Abstract
In the field of periodontology and implantology, assessment of the condition of teeth and surrounding alveolar bone depends largely on two-dimensional imaging modalities such as conventional and digital radiography. Though these modalities are very useful and have less radiation exposure, they still cannot determine a three-dimensional (3D) architecture of osseous defects. Hence, an imaging modality which would give an undistorted 3D vision of a tooth and surrounding structures is essential to improve the diagnostic potential. Cone-beam computed tomography (CBCT) provides 3D images that facilitate the transition of dental imaging from initial diagnosis to image guidance throughout the treatment phase. This technology offers increased precision, lower doses, and lower costs when compared with medical fan-beam CT. This review discusses all the finer details of CBCT which not only reveals 3D architecture of the periodontium but also helps to reconstruct it.
Keywords: 3-D imaging, cone beam computed tomography, periodontal applications
INTRODUCTION
In the field of periodontology, assessment of the condition of teeth and surrounding alveolar bone depends largely on traditional two-dimensional imaging modalities such as conventional radiography and digital radiography. Though these modalities are very useful and have less radiation exposure, they still cannot determine a three-dimensional (3D) architecture of osseous defects. Hence, an imaging modality which would give an undistorted 3D vision of a tooth and surrounding structures is essential to improve the diagnostic potential. A well diagnosed periodontal lesion warrants an appropriate treatment.
In the medical field, the 3D imaging using computed tomography (CT) has been available now for many years, but in the dental specialty, its application is restricted to the use in cases of maxillofacial trauma and diagnosis of head and neck diseases. Routine use of CT in dentistry is not accepted due to its cost, excessive radiation, and general practicality. In recent years, a new technology of cone-beam CT (CBCT) for acquiring 3D images of oral structures is now available to the dental clinics and hospitals. It is cheaper than CT, less bulky and generates low dosages of X-radiations. The innovative CBCT machines [Figure 1] designed for head and neck imaging are comparable in size with an orthopantomograph.
Figure 1.
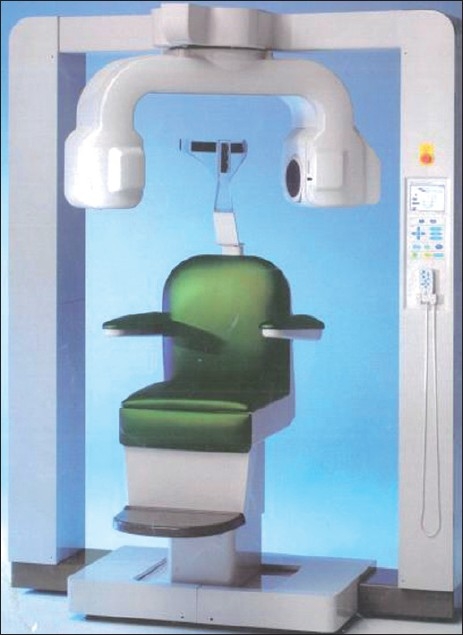
A CBCT machine designed for head and neck imaging
CBCT provides rapid volumetric image acquisition taken at different points in time that are similar in geometry and contrast, making it possible to evaluate differences occurring in the fourth dimension time. In its various dental applications, images of jaws and teeth can be visualized accurately with excellent resolution, can be restructured three dimensionally, and can be viewed from any angle [Figure 2]. Most significantly, patient radiation dose is five times lower than normal CT.
Figure 2.
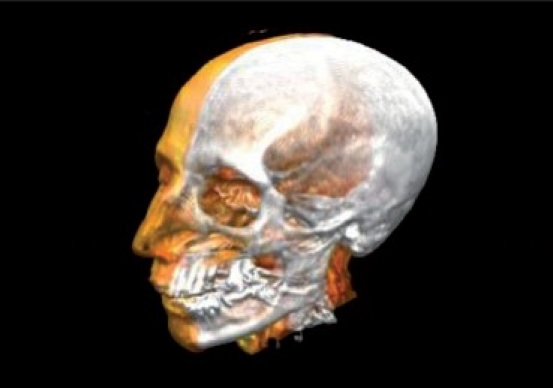
3D volume image of the dental and craniofacial complex
Today, CBCT scanning has become a valuable imaging modality in periodontology as well as implantology. For the detection of smallest osseous defects, CBCT can display the image in all its three dimensions by removing the disturbing anatomical structures and making it possible to evaluate each root and surrounding bone. In implant treatment, appropriate site or size can be chosen before placement, and osseointegration can be studied over a period of time.
This review discusses all the finer details of CBCT which has added a third dimension to the imaging in periodontics.
