragments, and intra-substance ACL tear combined with an avulsion fracture.
When there is a severe communition of the fragment, ACL fibers can be detached from the fragments and the staples might not have a good purchase and may result in early back out of the staple. In such special circumstances, ACL reconstruction at later date is the preferred treatment of choice. Also, in the cases where avulsion of ACL is accompanied with ACL mid-substance tear, ACL reconstruction should be planned. When avulsion fracture is combined with a partial tear of ACL, the largest fragment can be fixed by a staple and the torn fibers can be debrided preventing the need for ACL reconstruction. This has been shown in where the two large avulsed fragments were fixed with staples and the remaining intact fibers of ACL were preserved. These problems are circumvented by a preoperative MRI. So based on the study results we are now routinely taking preoperative MRI in all cases of ACL avulsions to rule out other ligament injuries, meniscal damage, and to document the integrity of the ACL fibers.
All patients obtained radiological union in a mean period of 8 weeks and all patients returned to their pre-injury activity level at the final follow up. Based on our study, arthroscopic fixation is a preferred method to treat displaced ACL avulsion fractures when compared to the previous methods of open fixation in terms of earlier mobilization, avoiding knee stiffness and residual instability. Among the various arthroscopic techniques, staple fixation is a simple and effective procedure that when applied aptly gives good clinical and functional outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Meyers MH, McKeever FM. Fracture of the Intercondylar Eminence of the tibia. J Bone Joint Surg Am. 1959;41:209–22. [PubMed] [Google Scholar]
- 2.Rademakers MV, Kerkhoffs GM, Kager J, Goslings JC, Marti RK, Raaymakers EL. Tibial spine fractures- a long-term followup study of open reduction and internal fixation. J Orthop Trauma. 2009;23:203–7. doi: 10.1097/BOT.0b013e31819b08ba. [DOI] [PubMed] [Google Scholar]
- 3.Zaricznyj B. Avulsion fracture of the tibial eminence: Treatment by open reduction and pinning. J Bone Joint Surg Am. 1977;59:1111–4. [PubMed] [Google Scholar]
- 4.Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children-A review of 31 cases. J Bone Joint Surg Br. 1992;74:848–52. doi: 10.1302/0301-620X.74B6.1447245. [DOI] [PubMed] [Google Scholar]
- 5.Song EK, Seon JK, Park SJ, Yoon TR. Clinical outcome of avulsion fracture of the anterior cruciate ligament between children and adults. J Pediatr Orthop B. 2009;18:335–8. doi: 10.1097/BPB.0b013e32832f06bd. [DOI] [PubMed] [Google Scholar]
- 6.Wilfinger C, Castellani C, Raith J, Pilhatsch A, Höllwarth ME, Weinberg AM. Nonoperative treatment of tibial spine fractures in children-38 patients with a minimum follow-up of 1 year. J Orthop Trauma. 2009;23:519–24. doi: 10.1097/BOT.0b013e3181a13fe4. [DOI] [PubMed] [Google Scholar]
- 7.Huang TW, Hsu KY, Cheng CY, Chen LH, Wang CJ, Chan YS, et al. Arthroscopic suture fixation of tibial eminence avulsion fractures (36 cases) Arthroscopy. 2008;24:1232–8. doi: 10.1016/j.arthro.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 8.McLennan JG. The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br. 1982;64:477–80. doi: 10.1302/0301-620X.64B4.6896515. [DOI] [PubMed] [Google Scholar]
- 9.Ahn JH, Yoo JC. Clinical outcome of arthroscopic reduction and suture for displaced acute and chronic tibial spine fractures. Knee Surg Sports Traumatol Arthrosc. 2005;13:116–21. doi: 10.1007/s00167-004-0540-6. [DOI] [PubMed] [Google Scholar]
- 10.Seon JK, Park SJ, Lee KB, Gadikota HR, Kozanek M, Oh LS, et al. A clinical comparison of screw and suture fixation of anterior cruciate ligament tibial avulsion fractures. Am J Sports Med. 2009;37:2334–9. doi: 10.1177/0363546509341031. [DOI] [PubMed] [Google Scholar]
- 11.Medler RG, Jansson KA. Arthroscopic treatment of fractures of the tibial spine. Arthroscopy. 1994;10:292–5. doi: 10.1016/s0749-8063(05)80114-8. [DOI] [PubMed] [Google Scholar]
- 12.In Y, Kim JM, Woo YK, Choi NY, Moon CW, Kim MW. Arthroscopic fixation of ACL avulsion fractures using bio absorbable suture anchors. Knee Surg Sports Traumatol Arthrosc. 2008;16:286–9. doi: 10.1007/s00167-007-0466-x. [DOI] [PubMed] [Google Scholar]