Abstract
Aim:
To compare the effect of experimental local-drug delivery system containing 2% whole turmeric (gel form) as an adjunct to scaling and root planing (SRP) with the effect achieved using SRP alone by assessing their respective effects on plaque, gingival inflammation, bleeding on probing pocket depth, relative attachment levels and trypsin-like enzyme activity of “red complex” microorganisms, namely, Bacteroides forsythus, Porphvromonas gingivalis and Treponema denticola.
Material and Methods:
Thirty subjects with chronic localized or generalized periodontitis with pocket depth of 5 to 7 mm were selected in a split-mouth study design. Control sites received SRP alone, while experimental sites received SRP plus experimental material (2% whole turmeric gel). Plaque index (PI), gingival index (GI), sulcus bleeding index (SBI), probing pocket depth (PPD), relative attachment loss (RAL), microbiological study of collected plaque sample for trypsin-like activity of “red complex” by BAPNA assay were the parameters recorded on day 0, 30 days and 45 days.
Results:
Both groups demonstrated statistically significant reduction in PI, GI, SBI, PPD; and gain in RAL. Significant reduction in the trypsin-like enzyme activity of “red complex” (BAPNA values) was observed for both the groups when compared to the baseline activity. Greater reduction was seen in all the parameters in the experimental group in comparison to the control group.
Conclusion:
The experimental local drug-delivery system containing 2% whole turmeric gel can be effectively used as an adjunct to scaling and root planing and is more effective than scaling and root planing alone in the treatment of periodontal pockets.
Keywords: BAPNA, local drug delivery, periodontitis, 2% whole turmeric gel
INTRODUCTION
Periodontitis has a multifactorial etiology, with primary etiologic agents being pathogenic bacteria that reside in the subgingival area. The goal of periodontal therapy is to prevent, arrest, control or eliminate periodontitis and to restore the lost form, function, esthetics and comfort.
Treatment of periodontal disease is routinely based on mechanical debridement of the tooth surface and appropriate and meticulous maintenance of oral hygiene. However, comprehensive mechanical debridement of sites with deep periodontal pockets is difficult to accomplish.[1] It alone may fail to eliminate the pathogenic microflora because of their location within the gingival and dental tissues or in other areas inaccessible to periodontal instruments. As an adjunctive approach, systemic or local administration of antibiotics is done because of the microbial etiology of periodontitis. Various disadvantages of the systemic antibiotic therapy, like hypersensitivity reaction, organ toxicity and development of resistant bacteria, coupled with its requirement of higher dosage to attain required GCF concentration at the target site, led to the use of local drug-delivery system.[2]
Some of the agents used till date are tetracyclines doxycycline and minocycline; metronidazole; and chlorhexidine, but they are relatively expensive. Hence this study was planned to evaluate turmeric, which is a common antiseptic used in the traditional system of Indian medicine, as a component of local drug-delivery system. Turmeric (haldi) is a rhizome of Curcuma longa and may be a more acceptable and viable option for the common man. It has proven properties like anti-inflammatory, antioxidant, antimicrobial, hepatoprotective, immunostimulant, antiseptic, antimutagenic, and it also accelerates wound healing.[3]
MATERIALS AND METHODS
Material
The Poona College of Pharmacy, Pune, Maharashtra, India, provided 2% whole turmeric gel. The composition of the gel was turmeric extract, 2%; pluronic polymer, 20%; and water q.s. N-benzoyl-L-arginine–p-nitroanilide (BAPNA; Sigma, St. Louis, Missouri, USA).
Methods
Clinical evaluation
Thirty subjects, from the outpatient department of Periodontology, Bharati Vidyapeeth Dental College and Hospital, Pune, diagnosed to have localized or generalized chronic periodontitis with pocket depth of 5 to 7 mm in at least 2 nonadjacent sites in different quadrants of the mouth and with at least 20 remaining teeth were considered for the present study.
Study protocol
The relevant data were recorded in a special pro forma sheet. Clinical examination was done in a dental chair, under standard conditions of light, using a mouth mirror, explorer, William's graduated periodontal probe and tweezer; and assessment of clinical parameters was carried out. Selected sites were randomly divided into control sites and experimental sites, which were treated by using split-mouth design.
