Abstract
Objectives. We investigated the association between housing insecurity and the health of very young children.
Methods. Between 1998 and 2007, we interviewed 22 069 low-income caregivers with children younger than 3 years who were seen in 7 US urban medical centers. We assessed food insecurity, child health status, developmental risk, weight, and housing insecurity for each child's household. Our indicators for housing insecurity were crowding (> 2 people/bedroom or > 1 family/residence) and multiple moves (≥ 2 moves within the previous year).
Results. After adjusting for covariates, crowding was associated with household food insecurity compared with the securely housed (adjusted odds ratio [AOR] = 1.30; 95% confidence interval [CI] = 1.18, 1.43), as were multiple moves (AOR = 1.91; 95% CI = 1.59, 2.28). Crowding was also associated with child food insecurity (AOR = 1.47; 95% CI = 1.34, 1.63), and so were multiple moves (AOR = 2.56; 95% CI = 2.13, 3.08). Multiple moves were associated with fair or poor child health (AOR = 1.48; 95% CI = 1.25, 1.76), developmental risk (AOR 1.71; 95% CI = 1.33, 2.21), and lower weight-for-age z scores (–0.082 vs −0.013; P = .02).
Conclusions. Housing insecurity is associated with poor health, lower weight, and developmental risk among young children. Policies that decrease housing insecurity can promote the health of young children and should be a priority.
In the United States, as in other countries, housing is considered a strong social determinant of health.1 Poor housing conditions have been linked to multiple negative health outcomes in both children and adults. The Department of Health and Human Services has defined housing insecurity as high housing costs in proportion to income, poor housing quality, unstable neighborhoods, overcrowding, or homelessness.2 Crowding in the home and multiple moves from home to home have clear negative associations for children. Crowding is negatively associated with mental health status,3 ability to cope with stress,4 child and parent interaction,5 social relationships,3 and sleep.3 It also increases the risk for childhood injuries,6 elevated blood pressure,5 respiratory conditions,7 and exposure to infectious disease.7 Adults8 and children9 living in crowded households are less likely to access health care services than are those in noncrowded households, and families with multiple moves are less likely to establish a medical home and seek out preventive health services for their children than are securely housed families.10
In older children and adolescents, a history of multiple moves has been associated with mental health concerns,11 substance abuse,12 increased behavior problems,13 poor school performance,13,14 and increased risk of teen pregnancy.15 Multiple moves in childhood can have lifelong impact, as evidenced by higher rates of adverse childhood events,16 lower global health ratings in adulthood,17 and increased mental health and behavior concerns lasting through adolescence and into adulthood.16 Grade-school children with more than 2 school moves are 2.5 times more likely to repeat a grade,18 and adolescents who experience school moves are 50% more likely not to graduate from high school.19
Access to affordable housing is likely to reduce the chances that a family will live in crowded conditions or make multiple moves within a short period of time. Since the Housing Act of 1937 was passed,20 30% of monthly adjusted income has been used as the threshold for affordable housing costs. But affordability by this definition is becoming increasingly less common. In 2008, half of renter households paid more than 30% of their income in rent, and nearly a quarter paid more than 50%.21 Increases in unemployment and the poverty rate since 2008 have likely increased the number of families living in housing that they are hard pressed to afford. Although poverty is higher among young children than among any other age group,22 little is known about the effects of housing insecurity on very young children who are considered housed, albeit precariously. We examined the health, developmental, and anthropometric correlates of housing insecurity among children younger than 3 years, using crowding and multiple moves as indicators.
METHODS
Between June 1998 and December 2007, researchers with the ongoing Children's HealthWatch study approached 36 618 adult caregivers of children younger than 3 years at Children's HealthWatch sites in 7 central-city medical centers serving diverse, low-income populations in Baltimore, MD; Boston, MA; Little Rock, AR; Los Angeles, CA; Minneapolis, MN; Philadelphia, PA; and Washington, DC. Institutional review board approval was obtained at each site prior to data collection and has been renewed annually since then.
