Abstract
This paper describes the protocols used at Childrens Hospital Los Angeles (CHLA) to protract the maxilla during early adolescence. It is a modification of techniques introduced by Eric Liou with his Alternate Rapid Maxillary Expansion and Constriction (ALT-RAMEC) technique. The main differences between the CHLA protocol and previous maxillary protraction protocols are the age the protraction is attempted, the sutural loosening by alternating weekly expansion with constriction and the use of Class III elastics to support and redirect the protraction by nightly facemask wear. The CHLA protocol entirely depends on patient compliance and must be carefully taught and monitored. In a cooperative patient, the technique can correct a Class III malocclusion that previously would have been treated with LeFort 1 maxillary advancement surgery. Thus, it is not appropriate for patients requiring 2 jaw surgeries to correct mandibular prognathism, occlusal cants or facial asymmetry. The maxillary protraction appears to work by a combination of skeletal advancement, dental compensation and rotation of the occlusal planes. Microscrew/microimplant/temporary anchorage devices have been used with these maxillary protraction protocols to assist in expanding the maxilla, increasing skeletal anchorage during protraction, limiting dental compensations and reducing skeletal relapse.
INTRODUCTION
Clefts of the lip and/or palate are among the most common birth anomalies. On average, cleft lip and palate occurs one in every 700 live births in the USA.1 In cleft lip and palate patients, the mandible is usually unaffected by the cleft and grows normally; however, the maxilla often does not grow as far forward and downward as the non-cleft child2, resulting in a short maxilla and a Class III malocclusion. The scar contracture that occurs from the hard palate repair is thought to distort the growth of the maxilla resulting in maxillary hypoplasia.3–8 Fibrosis results from the stripped periosteum and affects the vertical, transverse and anteroposterior growth of the maxilla. In addition, the fibrosis that results from the cleft lip repair is also thought to play a role in the maxillary deficiency.9 Approximately 22–26% of cleft lip and palate patients will need orthognathic surgery at the end of adolescent growth to correct the maxillary deficiency.10
For maxillary hypoplasia resulting in a difference between upper and lower jaw lengths, the standard of care is to surgically advance the maxillary bone and dentition in cleft patients with a LeFort I osteotomy after adolescent growth has completed. The advantages to surgical advancement of the upper jaw is that surgery targets bony correction, corrects the bite and can effect a significant facial change in patients with cleft lip and palate. However, orthognathic surgery requires a six to eight week recovery period, is expensive and can be associated with patient discomfort, liquid diet, facial swelling, and transient paresthesia and in some occasions, permanent loss of neurosensation. This surgery is more difficult to perform for cleft patients with Class III malocclusions than in non-cleft patients with Class III malocclusions, because of the scarring from previous surgeries, which restricts the forward movement of the maxilla. Furthermore, the scarring may also increase the relapse rate associated with maxillary surgical advancement in cleft patients. Rates of relapse in these patients have been reported to occur 5–80% of the time.11 Therefore, the patient with cleft lip and palate may go through the morbidity associated with orthognathic surgery and still relapse back to the prior Class III malocclusion.
Orthodontic treatment consists of extraction of teeth, proclination of the maxillary incisors and retraction of the mandibular incisors12 in patients with a mild underbite. However, orthodontic treatment only camouflages the malocclusion and can result in a deficient amount of supporting bone for the dentition.12 Another option is to treat the patient by orthopedic correction during the early mixed dentition at ages 7–9. This treatment can only correct Class III malocclusions with a negative overjet of 4–5 mm13 and advances the maxilla an average distance of 2.1 mm. The major drawback to early correction during growth is the recurrence of the underbite with mandibular growth; thereby, allowing the occlusion to revert back to a Class III malocclusion during adolescence.