PRINCIPLES AND EVOLUTION OF COMPUTED TOMOGRAPHY
The first CT scanner was developed in 1967 by Sir Godfrey N. Hounsfield, an engineer at EMI. Since then, CT technology rapidly underwent five developmental generations.
The first generation of CT scanners [Figure 3] used a single detector element to capture a beam of X-rays, corresponding to the integral of linear attenuation coefficients along a single line. It then translated horizontally to acquire the next line integral. After acquiring all the line integrals for a given position of the X-ray source, both the detector and source rotated one degree, a design known as the “translate-rotate” or “pencil-beam” scanner. Hounsfield's unit belonged to this generation, as did the first commercial CT scanners introduced in 1972. Interestingly, these first-generation CT scanners were designed to scan the head only.
Figure 3.
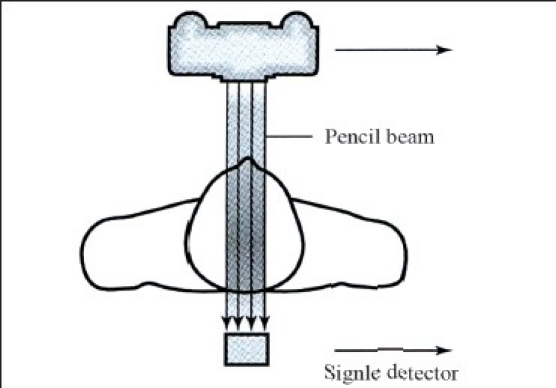
First-generation CT scanner
A second generation of CT systems [Figure 4] was introduced in 1975. These systems, also known as “hybrid” machines, used more than one detector and used small fan-beam, as opposed to pencil-beam, scanning. Like the first generation of CT scanners, these scanners also used a translate-rotate design, and were for the most part head-only scanners. Although the first iterations of full-body CT scanners also incorporated the translate-rotate design, image quality was poor due to patient motion artifacts caused by the significant amount of time required to take the scan.
Figure 4.
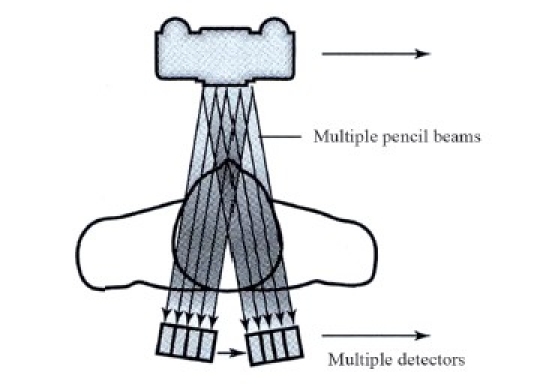
Second-generation CT scanner
The third-generation CT scanners [Figure 5] appeared in 1976 and are the systems most widely used today. These scanners use a large, arc-shaped detector that acquires an entire projection without the need for translation. This rotate-only design, frequently referred to as “fan-beam,” utilizes the power of the X-ray tube much more efficiently than the previous generations.
Figure 5.
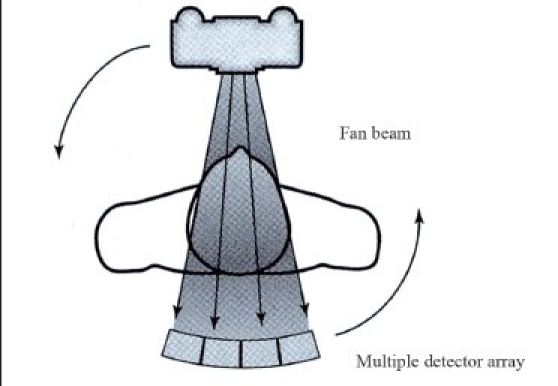
Third-generation CT scanner
The fourth-generation scanners [Figure 6] shortly followed third-generation scanners, replacing the arc-shaped detector with an entire circle of detectors. In this design, the X-ray tube rotates around the patient, while the detector stays stationary. Since these fourth-generation scanners tend to be more expensive and suffer from higher levels of Compton scatter artifacts, most of the commercially available CT scanners today are third-generation scanners.
Figure 6.
