Abstract
Inflammation is a complex, non-linear process central to many of the diseases that affect both developed and emerging nations. A systems-based understanding of inflammation, coupled to translational applications, is therefore necessary for efficient development of drugs and devices, for streamlining analyses at the level of populations, and for the implementation of personalized medicine. We have carried out an iterative and ongoing program of literature analysis, generation of prospective data, data analysis, and computational modeling in various experimental and clinical inflammatory disease settings. These simulations have been used to gain basic insights into the inflammatory response under baseline, gene-knockout, and drug-treated experimental animals for in silico studies associated with the clinical settings of sepsis, trauma, acute liver failure, and wound healing to create patient-specific simulations in polytrauma, traumatic brain injury, and vocal fold inflammation; and to gain insight into host-pathogen interactions in malaria, necrotizing enterocolitis, and sepsis. These simulations have converged with other systems biology approaches (e.g., functional genomics) to aid in the design of new drugs or devices geared towards modulating inflammation. Since they include both circulating and tissue-level inflammatory mediators, these simulations transcend typical cytokine networks by associating inflammatory processes with tissue/organ impacts via tissue damage/dysfunction. This framework has now allowed us to suggest how to modulate acute inflammation in a rational, individually optimized fashion. This plethora of computational and intertwined experimental/engineering approaches is the cornerstone of Translational Systems Biology approaches for inflammatory diseases.
Keywords: Inflammation, mathematical modeling, translational research, systems biology, computational biology
Inflammation, Complexity, and Translation
Inflammatory diseases include infection/sepsis, trauma, inflammatory bowel diseases, chronic wounds, rheumatologic disorders and asthma; many other diseases, such as cancer, diabetes, atherosclerosis, Alzheimer’s, and obesity are also associated with dysregulated inflammation. The U.S. National Institutes of Health (NIH) Roadmap Initiative has recently emphasized the need to apply systems biology methods to the study of inflammation [1]. The acute inflammatory response to biological stress (e.g., infection or tissue injury/damage) involves a cascade of events mediated by a large array of cells (e.g., mast cells, macrophages, neutrophils, natural killer cells, dendritic cells, and T- and B- lymphocytes) and molecules (inflammatory cytokines, free radicals, and Damage-Associated Molecular Pattern molecules [DAMPs]) that locate invading pathogens or damaged tissue, alert and recruit other cells and molecules, eliminate the offending agents, and finally restore the body to equilibrium [2].
Inflammation may also be driven by slower degenerative processes that share many common mediators with acute pro-inflammatory insults [3]. Inflammation causes damage to tissues, which in turn leads to the production of molecules that re-stimulate inflammation. This feedforward loop can lead to persistent, dysregulated inflammation that promotes organ dysfunction and death [4].
And yet, inflammation is not in and of itself detrimental. It is in most cases a well-coordinated communication network operating at an intermediate time scale between neural and longer-term endocrine processes [5,6]. Inflammation is necessary for the removal or reduction of challenges to the organism and subsequent restoration of homeostasis [5]. For example, we have recently found that plasma levels of the early inflammatory cytokine tumor necrosis factor-α (TNF) were significantly elevated within 6 h post-admission in 19 human trauma survivors vs. 4 non-survivors. Moreover, plasma TNF was inversely correlated with indices of organ dysfunction, both in the 23 patients taken together and in the survivor cohort.
Furthermore, swine exhibiting a robust TNF response following two different, clinically realistic trauma/hemorrhage paradigms, survived these insults, and those animals that did not mount an adequately robust TNF response died [7]. This requirement for robust early inflammatory responses may represent a means of communicating the extent of injury and perhaps also of preparing the body for a possible secondary infection. Indeed, in the setting of infection (e.g., malaria), TNF and interferon-γ responses help protect the host from infection [8–10]. However, hemorrhage and trauma, perhaps combined with failed attempts at therapy [11,12], can induce a long-term, dysregulated inflammatory response that affects several organ systems and sets in motion a vicious cycle of inflammation→damage→inflammation (see below) [5,13–17]. Thus, although the inflammatory response is pivotal in clearing invading organisms and offending agents and promoting tissue repair, these same responses carried out under a set of extreme conditions can also compromise healthy tissue and further exacerbate inflammation [5,18]. The question, then, is how do we harness the beneficial effects of inflammation and simultaneously keep inflammation below the threshold at which it becomes self-sustaining?
The acute inflammatory response is generally recognized as a complex system, based on the structure, behavior, and multifaceted roles described above. Biocomplexity refers to distinctive aspects of the structure, organization and behavior of biological systems, such as nonlinear dynamics due to multiple feedback loops, multi-scale emergent properties, robustness to perturbation (often coupled to surprising fragility at points of control), and non-intuitive, paradoxical behavior [19–21]. Both inflammation and associated processes (e.g. apoptosis and organ damage/dysfunction) have been studied at the molecular and cellular levels [22–32] and at the tissue and organ levels [33–40], including quantitative insights into the biology underlying experimental paradigms of acute inflammation in animals [41–43].
Translational research aims to apply scientific discoveries in basic science into clinical practice in order to improve healthcare [44]. Both the United States Food and Drug Administration in its “Critical Path” document [45] and the United States National Institutes of Health, in its “Roadmap” statement [46] have explicitly highlighted the need for multi-disciplinary teams utilizing computational technology to bridge the gap between mechanistic knowledge obtained from basic science research, as well as the translation of that knowledge via the development of effective clinical regimens. Accordingly, we have put forth the concept of “Translational Systems Biology” [4,6,47,48], which includes computational simulations of clinical trials [49,50,50–52], clinical diagnostics, streamlined usage of experimental animals [53], and rational device design [54]. In the context of inflammation, a large portion of Translational Systems Biology work has been carried out under the aegis of the Society of Complexity in Acute Illness (http://www.scai-med.org) and at the Center for Inflammation and Regenerative Modeling (www.mirm.pitt.edu/cirm).
Translational Systems Biology approaches strive to create a rational framework for traversing the current “fragmented continuum” of healthcare delivery, in which the domains of pre-clinical studies, clinical trials, in-hospital care, and eventual long-term care are separate [55]. Translational Systems Biology calls for the creation of models that are generated with an a priori focus on rapid translational application in areas such as in silico clinical trials, patient diagnostics, rational drug design, and long-term rehabilitative care [4,6,47,48,55].
More recently, we have expanded this definition to include a broader understanding and systems view of complex multi-host/pathogen interactions, as is the case in malaria [56,57]. While Translational Systems Biology methods have relied heavily on mechanistic computational simulations using equation-based [4,48,50,55] and agent-based [4,48,50,55,58] models, we have also begun to incorporate data-driven methods into this framework [55]. We refer the reader to the above references, as well as others of relevance for data-driven modeling of biological systems [59], for extensive discussions of the merits and pitfalls of the various computational methods used in the work discussed herein.
We have focused much of our mechanistic modeling work on the positive feedback loop of inflammation→d amage→inflammation [4]. Our overarching hypothesis is that DAMPs, (also known as “alarm/danger signals”) propagate inflammation in both infectious and sterile inflammatory settings using similar signaling pathways [4,17,60] and act as integrators of the inflammatory response and surrogates for an individual’s health status. The mechanistic emphasis of our simulations allows us to predict both inflammatory trajectories and morbidity/mortality outcomes [4].
Below, we discuss examples of how Translational Systems Biology approaches are being applied to the study of inflammation in various settings. We first examine studies utilizing data-driven and mechanistic modeling at the molecular/cellular level and at the tissue level. We then discuss how multi-scale modeling techniques are helping in the crucial process of translating modeling studies at the molecular and tissue levels to clinical useful insights at the whole-animal level, as well as the utility of both data-driven and mechanistic modeling at this higher level of organization. These insights include our increasing ability to predict the inflammatory responses of individuals.
We then describe population modeling studies aimed at streamlining a key process in clinical translation, namely the clinical trial. We next discuss modeling studies aimed addressing an emerging area of interest in many fields, namely the complex host-pathogen ecology. Finally, we touch on the interface of in silico and synthetic biology, in which modeling studies are central to the rational design of drugs and devices targeted at the inflammatory response.
Integrating Data-Driven and Mechanistic Modeling of Intracellular Processes
Much of the past work on Translational Systems Biology of inflammation was carried out using mechanistic modeling, and the computational models for those studies were developed subsequent to a thorough search of the relevant literature. The initial step in the development of these computational models, whether generated using equation- [4,6,50,61–64], agent- [4,6,50,58,65,66], or rule-based [67,68] computational techniques, was to integrate literature-derived information after a thorough evaluation/survey to determine a consensus on well-vetted mechanisms of inflammation.
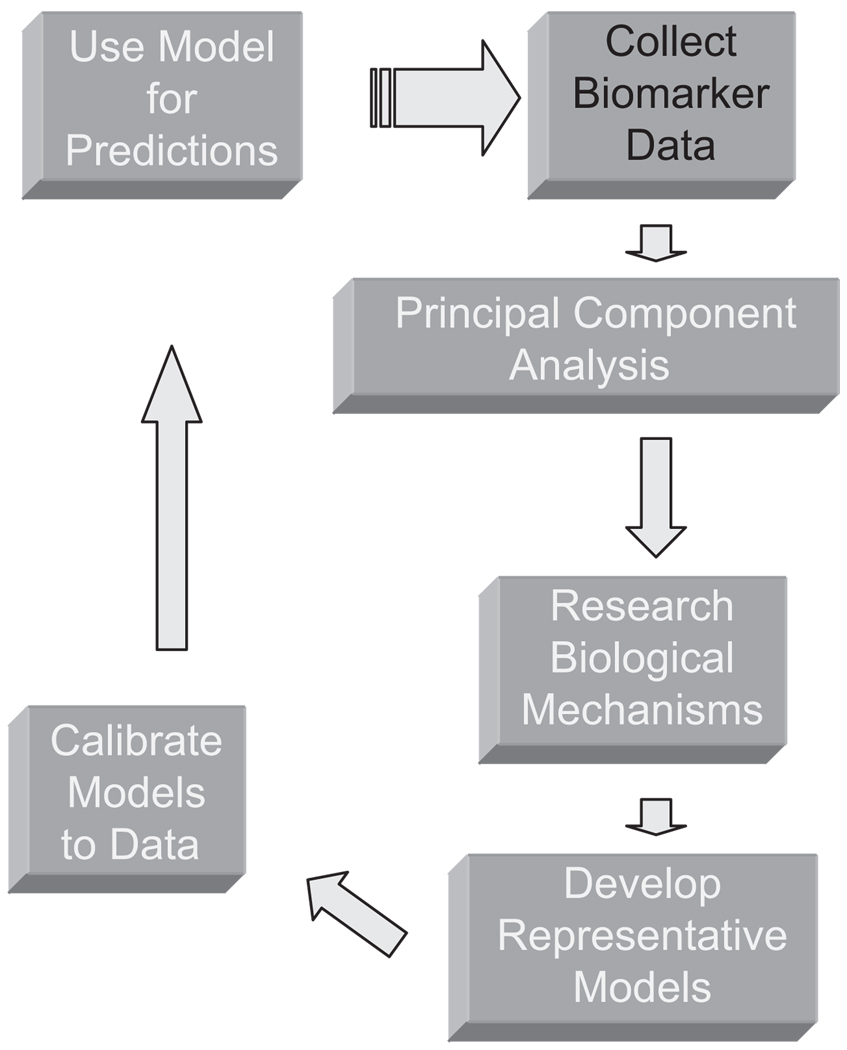
More recently, we have sought to utilize data-driven approaches applied to prospective datasets representing the dynamics of inflammatory analytes, not only in order to avoid possible bias in selection of variables and mechanisms to include in mechanistic models, but also as an adjunct means for systems-based discovery. We have begun to adopt an iterative process to which we had previously referred as “evidence-based modeling” [53,69], consisting of biomarker assay, data analysis/data-driven modeling to discern main drivers of a given inflammatory response [59], literature mining to link these principal drivers based on well-vetted and likely mechanisms, calibration to the original data, and then validation using data separate from the calibration data (Figure 1).
Figure 1.