For orthopedic correction of a short maxilla in the cleft lip and palate patient, facemask forces range from 300 to 700 grams of force and the time period of treatment can be as early as 6 years of age and as late as 12 years. Initial success at correcting dental crossbites at age 6–714 is tempered with limited success at protracting the maxilla at age 8–10.15 In 1996, So16 reported only an average of 1.3 mm of maxillary protraction in Class III patients with unilateral cleft lip and palate. There appears to be less movement of the maxillary skeleton as the patient ages15 and correction of the crossbite is the result of rotation of the occlusal plane.17 Long-term results of early protraction appear to be only a temporary correction which needs to be re-addressed during late adolescence with re-treatment14 Historically, orthopedic protraction was not successful in older patients to advance the maxilla in cleft lip and palate patients aged 9–12 years. A protocol of maxillary protraction developed by Liou and Tsai in 200518 includes three components: a 2-hinged rapid maxillary expander, repetitive weekly protocol of Alternate Rapid Maxillary Expansion and Constriction (Alt-RAMEC), and intraoral maxillary protraction springs. The innovative part of this technique is the sutural loosening accomplished by alternating expansion with constriction for eight weeks. This back and forth motion can mobilize the maxilla and protract the maxilla for longer distances.18–19 In the Alt-RAMEC protocol the maxilla is expanded for 7 consecutive days and constricted for 7 consecutive days for a total of 9 weeks. Following the Alt-RAMEC technique the maxilla is protracted with protraction springs for 3 months. This technique has been shown to advance the maxilla (defined as A point on a cephalometric tracing) an average of 5.8 mm.18,20
In this paper, we describe a variation of the Liou technique used at Childrens Hospital Los Angeles. The Liou prescription for success depends on several custom fabricated devices such as a 2-hinged rapid maxillary expander and a tooth-borne, intraoral maxillary protraction spring. During our early attempts, we found that these appliances could break and require frequent replacement at every appointment. Moreover, the springs could produce anterior open bites during protraction. At Childrens Hospital Los Angeles (CHLA), the technique has been modified to use a standard Hyrax rapid maxillary expansion appliance (RME, Orthodontic Store, Gaithersburg, MD) and fixed orthodontic appliances in the lower arch, Class III elastics and reverse-pull headgear or facemask. The use of standard techniques makes the Alt-RAMEC technique accessible to most orthodontists and eliminates the open bite side effect by utilizing a downward direction of pull. In fact, the modified technique can be used to close anterior open bites in patients. This technique, however, is completely dependent on patient cooperation as opposed to the original spring that was designed for a non-compliant patient.
The CHLA maxillary protraction protocol
The patients who received maxillary protraction were given a choice between maxillary protraction and surgery to correct their malocclusion and improve their facial esthetics. In our craniofacial team, the patients in the protraction group were considered surgical candidates for a LeFort I surgery to improve their occlusion and facial appearance. A typical profile of a patient with cleft lip and palate tended to show overclosure of the mandible, negligible maxillary incisor display, nasal deformity, a thin upper lip, a full lower lip and upright maxillary incisors due to lip tension from prior lip surgeries. The maxillary incisors could benefit from some form of maxillary incisor proclination in contrast to the patient without a facial cleft.
In our protocol, maxillary expansion and protraction was carried out before dental alignment with an archwire because additional space was created with arch expansion. If maxillary dental crowding were present, extractions were deferred until after expansion and protraction. The exceptions to this rule were the patients who had molars and premolars tilting in opposite directions which would prevent parallel draw of bands. These patients received limited orthodontics with sectional wires to improve the insertion and draw of a rapid palatal expander (RPE). The orthodontic setups for protraction and orthognathic surgery were similar as both treatments decompensated the anterior teeth in order to maximize skeletal correction during treatment. Table 1 summarizes the clinical protocol for maxillary protraction in an adolescent patient with cleft lip and palate.
Table 1.
The clinical protocol for maxillary protraction in a typical adolescent patient with Cleft lip and palate (CLP).
|
The management of the protraction technique was based on our experience and research with maxillary distraction osteogenesis21 Maxillary protraction is similar to distraction osteogenesis because the correction is attained gradually over a period of time, is limited to bony deficiencies and is not a suitable replacement for treatment plans involving two jaw or segmental surgeries. In both cases, overcorrection of the deformity was needed to plan for relapse when the expanders were removed. Unlike orthognathic surgery, the protraction process is dynamic and can change direction during the treatment; there can be many adjustments of the maxilla possible as it is pulled forward. For example, doubling the elastic pull on one side could provide asymmetric correction if one side lagged behind and rotated the maxilla to one side. Similarly, intra-arch elastics can help correct asymmetric expansions of the maxilla. During the first nine weeks, continuous alternation between expansion and constriction was used to loosen and maintain the sutures in a flexible state for maxillary protraction. During protraction, the patients were instructed to wear the facemask to “pull” the maxilla forward at night and