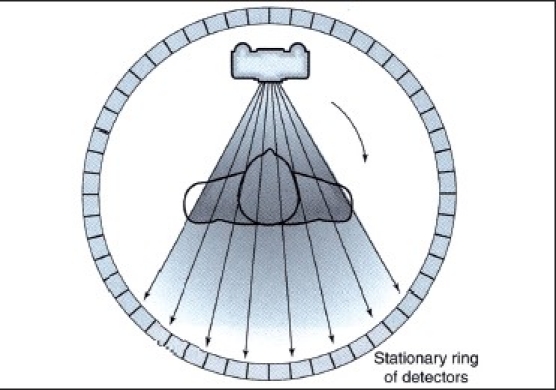
Fourth-generation CT scanner
The fifth-generation scanners [Figure 7] are high-speed CT scanners and also known as EBCT, that is, electron beam CT scanner. It also has dynamic spatial reconstruction ability with scan time of milliseconds.[1]
Figure 7.
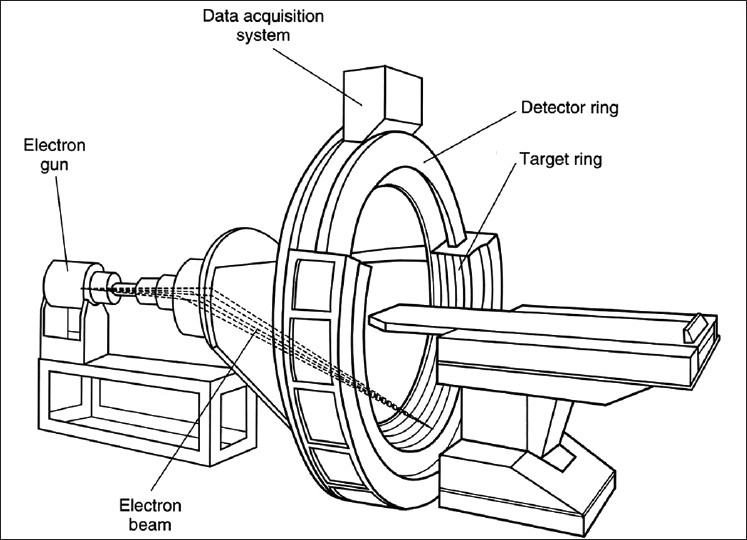
Fifth-generation CT scanner
After an initial period of rapid development, CT technology quickly matured and it was not until the early 1990s that CT research began anew. Recent advances in CT include multirow detectors and spiral scanning. Multirow scanning allows for the acquisition of several cross-sectional slices at the same time, reducing scanning times. Today's state-of-the-art scanners have 64 rows of detectors. Spiral (helical) scanning incorporates a moving table with the rotating X-ray tube, with the net effect that the X-ray tube describes a helical path around the patient.
Conventional CT scanners are large and expensive systems designed for full-body scanning at a high speed to minimize artifacts caused by movement of the heart, lungs, and bowels. They are not well-suited for dedicated dentomaxillofacial imaging, where cost considerations are important, space is often at a premium, and scanning requirements are limited to the head. The advent of CBCT technology has paved the way for the development of relatively small and inexpensive CT scanners dedicated for use in dentomaxillofacial imaging.
PRINCIPLES AND EVOLUTION OF CBCT
CBCT scanners utilize a two-dimensional detector, which allows for a single rotation of the gantry to generate a scan of the entire region of interest, as compared with conventional CT scanners whose multiple “slices” must be stacked to obtain a complete image. In comparison with conventional fan-beam or spiral-scan geometries, cone-beam geometry has higher efficiency in X-ray use, inherent quickness in volumetric data acquisition, and potential for reducing the cost of CT. The cone beam technique requires only a single scan to capture the entire object known as field of view which refers to the area of the anatomy that is captured with a cone of X-rays [Figure 8]. Thus, the time required to acquire a single cone-beam projection is the same as that required by a single fan-beam projection.
Figure 8.
