Abstract
Dental implants are being increasingly applied in the restoration of partial and completely edentulous patients. Often, in these patients, soft and hard tissue defects result from a variety of causes, such as, periodontal infection, trauma, and tooth loss. These create an anatomically less favourable foundation for ideal implant placement. For prosthetic-driven dental implant therapy, reconstruction of the alveolar bone, through a variety of regenerative surgical procedures has become predictable. This article documents the soft and hard tissue treatment management of a patient with Generalized Chronic Periodontitis, who required hard and soft tissue augmentation of the ridge, prior to implant placement. We augmented the height and width of the ridge (Seibert's Class III ridge deficiency) using an Autogenous J-shaped graft involving the chin and lower border of the mandible, followed by soft tissue augmentation of the ridge with a subepithelial connective tissue graft. A significant increase in the ridge dimensions was achieved.
Keywords: J-shaped graft, perio-esthetics, soft and hard tissue augmentation
INTRODUCTION
The field of surgical periodontics has undergone a major metamorphosis over time to provide a functionally as well as an esthetically pleasing outcome for all patients. Elimination of the etiological factors and restoration of the normal health of the periodontium is the primary objective of any periodontal therapy. However, the preliminary phase of periodontal therapy is the extraction of teeth with a hopeless prognosis. Replacement of missing teeth, even if extracted due to periodontal reasons, with dental implants, is gaining predictability by the day.
The consequences of tooth loss include pathological migration of other teeth and hard and soft tissue deficit. resorption proceeds quickly after tooth extraction and significantly reduces the possibility of placing implants without grafting procedures. Furthermore, in these patients, soft and hard tissue defects resulting from a variety of causes, such as, periodontal infection, trauma and tooth loss, create an anatomically less favourable foundation for ideal implant placement. Successful implant therapy is dependent upon an adequate volume of bone at the site of the implant placement, as the long-term prognosis of dental implant is adversely affected by inadequate bone volume.[1]
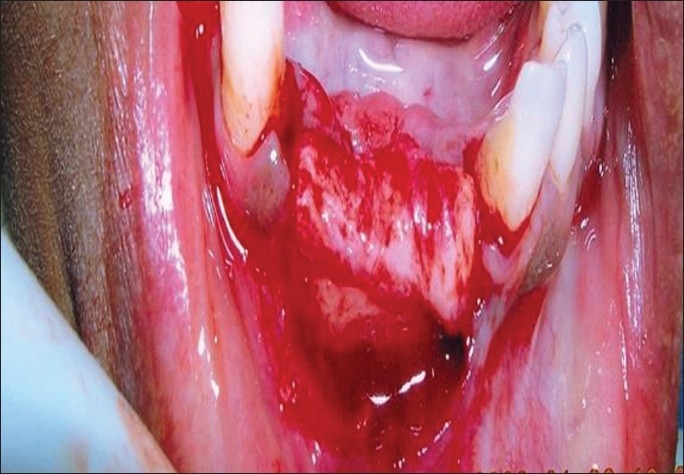
The uniqueness in this case report lies in the type of autogenous chin graft that we have used for the augmentation of the defect. As it was a Seibert's class III ridge defect, augmentation of the height and width of the defect was possible by this J-shaped graft, which was wedged into the defect in such a manner that the graft involving the base of the mandible was rotated to form the shape of the arch and the symphysial part was used to augment the defect in width [Figure 1]. Augmentation of the alveolar bone with such an inlay–onlay bone graft often provides the desired gain of bone, allows for the ideal placement of dental implants, and improves the esthetics phenomenally.
Figure 1.
