Abstract
Childhood obesity is a public health concern with significant health and economic impacts. We conducted a prospective experimental study in 4 classrooms in central Texas to determine the effect of desks that encourage standing rather than sitting on caloric expenditure in children. Students were monitored with calorie expenditure–measuring arm-bands worn for 10 days in the fall and spring. The treatment group experienced significant increases in calorie expenditure over the control group, a finding that has implications for policy and practice.
A 2010 report released by the Trust for America's Health and the Robert Wood Johnson Foundation entitled F as in Fat: How Obesity Threatens America's Future, 2010 states that the percentage of overweight and obese children is at or above 30% in 30 states.1 The probability of obese children becoming obese adults is significantly higher than is the probability among their nonobese counterparts.2,3 Obese children who grow into obese adults also have more severe health risks than do individuals with adult-onset obesity, including potential for a shorter lifespan.4,5
School-based physical activity programs and environmental changes have proven helpful in increasing health-enhancing physical activities for children.6-9 However, these activities typically concentrate on small portions of a child's day and miss the opportunity to increase health-enhancing physical activities throughout the entire school day, particularly during instructional time. The pilot study described in this brief targeted childhood obesity by increasing passive calorie expenditure in the classroom. Classroom environments were modified to increase standing (rather than sitting) by replacing students’ and teachers’ traditional seated desks with standing height desks specifically manufactured for this study (Artco-Bell, Temple, TX); standing height stools were also provided to allow students to sit at their discretion. This concept biased the classroom environment toward standing, encouraging healthy movements, and increased energy expenditure.
METHODS
The intervention was pilot tested during the 2009 to 2010 school year in 4 first-grade classrooms in an ethnically diverse elementary school in central Texas; the treatment and control classrooms were randomly selected. All of the desks in the 2 treatment classrooms were converted to stand–sit workstations with stools, whereas the control classrooms remained unaltered for the entire school year. Students were told about the desks during the consent–assent process, and their teachers reinforced that they could stand or sit at their discretion. In addition to calorie expenditure, our study investigated children's standing activity after giving them no specific instruction that they must stand or sit for any portion of their day. By the 12th week of school after the treatment, students had acclimated to their desks; 70% of the students were not using stools at all, standing 100% of the time at their primary homeroom workstation, and the other 30% were standing, on average, approximately 75% of the time. Differences in energy expenditure for the most frequent users compared with the least frequent users of the standing position were not measured because the mean time standing for treatment classes was 91% of homeroom time.
Eighty students (20 each in 4 classrooms) were contacted for potential inclusion in the study. Parental consent and child assent were obtained at the beginning of the school year for 71 participants (58 completed the study by recording complete data for both fall and spring data collections—31 from the treatment group and 27 from the control group). Every student in the treatment classrooms received the stand–sit desk; consent was solely for participation in the data collection activities. Those that did not consent were children whose parents who did not attend parent night and were unable to be reached in the 2 weeks afterward.