Thirty control sites were treated by scaling and root planing alone, and 30 experimental sites were treated with scaling and root planing followed by placement of the experimental material (2% whole turmeric gel) in the periodontal pocket. All participants were explained about the need, design of the study and its potential benefits. Informed written consent was obtained. The study protocol was approved by the Ethics Committee of the institution.
Recording of clinical and microbiological parameters
The parameters that were recorded include (1) plaque index (Turesky-Gilmore-Glickman modification of the Quigley-Hein, 1970)[4]; (2) gingival index (Loe and Silness, 1963)[5]; (3) sulcus bleeding index (Muhlemann and Son, 1971)[6]; (4) pocket depth measurement using William's graduated probe using acrylic stent[7]; (5) relative distance between base of pocket and fixed reference point on the stent for assessing clinical attachment gain or loss[7]; (6) microbiological study of collected plaque sample for trypsin-like activity of “red complex” microorganisms by BAPNA assay.[8] The above clinical and microbiological parameters were recorded on day 0, 30 days and 45 days.
Microbiological study
All the detectable supragingival soft deposits were removed, and subgingival plaque sample was collected by a sterile curette. The sample was suspended in a pre-weighed coded microcentrifuge tube containing a sterile buffer (Tris HCl; pH, 6.8) and stored at –80°C. The plaque samples were assessed for estimating trypsin-like protease activity.
An amount of 1 mL of a solution containing the enzyme substrate (N-benzoyl-L-arginine–p-nitroanilide, BAPNA; Sigma, St. Louis, Missouri, USA) was then added to the tubes. This suspension was vortexed and then placed in an ultrasound bath on ice for 10 minutes with 2-second cycles and 2-second intervals at 17 W using a 100-W ultrasonic processor. After 17 hours of incubation at 37°C, the reaction was stopped with ice and by the addition of 100 mL of glacial acetic acid. The absorbance was read at 405 nm by a spectrophotometer. The results were given in nanomoles of the product per minute per milligram of dental plaque wet weight.[9]
Periodontal therapy
The clinical and microbiological parameters were assessed at the baseline at selected sites, followed by thorough scaling and root planning (SRP). On completion of SRP, control sites were covered with Coe-Pak. The experimental site was isolated with cotton rolls to prevent contamination from saliva. The experimental local drug-delivery system was in liquid form (under refrigeration) and was carried in a syringe with a needle attached to it. With increasing temperature as in oral cavity, gel formation occurred, which could be used as a local drug to be delivered to the periodontal pocket. The pocket opening was covered with Coe-Pak to retain the material in the pocket, as well as to prevent the ingress of oral fluids. Subjects were recalled after 7 days for removal of the periodontal dressing, for oral hygiene maintenance instructions and recording of subjective and objective criteria. Recall visits were again scheduled after 30 days and 45 days of placement of local experimental drug for measuring the clinical parameters, microbiological study and for assessment of subjective and objective criteria as per the study design.
Statistical analysis
Post-treatment changes in various clinical parameters from day 0 occurring in different time intervals were analyzed by paired t test (intra-group). Inter-group comparisons of post-treatment changes were analyzed by unpaired t test. P<0.05 was considered as significant difference (Epi Info version 6.0).
RESULTS
A total of 60 sites in 30 patients were treated. Thirty sites received the experimental local drug (experimental sites), and 30 sites did not receive local drug. At the end of 45 days of observation, all the sites healed uneventfully. Neither complications nor allergic reactions that could be related to the experimental treatment modalities were observed.
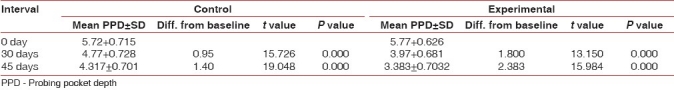
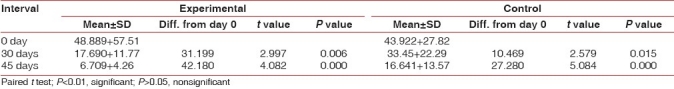
In the present study, statistically significant reduction in the mean plaque index, gingival index, sulcus bleeding index, probing pocket depth; and also statistically significant gain in clinical attachment in both the groups from the baseline was observed [Tables 1–5].