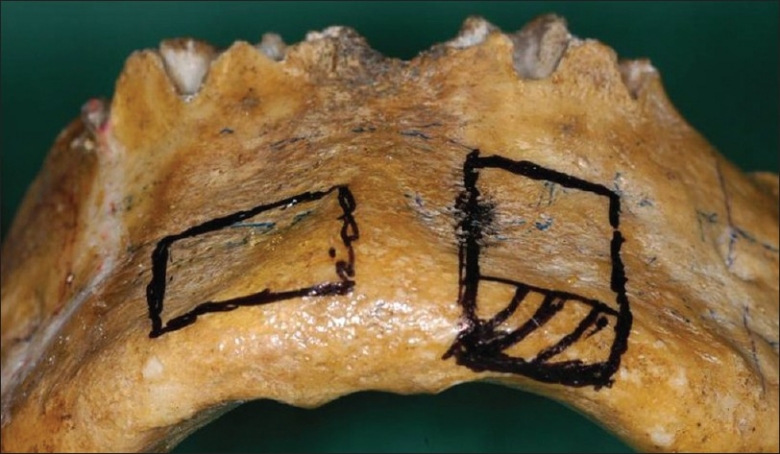
Anatomy of a J-shaped chin graft
In this case report, a combination of hard tissue and soft tissue augmentation of the edentulous area (Seibert's Class III ridge deficiency) was successfully performed, followed by implant placement.
CASE REPORT
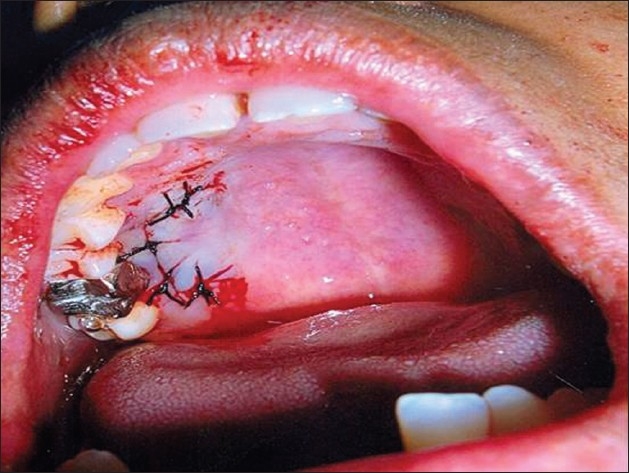
A 33-year-old female patient reported to the Outpatient clinic, in March 2007, with the chief complaint of mobility of the lower front teeth since three months. The patient was systemically healthy. Clinical examination revealed generalized gingival inflammation, bleeding on probing, and generalized probing pocket depths of 6 mm to 8 mm, and generalized clinical attachment loss of 3 mm to 4 mm. Grade III mobility was elicited in relation to 42 and 31. A provisional diagnosis of Generalized Chronic Periodontitis was made, which was well-supported by the supplemental evidence of generalized horizontal bone loss, as observed in the Orthopantomograph [Figure 2] and a full set of intraoral periapical radiographs taken. A final diagnosis of Generalized Chronic Periodontitis was established, followed by a tailor-made treatment plan, best suited for this particular case.
Figure 2.

Preoperative orthopantamograph
Treatment
Extraction of teeth 42 and 31, which had a hopeless prognosis due to grade III mobility was postponed for esthetic reasons. A thorough Phase I therapy was commenced, which included oral hygiene instructions with meticulous scaling and root planing. Re-evaluation of the probing depths, clinical parameters, and oral hygiene status of the patient was performed four weeks following the phase I therapy. As patient compliance to Phase I therapy was excellent and oral hygiene maintenance was satisfactory, phase II therapy was initiated. Flap surgery was performed in areas of persistent deep periodontal pockets in relation to all the four quadrants. The next stage of treatment aimed at reconstruction of sufficient dimensions of hard and soft tissues, for placement of implants in relation to the edentulous area at the 31, 41, and 42 region. A combination grafting procedure including hard tissue and soft tissue augmentation proved ideal. Phase II therapy included implant placement followed by prosthetic rehabilitation of the patient in the restorative phase (Phase III).
