Abstract
Objectives. We determined factors associated with hearing aid acquisition in older adults.
Methods. We conducted a population-based, prospective study that used information from 3 examinations performed on study participants as part of the Epidemiology of Hearing Loss Study (1993–2005). We included participants (n = 718; mean age = 70.5 years) who exhibited hearing loss at baseline or the first follow-up and had no prior history of hearing aid use. We defined hearing loss as a pure tone threshold average (PTA) at 0.5, 1, 2, and 4 kilohertz in the better ear of greater than 25 decibels Hearing Level.
Results. The 10-year cumulative incidence of hearing aid acquisition was 35.7%. Associated factors included education (college graduate vs all others: hazard ratio [HR] = 2.5; 95% confidence interval [CI] = 1.5, 4.1), self-perception of hearing (poor vs good or better: HR = 2.5; 95% CI = 1.3, 5.0), score on a perceived hearing handicap inventory (+ 1 difference: HR = 1.1; 95% CI = 1.0, 1.1), and PTA (+ 5 dB difference: HR = 1.4; 95% CI = 1.2, 1.6).
Conclusions. The low rate of hearing aid ownership among older adults is a problem that still needs to be addressed.
A number of observational studies have reported that hearing loss negatively affects quality of life.1–5 Among the participants in the Epidemiology of Hearing Loss Study (EHLS), significant relationships were found between severity of hearing loss and impaired physical and social functioning.1 Other studies have revealed a positive influence of hearing aid usage on quality of life.6–12 A systematic review and meta-analysis of studies related to hearing aids and quality of life concluded that hearing aid usage in adults was associated with improvements in psychological, social, and emotional well-being when hearing-specific and communication-specific measures were used for quality-of-life assessment.6 In a randomized trial among older patients at Veterans Affairs clinics, results suggested that hearing aid use led to significant improvements in social and emotional functioning, communication, cognition, and depression, with all effects except cognition being sustained for at least 1 year.7,8
Despite the psychosocial benefits of hearing aid use, it has been estimated that just 20% to 25% of hearing-impaired individuals use hearing aids.13–15 A 1995 study revealed that only about one third of adults aged 70 years or older who had a reported hearing problem had used hearing aids within the past year.16
Researchers have conducted clinic-based investigations and cross-sectional population studies and surveys to evaluate characteristics related to seeking help for a hearing loss and obtaining hearing aids. In general, the factors found to have an influence on the decision to seek help include a self-perception of reduced hearing ability or decline in hearing sensitivity, negative impact of hearing quality on daily life, and comments or encouragement from others.17–20 Conversely, studies investigating characteristics associated with not seeking treatment for a hearing loss have found that denial of the loss, self-image implications, fear of social consequences, fear of aging, acceptance of a hearing loss as a normal part of the aging process, and lack of social pressure have played a role.18,21 Hearing aids in particular were not sought because of concerns regarding cost, effectiveness, stigma, and discomfort.18,21,22
Previous studies have not been population based and prospective in nature and have not evaluated multiple factors simultaneously, including demographic characteristics, standard measures of hearing ability, and self-perception of hearing quality and handicap. Some studies have been conducted in clinical populations in which participants have already made a decision to seek help for a perceived hearing loss.17,20 Factors influencing the decision to acquire a hearing aid among patients seen at an audiology clinic may differ from those in effect among participants in a population-based study of aging.
Investigators in the Netherlands have conducted population studies, but those were cross-sectional in design; also, in the Netherlands the cost of a hearing aid may be partially reimbursed, either through public funding or the patient's employer.18,19 Because cost may be an important factor in the decision to acquire a hearing aid, the results of studies conducted in the Netherlands may be expected to differ from studies conducted in the United States, where hearing aids are not universally covered by private health insurance or Medicare. Previous survey work investigating the prevalence of hearing aid use in the United States has relied on self-reported hearing loss or hearing difficulty, which may introduce error and which prevents any adjustment for measured hearing loss.21,22 In addition, survey work is subject to response bias and may not be representative of the general population.
Our goal for this population-based study was to estimate, for the first time, the 10-year incidence of hearing aid acquisition among participants with a demonstrated hearing loss and to determine the factors that predicted hearing aid purchase.
METHODS
Participants were residents of Beaver Dam, Wisconsin, who had participated in the Beaver Dam Eye Study (BDES). The BDES began recruitment in 1987 and 1988 by inviting all residents of the city or township of Beaver Dam who were aged 43 through 84 years to participate in a population-based study of age-related eye disorders. Of the 5924 eligible residents, 4926 (83%) were examined in the first BDES phase, conducted from 1988 to 1990. The first follow-up BDES examination was performed 5 years later, from 1993 to 1995. At the same time, all baseline BDES participants were invited to participate in the first EHLS examination (EHLS-1). There were 3753 participants (82.6% of the 4541 living BDES participants) who participated in EHLS-1. Follow-up studies were conducted 5 years (EHLS-2) and 10 years (EHLS-3) after baseline. Additional details on the EHLS have previously been reported.23–25
Participants included in this study had a demonstrated hearing loss at either EHLS-1 or EHLS-2. We defined hearing loss as a pure-tone threshold average (PTA) at 0.5, 1, 2, and 4 kilohertz of more than 25 decibels Hearing Level (HL) in the better ear. Participants had no history of hearing aid use before the detection of a hearing loss.