Table 1.
Plaque index
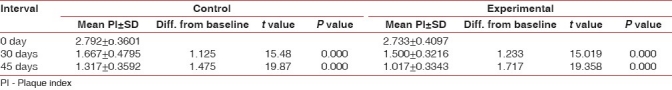
Table 5.
Relative attachment level
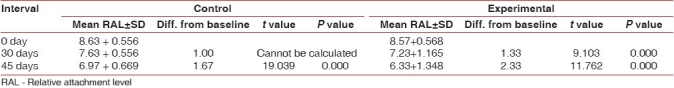
Table 2.
Gingival index
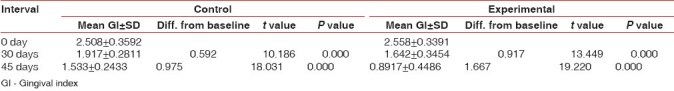
Table 3.
Sulcus bleeding index
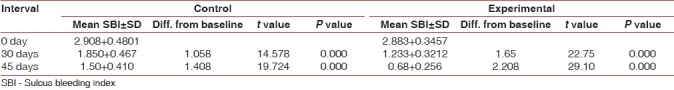
Table 4.
Probing pocket depth
Significant reduction in the trypsin-like enzyme activity of “red complex” microorganisms (BAPNA values) was observed for both the groups when compared to the baseline activity [Table 6]. However, greater reduction was observed in the experimental sites in comparison with the control sites [Tables 1–6].
Table 6.
Values of BAPNA
DISCUSSION
To the best of our knowledge, no studies on turmeric (in gel form) as a local drug-delivery system have been reported in literature. However, Adriana et al. (2001)[10] observed similar reductions in mean plaque index, gingival index, sulcus bleeding index, probing pocket depth; and gain in clinical attachment level using 1% chlorhexidine gel as an adjunct to SRP. In our study, turmeric was used in gel form. Bhandari and Shankwalkar[11] used turmeric in the form of a mouthwash. Similar reductions have been attributed to the use of turmeric in pure and water-soluble form as a consequence of its anti-inflammatory property.
To the best of our knowledge, no studies on turmeric (in gel form) as a local drug-delivery system and its microbiological evaluation by BAPNA (quantitative) assay have been reported in literature. Adriana et al. (2001)[10] observed reductions in PD and gain in CAL in BAPNA (qualitative)-positive sites. Drake et al.[12] and Han et al.[13] observed antimicrobial activity of turmeric. The reduction in BAPNA values in our study could be attributed to antibacterial activity of turmeric.
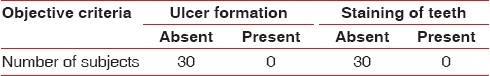
In terms of taste and comfort, the experimental material was found to be acceptable by all the subjects in our study. There was good biological acceptability, as evidenced by the absence of burning sensation, dryness/soreness, ulcer formation and staining of teeth [Tables 7 and 8].
Table 7.
Subjective criteria
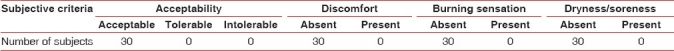
Table 8.
Objective criteria
It is clear from the results of the present study that the experimental local drug along with scaling and root planing is effective in removing the local irritants, reducing gingival inflammation, reducing pocket depth and also results in gain in clinical attachment. It also controls the localized infection and prevents new lesion formation.
The local drug-delivery system used in the present study is simple and easy to use. Its suitability for use with a syringe allows easy insertion into the pocket. Also, bioadhesive property of the experimental drug allows better retention. It is also biologically accepted without any side effects.