Hard tissue augmentation
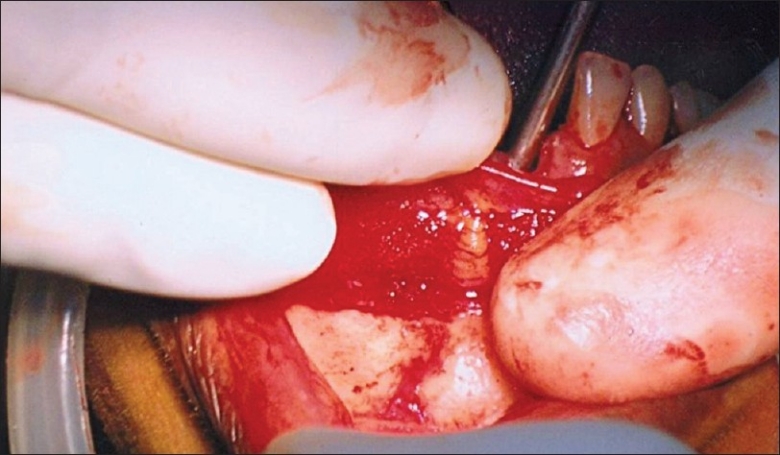
Under local anesthesia (2% Xylocaine with 1:80,000 adrenaline), high and vestibular incisions were placed extending from region 33 to 43. The chin was degloved (intra-oral surgical exposure of the bony mandibular chin) till the inferior border of the mandible [Figure 3]. A corticocancellous block bone graft (2 cm length×1 cm breadth) was harvested from the inferior border of the mandible (J graft) [Figure 4]. The recipient site was exposed with crestal incisions extending from region 33 to 43. The graft was tunneled and positioned on the crestal ridge and secured using a standard microscrew (1.5mm diameter) [Figures 5–7]. The flap was repositioned and sutured with 4-0 vicryl. Postoperative instructions were given. Medications including antibiotics and analgesics were prescribed. No major complications were recorded at the donor or recipient sites. Soft tissue healing was uneventful, and pain and swelling were comparable to the usual dentoalveolar procedures.
Figure 3.
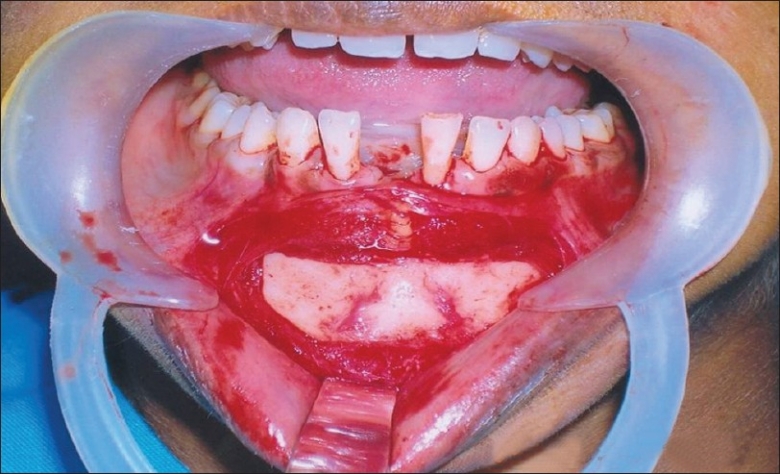
Clinical site of surgery
Figure 4.

Graft harvested
Figure 5.
Ridge split
Figure 7.

Graft in place
Figure 6.
J-shaped bone
Soft tissue augmentation
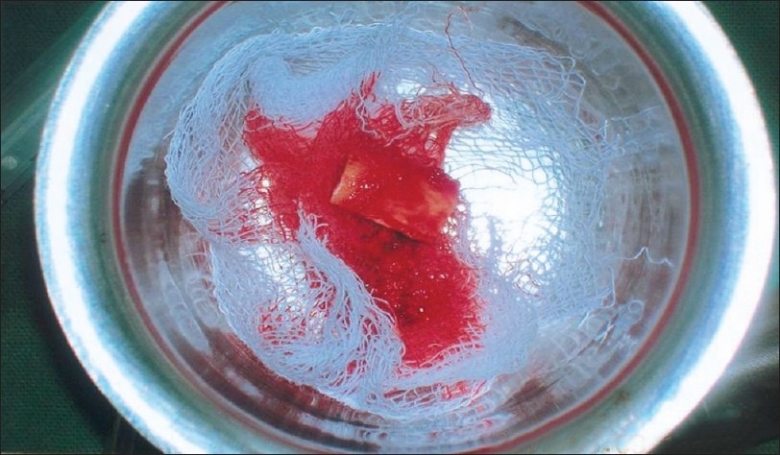
Following successful ridge augmentation using the block bone graft, soft tissue augmentation was performed. Under local anesthesia (2% Xylocaine with 1:80,000 adrenaline), the recipient site was exposed with crestal incisions extending from region 33 to 43. A subepithelial connective tissue graft was harvested from the donor site in relation to the 14, 15, 16 region. The graft was trimmed and positioned appropriately onto the recipient site [Figures 8 and 9]. Vestibuloplasty was performed extending from region 33 to 43. The flap was repositioned and sutured with 4-0 vicryl. Immediate postoperative orthopantamograph was taken to see if the graft and screws are secure [Figure 10] instructions were reinforced. Medications including antibiotics and analgesics were prescribed.