Measurements
Audiometry.
Pure-tone air-conduction thresholds (measured as decibel HL) were determined during each study period according to the American Speech-Language-Hearing Association guidelines.26 We followed American National Standards Institute standards for equipment calibration.27,28 We measured thresholds in both ears at 0.5, 1, 2, 3, 4, 6, and 8 kilohertz. We calculated 3 PTAs of the better ear: the average of the 0.5, 1, 2, and 4 kilohertz thresholds; the average of the 0.5, 1, and 2 kilohertz thresholds; and the average of the 4, 6, and 8 kilohertz thresholds. We used the female talker version of the NU-6 test (Northwestern University Auditory Test no. 6) for word recognition testing, conducted in quiet and in competing message. Word lists were presented at 36 decibels above the 2 kilohertz threshold in the better ear. For competing message, a single male talker was included at 8 decibels below the female voice.29,30 Word recognition scores consisted of the percentage of words the participant correctly stated. Previous publications have reported audiometric procedure details.23,30
Hearing aid acquisition.
Hearing aid usage was self-reported in response to the question: “Have you ever worn a hearing aid or amplifying device?” To be included, participants must have answered “no” at the time of the EHLS examination during which the hearing loss was first detected. Hearing aid acquisition was considered to have occurred if, at the EHLS examination(s) after the identification of a hearing loss detection (EHLS-2 or EHLS-3), the participant answered “yes” to the same question.
Covariates.
Covariates included age, gender, education, marital status (currently married, not married), self-perception of hearing quality (excellent, very good, good, fair, poor), self-perception of hearing loss (“Do you feel you have a hearing loss?”), perception of friends and relatives with respect to the participant's hearing, self-reported family history of hearing loss (father, mother, or siblings), impaired cognition, and the participant's score on the Hearing Handicap Inventory for the Elderly—Screening Version (HHIE-S) score.31
Education was modeled as a 4-level class variable (< 12, 12, 13–15, and ≥ 16 years) and as a dichotomous variable (< 16 vs ≥ 16 years [termed “college graduate”]). Impaired cognition was defined as a score of less than 24 on the Mini-Mental State Examination or a report of dementia by a proxy.32 The HHIE-S consists of 10 questions measuring the perceived social/situational and emotional effects of a hearing problem. Possible responses for each question are “no” (0 points), “yes” (4 points), and “sometimes” (2 points). Points are added across the 10 questions; thus, the HHIE-S score ranges from 0 to 40 points, with higher values indicating a greater degree of perceived handicap related to a hearing problem. For self-perception of hearing quality, we combined responses in the categories of excellent, very good, and good because of small numbers of responses in those categories.
Statistical Analyses
The follow-up period was divided into two 5-year segments, corresponding with the EHLS study phases. For participants whose hearing loss was diagnosed at EHLS-1, the first 5-year segment (0–5 years of follow-up) began at EHLS-1 and ended at EHLS-2, at which time hearing aid usage was ascertained. If the participant did not report using a hearing aid at that time, the second 5-year segment (5–10 years of follow-up) began at EHLS-2 and ended at EHLS-3, at which time hearing aid usage was again ascertained. For participants who did not have a hearing loss at EHLS-1 but did at EHLS-2, the first (and only) 5-year segment (0–5 years of follow-up) began at EHLS-2 and ended at EHLS-3.
To determine the strength of association between hearing aid acquisition and the covariates, we used Cox discrete-time proportional hazards modeling. For categorical factors, a reference category was chosen, and indicator variables were created for the remaining categories. Dichotomous factors were entered as 0 or 1. We used the covariate measurements collected at the beginning of each follow-up period, with the exception of impaired cognition. Because the Mini-Mental State Examination was not administered at EHLS-1, we used the cognition status determined at the end of each follow-up period.
Initial modeling was performed for each of the covariates separately, with age and gender adjustment only. All covariates were considered for the multivariate model, and we selected the final model in a stepwise fashion. Education and income were strongly correlated and provided approximately the same goodness of fit, so we chose education for the final model to increase sample size (there were more missing data for income). We computed hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) from the parameter estimates and their SEs. We used SAS version 9.1 (SAS Institute, Cary, NC) to perform all analyses.