Evidence-based modeling. Initial model components are determined from experimental data using Principal Component Analysis. Subsequently, model building follows an iterative process involving calibration from existing or new data, and validation from prediction of data. This process identifies both areas where a model is correct and where it is deficient relative to data and therefore must be corrected.
Data-driven methods [50,59,70], including network-based approaches [59,63,71–85] have indeed proven to be quite useful in systems biology applications. Principal components are orthonormal linear combinations of the data vector, with the property that they carry the largest variances in several orthogonal directions. This is a method that reduces the dimensionality of a problem by concentrating on just a few (usually up to five or six) statistically most significant orthonormal linear combinations. These combinations are called the leading principal components.
Principal Component Analysis (PCA) has been used in various systems biology applications, among them attempting to define the main drivers of a biological phenomenon. For example, Janes et al.. described the use of PCA to gain insights into the primary drivers of inflammation and apoptosis in an in vitro setting [86]. As a further example of the application of PCA to inflammation in an in vitro context, we have recently employed this technique to aid in determining the subset of variables that appears to drive a given inflammatory response. Cell supernatants from freshly isolated mouse hepatocytes were exposed to 1% hypoxia for various periods of time. These samples were then analyzed for the presence of 20 inflammatory cytokines and chemokines. In this study, ∽96% of the variance in the data could be described by a vector combination consisting predominantly of the chemokines KC, MIP-1α and MIG (Namas et al.., manuscript in preparation). Prior studies had suggested that KC is important to the outcome of trauma/hemorrhage in experimental animals [87]; our results point to hepatocytes as a likely cellular source of this chemokine.
In parallel to the data-driven analyses described above, mechanistic modeling was utilized to study pro-inflammatory signaling mechanisms. It is now appreciated that one mechanism by which the host can recognize both pathogen-derived products and DAMPs is via the Toll-like receptor (TLR) pathway and DAMP ligands such as HMGB1 [88–94]. Of the various TLRs, TLR4 appears to be central to the response to both bacteria and endogenous danger signals [60], yet much remains to be elucidated about its regulation in various inflammatory states [60,95–102].
Equation-based modeling [103,104], agent-based modeling [105], and rule-based modeling [106,107] were utilized to study signaling following aggregation of TLR4. These models reproduced various features of inflammatory signaling induced by bacterial lipopolysaccharide (LPS), including preconditioning, the effect of past history on a system’s behavior, which is a critical feature of many biological processes including the inflammatory response. Stimulation with two or more pro-inflammatory stimuli in succession can lead to responses that are equal to, greater than, or lesser than each stimulus in isolation. This feature may have critical relevance, since a therapeutic preconditioning stimulus might someday be used to augment natural inflammatory protective responses to a subsequent severe insult, or to blunt an overly-exuberant (and hence detrimental) inflammatory response [4].
Our ongoing goal is to unify a broad array of published and prospective in vitro studies of inflammation using techniques such as PCA to derive mechanistic models. We suggest that such models, driven initially by data but leveraging the power of mechanistic simulations, can lead to insights at the tissue, organ, and whole organism levels.
Mechanistic Modeling at the Tissue Level
Acute inflammation damages tissue, leading to the production of DAMPs that re-stimulate inflammation [17,108]. This feed-forward loop can lead to persistent, dysregulated inflammation that promotes organ dysfunction and death, though with a wide range of phenotypic features, as observed in sepsis, trauma, infectious diseases such as malaria, and cancer [4,109]. We have begun to address these complex issues in isolated tissues by using computational simulation in the setting of diabetic foot ulcers [110] and injured vocal folds [111]. We carried out this work largely using agent-based modeling.
We have recently created a new software platform for ABM, which we call SPARK (Simple Platform for Agent-based Representation of Knowledge; [112], a Java-based, open-source, parallel-enabled software that includes the ability to simulate agents of diverse sizes and shapes, can model three-dimensional space, and that contains advanced particle effects. Using the SPARK modeling environment, we created an ABM of a slice of liver tissue that can become infected with hepatitis C virus (HCV) or damaged in a sterile fashion that simulates exposure to toxic chemicals, and that through prolonged exposure to inflammation induced by these stresses can develop hepatocellular carcinoma (HCC) [58]. This ABM was calibrated qualitatively based on published literature data regarding the dynamics of cell populations and cytokines and their influence on inflammation and the early stages of HCC caused by chronic HCV infection, as well as published models of the effect of these inflammatory response elements on already established HCC. This ABM simulates the onset and progression of HCC in a patch of liver, arising from only a few cells (hypothetical cancer stem cells). The tissue environment of pro- and anti-inflammatory responses present in chronic infections, such as HCV, accelerates tumor formation. Associated processes are also modeled, including the formation of a hypoxic core in the center of the growing tumor, as well as tumor angiogenesis [58].
Additionally, we have examined the pathophysiology of Respiratory Syncytial Virus (RSV) infection. RSV is a common cause of bronchiolitis and pneumonia, and has been implicated in the pathogenesis of childhood asthma and reactive airway disease. The dynamics of viral replication in the lungs and the subsequent vigorous inflam-matory responses against RSV are critical and complex elements in the progression to respiratory diseases.
Computational simulation is a means of untangling some of this complexity, as has been done previously in the setting of influenza using equation-based models [113]. Accordingly, we developed an ABM that simulates innate immune activation induced by RSV in a small patch of ciliary epithelial cells. Our goal is to explain the tissue-level physiological derangement in terms of complex inflammatory cascades.
Central to the ABM is the positive feedback loop of tissue damage→inflammation→tissue damage, where “tissue damage” is mediated by DAMPs such as HMGB1 (a marker of the adverse effects of inflammation, as well as a driver for further inflammation). Our simulations suggest that even when the virus is cleared after an episode of acute infection, both pro- and anti-inflammatory cytokines remain elevated at later time points due to this positive feedback loop. The strength of the initial viral infection influences the inflammatory response, and subsequent viral clearance, in a nonlinear fashion. Interfering with viral replication (simulated treatment protocol) can also affect long term disease severity and downstream pulmonary abnormalities. Mapping clinical observations of cytokine levels during respiratory disease to our model may help translate mechanistic knowledge into the development of therapies for patient treatment.
Multi-Scale, Multi-Tissue Mechanistic Modeling: From Moleculeto Human
One of the primary challenges in effective translation of basic mechanistic knowledge is placing the reductionist-derived knowledge back into a clinical context. This reintegration of knowledge represents the essential challenge in the biomedical research community. Our goal is to utilize modeling to concatenate molecular, cellular, and tissue data into a whole-organism context, and to do so we have utilized multi-scale, multi-tissue model architectures. The primary example of this is the integration of intracellular signaling and synthetic pathways related to inflammatory signaling and the maintenance of epithelial barrier integrity into an ABM that reproduces a clinically relevant scenario of organ-organ crosstalk [114,115]. In this model, some of the intracellular modeling methods employed above [105,107] were used to produce rules that were encapsulated into a cell-level ABM that reproduced the function of gut and pulmonary epithelial barrier function with response to inflammatory stimuli. These tissue models were subsequently integrated with an endothelial-inflammatory cell ABM [37,52] to simulate the hollow organ morphology of both the gut and the lung. In this fashion, the ABMs were able to link two leading hypotheses for sepsis and multiple organ failure: that of epithelial barrier failure [116] and that of diffuse endothelial activation [117,118].
These two organ-level ABMs were then linked to model the gut-pulmonary axis of systemic inflammation, and the resulting ABM was able to reproduce clinical time courses for the development of acute respiratory distress syndrome (ARDS) secondary to mesenteric ischemia, as well as suggesting a cellular damage by-product as source of the pro-inflammatory mediator present in the mesenteric lymph [114]. This degree of multi-scale representation, from intracellular signaling and gene regulation to clinically relevant systemic behavior, demonstrates the capacity of translational computational modeling to synthesize mechanistic hypotheses from multiple scales into a single model. Below, we discuss modeling studies carried out at the whole-animal level and the translational insights derived from them.
Integrating Data-Driven and Mechanistic Modeling at the Whole-Animal Level
Similar to the in vitro settings described above, PCA was used in various inflammatory settings in vivo. For example, Daun et al. used a variant of PCA to reduce the dimensionality of the set of parameters that were allowed to vary for achieving a best fit of model trajectories to data obtained from endotoxemic rats [119], highlighting another practical application of this methodology for the process of mechanistic modeling (Figure 1).
More recently, we utilized multiplexing cytokine analysis coupled with statistical modeling to gain further insights into the inflammatory response to T/HS. Mice were subjected to surgical cannulation with or without subsequent hemorrhagic shock, using a computerized, closed-loop system [120]. The eight experimental groups were: a) 1, 2, 3, or 4 h T alone and b) 1, 2, 3, or 4 h of T/HS (25 mmHg). Plasma was assayed for 20 cytokines and NO2−/NO3−. PCA was carried out to determine the primary inflammatory drivers of inflammation in trauma alone vs. trauma/hemorrhagic shock. These studies pointed to MIG, IL-6, IL-10, IP-10, IL-12, TNF, and KC as potential differentiators of these two responses (Constantine et al., in preparation). Interestingly, hierarchical clustering analysis of these data was also carried out, and showed overlap between the inflammatory response to trauma vs. trauma/hemorrhagic shock, in support of our previous, modeling-derived findings [43]. Despite this overlap, multivariate modeling was carried out to determine if sham cannulation could be differentiated from cannulation followed by hemorrhagic shock based on cytokine profiles.
The most significant cytokines involved in the model were IL-12 (p40/p70), MIG, and KC. Based on this model, we were able to correctly differentiate between the trauma and trauma/hemorrhagic shock 80 to 88% of the time. Equation-based mechanistic models of inflammation induced by surgical trauma alone or in combination with hemorrhage could also distinguish these two responses [41,43,120]. Finally, these results concurred with our findings described above, namely that KC is produced by hepatocytes in settings of hypoxia/ischemia (which occurs in the process of hemorrhagic shock [119,121].
Combined in silico/in vivo studies in mice [41–43,120] and rats [119] have yielded many insights with regard to inflammation at the whole animal level, and are reviewed extensively elsewhere [4,6,50,53,55]. In addition, swine represent an attractive pre-clinical species due to their physiological similarity to humans and due to the ease of obtaining serial blood samples as well as continuous physiological measurements. We sought to determine the principal drivers of inflammation in porcine endo-toxemia and to model the process mathematically. We also sought to determine and model the time evolution of matrix metalloproteinases (MMPs).
Swine were subjected to endotoxemia, and serial plasma samples were assayed for inflammatory cytokines, NO2−/NO3− and MMPs. PCA was carried out in order to discern principal drivers of inflammation in this animal model. An equation-based model that describes the interrelationships among blood pressure, inflammatory cytokines, NO2−/NO3−, MMP-2, MMP-9, and the tissue inhibitors of metalloproteases (TIMPs) was created. Initial calibration of the model utilized literature data, and the model was refined with the data gathered prospectively in porcine endotoxemia. Temporal changes, similar to those observed for endotoxemic mice [41] and rats [119] were observed in all inflammatory analytes. TNF was produced to a high degree in all animals, and appeared to drive the early inflammatory response to LPS.
However, PCA suggested that IL-1β rather than TNF may be a main driver of later inflammation that leads to lung injury in this experimental preparation. The mathematical model was capable of describing the dynamics of inflammatory analytes in swine and predicted qualitative dynamics of MMP-2 and MMP-9 (Vodovotz et al., manuscript in preparation).
Animal models may simulate the human inflammatory response to various degrees [122,123]. However, the human inflammatory response may well be more multidimensional and complex, and the Translational Systems Biology framework is strongly focused on understanding the human condition through studies on human data [6]. As in our prior studies, we have utilized both data-driven and mechanistic models to examine the characteristics of patient sub-groups as well as the responses of individuals.