The study design was cross-sectional. At each study site, trained interviewers surveyed caregivers accompanying children younger than 3 years who were seeking care at acute or primary care clinics or hospital emergency departments during peak patient flow times. Interviewers did not approach caregivers of critically ill or injured children. Potential respondents were excluded if they did not speak English or Spanish (or, in Minneapolis only, Somali), were not knowledgeable about the child's household, had been interviewed previously, lived out of state, or did not consent to participate. The caregivers were approached in private settings.
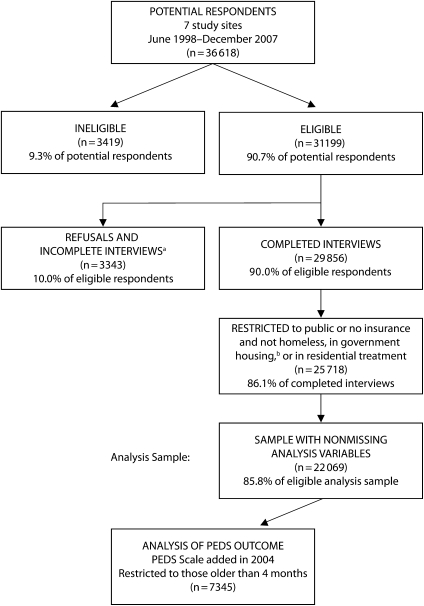
Of the 36 618 caregivers who were approached, 3419 (9.3%) were ineligible, and 3343 (10.9%) refused to participate or were not able to complete the interview (Figure 1). To ensure that sample participants had relatively similar economic backgrounds, participants with private insurance were excluded (n = 3358). Because our study interest concerned housing insecurity distinct from homelessness, we also excluded families who were homeless or living in shelters, residential treatment centers, or military facilities (n = 780) (Figure 1). Also eliminated were 3649 (14.2%) interviews that had missing data. This process yielded a final analysis sample of 22 069 caregiver/child dyads. Those with complete data were similar to those with incomplete data in terms of child's gender, birth weight, household employment, and number of children in the household. Caregivers with incomplete data were more likely to be Hispanic, foreign born, interviewed in Minneapolis, married, older, have less education, have breastfed their child, and not report depressive symptoms.
FIGURE 1.
Description of analytic sample selection: 7 US cities, 1998–2007.
Note. PEDS = Parents’ Evaluation of Developmental Status survey.
aRespondents who did not complete interview process.
bi.e., military housing.
Survey, Anthropometric, and Housing Insecurity Measures
From study inception, the survey covered multiple domains, including demographics, housing, reports of child health, and the United States Food Security Scale.23–26 Participants self-identified their race/ethnicity using definitions based on US Census Bureau definitions.27 We asked race/ethnicity questions to characterize the sample and to demonstrate the diversity of this population. Respondents characterized their child's health as excellent, good, fair, or poor using a question from the 1988–1994 National Health and Nutrition Examination Survey,28–30 which has been validated against medical chart review. Poor child health was defined as caregivers ranking children as being in either fair or poor health.31
Household food insecurity and child food insecurity were derived from the Food Security Scale in accordance with established procedures.23,25 Households were classified as food insecure if they scored at a level indicating they could not afford enough nutritious food for active, healthy lives, and if this condition resulted from constrained resources.23–25 Children were classified as food insecure if their caregivers reported that they met the criteria for either child hunger (skipping or reducing the size of child meals) or poor diet quality (relying on only a few foods or being unable to provide a balanced diet for children).24
In 2000 we expanded our survey to assess caregivers’ depressive symptoms, measured by a 3-item screen with a sensitivity of 100%, specificity of 88%, and positive predictive value of 66%, compared with the 8-item Rand screening instrument for depressive symptoms.32