Data collected on each student included gender; age; initial and final height, weight, and body mass index (weight in kg divided by height in m2); body fat percentage; and calorie expenditure measured by the BodyBugg armband (Apex Fitness, Westlake Village, CA) worn on the upper left arm during the course of 5 consecutive school days at 4 intervals during the school year. The BodyBugg armband device is self-calibrating; takes frequent measurements, which reduces wear time needed to collect data; reports actual wear time of the device; can distinguish between different activities and their intensities; and, unlike an accelerometer-only device, does not require movement to acquire data on energy expenditure. This type of armband has been used in studies on children and adults; early validation studies on children resulted in modifications of the algorithm in the software to improve accuracy and validity.10–17 The current algorithm, adjusted on the basis of findings of 2007 and 2008 studies, incorporates height, weight, gender, age, and handedness of the wearer to assess caloric expenditure when combined with measurement of heat flux, temperature, galvanic skin response, and a 3-axis accelerometer. The reported average error in measurement of caloric expenditure for a variety of activities with the current algorithm is 1.7%, with a high degree of repeatability.12
We explored the longitudinal structure of the data collected in this study by using multilevel statistical models.18 Time was included as a continuous variable measured in hours where 0 = baseline, 0.5 = 30 minutes, and 1 = 60 minutes. The lowest level of the data hierarchy (level 1) was the repeated measurements of calories burned per minute (yij) on each individual and the individuals themselves constituted the second level of the data hierarchy (level 2) as shown in the following equation:
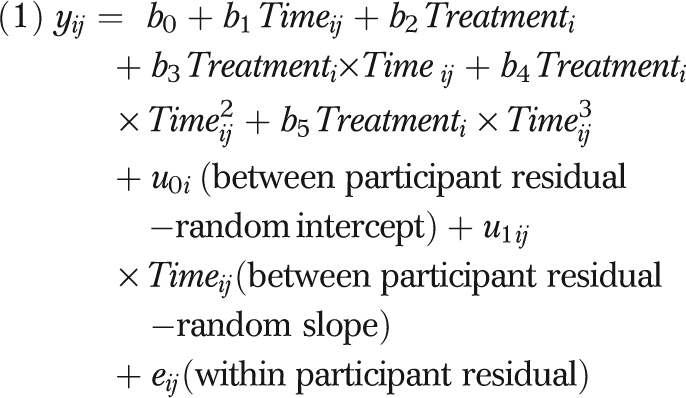 |
We accomplished model building by using a forward selection procedure in which powers of time were added 1 at a time to the base model including treatment group effects only. We then progressively added interaction terms between time and treatment effects and evaluated them with likelihood ratio tests.
RESULTS
Of the 13 students who did not complete the study, 4 left the study because of relocation in which the student was no longer attending the same school; these students did not differ from those who completed the study in any baseline measures. The other 9 students did not complete the study as a result of excessive absence and also did not differ from those who completed the study in any baseline measures.
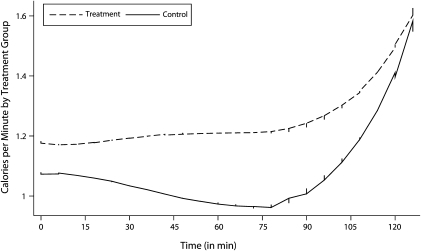
Figure 1 displays lowess curves of the raw data for the calories burned per minute over time (8:00 am–10:00 am) for the treated and control groups. We selected the analysis time period noted in Figure 1 out of the full school day because this was the time of day when both groups were in their classrooms at their primary workstation doing the same tasks.
FIGURE 1.
Lowess curves of the raw data for the calories burned per minute over time (8:00 am–10:00 am) among central Texas elementary school students using stand-biased desks versus control group: 2009–2010.
The results of the model presented in Table 1 indicate that the treatment group (n = 31) burned an average of 0.18 kilocalories per minute more than did the control group (n = 27; P = .022). Students in the treatment group burned 17% more calories than did those in the control group (treatment: mean initial weight = 25.2 kg; control: mean initial weight = 24.1 kg). Within the subset of participants over the 85th percentile in weight for their age and gender (treatment: mean initial weight = 30.3 kg [n = 12]; control: mean initial weight = 28.2 kg [n = 9]),19 children in the treatment group experienced a 32% increase in calorie expenditure compared with those in the control group (1.56 kcal/min vs 1.18 kcal/min). (The mean weights are given to show how similar the controls were to the treatments in the 2 sets of classrooms, but not to indicate results of caloric expenditure.)
TABLE 1.