Figure 8.
Sub-epithelial connective graft
Figure 9.
Connective tissue graft from palate
Figure 10.
Immediate postoperative OPG
Implant placement
Six months following the augmentation procedures, an orthopantamograph (OPG) was repeated and increased radiopacity was observed in relation to the alveolar ridge of the lower anterior region, suggestive of the regeneration of an adequate amount and height of the alveolar bone in that region (6 mm×3 mm) [Figure 11]. The microscrew was removed after observing the successful union of the graft in the orthopantamograph. Under local anesthesia (2% Xylocaine with 1:80,000 adrenaline), bilateral mental nerve block and infiltration anesthesia were given in relation to region 31, 41, and 42. Subcrestal incisions were placed and a mucoperiosteal flap was reflected buccally and lingually. Implant osteotomy was performed up to a diameter of 3.2mm and two implants (3.75×13 mm, Lifecare) were placed [Figure 12]. Primary stability of 40 N was achieved [Figure 13] and cover screws were placed. The flap was repositioned and sutured with 3-0 black silk. A periodontal pack was placed. Pressure dressing was given with Dynaplast to avoid subcutaneous hematoma. Postoperative instructions were given. Amoxicillin 500 mg t.i.d and Metronidazole 400 mg t.i.d were given for five days. Anti-inflammatory analgesic Combiflam (Ibuprofen 400 mg + Paracetamol 500 mg) was also prescribed. The sutures and pack were removed after seven days. The patient was rehabilitated with a provisional restoration to restore esthetics [Figure 14].
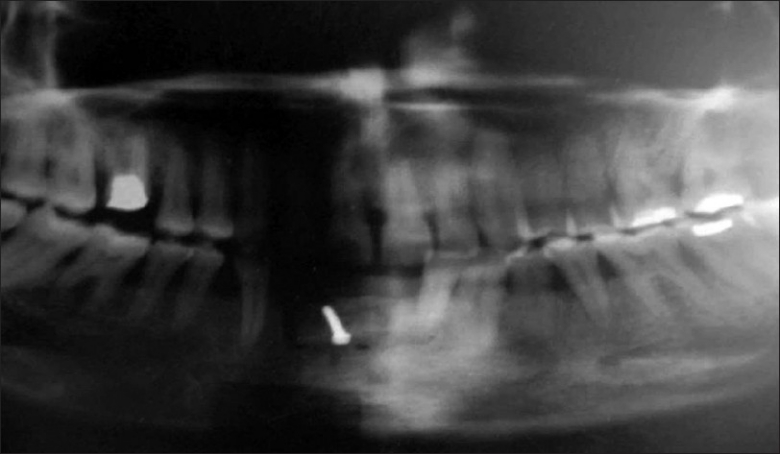
Figure 11.

After six months
Figure 12.
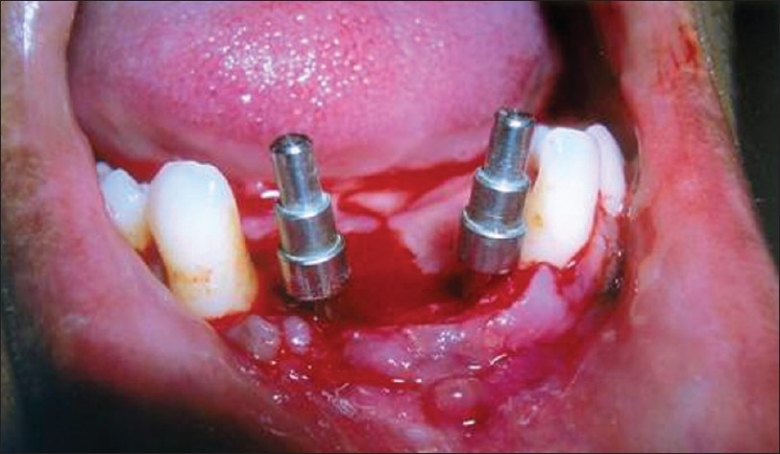
Implant placement
Figure 13.