We gave the Parents’ Evaluation of Developmental Status (PEDS) survey to a subset of 7345 caregivers with children older than 4 months from 2004 through 2007. Caregivers reported concerns about the child's development in 8 areas: expressive language, receptive language, fine motor skills, gross motor skills, behavior, social-emotional skills, self-help, and school. In addition, we asked caregivers 2 open-ended questions about concerns in the global/cognitive area and additional concerns. Other investigators have shown that children whose caregivers express 1 or more concerns on the PEDS are considered to be at developmental risk33–35 and experience from 8 to 20 times the risk of developmental and behavioral problems compared with children whose parents do not express concerns on the PEDS.36
Project staff or clinical staff used standard techniques to collect children's weight and length/height. When clinical staff collected these data, project staff obtained the data later via medical record reviews conducted on the same day as the interview. Anthropometric status was derived from the Centers for Disease Control and Prevention/National Center for Health Statistics 2000 age-gender standardized growth charts.37 We also calculated weight-for-age z scores.38
We divided the sample into 3 mutually exclusive groups according to their housing insecurity status. Families with no more than 1 move in the previous year and no indication of crowding were the referent securely housed group. We defined the 2 insecurely housed groups on the basis of crowding and multiple moves in the previous year. Using the US Department of Housing and Urban Development definition as a guideline,39 we defined crowding as having more than 2 people per bedroom or as temporarily living with other people because of economic difficulties (doubling up). Families that had moved 2 or more times in the previous year, with or without crowding, were classified as households with multiple moves.
Outcome variables included household food insecurity, child food insecurity, caregiver report of child's health status, developmental risk, and weight-for-age z scores. Weight-for-age z scores were expressed as a continuous variable. All other outcome variables were expressed as 2-level categorical variables.
Analysis
We developed separate multivariate logistic regression models for each of the dichotomous outcome variables, including a secondary analysis to examine whether adding maternal depressive symptoms might alter associations with housing insecurity (we assessed “maternal” depression for any female primary caregiver). We used general linear models for multivariate analysis of variance for continuous outcomes. Covariates included in each model were selected on theoretical grounds and on the basis of whether there was evidence of bivariate association with both the outcome of interest and with housing insecurity. To minimize the potential for collinearity, we calculated the correlation between pairs of independent variables, and we verified that no pair of variables included in the same regression model was highly correlated (i.e., r > 0.40). To determine how housing insecurity was related to child health variables, we used SAS 9.1 (SAS Institute, Cary, NC) to conduct multivariate analyses, using securely housed families as the referent category. All models were adjusted for city, maternal race/ethnicity, maternal place of birth (United States vs other), marital status, maternal education, mean number of children in the home, whether adults in the household were employed, mean child's age, whether the child was breastfed, and child's birth weight less than 2500 g.
RESULTS
Housing insecurity affected 46% of the study sample, with 41% of households experiencing crowding, and 5% of households experiencing multiple moves. As indicated in Table 1, housing insecurity was significantly associated with research site and more children in the home. Maternal older age, minority race/ethnicity, foreign place of birth, single marital status, lower education, depressive symptoms, and breastfeeding were also significantly associated with housing insecurity. Older child age was significantly associated with multiple moves.
TABLE 1.