We used multiplexing cytokine analysis of serial plasma samples, coupled with PCA followed by clustering analysis, in order to gain insights into the inflammatory responses of trauma patients. Twenty-five inflammatory cytokines along with NO2−/NO3− were studied serially in over 80 trauma patients. PCA was used both to reduce this multidimensional dataset and to suggest the subset of mediators that account for the most change, or variability, in the dataset. The variance in the data was characterized by an inflammatory response dominated by GM-CSF, IL-15, TNF, IL-10 and IL-1 receptor antagonist (IL-1ra) for all patients. In survivors, we found that GM-CSF, TNF, IL-10, IL-2, and IL-1ra are the main drivers, whereas in non-survivors IL-1ra, IL-10, IL-1β, IL-6, and TNF appeared to dominate the inflammatory response. Individualized PCA was carried out for 25 trauma survivors in first 24 hours post-trauma, in order to discern individual features of inflammation. We found that IL-1Ra, RANTES, MIP-1β, TNF, and IL-6 dominate in the first component in a large number of these patients. The Injury Severity Score (ISS, an established clinical scoring system) was significantly higher in patients who had TNF and IL-6 in their first component vs. patients who did not have these two cytokines as their principal component. Moreover, clustering based on the weights of the top five cytokines present in the principal components resulted in two large clusters that differed based on their Marshall Score (an index of organ damage; Ghuma et al, manuscript in preparation).
We have employed similar methodology in the setting of pediatric acute liver failure (PALF). The human liver is exposed to a constant barrage of bacterial, viral, pharmacologic, environmental, tissue, and food antigens and toxins via the portal vein and, to a lesser extent, the hepatic artery and must therefore be prepared to recognize and appropriately respond to those challenges. Fortunately, the liver is endowed with a distinctive cellular milieu that provides measured defensive strategies to maintain proper homeostasis [124,125]. A dysregulated or disordered response to these and other challenges would result in disrupted hepatic homeostasis and severe liver injury or liver failure [126]. Acute liver failure is especially devastating in the pediatric setting. Patients with PALF have increased risk for bacterial and fungal infections [127], aplastic anemia [128,129], and impaired cell-mediated and humoral immunity [127].
In some patients with indeterminate PALF, clinical improvement results following treatment with corticosteroids. These observations led us to develop the hypothesis that immune or inflammatory dysregulation is present in PALF and that computational modeling of clinical and inflammatory markers could predict outcome in PALF. We obtained data on cytokines and NO2−/NO3− on sera from four separate PALF patients, and subjected these data to PCA. Our results suggested that we may be able to separate patients based on outcome (survival vs. death) based on this type of analysis (Vodovotz Y, Mi Q, Squires R, unpublished observations). While additional work is needed, these findings raise the potential for multiplexed cytokine analysis coupled with patient-specific PCA as a potential biomarker framework for outcome prediction in inflammatory diseases.
In parallel to the data-driven approaches, we have also employed mechanistic modeling techniques to study the inflammatory responses of individuals. Our first foray into this field was in the setting of vocal fold injury, a process that engenders inflammation and a wound healing response [130]. A possible factor in the poor prognosis of patients that have vocal fold injuries (e.g., from over-use or following surgery) is that vocal fold scars display wide individual variability, hampering efforts to predict disease progression and treatment response across patients [130].
We used an ABM of inflammation and tissue healing, derived from literature on wounded skin as well as vocal folds, to simulate the process of healing in responses to the biomechanical stresses associated with phonotrauma [111]. This model reproduced the basic behavior of the inflammatory and wound healing responses expected in phonotrauma. Individual-specific variants of the model were created based on initial conditions in human subjects experiencing phonotrauma alone or in combination with further spontaneous speech or specialized voice modulation exercises. These modeling studies predicted that the long-term outcomes of wound healing outcomes would be substantially different in individuals exhibiting relatively small differences in the initial magnitude of tissue damage that were associated with the various treatment groups [111]. These results were consistent with data suggesting that large-amplitude/low-impact vocal fold tissue mobilization may actually reduce inflammation following acute phonotrauma [130]. Following this initial foray into constructing patient-specific variants of inflammation models, we have applied similar methods in diverse settings, as discussed below.
Equation-based modeling methods were also used to create patient-specific equation-based models in the setting of polytrauma. Human trauma patients were recruited into an observational study in which blood samples were obtained daily up to 1 week post-admission, then weekly thereafter. Plasma was assessed for TNF, IL-6, IL-10, and NO2−/NO3−. Trauma was modeled as an exponentially decaying function using the equation-based model developed calibrated originally using data from mice. [41]. The coefficient of the trauma function was scaled from 1–2 with 1 corresponding to the lowest ISS, and 2 to the highest ISS for any patient. The rate constants of the equation-based models that relate to generation of TNF, IL-6, IL-10, and NO2−/NO3− were estimated to fit the time course data of individual patients. Using this methodology, the resultant patient-specific models accurately predicted patient survival when ISS alone could not (Sarkar et al., unpublished observations).
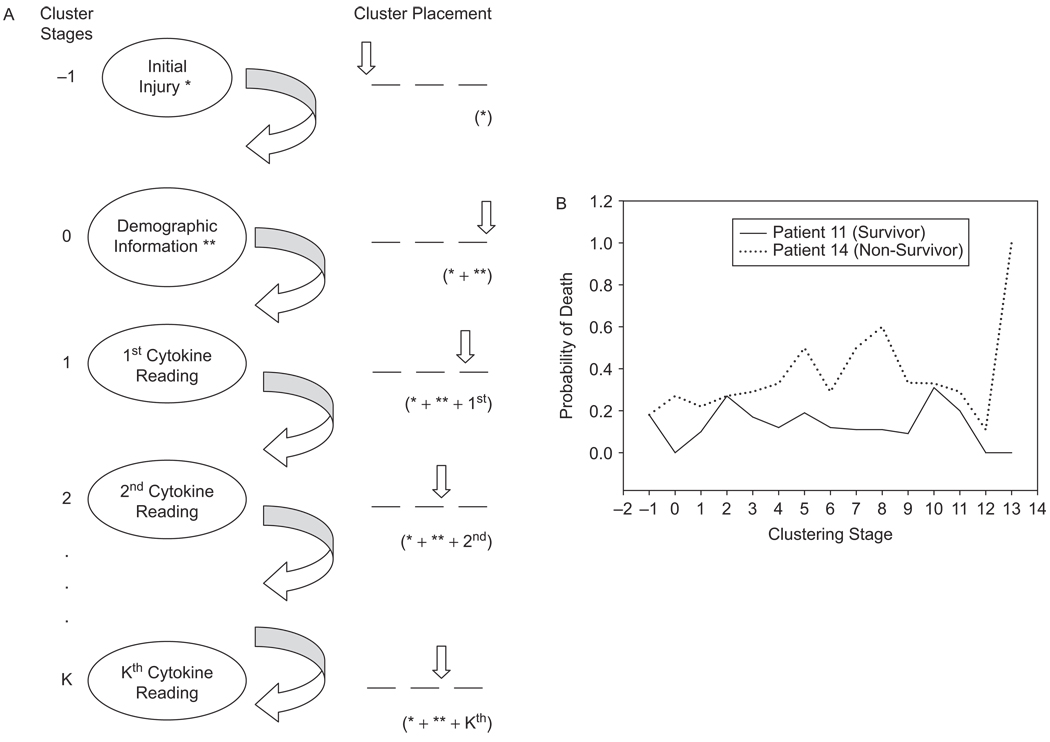
Similarly to polytrauma, inflammation induced by traumatic brain injury (TBI) can lead to both morbidity and mortality. We sought to develop data-driven models in order to predict outcomes post-TBI. Thirteen inflammatory cytokines were determined in serial cerebrospinal fluid samples from 27 TBI patients. The Glasgow Coma Scale (GCS) quantifies the nature of the initial brain injury on a numerical scale from 3 to 15. The time series variables varied both in length and in the time sequence at which they were collected. The Glasgow Outcome Score (GOS), the outcome variable, was taken as the variable to express, and predict, outcome as a function of the other input variables. Data on each subject, consisting of ten clinical (one-dimensional) variables, such as age, gender, and presence of infection, along with cytokine time series, were used to generate both multinomial logistic as well as probit models that predict low or high levels of GOS. In addition, a technique called “Dynamic Profiling” was developed, in which patients were clustered using Hartigan’s k-means method into disjoint groups at different stages of disease progression after the initial TBI (Figure 2A).
Figure 2.
Dynamic Profiling and its application to traumatic brain injury. Panel A: Dynamic Profiling is a novel technique that involves clustering subjects into disjoint groups based on initial and time-dependent changes in subject-characteristics, in order to predict outcomes of individuals. A cluster is a subset of subjects that share similar characteristics. In the specific case of traumatic brain injury (TBI), we utilize patient demographics (age, gender, severity of injury) along with the sequential change in cytokines over time in order to cluster patients. Panel B: application of Dynamic Profiling to predict outcomes in individual TBI patients. The probability of mortality as a function of clustering stage was predicted using Dynamic Profiling for Patients 11 and 14 (see text for details), which had similar initial cluster placements but for whom subsequent clustering suggested divergent trajectories with regard to probability of survival.
Initial clustering was based on GCS, and subsequent clustering was performed based on demographic information and then further, sequential clustering based on the levels of individual cytokines over time. These clusters assess the risk of death of a new patient after each cytokine reading, based on the existing information in the previous data in the cluster to which the new patient belongs at the time. The probability of death associated to a cluster after the kth cytokine reading is the ratio of patients who died to the total number of patients in that cluster (Figure 2A). We also use a prior distribution on mortality, which is then updated by the incoming data, for a Bayesian approach to Dynamic Profiling. A predictive logistic model for low (3 or less) or high levels (4 or more) of the GOS response, involving a full TNF effect and both linear and quadratic effects of IL-10, was obtained by using 80% of the available data and tested on the remaining 20%.
Using the Dynamic Profiling method, we suggest that clinical interventions be made at time points where the cluster to which a new patient belongs carries a low probability of survival based on the GOS outcomes associated to that cluster. A new subject may be steered, through clinical or surgical interventions, toward a cluster with as favorable a weight as possible. We illustrate the process of Dynamic Profiling in the setting of TBI with two patients (Figure 2B). Both subjects (11 and 14) belong to the same cluster, since subject 11 had a GCS score of 6, while subject 14 has GCS score 7. Despite this close ranking, patient 11 recovered with a GOS of 4, while patient 14 died. At Stage 0 clustering, when non-cytokine clinical and demographic variables were used to cluster (in addition to the GCS), subject 11 was placed in a cluster that had no deaths, while subject 14 was placed in the worst cluster (in which the chances of death were approximately 25–30%). With each subsequent clustering event, the probability of mortality for subject 14 increased (Figure 2B). These modeling-based studies suggest that interventions at certain times during the course of his or her hospital stay could potentially steer the patient toward a path to recovery from TBI.
We also utilized these same data on TBI patients for mechanistic modeling using ordinary differential equations. PCA suggested that the primary drivers of inflammation in TBI were TNF, IL-6, IL-10, MIP-1α, MIP-1β, and IL-8, and accordingly 27 patient-specific models were fit to these data. When comparing the prediction of damage vs. GOS as outcome, we achieved 60% prediction accuracy (16/27 patients) in our preliminary attempts. Ongoing studies include the generation of ensembles of models for each patient dataset, alternative models of TBI-induced inflammation, and various parameter fitting approaches.
Mechanistic Modeling at the Population Level: In Silico Clinical Trials
Clinical trial simulations are a central component of Translational Systems Biology [49,50,52,54] These simulations can be used as platforms to test the “proof of concept” of a candidate intervention, as well as instantiating narrowly defined mechanisms of action at the cellular/molecular level in a context that re-establishes their possible clinical significance. We have utilized both equation-based [49] and agent-based [52] models to carry out simulated clinical trials of a prototypical failed antisepsis therapy that had a promising pre-clinical profile, namely neutralizing anti-TNF antibodies [131,132]. These studies provided a degree of subgroup analysis not readily feasible in a “real-world” clinical trial, and suggested ways in which these trials may have been improved (and perhaps have succeeded) by judicious patient selection.
As a further example of the ability of our model to simulate clinical reality, we generated an in silico trial of 100,000 “cases” subjected to randomized levels of trauma and hemorrhage. The “patients” exhibited the same random characteristics described above, except that antibiotic was not “administered”. We carried out the simulation for 48 h to assess the qualitative validity of our model in the setting of acute, trauma-induced mortality. Death was defined as exceeding a certain threshold of damage/dysfunction, and over 3,000 simulated patients fit that criterion. We examined the characteristics of the “patients” that died, and found that, in agreement with published studies in both rodents and humans, death tended to occur in those cases in which IL-6 (examined at 6 h) [133] as well as early hypotension [134], were evident [50].