to wear Cassl III elastics during daytime to “hold” the results obtained by the facemask treatment at night. In terms of cooperation, the patient was told that maxillary protraction required full cooperation from the patient or treatment will fail. Intermittent usage was not effective because any interruption in placing tension on the sutures could cause early bone consolidation in a growing patient. In animal distraction studies, a thin cortical layer rapidly formed to span the distraction site-21 and stopped the distraction process. Presumably, whenever the protraction process stopped, a similar process could inhibit maxillary protraction. Clinically, patients need to be informed that failure to cooperate during the treatment process would result in the need to restart the treatment process from the beginning. Another problem is if the patient fails to cooperate in the middle of expansion and constriction, the screws in a half-expanded position could still turn without exerting an outward pressure by spinning in the turnbuckle housing. In these cases, RPE appliances were remade to accommodate the slightly expanded position, and the eight week expansion and constriction period was recalculated according to the restart date. At the end of orthodontic leveling, a .019x.022” stainless steel archwire was placed that extended to the second molar. Clamp on hooks with titanium inserts from TP Orthodontics (LaPorte,IN) were placed mesial to the mandibular canines to support Class III elastics. Heavy force elastics were used to protract the maxilla with the facemask and to maintain the correction with Class III elastics. Heavy force implies that the elastics were stretched to a point just before breaking. Patients typically progressed from 3/16” medium to 1/8” medium to 1/8” heavy elastics as the maxilla advanced in order to maintain heavy force pressure. If shorter elastics were needed, extra clamp-on hooks were placed medial to the lateral incisors to increase elastic pressure by forming an elastic triangle between the maxillary first molar, the canine and the lateral incisor hooks. To increase facemask force, the facemask elastics could be placed to the molar instead of the canine band or the facemask bar was reinserted away from the patient. If a patient did not wear Class III elastics, then any gain at night with headgear would recoil back during the day: there would be no net gain in anteroposterior correction. In a cooperative patient, a 3–4 mm anterior crossbite would correct to an edge-to-edge incisor relationship after two weeks. A Class II molar relationship with a 3 mm overjet could be produced one month later. When correction of the crossbite was not observed in two weeks, the patients were retested for compliance with the facemask and Class III elastics usage. In patients with deep underbites, a posterior bite plate made from glass ionomer cement was used to avoid occlusal interferences during the Class III correction. After correction, a protracted maxilla was maintained in the Class II position for 3 months before the RPE was removed. Class III elastics were used for a minimum 18 months following protraction as the teeth were being aligned and leveled. When orthodontic treatment was less than 18 months, then the patients were debanded and given clear acrylic retainers (1 mm Biocryl, Great Lakes Orthodontics, Tonawanda, NY) with embossed or bonded Class III buttons. These retainers allowed the patients to be debanded early yet provide interarch elastics wear for the 18 month period.
One goal in treatment was to overcorrect the Class III malocclusion into a Class II malocclusion. Highly motivated patients not only corrected the Class III malocclusion but could overcorrect to produce an 8 mm overjet. The overjet represented extra correction for dealing with relapse after the RPE was removed. Light Class II elastics placed late in treatment were used to correct the overcorrected occlusion.
Protraction of maxilla in adolescent patients
Figures 1, 2 and 3 show pre- and post-treatment records of our first protraction patient treated by the CHLA maxillary protraction, a 13-year old female who presented with repaired unilateral cleft lip and palate and a deficient maxilla. The frontal facial changes with maxillary protraction were similar to the LeFort 1 surgery: there was more nasal projection, more maxillary support for the dentition and nose, increased upper lip width and improved symmetry with the lower width, and more upper incisor display. The face looked natural as there are no steps created by surgical segments. With downward direction of elastic pull, there were no anterior open bites at the end of treatment with this protocol. The occlusion was not always an ideal Class I occlusion as most patients with cleft lip and palate were either missing a lateral incisor or had a smaller lateral incisor. Tight intercuspation of teeth was not always possible due to the tooth size discrepancies. However, there was a positive overjet and overbite. The upper dental midline was more difficult to control with protraction or distraction osteogenesis than with LeFort I surgery as surgery offered more control over the midline position, especially if the maxilla was segmented. If the midface was shallow with exopthalmus prior to protraction, then the protraction did not eliminate the facial concavity. Usually, a combination LeFort III/LeFort I surgery or malar implants would be recommended for these patients. In our pilot study of 30 patients, 24 were successfully treated with maxillary protraction. Of these 24 patients, none had additional surgery to correct residual problems. Six patients failed to complete the protraction treatment due to poor cooperation. All six patients were boys. One boy achieved overcorrection with the protocol, but then discontinued elastics shortly after attaining the desired result and relapsed to an edge-to-edge incisor relationship which was corrected using multi-loop edgewise (MEAW) mechanics.