RESULTS
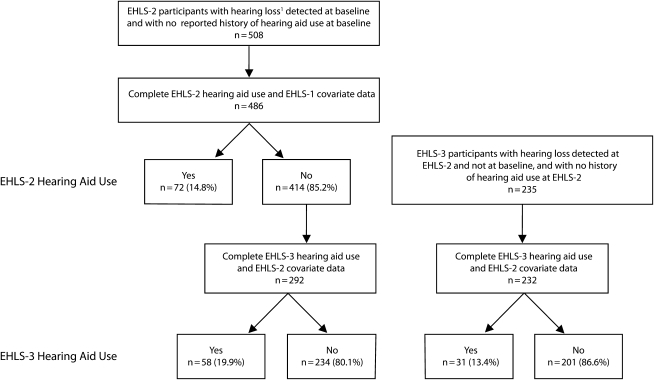
A total of 718 participants (mean age = 70.5 years) with a hearing loss were followed for at least 5 years (Figure 1). Among these participants, the 5-year incidence of hearing aid acquisition was 14.3%. The 5-year incidence of hearing aid acquisition was 14.8% for the 486 participants whose hearing loss was detected at EHLS-1 (baseline) and 13.4% for the 232 participants whose hearing loss was detected at EHLS-2. The 10-year cumulative incidence of hearing aid acquisition was 35.7%. Approximately 20% of the participants followed for 10 years acquired a hearing aid 5 to 10 years after a hearing loss was initially detected.
FIGURE 1.
Study population selection and incidence of hearing aid acquisition: Beaver Dam, WI, 1993–2005.
Note. EHLS = Epidemiology of Hearing Loss Study. Hearing loss is defined as a pure-tone threshold average at 0.5, 1, 2, and 4 kHz of greater than 25 dB hearing level in the better ear.
Results of age- and gender-adjusted analyses are presented in Table 1. Hearing aid acquisition was associated with education and a number of perceived hearing factors and hearing capacity measurements. College graduation significantly increased the likelihood of acquiring a hearing aid (HR = 1.8; 95% CI = 1.1, 2.9), and this relationship was stronger in the period of 5–10 years after hearing loss detection (HR = 2.6; 95% CI = 1.1, 6.1). Higher income also demonstrated a nonsignificant, positive relationship with hearing aid acquisition. Regarding the perceived hearing factors, a significant linear association existed between perceived hearing quality and aid acquisition (P < .01), with those reporting poor quality having a rate ratio of 6.2 (95% CI = 3.5, 11.0) compared with those reporting excellent, very good, or good hearing. In the first 5 years of follow-up after hearing loss detection, only 9.5% of the participants who rated their hearing as good or better acquired an aid, but close to 36% of participants who perceived their hearing as poor acquired an aid. In the 5- to 10-year follow-up period, nearly 41% of the participants who reported poor hearing obtained an aid, compared with about 13% of the participants reporting good or better hearing.
TABLE 1.
Distribution of Risk Factors for Incidence of Hearing Aid Acquisition: Beaver Dam, WI, 1993–2005
| 0–5 Years of Follow-Up> |
6–10 Years of Follow-Up |
Both Follow-Up Periods Combined,HR (95% CI) | |||||
| Risk Factors | Hearing Aid (n = 103) | No Hearing Aid (n = 615) | HR (95% CI) | Hearing Aid (n = 58) | No Hearing Aid (n = 234) | HR (95% CI) | |
| Men, % | 57.3 | 54.0 | 1.23 (0.78, 1.92) | 44.8 | 61.5 | 0.58 (0.32, 1.07) | 0.95 (0.66, 1.36) |
| Education (4 levels), y, % | |||||||
| < 12 (Ref) | 28.2 | 27.3 | 1.00 | 25.9 | 25.2 | 1.00 | 1.00 |
| 12 | 48.5 | 48.9 | 1.00 (0.60, 1.64) | 46.6 | 53.0 | 0.91 (0.45, 1.87) | 0.97 (0.65, 1.46) |
| 13–15 | 7.8 | 13.3 | 0.58 (0.25, 1.33) | 10.3 | 12.8 | 0.78 (0.27, 2.26) | 0.66 (0.35, 1.25) |
| ≥ 16 | 15.5 | 10.4 | 1.47 (0.74, 2.90) | 17.2 | 9.0 | 2.38 (0.89, 6.36) | 1.69 (0.97, 2.95) |
| College graduate (≥ 16 vs < 16 y) | 15.5 | 10.4 | 1.57 (0.86, 2.84) | 17.2 | 9.0 | 2.59 (1.10, 6.09) | 1.81 (1.12, 2.94) |
| Income, $, % | |||||||
| 0–9000 (Ref) | 12.2 | 11.1 | 1.00 | 14.0 | 9.4 | 1.00 | 1.00 |
| 10 000–19 000 | 21.1 | 30.3 | 0.62 (0.27, 1.42) | 16.0 | 23.3 | 0.54 (0.17, 1.74) | 0.63 (0.32, 1.22) |