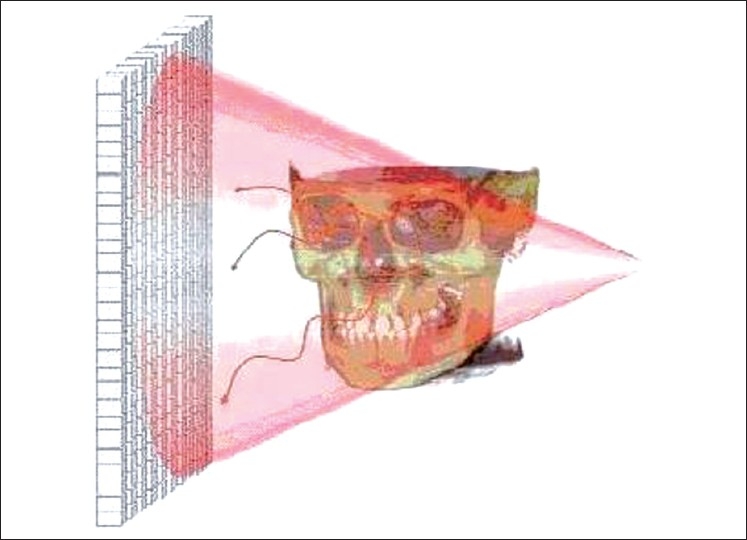
Cone beam geometry
A number of groups have worked on developing task-specific CBCT scanners over the past two decades. The first CBCT scanner ever to be built was built for angiography among other tasks at Mayo in 1982. Later, Fahrig et al., Wiesent et al., Saint-Felix et al., Ning et al., Schueler et al., and Kawata et al. have developed a CBCT CTA (Computed tomography angiography) system for angiographic imaging.[2–8] Jaffray and Siewerdsen[9] and Cho et al.[10] have also developed a CBCT system for radiotherapy applications. Efforts are being made toward dedicated CBCT-based imaging systems for mammography.[11]
Although CBCT has existed for over two decades, its true potential has not yet been fully tapped. Only recently, it has become possible to develop CBCT clinical systems that are both inexpensive and small enough to be used in operation theaters, medical and dental offices, emergency rooms, and intensive care.
Four technological and application-specific factors have converged to make this possible.
First, compact and high-quality flat-panel detector arrays were developed.
Second, the computer power necessary for cone-beam image reconstruction has become widely available and is relatively inexpensive.
Third, x-ray tubes necessary for cone-beam scanning are orders-of-magnitude that are less expensive than those required for conventional CT.
Fourth, by focusing on head/neck scanning only, one can eliminate the need for sub-second gantry rotation speeds that are needed for cardiac and thoracic imaging. This significantly reduces the complexity and cost of the gantry.
CBCT IMAGE PRODUCTION
CBCT machines scan patients in the following three possible positions: sitting, standing, or supine. Despite patient orientation within the equipment, the principles of image production remain the same. The four components of CBCT image production are as follows:
Acquisition configuration
Continuous or pulsed x-ray beam and charged couple device detectors moving synchronously around the fixed fulcrum within the patient's head.
Image detection:
It is determined by individual volume elements or voxels produced from the volumetric data set. CBCT units provide voxel resolutions that are isotropic (equal in all 3 dimensions).
Image reconstruction
The processing of acquired projection frames to the volumetric dataset is done on the personal computer which is called as reconstruction.
Image display
The compilation of all available voxels is presented to the clinician on the computer screen as secondary reconstructed images in three orthogonal planes.
Advantages of CBCT
It has a rapid scan time as compared with panoramic radiography.
It gives complete 3D reconstruction and display from any angle.
Its beam collimation enables limitation of X-radiation to the area of interest.
Image accuracy produces images with submillimeter isotropic voxel resolution ranging from 0.4 mm to as low as 0.076 mm.
Reduced patient radiation dose (29–477 μSv) as compared with conventional CT (approx. 2000 μSv). Patient radiation dose is five times lower than normal CT, as the exposure time is approximately 18 seconds, that is, one-seventh the amount compared with the conventional medical CT.
CBCT units reconstruct the projection data to provide interrelational images in three orthogonal planes (axial, sagittal, and coronal).
Multiplanar reformation is possible by sectioning volumetric datasets nonorthogonally.
Multiplanar image can be “thickened” by increasing the number of adjacent voxels included in the display, referred to as ray sum.
3D volume rendering is possible by direct or indirect technique.
The three positioning beams make patient positioning easy. Scout images enable even more accurate positioning.
Reduced image artifacts: CBCT projection geometry, together with fast acquisition time, results in a low level of metal artifact in primary and secondary reconstructions.
DISADVANTAGES
The only disadvantage is its cost. But considering the enormous benefits, this cost effect can be overlooked.
Indications of CBCT
- Evaluation of the jaw bones which includes the following:
- Pathology;
- Bony and soft tissue lesions;
- Periodontal assessment;
- Endodontic assessment;
- Alveolar ridge resorption;
- Recognition of fractures and structural maxillofacial deformities;
- Assessment of the inferior alveolar nerve before extraction of mandibular third molar impactions;
- Orthodontic evaluation—3D cephalometry;
- Temporomandibular joint evaluation; and
- Implant placement and evaluation
Airway assessment
Whenever there is need for 3D reconstructions
In short, CBCT is ideally suited for high-quality and affordable CT scanning of the head and neck in dentomaxillofacial applications.[12]
PERIODONTAL APPLICATIONS
The first reported applications of CBCT in periodontology were for diagnostic- and treatment-outcome evaluations of periodontitis.[13,14]
The impact of radiographic imaging on the diagnosis and treatment of periodontal disease has essentially remained unchanged for decades. Periodontal diagnosis relies primarily on traditional two-dimensional representation of the alveolar bone. Usefulness of CBCT for periodontal applications is still in progress. Field of interest for the use in periodontology would be the diagnostic and quantitative measurements of soft tissue and alveolar bone levels in three dimensions, imaging of periodontal intrabony defects, dehiscence and fenestration defects, diagnosis of furcation-involved molars, and implant site imaging.[12,13,15]
CBCT in assessment of PDL space
The earliest signs of periodontal disease in radiographs are fuzziness, break in the continuity of lamina dura, and a wedge-shaped radiolucent area at the mesial and distal aspect of the PDL space. In addition to this, the proper observation of PDL space may offer some potential regarding detection of occlusal trauma and the effects of systemic diseases on the periodontium.