We also simulated a series of anti-mediator clinical trials from the 1990s (including anti-TNF and anti-IL-1 regimens), along with hypothetical, multi-mediator therapies [52]. The interventions all represented manipulations of the intrinsic mediators represented in the model, (i.e. TNF, IL-1, GCSF and CD-11b/CD18) with the assumption that the drugs performed exactly as they had been intended from a mechanistic standpoint.
None of these interventions performed as had been hoped, with no significant improvement in survival, matching what was observed in the clinical trials [52]. The significance of this finding is the implication that these computational models can be used as means of dynamic knowledge representation for hypothesis visualization and verification [114]. In short, had there been the ability to evaluate the dynamic consequences of the then state-of-the-art mental models of inflammation, the basic conceptual flaws underlying the design of those therapies would have been evident prior to the execution of those clinical trials. The use of computational models in this fashion represents a vital aspect in the step-wise translation of knowledge from the bench to the bedside, and can be used at multiple points in the translational process [105,107,114,135].
We also applied agent-based modeling and simulated clinical studies to the case of tissue trauma, inflammation, and wound healing in the setting of chronic, non-healing diabetic foot ulcers (DFU) [110]. An ideal therapy for DFU should suppress excessive inflammation while enhancing the production of cytokines that enhance healing, and our simulations suggested ways in which this goal could be achieved. We also utilized the inherently stochastic features of agent-based modeling [6,48,50] to examine both the variability in a simulated population of DFU patients as well as the likelihood of therapeutic efficacy of existing (debridement, platelet-derived growth factor) and novel (anti-TNF, active or latent TGF-β1) therapies for DFU.
More recently, we have carried out simulated clinical trials of vaccination in the setting of inhalational anthrax, and suggested settings under which the combination of vaccination and antibiotic administration might be either useful or detrimental [51]. We have also worked to integrate modeling into actual trial design [53]. For example, equation-based models were able to produce a simulated placebo arm for an open-label Phase IV drug trial, with the goal of providing a means of comparison between the Phase IV and its preceding Phase III trial [136]. These more comprehensive models of inflammation and its effects on various aspects of physiology were used to prospectively predict the outcome of a phase III clinical trial, including predictions of the responses of patient sub-groups as well as risk stratification within the treatment protocol (J. Bartels, J. Sarkar, and S. Chang, unpublished data). These accomplishments suggest that the Translational Systems Biology approach may someday become a major component of the design and implementation of clinical trials.
Mechanistic Modeling of Host-Pathogen Ecology
Malaria, caused by the parasite Plasmodium falciparum and spread by the female Anopheles mosquito, affects 350–500 million people each year and kills 2 million. An intricate immune cross-talk occurs between the mammalian and anopheline hosts for Plasmodium, leading to the control of parasite numbers [56,137]. Key to this process is the mammalian cytokine TGF-β1, a central immune-modulating cytokine that is elevated in infected mammals. A key target of TGF-β1 regulation in the context of mammalian anti-malarial immunity is inducible nitric oxide (NO) synthase (iNOS) [137]. High levels of iNOS-derived NO lead to the activation of latent TGF-β1, which suppresses iNOS expression and limits host pathology. In the mosquito, ingested blood-derived TGF-β1 induces the expression of Anopheles stephensi NOS (AsNOS) and the synthesis of toxic NO reaction products that limit parasite development [56,137]. As in mammals, high levels of NO feed back to limit AsNOS induction [138]. Ingested TGF-β1 also induces the expression of the endogenous mosquito TGF-β superfamily ligand As60A Luckhart and Singh, unpublished).
Successful modeling of this complex biology may predict key signaling elements that can be targeted to block malaria parasite transmission. Accordingly, we have created a mathematical model of the relevant NO-TGF-β1-parasite interactions that occur in the mosquito midgut. Included in our model are (1) active and latent TGF-β1, (2) AsNOS, (3) an influence that represses AsNOS expression (X), (4) a function that accounts for the activation of latent TGF-β1, and (5) a function that accounts for the combined suppression and activation of AsNOS depending on the quantities X and TGF-β1. Since AsNOS expression appears to oscillate with time post-bloodfeeding in experimental systems, we calibrated model parameters to match these oscillations. The resulting simplified model depicts the oscillating expression of AsNOS suggested by our experimental data for a certain period of time.
Based on the results of our simulations and the known existence of the mosquito TGF-β homolog As60A and the known auto-induction of TGF-β1, we hypothesized that TGF-β1 induction of As60A expression may lead to persistently elevated TGF-β1-like activity, which together may act to maintain AsNOS oscillations. Thus, computational simulation of this complex, cross-species cross-talk may yield novel basic and translational insights into the biology, pathology, and ecology of malaria.
Necrotizing enterocolitis (NEC) is a severe disease of the gastrointestinal (GI) tract primarily observed in pre-term babies. Although not entirely understood, NEC is thought to be related to the physiological immaturity of the GI tract and the altered levels of normal flora in the intestines. Understanding the contributing factors of NEC can help suggest treatment strategies for re-establishing the integrity of the epithelial wall and preventing the propagation of inflammation. Several studies have shown a reduced incidence and severity of NEC in neonates treated with probiotics.
We have previously suggested simplified models of inflammation of relevance to NEC [139]. More recently, we used a mathematical model to predict the conditions under which probiotics may be successful in promoting the health of infants susceptible to NEC (Arciero et al., manuscript in preparation). The model was simulated in the presence and absence of probiotic treatment, and the effects of breast-feeding were considered.
In this study, a system of ordinary differential equations was used to track pathogenic and probiotic bacteria in the intestinal lumen and in the blood/tissue regions. The degree of “leakiness,” or permeability, of the intestinal epithelial layer was also treated as a variable. In this simulation, a healthy state corresponds to a low, baseline level of permeability with no bacteria in the blood. The two lumen bacteria species were assumed to leak into the blood/tissue region if they exceeded a given threshold.
Once in the blood/tissue, bacteria invoke an immune response. Injury to the epithelial wall occurs as a consequence of inflammation, and thus permeability increases with macrophage activation. Probiotics are assumed to compete with pathogenic bacteria in the lumen and decrease intestinal permeability. This model predicts that in the presence of probiotics, health is restored in many cases that would have otherwise exhibited sustained inflammation. Although probiotics are typically viewed as helpful, if the growth rate of probiotics increases substantially, permeability and bacteria levels in blood both increase, and the health state is compromised. A sensitive interplay between the strength of the immune response and the positive and negative effects of probiotics is therefore observed, suggesting conditions under which probiotics may be a successful treatment for infants suffering from NEC.
The clinical relevance of the interactions between the gut and its resident bacterial populations is not limited to the premature infant. Gut-derived sepsis is a critical component (perhaps THE critical component) in the management of the adult intensive care population [140,141]. Multiple factors that affect alterations of the host-pathogen relationship in the intensive care setting have immediate clinical relevance: the timing and form of intestinal feeding, the use of antibiotics and subsequent development of resistant strains of bacteria, the competition for scarce resources between resident bacterial populations and resultant shifts in those populations, and the activation of virulence factors in previously benign resident bacterial species [140,141]. This has led to a view of the host-pathogen relationship that draws upon dynamics evident in ecology and social systems [142]. In this paradigm, there are no inert actors; all the components of the system are linked in a dynamic fashion. In particular, the bacterial populations incorporate evolutionarily-derived rules represented in a game theory format. Game theory has been used to study the evolution of traits and strategies by viewing the “state of nature” as an iterated series of encounters [143].
Modeling bacterial survival strategies in this fashion eliminates the presumption that bacteria “intend” to cause disease. Rather, this modeling apporach characterizes bacterial behavior in terms of environment-driven decision-making regarding available survival strategies. This results in extremely robust trajectories in the shift from non-virulence to virulence, and consequently results in a situation that appears resistant to interventions. Computational approaches of this type are likely to be necessary in attempts to develop and test multi-modal treatments for gut-derived sepsis in the critical care population. The lessons learned from these studies may also be linked to other data-driven and mechanistic modeling studies, for example those aimed at reducing the rates of nosocomial infection in hospitals [144,145] as well as the spread of infectious disease such as malaria and influenza [146–154].
Toward the Rational, Systems-Based Modulation of Inflammation: Lessons from Translational Systems Biology
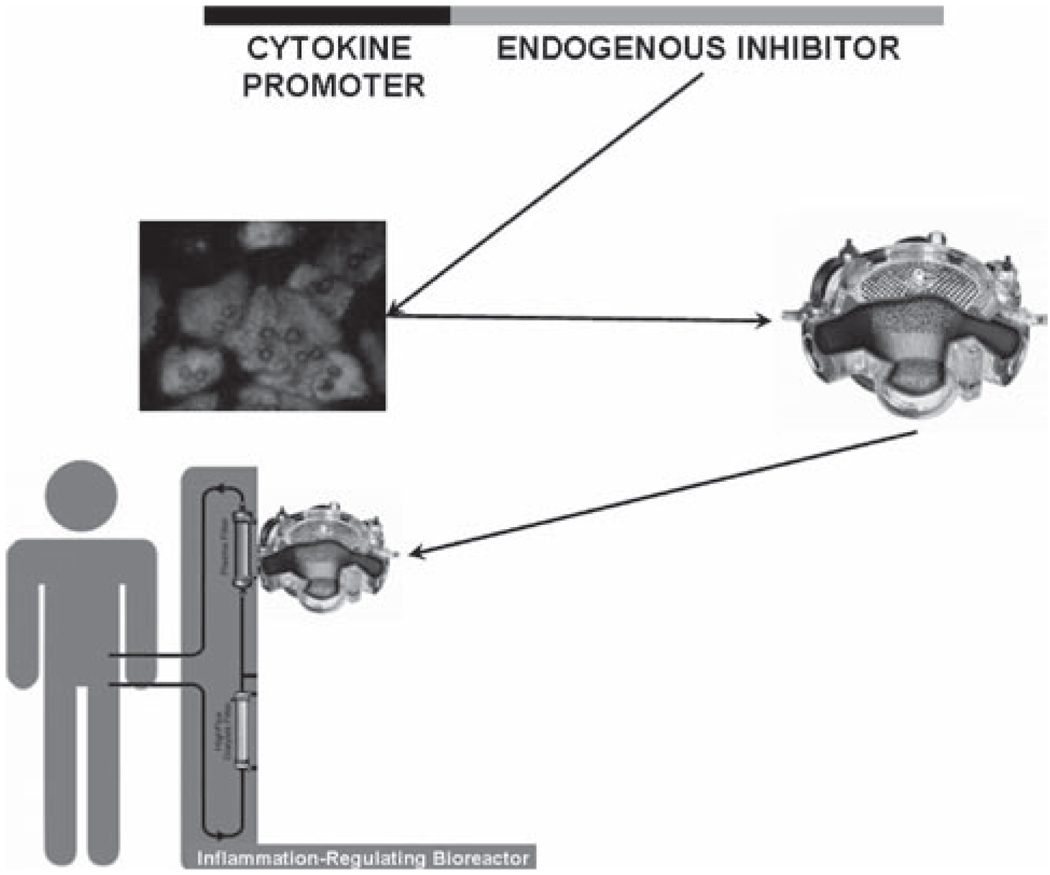
The central lesson from our Translational Systems Biology studies to date has been that the therapeutic goal for most, if not all, inflammatory diseases should not to be to abolish inflammation per se but rather to define its time course and reduce damage or dysfunction (i.e. promote healing) by modulating inflammation in a rational fashion. More specifically, our goal is to attenuate the vicious positive feedback cycle of inflammation→damage→inflammation [55], by allowing the body to re-equilibrate its inflammatory response through a repeated, incremental reduction of pro-inflammatory influences. To do so, we have conceived of and prototyped a self-regulating device for individualized control of inflammation (Figure 3). The basic concept of the proposed device is to create negative feedback proportional to the exact degree of inflammatory stimulus by invoking the production of these antagonists.
Figure 3.