| 20 000–29 000 | 24.4 | 21.0 | 1.09 (0.47, 2.49) | 24.0 | 28.2 | 0.90 (0.29, 2.75) | 1.02 (0.53, 1.97) |
| 30 000–44 000 | 25.6 | 21.5 | 1.10 (0.48, 2.55) | 24.0 | 19.3 | 1.80 (0.54, 6.05) | 1.25 (0.63, 2.46) |
| ≥ 45 000 | 16.7 | 16.1 | 0.99 (0.39, 2.52) | 22.0 | 19.8 | 1.78 (0.51, 6.20) | 1.16 (0.56, 2.43) |
| Married, % | 60.2 | 64.8 | 0.78 (0.48, 1.27) | 64.9 | 62.3 | 1.99 (0.98, 4.03) | 1.06 (0.71, 1.57) |
| Perceived hearing, % | |||||||
| Excellent, very good, good (Ref) | 39.8 | 63.6 | 1.00 | 29.3 | 50.0 | 1.00 | 1.00 |
| Fair | 46.6 | 32.4 | 2.34 (1.49, 3.68) | 48.3 | 41.9 | 2.22 (1.12, 4.40) | 2.31 (1.58, 3.36) |
| Poor | 13.6 | 4.1 | 5.67** (2.71, 11.87) | 22.4 | 8.1 | 9.68** (3.56, 26.27) | 6.16** (3.47, 10.96) |
| Self-perception of hearing loss | 86.0 | 67.3 | 3.21 (1.76, 5.86) | 91.2 | 77.2 | 3.55 (1.31, 9.58) | 3.39 (2.03, 5.65) |
| Family/friends think have hearing loss | 62.0 | 43.9 | 2.26 (1.43, 3.55) | 80.4 | 50.2 | 6.05 (2.83, 12.94) | 3.01 (2.05, 4.42) |
| Family history of hearing loss | 63.2 | 49.9 | 1.85 (1.15, 2.98) | 67.9 | 56.0 | 1.66 (0.86, 3.21) | 1.80 (1.22, 2.64) |
| Impaired cognition, % | 14.6 | 15.0 | 0.90 (0.48, 1.69) | 20.0 | 14.1 | 1.32 (0.61, 2.90) | 1.06 (0.65, 1.72) |
| Age, y, mean (SD) | 71.0 (10.0) | 70.4 (9.0) | 1.01 (0.99, 1.04) | 74.9 (8.8) | 72.3 (8.4) | 1.03 (0.99, 1.07) | 1.02 (0.996, 1.04) |
| HHIE-S score, mean (SD) | 11.2 (9.3) | 6.0 (6.9) | 1.08 (1.06, 1.11) | 11.9 (9.5) | 7.3 (6.9) | 1.09 (1.04, 1.13) | 1.08 (1.06, 1.11) |
| PTA0.5–4 kHz, better ear, mean (SD) | 35.7 (8.4) | 31.7 (5.3) | 1.60 (1.36, 1.87) | 39.3 (6.1) | 36.2 (6.9) | 1.33 (1.07, 1.67) | 1.51 (1.33, 1.72) |
| PTA0.5–2 kHz, better ear, mean (SD) | 27.9 (9.8) | 23.8 (7.0) | 1.44 (1.26, 1.66) | 32.7 (7.7) | 27.8 (8.6) | 1.33 (1.10, 1.60) | 1.41 (1.26, 1.57) |
| PTA4–8 kHz, better ear, mean (SD) | 63.2 (13.3) | 59.1 (14.2) | 1.11 (1.02, 1.21) | 63.4 (11.6) | 64.8 (14.2) | 0.96 (0.84, 1.09) | 1.06 (0.99, 1.14) |
| Word recognitionquiet, mean (SD) | 81.2 (15.2) | 87.4 (9.5) | 0.96 (0.94, 0.98) | 82.4 (12.6) | 83.0 (13.5) | 1.00 (0.98, 1.02) | 0.97 (0.96, 0.99) |
| Word recognitionnoise, mean (SD) | 34.0 (19.0) | 42.6 (18.8) | 0.97 (0.96, 0.99) | 35.0 (17.7) | 39.0 (18.0) | 0.99 (0.97, 1.01) | 0.98 (0.97, 0.99) |
Note. CI = confidence interval; HHIE-S = Hearing Handicap Inventory for the Elderly—Screening Version; HR = hazard ratio; PTA = pure-tone threshold average at 0.5, 1, 2, and 4 kHz in the better ear; hazard ratio for +5 dB difference in PTA. HRs were adjusted for age and gender.
**Test for trend P < .01.
Self-perception of hearing loss and having friends or relatives think that the participant had a hearing loss resulted in a rate of aid acquisition more than 3 times the rate of those without these factors. A family history of hearing loss was also significantly associated with hearing aid acquisition (HR = 1.8; 95% CI = 1.2, 2.6), as was the perceived degree of handicap related to hearing (HR1 unit of HHIE-S score = 1.08; 95% CI = 1.06, 1.11). With respect to the measurements of hearing ability, a higher PTA was associated with significantly elevated rates of aid acquisition, particularly for the average of the 0.5, 1, 2, and 4 kilohertz thresholds (+ 5 dB difference: HR = 1.5; 95% CI = 1.3, 1.7). Higher word recognition scores in quiet (HR = 0.97; 95% CI = 0.96, 0.99) and in competing message (HR = 0.98; 95% CI = 0.97, 0.99) resulted in lower rates of hearing aid aquisition.