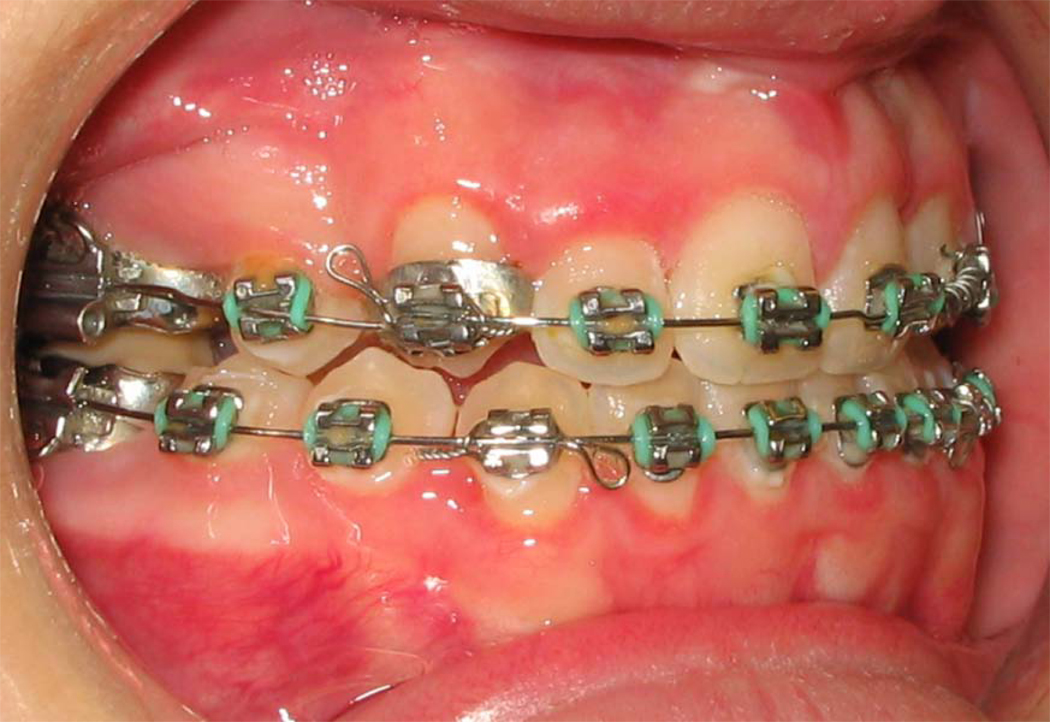
Figure 1.
Pretreatment. 13-year-old female with repaired unilateral cleft lip and palate planned for maxillary protraction. Fixed appliances were used to align premolars in preparation for maxillary protraction. (A) Extraoral frontal view; (B) extraoral profile view; (C) intraoral right lateral view; (D) intraoral frontal view; (E) intraoral left lateral view. (Color version of figure is available online.)
Figure 2.
Treatment changes in same patient after first three weeks of protraction. (A) Extaroral frontal view; (B) extraoral three-quarter view; (C) extraoral profile view; (D) intraoral right lateral view; (E) intraoral frontal view; (F) intraoral left lateral view; (G) palatal occlusal view; (H) mandibular occlusal view; (I) view of downward direction of elastic pull to facemask. (Color version of figure is available online.)
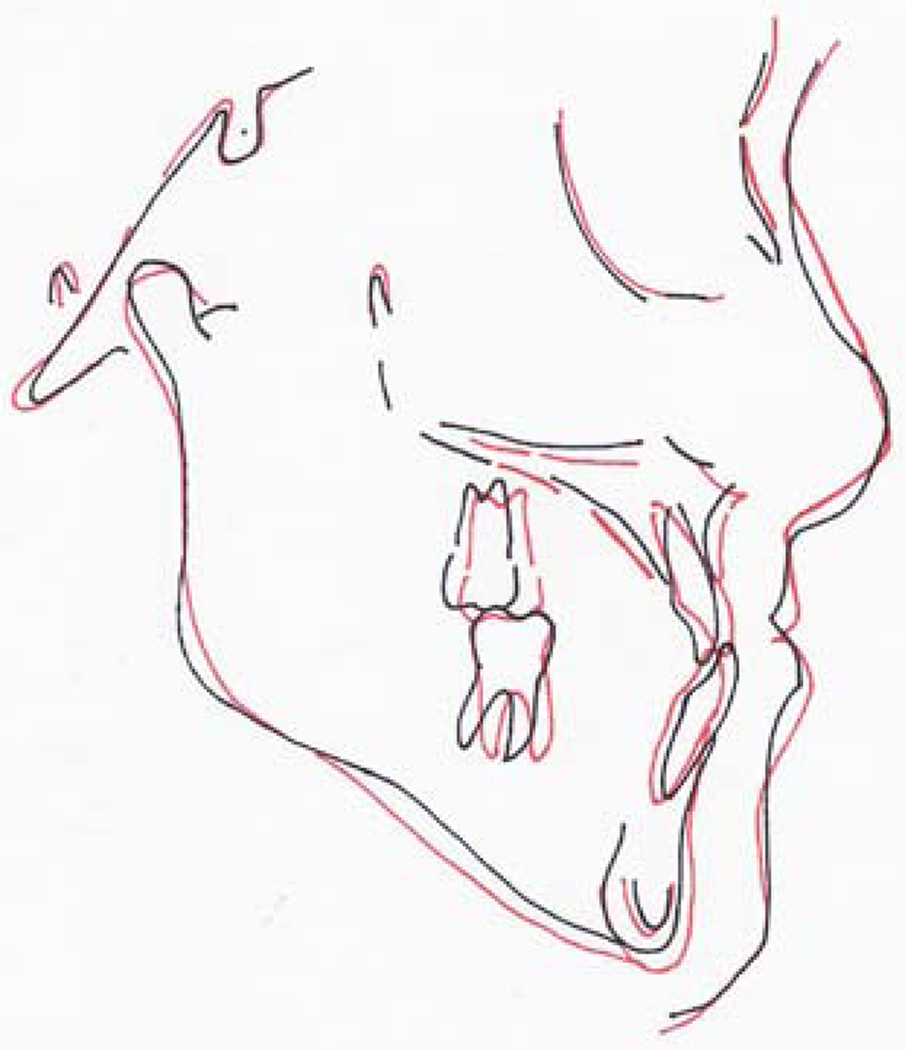
Figure 3.