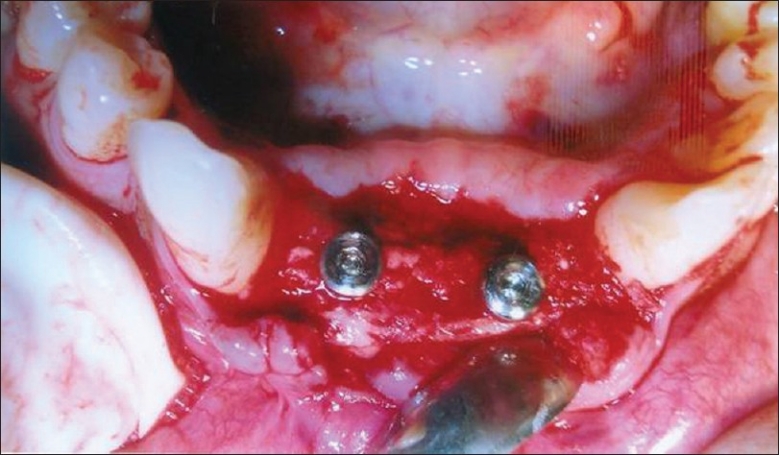
Implants in sound bone
Figure 14.

Provisonal restoration
DISCUSSION
A tooth with a poor periodontal prognosis is no longer a compromise to the esthetics and function of dentition. With the advent of implants, replacement of the extracted tooth with implants has become a predictable treatment modality. Dental implant treatment is a clinically established treatment modality with very good prognosis. However, in advanced stages of generalized periodontitis as in this case report, much of the supporting tissue has been lost. The limitations to the placement of implants in patients with tooth loss due to periodontitis are the inavailability of adequate bone and soft tissue for implant placement. Many different techniques are available for predictable bone augmentation. The approach is largely dependent on the extent of the defect and specific procedures to be performed for implant reconstruction. Surgical techniques to enhance alveolar bone volume include:[2]
Grafting techniques
Distraction osteogenesis
Bone splitting
Guided Bone Regeneration
Although intraoral or extraoral harvesting procedures are possible, intraoral sites have been preferred especially for the treatment of localized bone defects in partially edentulous jaws.[3] One main disadvantage of using autogenous bone grafts is the morbidity associated with the harvesting procedure.[4] Intraorally, the common donor sites include the chin and the area of the retromolar region in the mandible. However, intraoral harvesting procedures also have disadvantages, such as limited availability of bone grafts, complications including altered sensation of teeth, neurosensory disturbances, wound dehiscences, and infection.[4,5]
The uniqueness in this case report lies in the type of autogenous chin graft used for augmentation. Successful augmentation of the height and width was possible because of this J-shaped graft, which was wedged into the defect in such a way that the graft involving the mandible was rotated to form the shape of the arch and the symphysial part was used to augment the defect in width. Augmentation of the alveolar bone with such an inlay–onlay bone graft often provides the desired gain of bone, which allows for the ideal placement of dental implants, and improves esthetics phenomenally.
Compared with other bone graft materials, autogenous bone is considered the best bone graft material because it is osteogenic, in addition to being osteoconductive. Furthermore, there is no risk of rejection or adverse reaction to the graft material when it is autogenous.