Significant factors in the best-fitting multivariate model (with age and gender) included education (college graduate vs all others), self-perception of hearing quality, perceived degree of handicap related to hearing (HHIE-S score), and the PTA of the 0.5, 1, 2, and 4 kilohertz thresholds in the better ear (Table 2). There was no difference in the factors included in the best-fitting model for the 2 follow-up periods. College graduates were 2.5 times (95% CI = 1.5, 4.1) as likely to acquire a hearing aid as were those without a college degree. Participants who considered their hearing to be poor also had an HR of 2.5 (95% CI = 1.3, 5.0), compared with participants who perceived their hearing to be good or better. The rate of hearing aid acquisition also continued to have a significant, positive association with the HHIE-S score (+ 1 difference: HR = 1.05; 95% CI = 1.03, 1.08) and the PTA0.5–4, better ear (+ 5 dB difference: HR = 1.4; 95% CI = 1.2, 1.6).
TABLE 2.
Multivariate Model of Risk Factors for Incidence of Hearing Aid Acquisition: Beaver Dam, WI, 1993–2005
| Risk Factors | 0–5 Years of Follow-Up, HR (95% CI) | 6–10 Years of Follow-Up, HR (95% CI) | Both Follow-Up Periods Combined, HR (95% CI) |
| Age | 1.01 (0.98, 1.04) | 1.04 (0.99, 1.08) | 1.01 (0.99, 1.04) |
| Men | 0.99 (0.61, 1.60) | 0.36 (0.18, 0.74) | 0.73 (0.49, 1.08) |
| College graduate | 2.16 (1.15, 4.08) | 3.31 (1.30, 8.39) | 2.45 (1.46, 4.11) |
| Perceived hearing | |||
| Excellent, very good, good (Ref) | 1.00 | 1.00 | 1.00 |
| Fair | 1.58 (0.95, 2.61) | 1.74 (0.84, 3.62) | 1.63 (1.08, 2.47) |
| Poor | 2.07* (0.83, 5.15) | 4.34* (1.34, 14.04) | 2.50** (1.25, 5.03) |
| HHIE-S score | 1.05 (1.02, 1.09) | 1.05 (1.01, 1.10) | 1.05 (1.03, 1.08) |
| PTA0.5–4 kHz, better ear | 1.43 (1.20, 1.70) | 1.21 (0.94, 1.55) | 1.36 (1.18, 1.56) |
Note. CI = confidence interval; HHIE-S = Hearing Handicap Inventory for the Elderly—Screening Version; HR = hazard ratio; PTA = pure-tone threshold average at 0.5, 1, 2, and 4 kHz in the better ear; hazard ratio for +5 dB difference in PTA.
*Test for trend P ≤ .05; **test for trend P < .01.
Among participants who reported having been told that they would benefit from a hearing aid and who were followed for 10 years, prominent reasons given for not acquiring an aid included not needing it, the cost, the inconvenience of wearing an aid, and the poor hearing-aid experience of others (Table 3). The frequency of the cited reasons varied by gender and by the number of years since the hearing loss was detected. The most frequent responses cited as being the main reason for not obtaining an aid were cost (overall, 27%; women, 34%; men, 23%) and not needing an aid (overall, 26%; women, 27%; men, 25%).
TABLE 3.
Reasons for Not Acquiring a Hearing Aid: Beaver Dam, WI, 1993–2005
| 5 Years of Follow-Up |
10 Years of Follow-Up |
|||
| Reasons | Men (n = 58), % | Women (n = 32), % | Men (n = 29), % | Women (n = 10), % |
| Did not need it | 59.3 | 52.9 | 51.7 | 60.0 |
| Cost | 49.2 | 55.6 | 55.2 | 70.0 |
| Calls attention to handicap | 6.8 | 8.8 | 0.0 | 0.0 |
| Inconvenient to wear | 37.3 | 50.0 | 85.7 | 40.0 |
| Would not know where to buy | 17.6 | 13.8 | 17.2 | 0.0 |
| Poor experience of others | 31.0 | 45.5 | 55.2 | 60.0 |
| Too old to benefit | 5.2 | 15.6 | 7.1 | 0.0 |
Note. Table reports on participants whose pure-tone threshold average at 0.5, 1, 2, and 4 kHz in the better ear was determined to be greater than 25 dB Hearing Level at baseline. The only participants included are those who reported having been told that they would benefit from a hearing aid.