Post-treatment. (A) Intraoral frontal view patient wearing retainers with artificial tooth; (B) pre-and post treatment tracing; (C) vacuum-form retainers with buttons for Cl III elastics. (Color version of figure is available online.)
During treatment, three lateral cephalometric radiographs were taken on our protraction patients: a pre-treatment radiograph, a maximal protraction radiograph and a (3 month) post-protraction radiograph. Figure 4 shows both maxillary incisor proclination and skeletal movement during the change between the first and second radiograph as evidenced by the change in unbanded second molar positions. The change between the second and third radiograph illustrated overcorrection of the Class III malocclusion into an 8–9 mm Class II overjet. Light Class II elastics were used to reduce the overjet. The Class II elastics were discontinued once an ideal overjet was obtained. If left unchecked, skeletal relapse could occur while the dentition was maintained in occlusion with interarch elastics. A final cephalometric radiograph could appear as a dental compensation of a Class III malocclusion with rotation of the occlusal plane even though skeletal advancement occurred early during the first month of maxillary protraction. In a pilot study of thirty patients who underwent maxillary protraction, we measured four components of Class III correction: maxillary length (Co –A pt), maxillary incisor proclination (SN-MIA) and mandibular incisor retroclination (I-MPA), and occlusal plane (SN-OP, SN-GoGn). All four components played a role in correcting the occlusion but the relative amount each component contributed to the correction varied greatly among the patients as did their level of cooperation. In this small sample, we could not separate out why some patients had more skeletal correction than others. At the occlusal level, the Wits analysis showed a correction from Class III to Class I (p<.05, Fisher exact test). The maxilla lengthened as measured from Condylion (Co) to A pt (p<.05). The majority of patients showed dental compensation and rotation of the occlusal plane under continuous Class III elastic wear; however, these observations did not show statistical differences with an older group of control patients who were being prepared for orthognathic surgery. None of the twenty-four patients with cleft lip and palate who underwent maxillary protraction needed additional orthognathic surgery. In other words, additional mandibular growth did not cause a need for re-treatment of the Class III malocclusion. Currently, we are trying to profile the patient who chose protraction treatment and carried the protocol to completion. A consistent characteristic found in patients who failed maxillary protraction treatment was an inability to follow the protocol exactly as it was presented to them. Their treatment was interrupted by periods of poor cooperation when they did not have a daily routine for turning the expansion screw, using the facemask and Class III elastics. We advised our patients who considered maxillary protraction that this treatment required considerable commitment and cooperation from the patient and additional appointments are usually required to check their progress.
Figure 4.
Lateral cephalometric radiographs of a patient treated by maxillary protraction demonstrating the importance of overcorrection and settling after expander removal. (A) Lateral cephalographs taken before protraction; (B) overcorrection with 9 mm of overjet; (C) settling of occlusion at the end of treatment.