Nonetheless, risk of morbidity due to the surgical procedure such as bleeding and nerve injury must be avoided by careful, atraumatic surgical procedures, avoiding the anatomical structures and ensuring that the bone is not overheated. Exceeding 47°C is known to cause bone necrosis.[6] Studies by Hunt and Jovanovic, in 1999,[7] have reported minimal postoperative complications in harvesting block grafts, which is supported by studies by Cordero et al., in 2002,[8] who have achieved a mean lateral augmentation bone grafting of about 6.5±0.33 mm, with no major complications recorded at the donor or recipient sites. In our case report, an increase in height of 3 mm and a width of about 6mm was achieved after six months. However, surgical complications associated with the unfavorable anatomical structures and the necessity of large donor sites (e.g., symphysis and ramus buccal shelf)[9] had led to the use of allogenic grafting materials such as corticocancellous allograft blocks.[10]
The morphology of the soft tissues at the site of bone regeneration also has a significant impact on the result of treatment. Although soft tissue coverage is mandatory for successful bone augmentation, in areas where esthetics is of prime concern, careful determination of soft tissue morphology is important. In many situations, the availability of soft tissues will limit the amount of bone formation possible. The lack of soft tissue may retard bone volume gain, as complete soft tissue coverage of the augmented bone fails. In this scenario, it is better to perform soft tissue volume augmentation and perform bone augmentation as a second step.
Future outlook
Newer materials comprised of a matrix with optimal cell in-growth capacities and good mechanical properties providing space for tissue regeneration including growth and differentiation factors are in the research stage.
CONCLUSION
Various techniques and materials for alveolar ridge augmentation are available today, but it is most appropriate to use an evidence-based approach when a treatment plan is being developed for bone augmentation cases. Moreover, when bone augmentation for implant placement is considered, various biological principles should be followed for a predictable outcome. Proper examination and diagnosis, treatment planning, careful execution of the surgical procedures, postoperative follow-up, and appropriate implant loading are all important factors in achieving success. It is thus evident that for implant restorations with optimal function and esthetics, an interdisciplinary team approach is mandatory.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lekholm U, Adell R, Lindhe J, Brånemark PI, Eriksson B, Rockler B, et al. Marginal tissue reactions at osseointegrated titanium fixtures.(II) A cross sectional retrospective study. Int J Oral Maxillofac Surg. 1986;15:53–61. doi: 10.1016/s0300-9785(86)80011-4. [DOI] [PubMed] [Google Scholar]
- 2.Hammerle CH, Jung RE, Feloutzis A. A systematic review of the survivial of implants in bone sites augmented with barrier membranes in partially edentulous patients. J Clin Periodontol. 2002;29:226–31. doi: 10.1034/j.1600-051x.29.s3.14.x. [DOI] [PubMed] [Google Scholar]
- 3.Joshi A, Kostakis GC. An investigation of Post-operative morbidity following iliac crest bone harvesting. Br Dent J. 2004;196:169–71. doi: 10.1038/sj.bdj.4810945. [DOI] [PubMed] [Google Scholar]
- 4.Nkenke E, Schultz-Mosgau S, Radespiel-Tröger M, Kloss F, Neukam FW. Morbidity of harvesting of chin grafts: A prospective study. Clin Oral Implants Res. 2001;12:495–502. doi: 10.1034/j.1600-0501.2001.120510.x. [DOI] [PubMed] [Google Scholar]
- 5.Von Arx T, Hafliger J, Chappuis V. Neurosensory disturbances following bone harvesting in the symphysis: A prospective clinical study. Clin Oral Implants Res. 2005;16:432–93. doi: 10.1111/j.1600-0501.2005.01138.x. [DOI] [PubMed] [Google Scholar]
- 6.Erikkson RA, Albrektsson T. The effect of heat on bone regeneration:an experimental study on the rabbit using the bone growth chamber. J Oral Maxillofac Surg. 1984;42:705–11. doi: 10.1016/0278-2391(84)90417-8. [DOI] [PubMed] [Google Scholar]
- 7.Hunt DR, Jovanovic SA. Autogenous bone harvesting: a chin graft technique for particulate and monocortical grafts. Int J Periodontics Restorative Dent. 1999;19:165–73. [PubMed] [Google Scholar]
- 8.Cordaro L, Amade DS, Cordaro M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin Oral Implants Res. 2002;13:103–11. doi: 10.1034/j.1600-0501.2002.130113.x. [DOI] [PubMed] [Google Scholar]
- 9.Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12:767–76. [PubMed] [Google Scholar]
- 10.Pendarvis WT, Sandifer JB. Localised ridge augmentation using a block allograft with subsequent implant placement: A case series. Int J Periodontics Restorative Dent. 2008;28:509–15. [PubMed] [Google Scholar]