Sample Characteristics, by Housing Group: Children Younger Than 3 Years, 7 US Cities, 1998–2007
| Housing Groups |
||||
| Sample Characteristics | Secure Housing | Crowding | Multiple Moves | P |
| Housing group totals | 11 904 (54) | 9113 (41) | 1052 (5) | |
| Study site, no. (%) | < .001 | |||
| Baltimore, MD | 1896 (16) | 992 (11) | 90 (8) | |
| Boston, MA | 3556 (30) | 1982 (22) | 246 (24) | |
| Little Rock, AR | 2695 (23) | 1120 (12) | 282 (27) | |
| Los Angeles, CA | 540 (4) | 931 (10) | 55 (5) | |
| Minneapolis, MN | 2034 (17) | 2982 (33) | 266 (25) | |
| Philadelphia, PA | 1047 (9) | 643 (7) | 101 (10) | |
| Washington, DC | 136 (1) | 463 (5) | 12 (1) | |
| Child characteristics | ||||
| Girl, no. (%) | 5597 (47) | 4263 (47) | 463 (44) | .17 |
| Age, mo, mean (SD) | 12.8 (9.9) | 10.6 (9.4) | 16.3 (8.9) | < .001 |
| Breastfed, no. (%) | 5848 (49) | 5323 (58) | 540 (51) | < .001 |
| Birth weight < 2500 g, no. (%) | 1622 (14) | 1189 (13) | 163 (15) | .03 |
| Caregiver race/ethnicity, no. (%) | < .001 | |||
| Asian | 139 (1) | 158 (2) | 8 (1) | |
| Black | 7281 (61) | 4093 (45) | 482 (46) | |
| Hispanic | 2461 (21) | 3871 (42) | 310 (29) | |
| Native American | 93 (1) | 95 (1) | 20 (2) | |
| White | 1930 (16) | 896 (10) | 232 (22) | |
| Caregiver US born, no. (%) | 8821 (74) | 4726 (52) | 783 (74) | < .001 |
| Caregiver single marital status, no. (%) | 8031 (67) | 5452 (60) | 747 (71) | < .001 |
| Caregiver education, no. (%) | < .001 | |||
| Some school | 3386 (29) | 4110 (45) | 422 (40) | |
| High school diploma/GED | 5035 (42) | 3346 (37) | 389 (37) | |
| Post–high school | 3483 (29) | 1657 (18) | 241 (23) | |
| Caregiver age, y, mean (SD) | 26.4 (6.7) | 25.5 (6.2) | 25.5 (6.8) | < .001 |
| No. of children in home, mean (SD) | 2 (1.2) | 3(1.6) | 2 (1.5) | < .001 |
| ≥1 household member employed, no. (%) | 9280 (78) | 7578 (83) | 772 (73) | < .001 |
| Maternal depressive symptoms,a no. (%) | 2140 (22) | 1858 (27) | 349 (41) | < .001 |
Note. GED = general equivalency diploma. Caregivers were 93% mothers, 5% fathers, and 2% other.
Asked only of female caregivers.
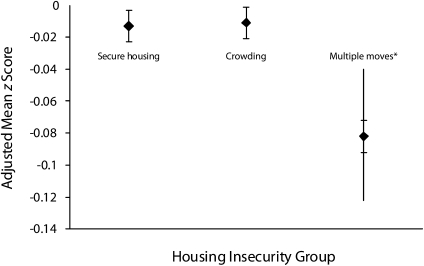
Household food insecurity (HFI) was found in 9% of families with secure housing, 12% of families with crowding, and 16% of families with multiple moves (P < .001). Child food insecurity (CFI) was found in 7% of families with secure housing, 17% of families with crowding, and 19% of families with multiple moves (P < .001). Multivariate analysis showed that, compared with the referent of secure housing, crowding was significantly associated with HFI (adjusted odds ratio [AOR] = 1.30; 95% confidence interval [CI] = 1.18, 1.43; P < .001) and with CFI (AOR = 1.47; 95% CI = 1.34, 1.63; P < .001) (Table 2). Multiple moves were also significantly associated with HFI (AOR = 1.91; 95% CI = 1.59, 2.28; P < .001) and CFI (AOR = 2.56; 95% CI = 2.13, 3.08; P < .001), with higher AORs than crowding and nonoverlapping confidence intervals. In addition, multiple moves were significantly associated with caregivers reporting their child's health as fair or poor (18% vs 11% of the securely housed, AOR = 1.48; 95% CI = 1.25, 1.76; P < .001) and reporting developmental risk as measured by the PEDS (22% vs 14% of the securely housed, AOR = 1.71; 95% CI = 1.33, 2.21; P < .001). Children in the multiple-moves group had significantly lower weight-for-age z scores than the secure-housing group (–0.082 vs −0.013; P = .02) (Figure 2).
TABLE 2.