A rationale for the use of microimplants for maxillary protraction
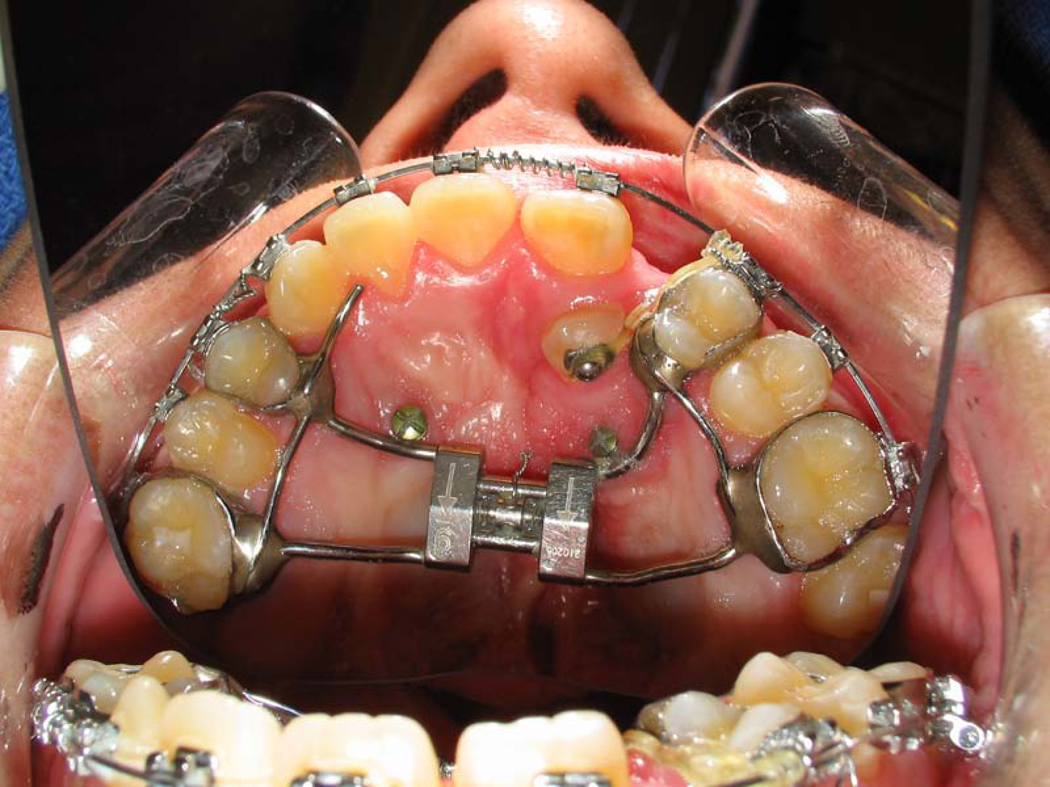
In our original study, we tried to calculate what percentage of the correction was attributable to maxillary incisor proclination, mandibular incisor retroclination, occlusal plane rotation and maxillary. The question we tried to address was how to increase the skeletal component percentage of the correction. Microimplants, known also as miniscrews and temporary anchorage devices (TADs) have the potential to transmit expansion and protraction forces directly to the bone and were used in a small number of patients to limit excessive dental compensation with Class III elastics and increase maxillary advancement in patients with large anterior crossbites that ranged from 8–14 mm. We found that microimplants could produce more skeletal change in our patients with cleft lip and palate while limiting skeletal relapse. Figure 5 shows the lateral cephalometric radiograph of a patient with a 12 mm Class III malocclusion and anterior open bite, who was originally referred for distraction of the maxilla. He was treated with microimplants and maxillary protraction because the patient refused surgery. Microimplants were placed near the palatal midline for the RPE to engage the palatal microimplants, thereby transferring the force of the intraoral elastics to the RPE and mobilized maxillary bone. After protraction, Class III elastics helped to limit the amount of skeletal relapse. A second set of microimplants were placed mesial to the mandibular canine in order to tie a metal wire loop between the microimplant and first molar band.22 This indirect wire tie was used to limit molar distalization and incisor retroclination during treatment with Class III elastics. The combination of maxillary and mandibular microimplants allowed very large malocclusions to be corrected without surgery. In our older patients, we found that it was possible to use microimplants to force the sutures open and to expand a maxilla; however, the expansion was not stable. Although RPE combined with microimplants expanded the maxilla without causing pain to an older patient, the screws tended to loosen during repetitive expansion and constriction. For a stable expansion in older patients, palatal distractors such as the Surgi-Tec distractor (Brussels, Belgium) that are completely bone borne were used with Surgical Assistance Rapid Palatal Expansion (SARPE).
Figure 5.
Microimplant-supported maxillary protraction. (A) Extraoral profile view; (B) intraoral frontal view showing lower microimplant position; (C) intraoral frontal view showing treatment changes; (D) palatal occlusal view showing microimplant positions; (E) pre-treatment lateral cephalogram; (F) post-treatment cephalogram after four months of maxillary protraction; (G) post-treatment extraoral profile view. (Color version of figure is available online.)