Calories Burned per Minute Over Time Among Central Texas Elementary School Students Using Stand-Biased Desks Versus Control Group: 2009–2010
| Model Parameter | b (SE) | Z | P | 95% CI |
| Fixed effects | ||||
| b0 (intercept) | −338.815 (19.538) | −17.341 | <.001 | −377.110, −300.520 |
| b1 (treatment) | 0.182 (0.080) | 2.287 | .022 | 0.026, 0.338 |
| b2 (treatment × time) | 109.467 (6.161) | 17.769 | <.001 | 97.393, 121.542 |
| b3 (treatment × time2) | −11.729 (0.646) | −18.156 | <.001 | −12.995, −10.463 |
| b4 (treatment × time3) | 0.418 (0.023) | 18.552 | <.001 | 0.374, 0.462 |
| Random effects | ||||
| var(u1ij × timeij) | 0.001 (0.000) | 2.167 | .03 | 0.000, 0.001 |
| var(u0i) | 0.053 (0.022) | 2.359 | .018 | 0.023, 0.121 |
| var(eij) | 0.120 (0.002) | 54.730 | <.001 | 0.116, 0.124 |
Note. CI = confidence interval. The time period during which data were collected was 8:00 AM to 10:00 AM.
DISCUSSION
Although our results are limited because of sample size, they are promising and provide a basis for further research on cost-effectiveness of stand–sit desks in preventing childhood obesity. The implementation cost of this intervention is relatively low; the stand–sit desk and stool units cost approximately 20% more than did the standard ones. Other than the initial investment, schools incur no ongoing costs and give up no instructional time. Further, interviews with teachers and parents of students in the treatment group indicated a positive effect on child behavior and classroom performance, which is supported by the literature.20 The majority of parents (70%) whose children were in the treatment classrooms felt that standing in the classroom positively affected their child's classroom behavior. A teacher in one of the treatment classrooms stated:
When standing, the students were more focused, and I could keep their attention for longer… . I have one student with severe ADHD [attention-deficit/hyperactivity disorder], and this really helped him academically.
Additional research will also explore these effects, aiming to document academic incentives for schools to use stand–sit desks.
Our study contributes unique information to the knowledge base in that we used measures of caloric expenditure; other studies have measured only movement using an accelerometer.21–23 Recent research into sedentary behaviors has indicated health outcomes beyond caloric expenditure for reducing seated time, including improved metabolic profiles, improvements in high-density lipoprotein production, lipoprotein lipase activity, and blood glucose control.24–27 In addition to these findings, Hamilton et al.28,29 reported that standing muscle activity causes isometric contraction of postural muscles, which produces electromyographic and skeletal muscle lipoprotein lipase changes resulting in additional biomarkers for health benefits. A larger longitudinal study is warranted that should examine students’ in-school and out-of-school activity, as well as caloric consumption to ascertain whether the students compensate for the extra calories burned by altering other behaviors. If the stand–sit desks are found to have similar effects on a larger sample, this finding would have significant policy implications for schools, districts, states, and the country and could force us to rethink traditional classroom design.
Acknowledgments
The authors wish to thank and acknowledge the funders that made this study possible: the United Way of the Brazos Valley, the Texas A&M School of Rural Public Health, and Artco-Bell. This study was also made possible, in part, by the Prevention Research Centers Program at the Centers for Disease Control and Prevention through cooperative agreement U48DP000045.
Note. The conclusions of this article are those of the authors and do not represent the official position of the Centers for Disease Control and Prevention.
Human Participant Protection
The study was approved by the institutional review board at Texas A&M University and the Research Review Board of the College Station Independent School District.