CBCT ex vivo visualization of the periodontal ligament and periodontal ligament space has been evaluated in comparison with radiography with mixed results.[16]
CBCT for periodontal defect measurements
The extent of periodontal marginal bone loss is not always easy to determine and certainly not the extent with which furcation areas are involved. CBCT images provide better diagnostic and quantitative information on periodontal bone levels in three dimensions than conventional radiography. CBCT is found to be as accurate as direct measurements using a periodontal probe and as reliable as radiographs for interproximal areas. Although two-dimensional radiography is of use for interproximal lesions, its limitation was anticipated during early investigations, determining its diagnostic value for periapical and periodontal disease [Figures 9 and 10]. So, when buccal and lingual defects cannot be diagnosed with radiography, CBCT is a superior technique.[17–21]
Figure 9.
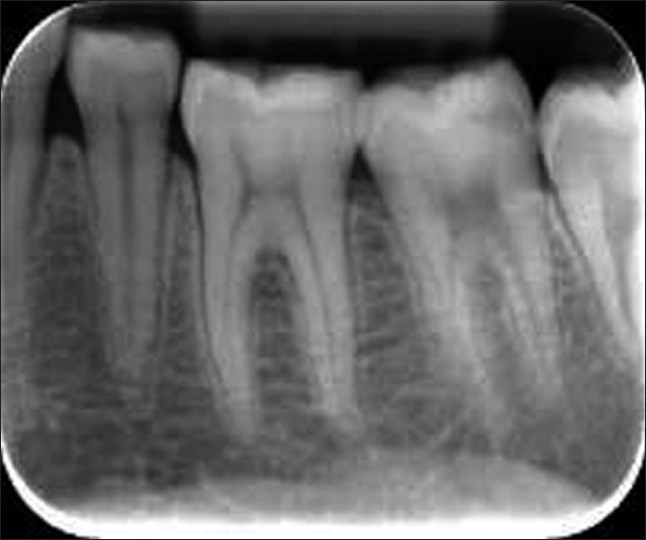
IOPA radiograph of mandibular molar region
Figure 10.
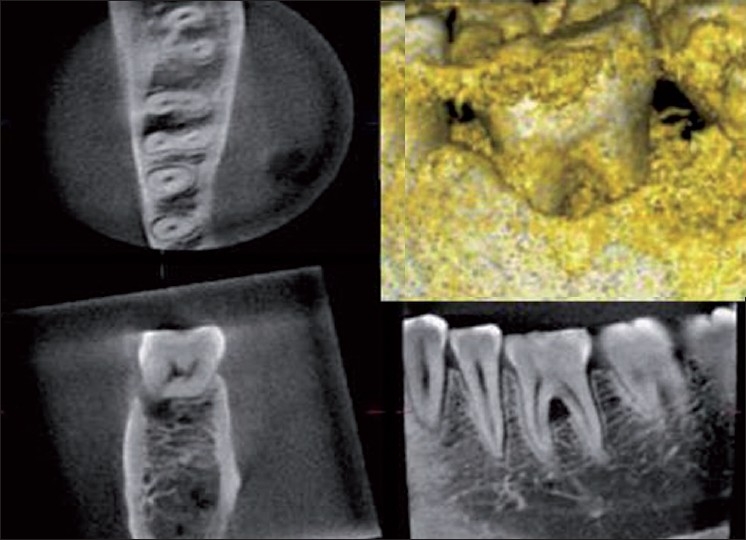
CBCT images of mandibular first molar showing the marginal bone defect and the precisely assessed degree of bone loss. In the upper right corner is a 3D image based on the radiographic volume data
A study on the use of CBCT to examine the geometric relationship between the roots and furcation areas of the mandibular first molars has verified that the X-ray beam projection angle affects the accuracy and diagnosis of a furcation defect. Changes in horizontal angulation cause geometric distortion in intraoral radiography [Figure 11].[22]
Figure 11.