The placement of microimplants required planning to be done early on. If microimplants were to be used with RPEs, then the original design of the hyrax RPE was modified so that the screw housing was seated high in the palatal vault near the mucosa in order to engage the microimplant. For the mandibular microimplants, only the gingiva at the site of microimplant access was anesthetized by local anesthetics prior to placement. During positioning of the microimplant, a painful response from the patient would warn the orthodontist and surgeon that the microimplant had encroached the mental nerve or dental root and needed to be redirected.
Although maxillary protraction may theoretically be possible in older patients, many patients in their late teens are not cooperative enough to wear facemasks and elastics. Orthognathic surgery which is faster and less dependent on patient compliance should be the first choice for adult and late teenage patients with a skeletal Class III discrepancy. For the patient with cleft lip and palate and maxillary hypoplasia who is unwilling to undergo orthognathic surgery, a SARPE with a LeFort 1 cut can be used to simultaneously expand and protract the maxilla. The recovery for this surgery is less than a week. In terms of skeletal versus dental movements, the SARPE paradoxically produced a high amount of maxillary incisor proclination and lower incisor retroclination. It is not known whether palatal microimplants can limit this protraction response.
DISCUSSION
Maxillary protraction during early adolescence can be a viable alternative to orthognathic surgery in certain cleft lip and palate patients. This technique worked well when an adolescent patient was highly motivated. Thus far, the maxillary protraction protocol has been more successful in girls than in boys during the middle school years. The reasons for patient compliance varied: some patients wanted earlier correction of the facial deformity, some feared orthognathic surgery. The protraction protocol did not work in patients who intermittently followed the protocol, did not overcorrect into Class II occlusion or discontinued the Class III elastics before bony consolidation occurred. Maxillary protraction is therefore not for all patients. Weekly visits screened for problems with the technique or the compliance as the patient was tested for competency with the expansion/constriction and facemask treatment. The patient should be able to insert the activator key into the turnbuckle hole of the RPE and without hand support. If the activator key did not stay in the turnbuckle hole, then it was not properly inserted. In addition, we checked whether the expander was in an expanded position after 28 turns (4 turns/day for seven days) were completed. When patients reported pain during expansion, then they may have been too old to be expanded with an RPE due to early fusion of the maxillary sutures. Their treatment was changed to conventional orthognathic surgery or SARPE/LeFort 1 protraction. In one case, late dental eruption of permanent teeth delayed the timing of treatment and caused problems when the maxillary sutures fused before the permanent dentition had completed their eruption.
For the orthodontist, the protocol involves an additional cost for making appliances, remaking appliances that do not fit well and extra patient appointments. Some patients will stop the protocol procedures within the first month and elect surgery. It is helpful to let patients considering maxillary protraction meet other patients undergoing protraction treatment for mutual encouragement and for patients to see the final outcomes. Our interest in this technique continues because thus far, we have not re-treated any of the patients with surgery if they completed the maxillary protraction protocol. Treatment relapse often occurred but in most cases, it was planned for by overcorrection. Our treatment failures occurred early during the expansion/constriction phase of treatment. Either the device failed or patient compliance issues were identified. Thus, the first three to four months of treatment was used to determine whether the treatment would be successful and avoid long-term investments of time and resources. Most parents were not sure whether their child would be compliant enough to carry out the protocol but were willing to try out the technique in order to avoid orthognathic surgery.
We have used microimplants in challenging cases per our patient’s request. Some of these patients were candidates for maxillary distraction osteogenesis and secondary orthognathic surgery However, at this time, it (what is “it” your protocol- please be specific because it is unclear?) is an experimental procedure and requires more study. With maxillary protraction, microimplants are likely to play a role in maximizing skeletal change and preventing skeletal relapse. As a closing note, it should be noted that orthodontists tend to adapt other techniques into their practice. The most common mistakes by other orthodontists when trying our protocol were forgetting to use Class III elastics to support the protraction and placing a maxillary archwire during expansion and constriction.