Variables Associated With Insecure Housing, by Housing Group: Children Younger Than 3 Years, 7 US Cities, 1998–2007
| Secure Housing (Ref) |
Crowding |
Multiple Moves |
||||||
| Variables | Unadjusted No. (%) | AOR (95% CI) | Unadjusted No. (%) | AOR (95% CI) | P | Unadjusted No. (%) | AOR (95% CI) | P |
| Household food insecurity (n = 22 069) | 1052 (9) | 1.0 | 1060 (12) | 1.30 (1.18, 1.43) | < .001 | 166 (16) | 1.91 (1.59, 2.28) | < .001 |
| Child food insecurity (n = 22 069) | 872 (7) | 1.0 | 1513 (17) | 1.47 (1.34, 1.63) | < .001 | 204 (19) | 2.56 (2.13, 3.08) | < .001 |
| Caregiver report of fair/poor child health (n = 22 069) | 1313 (11) | 1.0 | 1193 (13) | 1.07 (0.98, 1.18) | .14 | 192 (18) | 1.48 (1.25, 1.76) | < .001 |
| Caregiver report of child developmental risk (after 2004, n = 7345) | 621 (14) | 1.0 | 355 (14) | 1.06 (0.91, 1.23) | .49 | 96 (22) | 1.71 (1.33, 2.21) | < .001 |
Note. AOR = adjusted odds ratio; CI = confidence interval. Analyses are adjusted for site, race/ethnicity, US-born mother, marital status, maternal age, education, mean child's age, mean number of children in the home, household employment, breastfeeding, and low birth weight. Secure housing is the referent group.
FIGURE 2.
Adjusted mean weight-for-age z scores by housing group: children younger than 3 years, 7 US cities, 1998–2007.
Note. Least squares mean weight-for-age z scores by levels of housing insecurity were adjusted for site, race/ethnicity, US-born mother versus immigrant mother, maternal age, marital status, caregiver education, mean child's age, mean number of children in the home, household employment, breastfeeding, and low birth weight.* P = .02.
When we added maternal depressive symptoms to the models as a covariate, the associations of housing insecurity with fair/poor child health and developmental risk were somewhat attenuated but remained significant. The AOR between multiple moves and fair/poor child health diminished only slightly, from 1.48 (95% CI = 1.25, 1.76) to 1.40 (95% CI = 1.16, 1.70; P < .001), whereas the AOR between multiple moves and developmental risk diminished from 1.71 (95% CI = 1.33, 2.21) to 1.53 (95% CI = 1.18, 1.99; P = .001), remaining significant but showing partial attenuation. Maternal depressive symptoms were significantly associated with HFI, CFI, fair/poor child health, and developmental risk (P < .001) but not with weight-for-age z score. CFI was also tested as a mediator of the association between housing insecurity and child weight for age, but results did not differ from our primary analysis.
DISCUSSION
Homeless children are recognized as being vulnerable to multiple health risks, but there are millions of less visible children whose health, development, and growth may be compromised by living in insecure housing. Nearly half of our sample (46%) had experienced housing insecurity within the past year. We found housing insecurity to be associated with measures of poor health, growth, and development in young children, which is consistent with findings of research on samples of adults and older children. Housing insecurity is also an important marker for food insecurity. Multiple moves had a stronger relation with food insecurity and fair/poor child health than crowding, suggesting that multiple moves are a more severe form of housing insecurity. Whereas crowding may be used as a coping strategy to avoid outright homelessness, housing transiency as reflected by multiple moves may indicate a lack of social ties40 to assist families during household crises.
We found that, compared with the rest of our sample, very young children in households with multiple moves had worse caregiver-reported health status, increased developmental risk, and average weight for age that was lower than expected. Although the magnitude of the weight-for-age z-score differences between the groups was not large, the negative growth differences in this group of very young children are cause for concern. Similar to multiple moves, crowding was associated with HFI and CFI, but to a lesser degree. Children living in households with both housing insecurity and food insecurity experience dual threats because food insecurity has been independently associated with children's risk for hospitalization,41 poor health,41 developmental delays,42 anemia,43,44 and the mother's risk for depressive symptoms.45,46
The potential life-course effects of housing insecurity during early childhood are important. Shonkoff et al. made a case that stress or disruption during childhood is a precursor to chronic disease in adulthood.47 The relationship between housing insecurity and outcomes of poor child health, diminished weight, increased developmental risk, and greater likelihood of food insecurity suggest that policies promoting stable housing may have latent positive long-term health impacts.