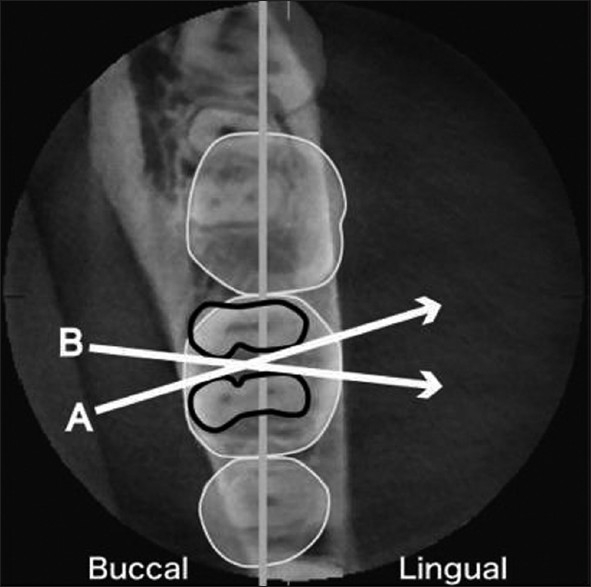
CBCT to examine the geometric relationship between the roots and furcation areas of the mandibular first molars
Soft tissue CBCT for the measurement of gingival tissue and the dimensions of the dentogingival unit
This novel method is based on CBCT technology called soft tissue CBCT (ST-CBCT), to visualize and precisely measure distances corresponding to the hard and soft tissues of the periodontium and dentogingival attachment apparatus. With this simple and noninvasive technique, clinicians are able to determine the relationships between
gingival margin and the facial bone crest,
gingival margin and the cemento-enamel junction (CEJ), and
CEJ and facial bone crest.
The width of the facial and palatal/lingual alveolar bone and the width of the facial and palatal/lingual gingival also could be measured[23] [Figures 12 and 13].
Figure 12.

Image of the soft tissue CBCT scan showing a dark space (asterisks) on the facial and palatal/lingual aspects, allowing the clear visualization of the facial (arrow) and palatal (arrowhead) gingiva
Figure 13.

(a) Measurement of the thickness of the facial gingiva performed on the image of the patient with a thick periodontal biotype (soft tissue cone-beam computed tomography scan). (b) Measurement of the distance of the gingival margin to the facial bone crest. (c) Measurement of the distance of the gingival margin to the cemento-enamel junction. Dotted lines represent the long axis of the tooth
Tissue biotypes have been linked to the outcomes of periodontal and implant therapy. When tissue biotypes of 22 fresh cadaver heads were assessed clinically and radiographically with CBCT scans, the labial gingival thickness was moderately associated with the underlying bone thickness measured with CBCT. These measurements were an accurate representation of the clinical thickness of both labial gingiva and alveolar bone.[24]
ST-CBCT will certainly aid clinicians in the planning and execution of a number of procedures in dentistry with increased predictability.
CBCT precision in alveolar bone density measurement
Radiographic follow-up of bone healing after grafting is challenging because of the overlapping of gaining and losing areas within the graft. The new volumetric imaging method, CBCT, offers an opportunity to see inside the bone and pinpoint and measure densities in small localized areas such as a vertical periodontal defect, or an alveolar bone graft. This precision would make it possible to reproducibly quantify the bone remodeling after bone grafting.[14]
CBCT for diagnostic imaging for the implant patient
For the evaluation of implant placement, many radiographic projections are available, each with advantages and disadvantages. Radiography is an essential diagnostic tool for implant design and successful treatment of the implant patient. Selection of appropriate radiographic modality will provide the maximum diagnostic information, help avoid unwanted complications, and maximize treatment outcomes while delivering “as low as reasonably achievable” radiation dose to the patient.[15]
Clinicians have been diagnosing, treatment planning, placing, and restoring modern dental implants using periapical and panoramic imaging films to assess bone anatomy for several decades. Two-dimensional film images have been found to have limitations because of inherent distortion factors, and the noninteractive nature of film itself provides little information regarding bone density, bone width, or spatial proximity of vital structures.
Diagnostic imaging techniques must always be interpreted in conjunction with good clinical examination. Many factors influence the selection of radiographic techniques for a particular case, including cost, availability, radiation exposure, and case type. The decision is a balance between these factors and the desire to minimize risk of complications to the patient.
Cross-sectional imaging modalities that include conventional x-ray tomography, computer tomography, and CBCT are valuable imaging modalities.