Acknowledgements
The multicenter clinical trial is being planned through a grant from the NIDCR: NIH R21 DE19164-01
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hennekam RCM, Krantz ID, Allanson JE, editors. Gorlin’s Syndromes of the Head and Neck. 5th edition. Oxford University Press; 2010. Orofacial clefting syndrome: General aspects; p. 943. [Google Scholar]
- 2.Vargervik K. Growth characteristics of the premaxilla and orthodontic treatment principles in bilateral cleft lip and palate. Cleft Palate Craniofac J. 1983;20:289–302. [PubMed] [Google Scholar]
- 3.Arosarena OA. Cleft Lip and Palate. Otolaryngol Clin N Am. 2007;40:27–60. doi: 10.1016/j.otc.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Liao YF, Mars M. Long-term effects of clefts on craniofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2005a;42:601–609. doi: 10.1597/04-163r.1. [DOI] [PubMed] [Google Scholar]
- 5.Liao YF, Mars M. Long-term effects of palate repair on craniofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2005b;42:594–600. doi: 10.1597/04-077r.1. [DOI] [PubMed] [Google Scholar]
- 6.Liao YF, Mars M. Long-term effects of lip repair on dentofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2005c;42:526–532. doi: 10.1597/04-015.1. [DOI] [PubMed] [Google Scholar]
- 7.Mars M, Houston WJB. A preliminary study of facial growth and morphology in unoperated male unilateral cleft lip and palate subjects over 13 years of age. Cleft Palate Craniofac J. 1990;27:7–10. doi: 10.1597/1545-1569(1990)027<0007:apsofg>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 8.Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 1987;24:5–77. [PubMed] [Google Scholar]
- 9.Wolford LM, Stevao ELL. Proc (Bayl Univ Med Cent) 2002;15(3):250–254. doi: 10.1080/08998280.2002.11927848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaban LB, Troulis MJ. Sequential Management of the Child with Cleft Lip and Palate. In: Kaban LB, Troulis MJ, editors. Pediatric Oral and Maxillofacial Surgery. Philadelphia: Saunders; 2004. pp. 418–419. [Google Scholar]
- 11.Rachmiel A. Treatment of maxillary cleft palate: distraction osteogenesis versus orthognathic surgery-part one: maxillary distraction. J Oral & Maxillofac Surg. 2007;65(4):753–757. doi: 10.1016/j.joms.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Steinberg B, Padwa BL, Boyne P, Kaban L. State of the art in oral and maxillofacial surgery: treatment of maxillary hypoplasia and anterior palatal and alveolar clefts. Cleft Palate Craniofac J. 2000;37:421–422. doi: 10.1597/1545-1569_2000_037_0421_ltte_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 13.Williams MD, Sarver DM, Sadowsky PL, Bradley E. Combined rapid maxillary expansion and protraction facemask in the treatment of Class III malocclusions in growing children: a prospective long-term study. Semin Orthod. 1997;3:265–274. doi: 10.1016/s1073-8746(97)80059-x. [DOI] [PubMed] [Google Scholar]
- 14.Tindlund RS. Orthopedic protraction of the midface in the deciduous dentition. Results covering 3 years out of treatment. J Craniomaxillofac Surg. 1989;17 Suppl 1:17–19. doi: 10.1016/s1010-5182(89)80032-0. [DOI] [PubMed] [Google Scholar]
- 15.Ranta R. Orthodontic treatment in adults with cleft lip and palate. J Craniomaxillofac Surg. 1989;17 Suppl 1:42–44. doi: 10.1016/s1010-5182(89)80041-1. [DOI] [PubMed] [Google Scholar]
- 16.So LL. Effects of reverse headgear treatment on sagittal correction in girls born with unilateral complete cleft lip and cleft palate-skeletal and dental changes. Am J Orthod Dentofacial Orthop. 1996;109:140–147. doi: 10.1016/s0889-5406(96)70174-9. [DOI] [PubMed] [Google Scholar]
- 17.Buschang PH, Porter C, Genecov E, Genecov D, Sayler KE. Face mask therapy of preadolescents with unilateral cleft lip and palate. Angle Orthod. 1994;64:145–150. doi: 10.1043/0003-3219(1994)064<0145:FMTOPW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Liou EJ, Tsai WC. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005;42:121–127. doi: 10.1597/03-107.1. [DOI] [PubMed] [Google Scholar]
- 19.Liou EJ. Effective maxillary orthopedic protraction for growing Cl III patients: a clinical application simulates distraction osteogenesis. Prog Orthod. 2005;6:154–171. [PubMed] [Google Scholar]
- 20.Do-Delatour T, Ngan P, Martin CA, Ramus T, Gunel E. Effect of alternate maxillary expansion and contraction on protraction of the maxilla: A pilot study. HKDJ. 2009;6:72–82. [Google Scholar]
- 21.Shang W, Scadeng M, Yamashita DD, et al. Manipulating the Mandibular Distraction Site at Different Stages of Consolidation. J Oral Maxillofac Surg. 2007;65:840–846. doi: 10.1016/j.joms.2005.10.037. [DOI] [PubMed] [Google Scholar]
- 22.Vachiramon A, Urata M, Kyung HM, et al. Clinical applications of orthodontic microimplants in craniofacial patients. Cleft Palate Craniofac J. 2009;46:136–146. doi: 10.1597/06-219.1. [DOI] [PubMed] [Google Scholar]