Self-regulating, individualized inflammation-modulating bioreactor. Plasmids consisting of cytokine-sensitive promoters upstream of endogenous cytokine inhibitors have been constructed using standard molecular biology techniques. The plasmids have been transfected into hepatocyte cell lines. The cells are seeded into bioreactors. In the future, such bioreactors could be connected extracorporeally in order to modulate inflammation in a disease- and patient-specific manner.
Since inflammation is driven and regulated by cytokines [5] and regulated in part by the production of endogenous cytokine antagonists [155], we hypothesize that in response to a given inflammatory cytokine such rational therapy might stimulate the release of a defined amount of a given cytokine’s endogenous inhibitor or neutralizing protein. Examples include: TNF and its endogenous inhibitor, soluble TNF receptor (sTNFR), as well as IL-1β and IL-1ra [5]. Both sTNFR [156] and IL-1ra [157] are in development by the biotechnology industry as candidate therapeutics for various diseases.
The current paradigm for treatment of acute inflammation is to define a mediator and then antagonize it. In this paradigm, the antagonist is delivered in a randomized fashion in the setting of a clinical trial (or, in the unlikely event of a successful clinical trial, the antagonist is delivered to the patient whenever deemed clinically necessary, generally with incomplete diagnostic information).
Instead, what is needed is a personalized (yet standardized) inflammation-modulating therapy. We have proposed just such a device, based on short-circuiting the mediator-inhibitor feedback loop by genetically modifying cells so that they respond to a given cytokine by producing its natural antagonist. We have shown that such a feedback loop can indeed function in vitro and in a biohybrid device setting (Mikheev M, Vodovotz Y, unpublished observations).
The proposed device could be standardized, since it could consist of a multi-compartment, hollow fiber-based bioreactor with integral oxygenation, populated with a defined set of gene-modified cells derived from a well-characterized cell line, rather than using autologous cells. This feature should reduce regulatory hurdles. The device would be personalized, since a given patient’s individual production of cytokines would be counteracted in a precise fashion and only as required. The basic premise of this device has been demonstrated in vitro, and prototypes of the device based on an existing liver bioreactor design [158] have already been built (Mikheev, M, Vodovotz Y, unpublished observations). Importantly, we have built the computational infrastructure necessary to design such a device in a rational fashion, in order to tailor the specific characteristics of the device for both the disease and the individual in a practical manner.
Conclusions and Future Directions
The field of acute inflammation is inundated with literature that describes various aspects of the process but fails to link them in a holistic fashion that has clinical translation as its main goal. Translational Systems Biology aims to unify mechanisms described in the scientific literature using methods and tools developed by the computational and systems biology communities. By harnessing this approach, we hope to suggest novel insights into the pathobiology of inflammation and the intertwined damage/healing response, and add a mechanistic, rational basis to the design and implementation of therapies. The not-too-distant future includes rational, model-driven design and testing of novel therapies; clinical trials that are first run in silico; inpatient care in which diagnosis is aided by mathematical models [159]; outpatient care plans prepared using model-driven decisions along the fragmented continuum of care, and the analysis of the epidemiological impact of clinical interventions on host-pathogen interactions.
The ultimate therapeutic utility of these approaches is still in debate within the clinical community [160]. We in the Translational Systems Biology community hope that the exciting developments outlined herein, and the many more on the way, will build bridges to the larger computational and systems biology communities to aid us in these translational efforts.
Acknowledgements
The authors would like to acknowledge the contributions to this work of the following investigators, students, and postdoctoral fellows: Julia Arciero, Arie Baratt, Timothy R. Billiar, Frederick D. Busche, David Carney, Carson Chow, Gilles Clermont, Judy Day, Edwin Dietch, Russell Delude, Joyeeta Dutta-Moscato, James Faeder, Rena Feinman, Ali Ghuma, Mitchell P. Fink, David Hackam, Rukmini Kumar, Claudio Lagoa, Ryan M. Levy, Nicole Li, Maxim Mikheev, Rajaie Namas, Gary Nieman, Patricio Polanco, Ian Price, Jose M. Prince, Juan Carlos Puyana, Angela Reynolds, Beatrice Riviere, Matthew Rosengart, Alexey Solovyev, David L. Steed, Joshua Sullivan, David Swigon, Andres Torres, Jefrey Upperman, Katherine Verdolini, Ivan Yotov, Cordelia Ziraldo, and Sven Zenker. Additionally, several excellent technicians (Derek Barclay, David Gallo, and Binnie Betten) contributed to this work. We would also like to thank Alan Russell and Cliford Brubaker for their unwavering support.
This work was supported in part by the National Institutes of Health grants R01-GM-67240, P50-GM-53789, R33-HL-089082, R01-HL080926, R01-AI080799, and R01-HL-76157; National Institute on Disability and Rehabilitation Research grant H133E070024; as well as grants from the Commonwealth of Pennsylvania, the Pittsburgh Lifesciences Greenhouse, and the Pittsburgh Tissue Engineering Initiative. Te Pediatric Acute Liver Failure (PALF) Study Group is supported by the NIH-NIDDK UO1-DK072146-05. Dr. Vodovotz is a co-founder of and consultant to Immunetrics, Inc., which has licensed from the University of Pittsburgh the rights to commercialize aspects of the mathematical modeling of inflammation. Drs. An and Ermentrout are also consultants to Immunetrics, Inc.
Abbreviations
- ABM
agent-based model
- AsNOS
Anopheles stephensi nitric oxide synthase
- DAMP
damage-associated molecular pattern molecule
- DFU
diabetic foot ulcer
- GCS
Glasgow Coma Scale
- G-CSF
granulocyte colony stimulating factor
- GM-CSF
granulocyte-macrophage colony
- GOS
The Glasgow Outcome Score; stimulating factor
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- HMGB1
high molecular weight group box-1
- IL
interleukin
- IL-1ra
IL-1 receptor antagonist
- iNOS
inducible nitric oxide synthase
- IP-10
interferon-γ inducible protein of 10 kDa
- ISS
injury severity score
- KC
keratinocyte-derived chemokine
- LPS
gram-negative bacterial lipopolysaccharide
- MIG
monokine induced by interferon-γ
- MIP-1α
macrophage inflammatory protein-1α
- MMP
matrix metalloproteinase
- NEC
necrotizing enterocolitis
- NO
nitric oxidePALF, pediatric acute liver failure
- PCA
Principal Component Analysis
- RANTES
regulated on activation normal T cell expressed and secreted
- RSV
respiratory syncytial virus
- SPARK
Simple Platform for Agent-based Representation of Knowledge
- sTNFR
soluble tumor necrosis factor-α receptor
- TBI
traumatic brain injury
- TGF-β1
transforming growth factor-β1
- TIMP
tissue inhibitor of metalloprotease
- TLR
Toll-like receptor
- TNF
tumor necrosis factor-α
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.2007 < http://nihroadmasp.nih.gov/2008initiatives.asp>.
- 2.Brown KL, Cosseau C, Gardy JL, Hancock RE. Complexities of targeting innate immunity to treat infection. Trends Immunol. 2007;28:260–266. doi: 10.1016/j.it.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 4.Vodovotz Y, Constantine G, Rubin J, Csete M, Voit EO, An G. Mechanistic simulations of inflammation: Current state and future prospects. Math. Biosci. 2009;217:1–10. doi: 10.1016/j.mbs.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nathan C. Points of control in inflammation. Nature. 2002;420:846–852. doi: 10.1038/nature01320. [DOI] [PubMed] [Google Scholar]
- 6.Vodovotz Y, Csete M, Bartels J, Chang S, An G. Translational systems biology of inflammation. PLoS. Comput. Biol. 2008;4:1–6. doi: 10.1371/journal.pcbi.1000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Namas R, Ghuma A, Torres A, Polanco P, Gomez H, Barclay D, Gordon L, Zenker S, Kim HK, Hermus L, et al. An adequately robust early TNF-a response is a hallmark of survival following trauma/hemorrhage. PLoS ONE. 2009;4:e8406. doi: 10.1371/journal.pone.0008406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Furuta T, Kikuchi T, Iwakura Y, Watanabe N. Protective roles of mast cells and mast cell-derived TNF in murine malaria. J. Immunol. 2006;177:3294–3302. doi: 10.4049/jimmunol.177.5.3294. [DOI] [PubMed] [Google Scholar]
- 9.D’Ombrain MC, Robinson LJ, Stanisic DI, Taraika J, Bernard N, Michon P, Mueller I, Schofield L. Association of early interferon-gamma production with immunity to clinical malaria: a longitudinal study among Papua New Guinean children. Clin. Infect. Dis. 2008;47:1380–1387. doi: 10.1086/592971. [DOI] [PubMed] [Google Scholar]
- 10.Robinson LJ, D’Ombrain MC, Stanisic DI, Taraika J, Bernard N, Richards JS, Beeson JG, Tavul L, Michon P, Mueller I, et al. Cellular tumor necrosis factor, gamma interferon, and interleukin-6 responses as correlates of immunity and risk of clinical Plasmodium falciparum malaria in children from Papua New Guinea. Infect. Immun. 2009;77:3033–3043. doi: 10.1128/IAI.00211-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santos CC, Zhang H, Liu M, Slutsky AS. Bench-to-bedside review: Biotrauma and modulation of the innate immune response. Crit Care. 2005;9:280–286. doi: 10.1186/cc3022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alverdy J, Zaborina O, Wu L. The impact of stress and nutrition on bacterial-host interactions at the intestinal epithelial surface. Curr. Opin. Clin. Nutr. Metab Care. 2005;8:205–209. doi: 10.1097/00075197-200503000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Vincent JL, Ferreira F, Moreno R. Scoring systems for assessing organ dysfunction and survival. Crit Care Clin. 2000;16:353–366. doi: 10.1016/s0749-0704(05)70114-7. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg AL. Recent innovations in intensive care unit risk-prediction models. Curr. Opin. Crit Care. 2002;8:321–330. doi: 10.1097/00075198-200208000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Schlag G, Redl H. Mediators of injury and inflammation. World J Surg. 1996;20:406–410. doi: 10.1007/s002689900064. [DOI] [PubMed] [Google Scholar]
- 16.Stoiser B, Knapp S, Talhammer F, Locker GJ, Kofler J, Hollenstein U, Staudinger T, Wilfing A, Frass M, Burgmann H. Time course of immunological markers in patients with the systemic inflammatory response syndrome: evaluation of sCD14, sVCAM-1, sELAM-1, MIP-1 alpha and TGF-beta 2. Eur J Clin Invest. 1998;28:672–678. doi: 10.1046/j.1365-2362.1998.00326.x. [DOI] [PubMed] [Google Scholar]