Of all the three, CBCT scanning is the most successful, useful, and valuable imaging modality for 3D and cross-sectional evaluation of the implant patient [Figure 14]. It has similar advantages and disadvantages as CT scanning. The most significant difference is that CBCT imaging requires much less radiation exposure.
Figure 14.
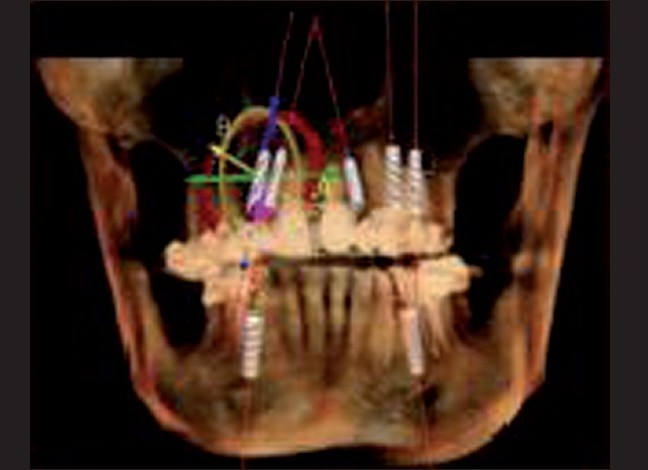
Virtual implant placement using cone beam CT scan
Location is the most important factor while placing an implant. From 3D planning to CT-directed placement, to take the advantage of available bone and avoid anatomic structures, the science of implantology has been revolutionized by 3D imaging. Not only has it added safety and accuracy, it has also minimized or eliminated the need for supportive procedures like bone and tissue grafting in many situations.
Software and technology development trends suggest that in the near future, CBCT scans will be used to develop a patient-specific 3D model that will be used for implant diagnosis, treatment planning, treatment simulation, implant placement (surgery), and tooth replacement (restoration of implant).
Limitations of CBCT
Current CBCT technology has limitations related to the “cone-beam” projection geometry, detector sensitivity, and contrast resolution that produces images that lack the clarity and usefulness of conventional CT images. The clarity of CBCT images is affected by artifacts, noise, and poor soft tissue contrast.
Controversies
As with any emerging imaging technology, use of CBCT scanners has been the subject of criticism as well as acclaim. The technology itself is limited by lack of user experience and what is currently a relatively small body of related literature. Research on this technology is still preliminary, without prospective studies that convincingly demonstrate its benefit compared with conventional CT.
Office-based CBCT imaging is usually performed and interpreted by non-radiologists, often without the accreditation, training, or licensure afforded by the radiology community. So, to address this issue, emphasizing the role of the practitioner in obtaining and interpreting CBCT images is necessary.
CONCLUSION
As CBCT scanning is finding more and more applications in dentomaxillofacial radiology, it stands as the privileged field of imaging in periodontics. Current methods of detecting alveolar bone level changes over time or determining 3D architecture of osseous defects are inadequate. This issue has been addressed by the recent low-cost CBCT machines, which has resulted in production of an affordable, low-radiation high-quality 3-D data. CBCT is an essential diagnostic tool also for selection of implant design and its placement. CBCT provides high quality of diagnostic images that have an absorbed dose that is comparable with other dental surveys and less than a conventional CT and thus following the principles of radiation protection to reduce the radiations “as low as reasonably achievable” (ALARA).