DISCUSSION
We found that close to two thirds of the individuals with a hearing loss who were followed for 10 years did not acquire a hearing aid, despite the fact that hearing and perceived hearing handicap worsened over this period (mean PTA0.5–4 kHz, better ear: baseline = 31.3, follow-up = 40.3, P < .001; mean word recognitioncompeting message: baseline = 42.5%, follow-up = 30.5%, P < .001; mean HHIE-S: baseline = 5.7, follow-up = 9.9, P < .001) and the fact that participants were participating in a study focused on hearing. The 5-year incidence of hearing aid acquisition was 14%, and the 10-year incidence was 36%. These rates are similar to previously reported prevalence rates of hearing aid use. In the baseline EHLS cohort we found that among individuals with a hearing loss (PTA0.5–4 kHz, worse ear > 25 dB), 20.7% had a history of using a hearing aid, although only 14.6% were current users.13 In a slightly older study population from the Framingham cohort (age range 63–95 years in 1983–1985), 25% of the participants who reported a hearing problem stated that they had used an aid at some time.33 Among a group of Netherlands participants who were aged 85 years between 1997 and 1999 and who had a PTA1–4 kHz, better ear greater than 35 decibels HL, 23% agreed to a first-time hearing aid fitting within the next year.34
Factors found to be significantly and independently related to first-time use of a hearing aid included education (college graduate), hearing loss severity (measured as the PTA0.5–4 kHz, better ear), hearing handicap score, and self-perception of hearing quality. These factors were the same for both acquisition within the first 5 years and acquisition within 5–10 years after detection. Education and income are correlated, and digital hearing aids are expensive, so it is likely that income may have accounted for some of the observed education effect in our study. In previous clinical and survey work, self-perceived hearing quality has been found to be associated with hearing aid purchase.15,17 In a recent clinic-based investigation, a 10-point scale for self-rating of hearing ability was found to be a significantly strong predictor of hearing aid purchase (odds ratio = 0.47 for 1 unit improvement).17 However, no adjustment was made for other potential predictors. In the 2004 survey of National Family Opinion participants, close to 64% of first-time hearing aid owners stated that a self-perceived decline in hearing influenced the decision to acquire an aid.15
We focused on hearing aid acquisition after the identification of a hearing impairment in a population-based investigation of aging and sensory loss; however, we did not focus on the decision to seek help for a hearing problem. Studies have found that self-perceived hearing quality and the impact of hearing loss on daily life are influential factors in an individual's decision to seek help for hearing difficulties.18–20 In a group of participants aged 55 years or older with a PTA0.5–4 kHz, better ear of 30 decibels HL or higher, the rate of physician consultation was significantly associated with self-perception of hearing quality, whether the participant's hearing was bothersome on a daily basis, whether others had complained about the participant's hearing, and whether others had advised the participant to obtain a hearing aid.19
We found that the reasons most often cited for not acquiring an aid were the perception that the aid was unnecessary, the cost, the inconvenience, and the poor experience of others. Similar reasons have been previously reported.21,22,33,34 In a 1998 survey of older National Family Opinion panel members (aged 50 years or older), close to 70% of the hearing-impaired respondents who were not using hearing aids stated that their hearing was not bad enough to need an aid or that they could get along without one, and 55% felt that hearing aids were too expensive.21 The strong impact of the negative experience of others has also previously been noted.22,34 Many aspects of using hearing aids can be difficult for older adults, including changing the battery, cleaning the ear mold, and inserting the aid into the ear.35 Cognitive and functional ability, poor benefit, discomfort with background noise, discomfort in noisy situations, and poor fit have been found to be related to the use of hearing aids.36,37 All of these factors may enter into the consideration of the poor experience of others and the perception that hearing aids are inconvenient.
Recent improvements in the technology related to hearing-assistive devices include digital processing and directional microphones, but it has not yet been determined that these improvements have led or will lead to greater use of the devices.38 The optimum timing for the introduction of aid(s) in relation to age and the course of hearing decline also needs to be established.39,40 The high number of individuals dissatisfied with the performance of their hearing aids may be partially related to when the aid was first fitted and the approach used for adapting to the new device. If a hearing aid is fitted too early in the progression of hearing loss, a benefit substantial enough to offset the time, effort, and cost involved in using the new hearing aid may not be seen. If the hearing aid is fitted too late, after the individual has already established compensatory mechanisms, additional difficulties involved in adapting to amplified sound may occur.
We did not observe any difference in the significant predictors for the 2 time periods (i.e., 0–5 years after hearing-loss detection vs 5–10 years after hearing-loss detection). In addition, results for the 0–5-year period showed that the rate of aid acquisition and the factors related to it did not significantly vary between participants whose hearing loss was detected at baseline (which includes those who had long-standing hearing loss) and those with newly detected hearing loss (i.e., hearing loss detected at the first follow-up). Therefore, there was no suggestion that time since hearing loss detection influenced the factors related to aid acquisition.