- 17.Matzinger P. The danger model: a renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 18.Jarrar D, Chaudry IH, Wang P. Organ dysfunction following hemorrhage and sepsis: mechanisms and therapeutic approaches (Review) Int. J. Mol. Med. 1999;4:575–583. doi: 10.3892/ijmm.4.6.575. [DOI] [PubMed] [Google Scholar]
- 19.Kitano H. Systems biology: a brief overview. Science. 2002;295:1662–1664. doi: 10.1126/science.1069492. [DOI] [PubMed] [Google Scholar]
- 20.Csete ME, Doyle JC. Reverse engineering of biological complexity. Science. 2002;295:1664–1669. doi: 10.1126/science.1069981. [DOI] [PubMed] [Google Scholar]
- 21.Doyle J, Csete M. Rules of engagement. Nature. 2007;446:860. doi: 10.1038/446860a. [DOI] [PubMed] [Google Scholar]
- 22.Fussenegger M, Bailey JE, Varner J. A mathematical model of caspase function in apoptosis. Nat. Biotechnol. 2000;18:768–774. doi: 10.1038/77589. [DOI] [PubMed] [Google Scholar]
- 23.Cobb JP, Buchman TG, Karl IE, Hotchkiss RS. Molecular biology of multiple organ dysfunction syndrome: injury, adaptation, and apoptosis. Surg. Infect. (Larchmt.) 2000;1:207–215. doi: 10.1089/109629600750018132. [DOI] [PubMed] [Google Scholar]
- 24.Maier RV. Pathogenesis of multiple organ dysfunction syndrome - endotoxin, inflammatory cells, and their mediators: cytokines and reactive oxygen species. Surg. Infect. (Larchmt.) 2000;1:197–205. doi: 10.1089/109629600750018123. [DOI] [PubMed] [Google Scholar]
- 25.Goldstein B, Faeder JR, Hlavacek WS, Blinov ML, Redondo A, Wofsy C. Modeling the early signaling events mediated by FcepsilonRI. Mol. Immunol. 2002;38:1213–1219. doi: 10.1016/s0161-5890(02)00066-4. [DOI] [PubMed] [Google Scholar]
- 26.Hlavacek WS, Faeder JR, Blinov ML, Perelson AS, Goldstein B. The complexity of complexes in signal transduction. Biotechnol. Bioeng. 2003;84:783–794. doi: 10.1002/bit.10842. [DOI] [PubMed] [Google Scholar]
- 27.Faeder JR, Hlavacek WS, Reischl I, Blinov ML, Metzger H, Redondo A, Wofsy C, Goldstein B. Investigation of early events in Fc epsilon RI-mediated signaling using a detailed mathematical model. J. Immunol. 2003;170:3769–3781. doi: 10.4049/jimmunol.170.7.3769. [DOI] [PubMed] [Google Scholar]
- 28.Goldstein B, Faeder JR, Hlavacek WS. Mathematical and computational models of immune-receptor signalling. Nat. Rev. Immunol. 2004;4:445–456. doi: 10.1038/nri1374. [DOI] [PubMed] [Google Scholar]
- 29.Faeder JR, Blinov ML, Goldstein B, Hlavacek WS. Combinatorial complexity and dynamical restriction of network flows in signal transduction. Syst. Biol. (Stevenage.) 2005;2:5–15. doi: 10.1049/sb:20045031. [DOI] [PubMed] [Google Scholar]
- 30.Blinov ML, Yang J, Faeder JR, Hlavacek WS. Depicting signaling cascades. Nat. Biotechnol. 2006;24:137–138. doi: 10.1038/nbt0206-137. [DOI] [PubMed] [Google Scholar]
- 31.Bagci EZ, Vodovotz Y, Billiar TR, Ermentrout GB, Bahar I. Bistability in apoptosis: Roles of Bax, Bcl-2 and mitochondrial permeability transition pores. Biophys. J. 2006;90:1546–1559. doi: 10.1529/biophysj.105.068122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eissing T, Conzelmann H, Gilles ED, Allgower F, Bullinger E, Scheurich P. Bistability analyses of a caspase activation model for receptor-induced apoptosis. J Biol. Chem. 2004;279:36892–36897. doi: 10.1074/jbc.M404893200. [DOI] [PubMed] [Google Scholar]
- 33.Seely AJ, Christou NV. Multiple organ dysfunction syndrome: exploring the paradigm of complex nonlinear systems. Crit Care Med. 2000;28:2193–2200. doi: 10.1097/00003246-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Buchman TG, Cobb JP, Lapedes AS, Kepler TB. Complex systems analysis: a tool for shock research. Shock. 2001;16:248–251. doi: 10.1097/00024382-200116040-00002. [DOI] [PubMed] [Google Scholar]
- 35.Farmer JD, Kaufman SA, Packard NH, Perelson AS. Adaptive dynamic networks as models for the immune system and autocatalytic sets. Ann. N.Y. Acad. Sci. 1987;504:118–131. doi: 10.1111/j.1749-6632.1987.tb48728.x. [DOI] [PubMed] [Google Scholar]
- 36.Alt W, Lauffenburger DA. Transient behavior of a chemotaxis system modelling certain types of tissue inflammation. J. Math. Biol. 1987;24:691–722. doi: 10.1007/BF00275511. [DOI] [PubMed] [Google Scholar]
- 37.An G. Agent-based computer simulation and SIRS: building a bridge between basic science and clinical trials. Shock. 2001;16:266–273. doi: 10.1097/00024382-200116040-00006. [DOI] [PubMed] [Google Scholar]
- 38.Kumar R, Clermont G, Vodovotz Y, Chow CC. The dynamics of acute inflammation. J. Teoretical Biol. 2004;230:145–155. doi: 10.1016/j.jtbi.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 39.Reynolds A, Rubin J, Clermont G, Day J, Vodovotz Y, Ermentrout GB. A reduced mathematical model of the acute inflammatory response: I. Derivation of model and analysis of anti-inflammation. J. Teor. Biol. 2006;242:220–236. doi: 10.1016/j.jtbi.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 40.Day J, Rubin J, Vodovotz Y, Chow CC, Reynolds A, Clermont G. A reduced mathematical model of the acute inflammatory response: II. Capturing scenarios of repeated endotoxin administration. J. Theor. Biol. 2006;242:237–256. doi: 10.1016/j.jtbi.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 41.Chow CC, Clermont G, Kumar R, Lagoa C, Tawadrous Z, Gallo D, Betten B, Bartels J, Constantine G, Fink MP, et al. The acute inflammatory response in diverse shock states. Shock. 2005;24:74–84. doi: 10.1097/01.shk.0000168526.97716.f3. [DOI] [PubMed] [Google Scholar]
- 42.Prince JM, Levy RM, Bartels J, Baratt A, Kane JM, III, Lagoa C, Rubin J, Day J, Wei J, Fink MP, et al. In silico and in vivo approach to elucidate the inflammatory complexity of CD14-deficient mice. Mol. Med. 2006;12:88–96. doi: 10.2119/2006-00012.Prince. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lagoa CE, Bartels J, Baratt A, Tseng G, Clermont G, Fink MP, Billiar TR, Vodovotz Y. The role of initial trauma in the host’s response to injury and hemorrhage: Insights from a comparison of mathematical simulations and hepatic transcriptomic analysis. Shock. 2006;26:592–600. doi: 10.1097/01.shk.0000232272.03602.0a. [DOI] [PubMed] [Google Scholar]
- 44.Keramaris NC, Kanakaris NK, Tzioupis C, Kontakis G, Giannoudis PV. Translational research: from benchside to bedside. Injury. 2008;39:643–650. doi: 10.1016/j.injury.2008.01.051. [DOI] [PubMed] [Google Scholar]
- 45.Food,and Drug Administration. Innovation or Stagnation: Challenge and Opportunity on the Critical Path to New Medical Products. 2004. p. 1. [Google Scholar]
- 46.NIH Roadmap for Medical Research: Research Teams. 2006. [Google Scholar]
- 47.An G, Hunt CA, Clermont G, Neugebauer E, Vodovotz Y. Challenges and rewards on the road to translational systems biology in acute illness: Four case reports from interdisciplinary teams. J. Crit. Care. 2007;22:169–175. doi: 10.1016/j.jcrc.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.An G, Vodovotz Y. Translational systems biology: Introduction of an engineering approach to the pathophysiology of the burn patient. J. Burn Care Res. 2008;29:277–285. doi: 10.1097/BCR.0b013e31816677c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clermont G, Bartels J, Kumar R, Constantine G, Vodovotz Y, Chow C. In silico design of clinical trials: a method coming of age. Crit Care Med. 2004;32:2061–2070. doi: 10.1097/01.ccm.0000142394.28791.c3. [DOI] [PubMed] [Google Scholar]
- 50.Vodovotz Y, Clermont G, Chow C, An G. Mathematical models of the acute inflammatory response. Curr. Opin.Crit Care. 2004;10:383–390. doi: 10.1097/01.ccx.0000139360.30327.69. [DOI] [PubMed] [Google Scholar]
- 51.Kumar R, Chow CC, Bartels J, Clermont G, Vodovotz Y. A mathematical simulation of the inflammatory response to anthrax infection. Shock. 2008;29:104–111. doi: 10.1097/SHK.0b013e318067da56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.An G. In-silico experiments of existing and hypothetical cytokine-directed clinical trials using agent based modeling. Crit Care Med. 2004;32:2050–2060. doi: 10.1097/01.ccm.0000139707.13729.7d. [DOI] [PubMed] [Google Scholar]
- 53.Vodovotz Y, Chow CC, Bartels J, Lagoa C, Prince J, Levy R, Kumar R, Day J, Rubin J, Constantine G, et al. In silico models of acute inflammation in animals. Shock. 2006;26:235–244. doi: 10.1097/01.shk.0000225413.13866.fo. [DOI] [PubMed] [Google Scholar]
- 54.Vodovotz Y. Deciphering the complexity of acute inflammation using mathematical models. Immunologic Res. 2006;36:237–246. doi: 10.1385/IR:36:1:237. [DOI] [PubMed] [Google Scholar]
- 55.Vodovotz Y, An G. Systems Biology and Inflammation. In: Yan Q, editor. Systems Biology in Drug Discovery and Development: Methods and Protocols. Totowa, NJ: Springer Science & Business Media; 2009. In Press. [Google Scholar]
- 56.Akman-Anderson L, Vodovotz Y, Zamora R, Luckhart S. Bloodfeeding as an Interface of Mammalian and Arthropod Immunity. In: Beckage N, editor. Insect Immunology. San Diego, CA: Elsevier; 2007. pp. 149–177. [Google Scholar]
- 57.Drexler AL, Vodovotz Y, Luckhart S. Plasmodium development in the mosquito: biology bottlenecks and opportunities for mathematical modeling. Trends Parasitol. 2008;24:333–336. doi: 10.1016/j.pt.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.An G, Mi Q, Dutta-Moscato J, Solovyev A, Vodovotz Y. Agent-based models in translational systems biology. WIRES. 2009;1:159–171. doi: 10.1002/wsbm.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Janes KA, Yaffe MB. Data-driven modelling of signal-transduction networks. Nat. Rev. Mol. Cell Biol. 2006;7:820–828. doi: 10.1038/nrm2041. [DOI] [PubMed] [Google Scholar]
- 60.Mollen KP, Anand RJ, Tsung A, Prince JM, Levy RM, Billiar TR. Emerging paradigm: toll-like receptor 4-sentinel for the detection of tissue damage. Shock. 2006;26:430–437. doi: 10.1097/01.shk.0000228797.41044.08. [DOI] [PubMed] [Google Scholar]
- 61.Edelstein-Keshet L. Mathematical models in biology. New York: Random House; 1988. [Google Scholar]
- 62.Bailey JE. Mathematical modeling and analysis in biochemical engineering: past accomplishments and future opportunities. Biotechnol. Prog. 1998;14:8–20. doi: 10.1021/bp9701269. [DOI] [PubMed] [Google Scholar]
- 63.Neves SR, Iyengar R. Modeling of signaling networks. Bioessays. 2002;24:1110–1117. doi: 10.1002/bies.1154. [DOI] [PubMed] [Google Scholar]
- 64.Clermont G, Vodovotz Y, Rubin J. Equation-Based Models of Dynamic Biological Systems. In: Aird WC, editor. Endothelial Biomedicine. Cambridge, MA: Cambridge University Press; 2007. pp. 1780–1785. [Google Scholar]
- 65.Ermentrout GB, Edelstein-Keshet L. Cellular automata approaches to biological modeling. J. Theor. Biol. 1993;160:97–133. doi: 10.1006/jtbi.1993.1007. [DOI] [PubMed] [Google Scholar]
- 66.Grimm V, Revilla E, Berger U, Jeltsch F, Mooij WM, Railsback SF, Tulke HH, Weiner J, Wiegand T, DeAngelis DL. Pattern-oriented modeling of agent-based complex systems: lessons from ecology. Science. 2005;310:987–991. doi: 10.1126/science.1116681. [DOI] [PubMed] [Google Scholar]