Young children may be particularly vulnerable to the lack of a stable environment or to the stress of their families going through periods of housing insecurity. Social disorganization theory suggests that environmental factors such as housing insecurity influence parenting and child behavior.48 Housing insecurity impedes the development of role models, informal neighborhood social supports, connections to resources such as child care, family participation in the social environment, and establishment of a medical home for consistent health care. All of these social factors are important to families with young children. Other social models discuss a competition process whereby neighbors compete for scarce community resources and services, impairing parental mental and physical health and influencing parental behaviors in ways that negatively affect the health of their children. Neighborhoods where families know and trust each other and community-level interventions that ensure adequate, safe, and affordable housing can positively affect the physical and mental health of parents and children.49
Programs offering housing subsidies or energy assistance have been shown to protect against child health concerns, including hospitalizations50 and poor growth,51 as well as anemia.52 Mills et al. found that families receiving housing subsidies moved less frequently and were less crowded than families that did not receive a subsidy.53 Despite the benefits of subsidized housing, only 1 out of 4 eligible households receives housing assistance.54 Meyers et al. found that children younger than 3 years who lived in food-insecure households that were eligible for housing subsidies but did not receive them were more than twice as likely to have growth delays as measured by weight for age compared with those receiving housing subsidies.51 Frank et al. showed that children in families receiving energy assistance had lower odds of acute hospitalizations and diminished risk of having weight-for-age z scores that were more than 2 standard deviations below the mean.50
Recent increases in unemployment, housing foreclosures (including those related to subprime lending), and the continued demand for low-income housing all contribute to an environment of housing insecurity.21 Although all socioeconomic groups are affected by housing insecurity, low-income households are particularly at risk because of their already constrained financial resources and lack of reserve funds. Low-income families often pay a larger proportion of their income for housing than do higher-income households, which decreases the resources available for other necessities such as food, transportation, heat, and medical care.21
There are several methodological limitations that should be considered when interpreting these data. First, because of the cross-sectional design of this study, it is not possible to determine cause-and-effect relationships on the basis of our findings. Furthermore, although we controlled for important confounding variables, other unmeasured confounders may exist. We further acknowledge that, despite our use of previously independently validated questions whenever possible, respondents may have over- or underreported negative child outcomes. Because this study assesses families from low-income backgrounds in emergency rooms and hospital-based clinics, their children are already at elevated risk for developmental and health concerns and may not be representative of all low-income children. However, we excluded urgently ill or injured children, so some of the highest-risk children may not have been included in this study.
In addition, families that were excluded from the analyses because of incomplete data represent a high-risk segment of the study population, judged on the basis of demographic variables of caregiver education, maternal race/ethnicity, and maternal country of birth. Therefore, it is possible that excluding these families from the analyses contributes to underestimating the impact of housing insecurity. Finally, our measurement of housing insecurity does not incorporate measures of housing safety or quality of neighborhood conditions; nor does it consider affordability.
Nevertheless, the association between housing insecurity and measures of children's health and development provide evidence of the vulnerability of children who have insecure housing but who are not homeless. Low-income children often bear the burden of multiple risk factors for adverse outcomes, some of which (such as housing insecurity) can be addressed through public policies. Governmental action and community investment in expanding the supply of affordable housing, increasing funding for housing assistance programs, and stabilizing families in uncrowded housing they can afford can alleviate housing insecurity. Protecting families with young children from being economically forced into crowded conditions and frequent moves should be a policy priority.