CONCLUSION
It can be concluded that the experimental local drug-delivery system containing 2% whole turmeric gel can be effectively used as an adjunct to scaling and root planing and is more effective than scaling and root planing alone in the treatment of periodontal pockets. When used as an adjunct to scaling and root planing, it helps in reduction of pocket depth and gain of clinical attachment. It is a beneficial antimicrobial, anti-inflammatory and anti-plaque agent. It also shows favorable reduction of trypsin-like enzyme activity of microorganisms associated with periodontal disease. The experimental material was biologically well accepted by the oral tissues and showed good acceptability with no side effects by all the subjects in the study. The experimental local drug-delivery system is easy to use, is a noninvasive technique and requires less chair side time.
To elucidate the use of this local drug-delivery system in future, a long-term study carried out on a large sample of subjects is required. Also, in addition to BAPNA assay, culture methods for microbiological analysis of individual periodontopathogens should be used. An attempt should be made to find out the efficacy of the experimental material in comparison to other marketed local drug-delivery systems.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Cobb CM. Non surgical pocket therapy: Mechanical. Ann Periodontol. 1996;1:443–90. doi: 10.1902/annals.1996.1.1.443. [DOI] [PubMed] [Google Scholar]
- 2.Greenstein G. Local drug delivery in the treatment of periodontal diseases: Assessing the clinical significance of the results. J Periodontol. 2006;77:565–78. doi: 10.1902/jop.2006.050140. [DOI] [PubMed] [Google Scholar]
- 3.Chattopadhyay I, Biswas K, Bandyopadhyay U, Banerjee RK. Turmeric and curcumin: Biological actions and medicinal applications. Curr Sci. 2004;87:44–53. [Google Scholar]
- 4.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of vitamin C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 5.Loe H, Silness J. Periodontal disease in pregnancy. Acta Odontol Scand. 1963;21:533–42. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 6.Muhlemann HR, Son S. Gingival sulcus bleeding – a leading symptom in initial gingivitis. Helevetia Odontologica Acta. 1971;15:107–13. [PubMed] [Google Scholar]
- 7.Clark DC, Chin Quee T, Bergeron MJ, Chan EC, Lautar-Lemay C, de Gruchy K. Reliability of attachment level measurements using the cementoenamel junction and plastic stent. J Periodontol. 1987;58:115–8. doi: 10.1902/jop.1987.58.2.115. [DOI] [PubMed] [Google Scholar]
- 8.Syed SA, Gusberti FA, Loesche WJ, Lang NP. Diagnostic potential of chromogenic substrates for rapid detection of bacterial enzymatic activity in health and diseaseassociated periodontal plaques. J Periodontol Res. 1984;19:618–21. doi: 10.1111/j.1600-0765.1984.tb01327.x. [DOI] [PubMed] [Google Scholar]
- 9.Del Peloso Ribeiro E, Bittencourt S, Nociti FH, Jr, Sallum EA, Sallum AW, Casati MZ. Comparative Study of Ultrasonic Instrumentation for the Non-Surgical Treatment of Interproximal and Non-Interproximal Furcation Involvements. J Periodontol. 2007;78:224–30. doi: 10.1902/jop.2007.060312. [DOI] [PubMed] [Google Scholar]
- 10.Vinholis AH, Figueiredo LC, Marcantonio Júnior E, Marcantonio RA, Salvador SL, Goissis G. Subgingival utilization of 1% chlorhexidine collagen gel for the treatment of periodontal pockets.A clinical and microbiological study. Braz Dent J. 2001;12:209–13. [PubMed] [Google Scholar]
- 11.Bhandari H, Shankwalkar GB. Clinical assessment of action of combination of indigenous drugs on dental plaque, calculus and gingivitis. Dissertation Submitted to the University of Bombay. 1980 [Google Scholar]
- 12.Drake D, Halt S, Schwartz J, Mager D, Kozlowski VA. Effects of environmental agents on bacteria of the oral cavity. Clin Oral Microbiol. 2004;108 [Google Scholar]
- 13.Han SH, Yu HH, Shin HS, Lee SI, Kim KJ, Geong SI. Antibacterial activity of curcumin and bisdimethyl-curcumin isolated from curcuma longa. Microbiology and Immunology. 2004;19 [Google Scholar]