- 67.Faeder JR, Blinov ML, Goldstein B, Hlavacek WS. Rule-based modeling of biochemical networks. Complexity. 2005;10:22–41. [Google Scholar]
- 68.Hlavacek WS, Faeder JR, Blinov ML, Posner RG, Hucka M, Fontana W. Rules for modeling signal-transduction systems. Sci STKE. 2006;2006:re6. doi: 10.1126/stke.3442006re6. [DOI] [PubMed] [Google Scholar]
- 69.Vodovotz Y, Clermont G, Hunt CA, Lefering R, Bartels J, Seydel R, Hotchkiss J, Ta’asan S, Neugebauer E, An G. Evidence-based modeling of critical illness: An initial consensus from the Society for Complexity in Acute Illness. J. Crit Care. 2007;22:77–84. doi: 10.1016/j.jcrc.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Clermont G, Chow CC, Constantine GM, Vodovotz Y, Bartels J. Mathematical and Statistical Modeling of Acute Inflammation; Classification, Clustering, and Data Mining Applications. Proceedings of the International Meeting of Classification Societies; New York: Springer Verlag; 2004. pp. 457–467. [Google Scholar]
- 71.Montague G, Morris J. Neural-network contributions in biotechnology. Trends Biotechnol. 1994;12:312–324. doi: 10.1016/0167-7799(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 72.Lengeler JW. Metabolic networks: a signal-oriented approach to cellular models. Biol. Chem. 2000;381:911–920. doi: 10.1515/BC.2000.112. [DOI] [PubMed] [Google Scholar]
- 73.Bornholdt S. Modeling genetic networks and their evolution: a complex dynamical systems perspective. Biol. Chem. 2001;382:1289–1299. doi: 10.1515/BC.2001.161. [DOI] [PubMed] [Google Scholar]
- 74.Chaplain M, Anderson A. Mathematical modelling of tumour-induced angiogenesis: network growth and structure. Cancer Treat. Res. 2004;117:51–75. doi: 10.1007/978-1-4419-8871-3_3. [DOI] [PubMed] [Google Scholar]
- 75.Vogels TP, Rajan K, Abbott LF. Neural network dynamics. Annu. Rev. Neurosci. 2005;28:357–376. doi: 10.1146/annurev.neuro.28.061604.135637. [DOI] [PubMed] [Google Scholar]
- 76.Tekirian TL, Thomas SN, Yang A. Advancing signaling networks through proteomics. Expert. Rev. Proteomics. 2007;4:573–583. doi: 10.1586/14789450.4.4.573. [DOI] [PubMed] [Google Scholar]
- 77.Stransky B, Barrera J, Ohno-Machado L, De Souza SJ. Modeling cancer: integration of “omics” information in dynamic systems. J Bioinform. Comput. Biol. 2007;5:977–986. doi: 10.1142/s0219720007002990. [DOI] [PubMed] [Google Scholar]
- 78.Chaouiya C. Petri net modelling of biological networks. Brief. Bioinform. 2007;8:210–219. doi: 10.1093/bib/bbm029. [DOI] [PubMed] [Google Scholar]
- 79.Nikiforova VJ, Willmitzer L. Network visualization and network analysis. EXS. 2007;97:245–275. doi: 10.1007/978-3-7643-7439-6_11. [DOI] [PubMed] [Google Scholar]
- 80.Wang E, Lenferink A, O’Connor-McCourt M. Cancer systems biology: exploring cancer-associated genes on cellular networks. Cell Mol. Life Sci. 2007;64:1752–1762. doi: 10.1007/s00018-007-7054-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Goncharova LB, Tarakanov AO. Molecular networks of brain and immunity. Brain Res. Rev. 2007;55:155–166. doi: 10.1016/j.brainresrev.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 82.Christensen C, Takar J, Albert R. Systems-level insights into cellular regulation: inferring, analysing, and modelling intracellular networks. IET. Syst. Biol. 2007;1:61–77. doi: 10.1049/iet-syb:20060071. [DOI] [PubMed] [Google Scholar]
- 83.Rho S, You S, Kim Y, Hwang D. From proteomics toward systems biology: integration of different types of proteomics data into network models. BMB. Rep. 2008;41:184–193. doi: 10.5483/bmbrep.2008.41.3.184. [DOI] [PubMed] [Google Scholar]
- 84.Han JD. Understanding biological functions through molecular networks. Cell Res. 2008;18:224–237. doi: 10.1038/cr.2008.16. [DOI] [PubMed] [Google Scholar]
- 85.Li H, Xuan J, Wang Y, Zhan M. Inferring regulatory networks. Front Biosci. 2008;13:263–275. doi: 10.2741/2677. [DOI] [PubMed] [Google Scholar]
- 86.Janes KA, Albeck JG, Gaudet S, Sorger PK, Lauffenburger DA, Yaffe MB. A systems model of signaling identifies a molecular basis set for cytokine-induced apoptosis. Science. 2005;310:1646–1653. doi: 10.1126/science.1116598. [DOI] [PubMed] [Google Scholar]
- 87.Frink M, Hsieh YC, Hsieh CH, Pape HC, Choudhry MA, Schwacha MG, Chaudry IH. Keratinocyte-derived chemokine plays a critical role in the induction of systemic inflammation and tissue damage after trauma-hemorrhage. Shock. 2007;28:576–581. doi: 10.1097/shk.0b013e31814b8e0d. [DOI] [PubMed] [Google Scholar]
- 88.Tsung A, Sahai R, Tanaka H, Nakao A, Fink MP, Lotze MT, Yang H, Li J, Tracey KJ, Geller DA, et al. The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J. Exp. Med. 2005;201:1135–1143. doi: 10.1084/jem.20042614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Izuishi K, Tsung A, Jeyabalan G, Critchlow ND, Li J, Tracey KJ, DeMarco RA, Lotze MT, Fink MP, Geller DA, et al. Cutting edge: high-mobility group box 1 preconditioning protects against liver ischemia-reperfusion injury. J. Immunol. 2006;176:7154–7158. doi: 10.4049/jimmunol.176.12.7154. [DOI] [PubMed] [Google Scholar]
- 90.Yang R, Harada T, Mollen KP, Prince JM, Levy RM, Englert JA, Gallowitsch-Puerta M, Yang L, Yang H, Tracey KJ, et al. Anti-HMGB1 Neutralizing Antibody Ameliorates Gut Barrier Dysfunction and Improves Survival after Hemorrhagic Shock. Mol. Med. 2006 doi: 10.2119/2006-00010.Yang. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tsung A, Zheng N, Jeyabalan G, Izuishi K, Klune JR, Geller DA, Lotze MT, Lu L, Billiar TR. Increasing numbers of hepatic dendritic cells promote HMGB1-mediated ischemia-reperfusion injury. J Leukoc. Biol. 2007;81:119–128. doi: 10.1189/jlb.0706468. [DOI] [PubMed] [Google Scholar]
- 92.Fan J, Li Y, Levy R, Fan JJ, Hackam DJ, Vodovotz Y, Billiar TR, Wilson MA. Hemorrhagic shock induces NAD(P)H oxidase activation in neutrophils: Role of HMGB1-TLR4 signaling. J. Immunol. 2007;178:6573–6580. doi: 10.4049/jimmunol.178.10.6573. [DOI] [PubMed] [Google Scholar]
- 93.Tsung A, Klune JR, Zhang X, Jeyabalan G, Cao Z, Peng X, Stolz DB, Geller DA, Rosengart MR, Billiar TR. HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J Exp. Med. 2007;204:2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A. HMGB1: endogenous danger signaling. Mol. Med. 2008;14:476–484. doi: 10.2119/2008-00034.Klune. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Muzio M, Polentarutti N, Bosisio D, Manoj Kumar PP, Mantovani A. Toll-like receptor family and signalling pathway. Biochem. Soc. Trans. 2000;28:563–566. doi: 10.1042/bst0280563. [DOI] [PubMed] [Google Scholar]
- 96.O’Neill L. The Toll/interleukin-1 receptor domain: a molecular switch for inflammation and host defence. Biochem. Soc. Trans. 2000;28:557–563. doi: 10.1042/bst0280557. [DOI] [PubMed] [Google Scholar]
- 97.Muzio M, Polentarutti N, Bosisio D, Manoj Kumar PP, Mantovani A. Toll-like receptor family and signalling pathway. Biochem. Soc. Trans. 2000;28:563–566. doi: 10.1042/bst0280563. [DOI] [PubMed] [Google Scholar]
- 98.Beutler B, Poltorak A. Sepsis and evolution of the innate immune response. Crit Care Med. 2001;29:S2–S6. doi: 10.1097/00003246-200107001-00002. [DOI] [PubMed] [Google Scholar]
- 99.Beutler B. TLR4 as the mammalian endotoxin sensor. Curr. Top. Microbiol. Immunol. 2002;270:109–120. doi: 10.1007/978-3-642-59430-4_7. [DOI] [PubMed] [Google Scholar]
- 100.Beutler B, Hoebe K, Du X, Ulevitch RJ. How we detect microbes and respond to them: the Toll-like receptors and their transducers. J. Leukoc. Biol. 2003;74:479–485. doi: 10.1189/jlb.0203082. [DOI] [PubMed] [Google Scholar]
- 101.Janssens S, Beyaert R. Role of Toll-like receptors in pathogen recognition. Clin. Microbiol. Rev. 2003;16:637–646. doi: 10.1128/CMR.16.4.637-646.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Arroyo-Espliguero R, Avanzas P, Jeffery S, Kaski JC. CD14 and toll-like receptor 4: a link between infection and acute coronary events? Heart. 2004;90:983–988. doi: 10.1136/hrt.2002.001297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rivière B, Epshteyn Y, Swigon D, Vodovotz Y. A simple mathematical model of signaling resulting from the binding of lipopolysaccharide with Toll-like receptor 4 demonstrates inherent preconditioning behavior. Math. Biosci. 2009;217:19–26. doi: 10.1016/j.mbs.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Foteinou PT, Calvano SE, Lowry SF, Androulakis IP. Modeling endotoxin-induced systemic inflammation using an indirect response approach. Math. Biosci. 2009;217:27–42. doi: 10.1016/j.mbs.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.An G. A model of TLR4 signaling and tolerance using a qualitative, particle event-based method: Introduction of Spatially Configured Stochastic Reaction Chambers (SCSRC) Math. Biosci. 2009;217:43–52. doi: 10.1016/j.mbs.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 106.Faeder JR, Blinov ML, Hlavacek WS. Rule-based modeling of biochemical systems with BioNetGen. In: Maly IV, editor. Methods in Molecular Biology: Systems Biology. Totowa, NJ: Humana Press; 2008. pp. 113–168. [DOI] [PubMed] [Google Scholar]
- 107.An G, Faeder JR. Detailed qualitative dynamic knowledge representation using a BioNetGen model of TLR-4 signaling and preconditioning. Math. Biosci. 2009;217:53–63. doi: 10.1016/j.mbs.2008.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gallucci S, Matzinger P. Danger signals: SOS to the immune system. Curr. Opin. Immunol. 2001;13:114–119. doi: 10.1016/s0952-7915(00)00191-6. [DOI] [PubMed] [Google Scholar]
- 109.Clark IA, Budd AC, Alleva LM. Sickness behaviour pushed too far–the basis of the syndrome seen in severe protozoal, bacterial and viral diseases and post-trauma. Malar. J. 2008;7:208. doi: 10.1186/1475-2875-7-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mi Q, Rivière B, Clermont G, Steed DL, Vodovotz Y. Agent-based model of inflammation and wound healing: insights into diabetic foot ulcer pathology and the role of transforming growth factor-b1. Wound Rep. Reg. 2007;15:617–682. doi: 10.1111/j.1524-475X.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 111.Li NYK, Verdolini K, Clermont G, Mi Q, Hebda PA, Vodovotz Y. A patient-specific in silico model of inflammation and healing tested in acute vocal fold injury. PLoS ONE. 2008;3:e2789. doi: 10.1371/journal.pone.0002789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Solovyev A, Mikheev M, Zhou L, Dutta-Moscato J, Ziraldo C, An G, Vodovotz Y, Mi Q. SPARK: A framework for multi-scale agent-based biomedical modeling. SCS Press. Proceedings of the 2010 Agent-Directed Simulation Symposium; 2010 Apr 12; Orlando, FL. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hancioglu B, Swigon D, Clermont G. A dynamical model of human immune response to influenza A virus infection. J. Theor. Biol. 2007;246:70–86. doi: 10.1016/j.jtbi.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 114.An G. Introduction of a agent based multi-scale modular architecture for dynamic knowledge representation of acute inflammation. Theor. Biol. Med. Model. 2008;5 doi: 10.1186/1742-4682-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.An G. Dynamic Knowledge Representation using Agent Based Modeling: Ontology Instantiation and Verification of Conceptual Models. In: Maly I, editor. Systems Biology: Methods in Molecular Biology Series. Totowa, NJ: Humana Press; 2009. pp. 445–468. [DOI] [PubMed] [Google Scholar]