References
- 1.Levi J, Vinter S, St Laurent R, Segal LM. F as in Fat: How Obesity Threatens America's Future, 2010. Washington, DC: Trust for America's Health; 2010 [Google Scholar]
- 2.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22(2):167–177 [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873 [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718 [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein E, Brown D, Wrage L, Allaire B, Hoerger T. Individual and aggregate years-of-life-lost associated with overweight and obesity. Obesity (Silver Spring). 2010;18(2):333–339 [DOI] [PubMed] [Google Scholar]
- 6.Simons-Morton BG, Parcel GS, Baranowski T, Forthofer R, O'Hara NM. Promoting physical activity and healthful diet among children: results of a school-based intervention study. Am J Public Health. 1991;81(8):986–991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gortmaker SL, Cheung LW, Peterson KE, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children. Arch Pediatr Adolesc Med. 1999;153(9):975–983 [DOI] [PubMed] [Google Scholar]
- 8.Strong WB, Malina RM, Blimkie CJR, et al. Evidence-based physical activity for school-age youth. J Pediatr. 2005;146(6):732–737 [DOI] [PubMed] [Google Scholar]
- 9.Dobbins M, DeCorby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6-18. Cochrane Database Syst Rev. 2009;(Issue 3):CD007651. [DOI] [PubMed] [Google Scholar]
- 10.Arvidsson D, Slinde F, Hulthen L. Free-living energy expenditure in children using multi-sensor activity monitors. Clin Nutr. 2009;28(3):305–312 [DOI] [PubMed] [Google Scholar]
- 11.Calabro MA, Welk GJ, Carriquiry AL, Nusser SM, Beyler NK, Mathews CE. Validation of a computerized 24-hour physical activity recall (24PAR) instrument with pattern-recognition activity monitors. J Phys Act Health. 2009;6(2):211–220 [DOI] [PubMed] [Google Scholar]
- 12.Calabro MA, Welk GJ, Eisenmann JC. Validation of the SenseWear Pro Armband algorithms in children. Med Sci Sports Exerc. 2009;41(9):1714–1720 [DOI] [PubMed] [Google Scholar]
- 13.Dorminy CA, Choi L, Akohoue SA, Chen KY, Buchowski MS. Validity of a multisensor armband in estimating 24-h energy expenditure in children. Med Sci Sports Exerc. 2008;40(4):699–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andreacci JL, Dixon CB, Dube JJ, McConnell TR. Validation of SenseWear Pro2 Armband to assess energy expenditure during treadmill exercise in children 7-10 years of age. J Exerc Physiol Online. 2007;10(4):35–42 [Google Scholar]
- 15.Arvidsson D, Slinde F, Larsson S, Hulthen L. Energy cost of physical activities in children: validation of SenseWear Armband. Med Sci Sports Exerc. 2007;39(11):2076–2084 [DOI] [PubMed] [Google Scholar]
- 16.Welk GJ, McClain JJ, Eisenmann JC, Wickel EE. Field validation of the MTI Actigraph and BodyMedia armband monitor using the IDEEA monitor. Obesity (Silver Spring). 2007;15(4):918–928 [DOI] [PubMed] [Google Scholar]
- 17.Fruin ML, Rankin JW. Validity of a multi-sensor armband in estimating rest and exercise energy expenditure. Med Sci Sports Exerc. 2004;36(6):1063–1069 [DOI] [PubMed] [Google Scholar]
- 18.Goldstein H. Multilevel Statistical Models. New York, NY: Edward Arnold Publishers; 2003 [Google Scholar]
- 19.Centers for Disease Control and Prevention About BMI for Children and Teens. Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Accessed July 7, 2010
- 20.Centers for Disease Control and Prevention The Association Between School-Based Physical Activity, Including Physical Education, and Academic Performance. Atlanta, GA: US Dept of Health and Human Services; 2010 [Google Scholar]
- 21.Lanningham-Foster L, Foster RC, McCrady SK, et al. Changing the school environment to increase physical activity in children. Obesity (Silver Spring). 2008;16(8):1849–1853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saulny S. Students stand when called upon, and when not. New York Times. February 24, 2009; sect A:1 [Google Scholar]
- 23.Benjamin M, Nellis R. INL teams with Mayo Clinic, local school for student workstation study. INL News Release. February 18, 2010. Available at: http://inlportal.inl.gov/p9ortal/server.pt?open=514&objID=1555&mode=2&featurestory=DA_537963. Accessed March 4, 2010 [Google Scholar]
- 24.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–666 [DOI] [PubMed] [Google Scholar]
- 26.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–1389 [DOI] [PubMed] [Google Scholar]
- 27.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003; 551(Pt 2):673–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardiovasc Risk Rep. 2008;2(4):292–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655–2667 [DOI] [PubMed] [Google Scholar]