Our study was population-based in a relatively large population and was prospective in nature, with 10 years of follow-up. We used standard audiometric methods to measure hearing capacity, and we collected information on hearing aid usage, demographic characteristics, and perceived hearing ability at 5-year follow-up intervals. We were able to evaluate whether the length of time since the hearing loss was detected influenced which factors predicted hearing aid acquisition. However, for the participants whose hearing loss was identified at baseline, we did not have information regarding how long it had been since the hearing loss was first detected, and we could not assess the question of the timing of aid fitting in more detail.
Other limitations included having self-reported family history information for parents and siblings but not for spouses. Hearing aid experience among spouses may very well influence the likelihood of acquiring an aid. Finally, the observed rates of hearing aid acquisition will vary by the level of hearing loss chosen as the definition of hearing loss. Our definition of hearing loss (PTA0.5–4 kHz, better ear > 25 dB) may not be optimal and may not be the level at which audiologists recommend an aid. It may also be that information on hearing loss across frequencies is important in the fitting of an aid, although in our work, individual frequency data were not significant predictors of hearing aid acquisition.
Widespread acceptance of rehabilitive aids, particularly hearing aids, for the treatment of hearing loss has not been achieved and remains a challenge. In addition to technological advancements, work is needed to determine the most effective approaches for overcoming the personal and societal barriers affecting the acquisition and continued use of hearing aids.
Acknowledgments
This study was supported by the National Institute On Aging (award R37AG011099) and the National Eye Institute (award EY06594).
The authors thank the residents of Beaver Dam, Wisconsin, for their continued commitment to the study.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
Human Participant Protection
The Health Sciences institutional review board of the University of Wisconsin approved the study protocol. Participants provided written informed consent.
References
- 1.Dalton DS, Cruickshanks KJ, Klein BEK, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003;43(5):661–668 [DOI] [PubMed] [Google Scholar]
- 2.Carabellese C, Appollonio I, Rozzini R, et al. Sensory impairment and quality of life in a community elderly population. J Am Geriatr Soc. 1993;41(4):401–407 [DOI] [PubMed] [Google Scholar]
- 3.Reuben DB, Mui S, Damesyn M, et al. The prognostic value of sensory impairment in older persons. J Am Geriatr Soc. 1999;47(8):930–935 [DOI] [PubMed] [Google Scholar]
- 4.Pugh KC, Crandell CC. Hearing loss, hearing handicap, and functional health status between African American and Caucasian American seniors. J Am Acad Audiol. 2002;13(9):493–502 [PubMed] [Google Scholar]
- 5.Wallhagen MI, Strawbridge WJ, Shema SJ, et al. Comparative impact of hearing and vision impairment on subsequent functioning. J Am Geriatr Soc. 2001;49(8):1086–1092 [DOI] [PubMed] [Google Scholar]
- 6.Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force on the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol. 2007;18(2):151–183 [DOI] [PubMed] [Google Scholar]
- 7.Mulrow CD, Aguilar C, Endicott JE, et al. Quality-of-life changes and hearing impairment. Ann Intern Med. 1990;113(3):188–194 [DOI] [PubMed] [Google Scholar]
- 8.Mulrow CD, Tuley MR, Aguilar C. Sustained benefits of hearing aids. J Speech Hear Res. 1992;35(6):1402–1405 [DOI] [PubMed] [Google Scholar]
- 9.Kricos PB, Erdman S, Bratt GW, Williams DW. Psychosocial correlates of hearing aid adjustment. J Am Acad Audiol. 2007;18(4):304–322 [DOI] [PubMed] [Google Scholar]
- 10.Stark P, Hickson L. Outcomes of hearing aid fitting for older people with hearing impairment and their significant others. Int J Audiol. 2004;43:390–398 [DOI] [PubMed] [Google Scholar]
- 11.Yueh B, Souza PE, McDowell JA, et al. Randomized trial of amplification strategies. Arch Otolaryngol Head Neck Surg. 2001;127(10):1197–1204 [DOI] [PubMed] [Google Scholar]
- 12.Appollonio I, Carabellese C, Frattola L, Trabucchi M. Effects of sensory aids on the quality of life and mortality of elderly people: a multivariate analysis. Age Ageing. 1996;25(2):89–96 [DOI] [PubMed] [Google Scholar]
- 13.Popelka MM, Cruickshanks KC, Wiley TL, Tweed TS, Klein BEK, Klein R. Low prevalence of hearing aid use among older adults with hearing loss: the Epidemiology of Hearing Loss Study. J Am Geriatr Soc. 1998;46(9):1075–1078 [DOI] [PubMed] [Google Scholar]