- 116.Fink MP, Delude RL. Epithelial barrier dysfunction: a unifying theme to explain the pathogenesis of multiple organ dysfunction at the cellular level. Crit Care Clin. 2005;21:177–196. doi: 10.1016/j.ccc.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 117.Aird WC. Vascular bed-specific hemostasis: Role of endothelium in sepsis pathogenesis. Crit. Care Med. 2001;29 Suppl:S28–S35. doi: 10.1097/00003246-200107001-00013. [DOI] [PubMed] [Google Scholar]
- 118.Aird WC. Endothelium as a therapeutic target in sepsis. Curr. Drug Targets. 2007;8:501–507. doi: 10.2174/138945007780362782. [DOI] [PubMed] [Google Scholar]
- 119.Daun S, Rubin J, Vodovotz Y, Roy A, Parker R, Clermont G. An ensemble of models of the acute inflammatory response to bacterial lipopolysaccharide in rats: Results from parameter space reduction. J. Theor. Biol. 2008;253:843–853. doi: 10.1016/j.jtbi.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 120.Torres A, Bentley T, Bartels J, Sarkar J, Barclay D, Namas R, Constantine G, Zamora R, Puyana JC, Vodovotz Y. Mathematical modeling of post-hemorrhage inflammation in mice: Studies using a novel, computer-controlled, closed-loop hemorrhage apparatus. Shock. 2009;32:172–178. doi: 10.1097/SHK.0b013e318193cc2b. [DOI] [PubMed] [Google Scholar]
- 121.McCloskey CA, Kameneva MV, Uryash A, Gallo DJ, Billiar TR. Tissue hypoxia activates JNK in the liver during hemorrhagic shock. Shock. 2004;22:380–386. doi: 10.1097/01.shk.0000140660.78744.bf. [DOI] [PubMed] [Google Scholar]
- 122.Parker SJ, Watkins PE. Experimental models of gram-negative sepsis. J. Surg. 2001;88:22–30. doi: 10.1046/j.1365-2168.2001.01632.x. [DOI] [PubMed] [Google Scholar]
- 123.Marshall JC, Deitch E, Moldawer LL, Opal S, Redl H, Poll TV. Preclinical models of shock and sepsis: what can they tell us? Shock. 2005;24 Suppl 1:1–6. doi: 10.1097/01.shk.0000191383.34066.4b. [DOI] [PubMed] [Google Scholar]
- 124.Doherty DG, O’Farrelly C. Innate and adaptive lymphoid cells in the human liver. Immunol. Rev. 2000;174:5–20. doi: 10.1034/j.1600-0528.2002.017416.x. [DOI] [PubMed] [Google Scholar]
- 125.Gao B, Jeong WI, Tian Z. Liver: An organ with predominant innate immunity. Hepatology. 2008;47:729–736. doi: 10.1002/hep.22034. [DOI] [PubMed] [Google Scholar]
- 126.Antoniades CG, Berry PA, Wendon JA, Vergani D. The importance of immune dysfunction in determining outcome in acute liver failure. J. Hepatol. 2008;49:845–861. doi: 10.1016/j.jhep.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 127.Lee WM. Acute liver failure. N. Engl. J. Med. 1993;329:1862–1872. doi: 10.1056/NEJM199312163292508. [DOI] [PubMed] [Google Scholar]
- 128.Brown KE, Tisdale J, Barrett AJ, Dunbar CE, Young NS. Hepatitis-associated aplastic anemia. N. Engl. J. Med. 1997;336:1059–1064. doi: 10.1056/NEJM199704103361504. [DOI] [PubMed] [Google Scholar]
- 129.Rolando N, Harvey F, Brahm J, Philpott-Howard J, Alexander G, Gimson A, Casewell M, Fagan E, Williams R. Prospective study of bacterial infection in acute liver failure: an analysis of fifty patients. Hepatology. 1990;11:49–53. doi: 10.1002/hep.1840110110. [DOI] [PubMed] [Google Scholar]
- 130.Branski RC, Verdolini K, Sandulache V, Rosen CA, Hebda PA. Vocal fold wound healing: a review for clinicians. J. Voice. 2006;20:432–442. doi: 10.1016/j.jvoice.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 131.Reinhart K, Menges T, Gardlund B, Harm ZJ, Smithes M, Vincent JL, Tellado JM, Salgado-Remigio A, Zimlichman R, Withington S, et al. Randomized, placebo-controlled trial of the anti-tumor necrosis factor antibody fragment afelimomab in hyperinflammatory response during severe sepsis: The RAMSES Study. Crit Care Med. 2001;29:765–769. doi: 10.1097/00003246-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 132.Fisher CJ, Jr, Opal SM, Dhainaut JF, Stephens S, Zimmerman JL, Nightingale P, Harris SJ, Schein RM, Panacek EA, Vincent JL, et al. Influence of an anti-tumor necrosis factor monoclonal antibody on cytokine levels in patients with sepsis. The CB0006 Sepsis Syndrome Study Group. Crit Care Med. 1993;21:318–327. doi: 10.1097/00003246-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 133.Remick DG, Bolgos GR, Siddiqui J, Shin J, Nemzek JA. Six at six: interleukin-6 measured 6 h after the initiation of sepsis predicts mortality over 3 days. Shock. 2002;17:463–467. doi: 10.1097/00024382-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 134.Zenati MS, Billiar TR, Townsend RN, Peitzman AB, Harbrecht BG. A brief episode of hypotension increases mortality in critically ill trauma patients. J Trauma. 2002;53:232–236. doi: 10.1097/00005373-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 135.Chau TA, McCully ML, Brintnell W, An G, Kasper KJ, Vines ED, Kubes P, Haeryfar SM, McCormick JK, Cairns E, et al. Toll-like receptor 2 ligands on the staphylococcal cell wall downregulate superantigen-induced T cell activation and prevent toxic shock syndrome. Nat. Med. 2009;15:641–648. doi: 10.1038/nm.1965. [DOI] [PubMed] [Google Scholar]
- 136.Chang S, Baratt A, Clermont G, Planquois J-M, Yan SB, Williams M, Macias W. Mathematical model predicting outcomes of sepsis patients treated with Xigris(R): ENHANCE trial. Shock. 2006;25:70–71. [Abstract] [Google Scholar]
- 137.Vodovotz Y, Zamora R, Lieber MJ, Luckhart S. Cross-talk between nitric oxide and transforming growth factor-b1 in malaria. Curr. Mol. Med. 2004;4:787–797. doi: 10.2174/1566524043359999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Luckhart S, Lieber MJ, Singh N, Zamora R, Vodovotz Y. Low levels of mammalian TGF-b1 are protective against malaria parasite infection, a paradox clarified in the mosquito host. Exp. Parasitol. 2008;118:290–296. doi: 10.1016/j.exppara.2007.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Upperman JS, Lugo B, Camerini V, Yotov I, Rubin J, Clermont G, Zamora R, Ermentrout GB, Ford HR, Vodovotz Y. Mathematical modeling in NEC - A new look at an ongoing problem. J. Pediatr. Surg. 2007;42:445–453. doi: 10.1016/j.jpedsurg.2006.10.053. [DOI] [PubMed] [Google Scholar]
- 140.Alverdy JC, Laughlin RS, Wu L. Influence of the critically ill state on host-pathogen interactions within the intestine: gut-derived sepsis redefined. Crit Care Med. 2003;31:598–607. doi: 10.1097/01.CCM.0000045576.55937.67. [DOI] [PubMed] [Google Scholar]
- 141.Alverdy JC, Chang EB. The re-emerging role of the intestinal microflora in critical illness and inflammation: why the gut hypothesis of sepsis syndrome will not go away. J. Leukoc. Biol. 2008;83:461–466. doi: 10.1189/jlb.0607372. [DOI] [PubMed] [Google Scholar]
- 142.An G. Modeling sepsis as ecological collapse and social disorder: Bacterial game theory, scarcity and insurrection. Shock. 2008;29:100–101. [Abstract] [Google Scholar]
- 143.Axelrod R, Hamilton WD. The evolution of cooperation. Science. 1981;211:1390–1396. doi: 10.1126/science.7466396. [DOI] [PubMed] [Google Scholar]
- 144.Evans RS, Burke JP, Pestotnik SL, Classen DC, Menlove RL, Gardner RM. Prediction of hospital infections and selection of antibiotics using an automated hospital database. 1990 [Unpublished] [Google Scholar]
- 145.Hotchkiss JR, Strike DG, Crooke PS. Pathogen transmission and clinic scheduling. Emerg. Infect. Dis. 2006;12:159–162. doi: 10.3201/eid1201.050349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Najera JA. A critical review of the field application of a mathematical model of malaria eradication. Bull. World Health Organ. 1974;50:449–457. [PMC free article] [PubMed] [Google Scholar]
- 147.Flahault A, Deguen S, Valleron AJ. A mathematical model for the European spread of influenza. Eur. J. Epidemiol. 1994;10:471–474. doi: 10.1007/BF01719679. [DOI] [PubMed] [Google Scholar]
- 148.Levin BR. Models for the spread of resistant pathogens. Neth. J Med. 2002;60:58–64. [PubMed] [Google Scholar]
- 149.Ferguson NM, Mallett S, Jackson H, Roberts N, Ward P. A population-dynamic model for evaluating the potential spread of drug-resistant influenza virus infections during community-based use of antivirals. J. Antimicrob. Chemother. 2003;51:977–990. doi: 10.1093/jac/dkg136. [DOI] [PubMed] [Google Scholar]
- 150.Teboh-Ewungkem MI, Podder CN, Gumel AB. Mathematical Study of the Role of Gametocytes and an Imperfect Vaccine on Malaria Transmission Dynamics. Bull. Math. Biol. 2009 doi: 10.1007/s11538-009-9437-3. [DOI] [PubMed] [Google Scholar]
- 151.Tasman H, Soewono E, Sidarto KA, Syafruddin D, Rogers WO. A model for transmission of partial resistance to anti-malarial drugs. Math. Biosci. Eng. 2009;6:649–661. doi: 10.3934/mbe.2009.6.649. [DOI] [PubMed] [Google Scholar]
- 152.Rafikov M, Bevilacqua L, Wyse AP. Optimal control strategy of malaria vector using genetically modified mosquitoes. J. Theor. Biol. 2009;258:418–425. doi: 10.1016/j.jtbi.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 153.Li J. A malaria model with partial immunity in humans. Math. Biosci. Eng. 2008;5:789–801. doi: 10.3934/mbe.2008.5.789. [DOI] [PubMed] [Google Scholar]
- 154.Chitnis N, Hyman JM, Cushing JM. Determining important parameters in the spread of malaria through the sensitivity analysis of a mathematical model. Bull. Math. Biol. 2008;70:1272–1296. doi: 10.1007/s11538-008-9299-0. [DOI] [PubMed] [Google Scholar]
- 155.Larrick JW, Wright SC. Native cytokine antagonists. Baillieres Clin. Haematol. 1992;5:681–702. doi: 10.1016/s0950-3536(11)80012-0. [DOI] [PubMed] [Google Scholar]
- 156.Fernandez-Botran R, Crespo FA, Sun X. Soluble cytokine receptors in biological therapy. Expert.Opin.Biol.Ter. 2002;2:585–605. doi: 10.1517/14712598.2.6.585. [DOI] [PubMed] [Google Scholar]
- 157.Dinarello CA. Blocking IL-1 in systemic inflammation. J.Exp. Med. 2005;201:1355–1359. doi: 10.1084/jem.20050640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gerlach JC. Bioreactors for extracorporeal liver support. Cell Transplant. 2006;15 Suppl 1:S91–S103. doi: 10.3727/000000006783982296. [DOI] [PubMed] [Google Scholar]
- 159.Zenker S, Rubin J, Clermont G. From inverse problems in mathematical physiology to quantitative differential diagnoses. PLoS. Comput. Biol. 2007;3:e204. doi: 10.1371/journal.pcbi.0030204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Marshall JC. Through a glass darkly: the brave new world of in silico modeling. Crit Care Med. 2004;32:2157–2159. doi: 10.1097/01.ccm.0000142935.34916.b5. [DOI] [PubMed] [Google Scholar]