To conclude, CBCT with its high spatial resolution, affordability, smaller size, lower acquisition and maintenance have made it as a natural fit in periodontal imaging.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Robb RA. The dynamic spatial reconstructor: An x-ray video fluoroscopic ct scanner for dynamic volume imaging of moving organs. IEEE Trans Med Imaging. 1982;1:22–33. doi: 10.1109/TMI.1982.4307545. [DOI] [PubMed] [Google Scholar]
- 2.Fahrig R, Fox AJ, Lownie S, Holdsworth DW. Use of a C-arm system to generate true three-dimensional computed rotational angiograms: Preliminary in vitro and in vivo results. Am J Neuroradiol. 1997;18:1507–14. [PMC free article] [PubMed] [Google Scholar]
- 3.Fahrig R, Nikolov H, Fox AJ, Holdsworth DW. A three-dimensional cerebrovascular flow phantom. Med. Phys. 26 8. 1999:1589–1599. doi: 10.1118/1.598672. [DOI] [PubMed] [Google Scholar]
- 4.Wiesent K, Barth K, Navab N, Durlak P, Brunner T, Schuetz O, et al. Enhanced 3D reconstruction algorithm for c-arm systems suitable for interventional procedures. IEEE Trans Med Imaging. 2000;19:391–403. doi: 10.1109/42.870250. [DOI] [PubMed] [Google Scholar]
- 5.Saint-Félix D, Trousset Y, Picard C, Ponchut C, Roméas R, Rougée A. In vivo evaluation of a new system for 3D computerized angiography. Phys Med Biol. 1994;39:583–95. doi: 10.1088/0031-9155/39/3/020. [DOI] [PubMed] [Google Scholar]
- 6.Ning R, Chen B, Yu R, Conover D, Tang X, Ning Y. Flat panel detector-based cone beam volume CT angiography imaging: System evaluation. IEEE Trans Med Imaging. 2000;19:949–63. doi: 10.1109/42.887842. [DOI] [PubMed] [Google Scholar]
- 7.Schueler BA, Sen A, Hsiung HH, Latchaw RE, Hu X. Three-dimensional vascular reconstruction with a clinical X-ray angiography system. Acad Radiol. 1997;4:693–9. doi: 10.1016/s1076-6332(97)80141-9. [DOI] [PubMed] [Google Scholar]
- 8.Kawata Y, Niki N, Kumazaki T. Measurement of blood vessel characteristics for disease detection based on cone beam CT images. IEEE Trans Nuc Sci. 1996;43:3348–54. [Google Scholar]
- 9.Jaffray DA, Siewerdsen JH. Cone-beam computed tomography with a flat-panel imager: Initial performance characterization. Med Phys. 2000;27:1311–23. doi: 10.1118/1.599009. [DOI] [PubMed] [Google Scholar]
- 10.Cho PS, Johnson RH, Griffin TW. Cone-beam CT for radiotherapy applications. Phys Med Biol. 1995;40:1863–83. doi: 10.1088/0031-9155/40/11/007. [DOI] [PubMed] [Google Scholar]
- 11.Ning R, Chen B. Cone beam volume CT mammographic imaging: Feasibility study. In Presented at Proceedings of SPIE - The International Society for Optical Engineering. 2001 [Google Scholar]
- 12.Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48. doi: 10.1046/j.0906-6713.2003.003423.x. [DOI] [PubMed] [Google Scholar]
- 13.Tynd all DA, Rathore S. Conone ne-beam CT diagnostic applications: Caries, periodontal bone assessment, and endodontic applications. Dent Clin North Amnone. 2008;52:825–41. doi: 10.1016/j.cden.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Ito K, Yoshinuma N, Goke E, Arai Y, Shinoda K. Clinical application of a new compact computed tomography system for evaluating the outcome of regenerative therapy: A case report. J Periodontol. 2001;72:696–702. doi: 10.1902/jop.2001.72.5.696. [DOI] [PubMed] [Google Scholar]
- 15.Newman MG, Takei H, Carranza FA, Jr, Klokkevold PR. Carranza's Clinical Periodontology. 10th ed. India: Elsevier publication; 2007. Diagnostic imaging for the implant patient; pp. 1105–18. [Google Scholar]
- 16.Ozmeric N, Kostioutchenko I, Hägler G, Frentzen M, Jervøe-Storm PM. Cone-beam computed tomography in assessment of periodontal ligament space: In vitro study on artificial tooth model. Clin Oral Investig. 2008;12:233–9. doi: 10.1007/s00784-008-0186-8. [DOI] [PubMed] [Google Scholar]
- 17.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: An in vitro study on native pig and human mandibles. J Periodontol. 2005;76:665–73. doi: 10.1902/jop.2005.76.5.665. [DOI] [PubMed] [Google Scholar]
- 18.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 19.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:395–401. doi: 10.1016/j.tripleo.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–24. doi: 10.1259/dmfr/26475758. [DOI] [PubMed] [Google Scholar]
- 21.Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: An in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008;37:252–60. doi: 10.1259/dmfr/57711133. [DOI] [PubMed] [Google Scholar]
- 22.Hishikawa T, Izumi M, Naitoh M, Furukawa M, Yoshinari N, Kawase H, et al. The effect of horizontal X-ray beam angulation on the detection of furcation defects of mandibular first molars in intraoral radiography. Dentomaxillofac Radiol. 2010;39:85–90. doi: 10.1259/dmfr/99338642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Januário AL, Barriviera M, Duarte WR. Soft tissue cone-beam computed tomography: A novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent. 2008;20:366–73. doi: 10.1111/j.1708-8240.2008.00210.x. [DOI] [PubMed] [Google Scholar]
- 24.Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81:569–74. doi: 10.1902/jop.2009.090591. [DOI] [PubMed] [Google Scholar]