- 14.Kochkin S. MarkeTrak III: higher hearing aid sales don't signal better market penetration. Hear J. 1992;45(7):47–54 [Google Scholar]
- 15.Kochkin S. MarkeTrak VII: hearing loss population tops 31 million people. Hear Rev. 2005;12(7):16–29 [Google Scholar]
- 16.Desai M, Pratt LA, Lentzner H, Robinson KN. Trends in vision and hearing among older Americans. Aging Trends. 2001;2:1–8 [DOI] [PubMed] [Google Scholar]
- 17.Palmer CV, Solodar HS, Hurley WR, Byrne DC, Williams KO. Self-perception of hearing ability as a strong predictor of hearing aid purchase. J Am Acad Audiol. 2009;20(6):341–347 [DOI] [PubMed] [Google Scholar]
- 18.van den Brink RHS, Wit HP, Kempen GI, van Heuvelen MJ. Attitude and help-seeking for hearing impairment. Br J Audiol. 1996;30(5):313–324 [DOI] [PubMed] [Google Scholar]
- 19.Duijvestijn JA, Anteunis LJ, Hoek CJ, van den Brink RH, Chenault MN, Manni JJ. Help-seeking behaviour of hearing-impaired persons aged > or = 55 years; effect of complaints, significant others and hearing aid image. Acta Otolaryngol. 2003;123(7):846–850 [DOI] [PubMed] [Google Scholar]
- 20.Mahoney CF, Stephens SD, Cadge BA. Who prompts patients to consult about hearing loss? Br J Audiol. 1996;30(3):153–158 [DOI] [PubMed] [Google Scholar]
- 21.National Council on Aging The consequences of untreated hearing loss in older persons. ORL Head Neck Nurs. 2000;18(1):12–16 [PubMed] [Google Scholar]
- 22.Kochkin S. MarkeTrak III: why 20 million in US don't use hearing aids for their hearing loss. Hear J. 1993;46(1):20–27 [Google Scholar]
- 23.Cruickshanks KJ, Wiley TL, Tweed TS, et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: the Epidemiology of Hearing Loss Study. Am J Epidemiol. 1998;148(9):879–886 [DOI] [PubMed] [Google Scholar]
- 24.Klein R, Klein BEK, Linton KLP, et al. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991;98(8):1310–1315 [DOI] [PubMed] [Google Scholar]
- 25.Klein R, Klein BEK, Lee KP. Changes in visual acuity in a population: the Beaver Dam Eye Study. Ophthalmology. 1996;103(8):1169–1178 [DOI] [PubMed] [Google Scholar]
- 26.American Speech-Language-Hearing Association Guidelines for manual pure-tone threshold audiometry. ASHA. 1978;20(4):297–301 [PubMed] [Google Scholar]
- 27.American National Standards Institute Specification for Audiometers (S3.6). New York, NY: American National Standards Institute; 1989 [Google Scholar]
- 28.American National Standards Institute Maximum Permissible Ambient Noise Levels for Audiometric Test Rooms (S3.1). New York, NY: American National Standards Institute; 1992 [Google Scholar]
- 29.Wilson RH, Zizz CA, Shanks JE, et al. Normative data in quiet, broadband noise, and competing message for Northwestern University auditory test no. 6 by a female speaker. J Speech Hear Disord. 1990;55(4):771–778 [DOI] [PubMed] [Google Scholar]
- 30.Wiley TL, Cruickshanks KJ, Nondahl DM, et al. Aging and word recognition in competing message. J Am Acad Audiol. 1998;9(3):191–198 [PubMed] [Google Scholar]
- 31.Ventry IM, Weinstein BE. Identification of elderly people with hearing problems. ASHA. 1983;25(7):37–42 [PubMed] [Google Scholar]
- 32.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198 [DOI] [PubMed] [Google Scholar]
- 33.Gates GA, Cooper JC, Kannel WB, Miller NJ. Hearing in the elderly: the Framingham cohort, 1983–1985. Part 1. Basic audiometric results. Ear Hear. 1990;11(4):247–256 [PubMed] [Google Scholar]
- 34.Gussekloo J, de Bont LE, von Faber M, et al. Auditory rehabilitation of older people from the general population—the Leiden 85-Plus Study. Br J Gen Pract. 2003;53(492):536–540 [PMC free article] [PubMed] [Google Scholar]
- 35.Stephens SD, Meredith R. Physical handling of hearing aids by the elderly. Acta Otolaryngol Suppl. 1990;476:281–285 [DOI] [PubMed] [Google Scholar]
- 36.Lupsakko TA, Kautiainen HJ, Sulkava R. The non-use of hearing aids in people aged 75 years and over in the city of Kuopio in Finland. Eur Arch Otorhinolaryngol. 2005;262(3):165–169 [DOI] [PubMed] [Google Scholar]
- 37.Kochkin S. MarkeTrak V: “why my hearing aids are in the drawer”: the consumers’ perspective. Hear J. 2000;53(2):34–41 [Google Scholar]
- 38.Edwards B. The future of hearing aid technology. Trends Amplif. 2007;11(1):31–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pichora-Fuller MK, Singh G. Effects of age on auditory and cognitive processing: implications for hearing aid fitting and audiologic rehabilitation. Trends Amplif. 2006;10(1):29–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brooks DN. The time course of adaptation to hearing aid use. Br J Audiol. 1996;30(1):55–62 [DOI] [PubMed] [Google Scholar]