Acknowledgments
This research was supported by the Annie E. Casey Foundation, the Anthony Spinazzola Foundation, the Hartford Foundation for Public Giving, the Claneil Foundation, the Eos Foundation, Feeding America, the Gryphon Fund, the Krupp Family Foundation, the Larson Family Foundation, the Paul and Phyllis Fireman Charitable Foundation, the Pew Charitable Trusts, the W. K. Kellogg Foundation, Susan Schiro and Peter Manus, and anonymous donors.
We are grateful to the families who participated in this study and to our multilingual interviewers at all sites. We also thank Zhaoyan Yang, MA, Anna Quigg, MA, Katherine Joyce, MPH, Kathleen W. Barrett, MSE, Gabriela Santamaria, MA, Tu Quan, MPH, Linda Carson, Jennifer Breaux, MPH, and Ashley Schiffmiller. Special thanks also go to Elizabeth L. March, MCP, and Karin Rhodes, MD, for their careful review of and comments on drafts of the article.
Human Participant Protection
The institutional review boards of Boston University Medical Center, Hennepin County Medical Center, Drexel University College of Medicine, University of Arkansas for Medical Sciences, and University of Maryland School of Medicine approved the study protocol at the beginning of the study. We obtained renewal of the protocol approval from each institutional review board annually.
References
- 1.Satcher D. Include a social determinants of health approach to reduce health inequities. Public Health Rep. 2010;125(suppl 4):6–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson A, Meckstroth A. Ancillary services to support welfare to work. Washington, DC: US Dept of Health and Human Services; June 22, 1998:20–23. Available at: http://aspe.hhs.gov/hsp/isp/ancillary/front.htm. Accessed April 28, 2010 [Google Scholar]
- 3.Gove WR, Hughes M, Galle OR. Overcrowding in the home: an empirical investigation of its possible pathological consequences. Am Sociol Rev. 1979;44(1):59–80 [PubMed] [Google Scholar]
- 4.Lepore SJ, Evans GW, Palsane MN. Social hassles and psychological health in the context of chronic crowding. J Health Soc Behav. 1991;32(4):357–367 [PubMed] [Google Scholar]
- 5.Evans GW, Lepore SJ, Shejwal BR, Palsane MN. Chronic residential crowding and children's well-being: an ecological perspective. Child Dev. 1998;69(6):1514–1523 [PubMed] [Google Scholar]
- 6.Delgado J, Ramirez-Cardich ME, Gilman RH, et al. Risk factors of burns in children: crowding, poverty, and poor maternal education. Inj Prev. 2002;8(1):38–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cardoso MR, de Góes Siqueira LF, Alves FM, D'Angelo LA. Crowding: risk factor or protective factor for lower respiratory disease in young children? BMC Public Health. 2004;4:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma CT, Gee L, Kushel MB. Associations between housing instability and food insecurity with health care access in low-income children. Ambul Pediatr. 2008;8(1):50–57 [DOI] [PubMed] [Google Scholar]
- 10.Fowler MG, Simpson GGA, Schoendorf KC. Families on the move and children's health care. Pediatrics. 1993;91(5):934–940 [PubMed] [Google Scholar]
- 11.Gilman SE, Kawachi I, Fitzmaurice GM, Buka L. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychol Med. 2003;33(8):1341–1355 [DOI] [PubMed] [Google Scholar]
- 12.DeWit DJ. Frequent childhood geographic relocation: its impact on drug use initiation and the development of alcohol and other drug-related problems among adolescents and young adults. Addict Behav. 1998;23(5):623–634 [DOI] [PubMed] [Google Scholar]
- 13.Simpson GA, Fowler MG. Geographic mobility and children's emotional/behavioral adjustment and school functioning. Pediatrics. 1994;93(2):303–309 [PubMed] [Google Scholar]
- 14.Wood D, Halfon N, Scarlata D, Newacheck P, Nessim S. Impact of family relocation on children's growth, development, school function and behavior. JAMA. 1993;270(11):1334–1338 [PubMed] [Google Scholar]
- 15.Jelleyman T, Spencer N. Residential mobility in childhood: a systematic review. J Epidemiol Community Health. 2008;62(7):584–592 [DOI] [PubMed] [Google Scholar]
- 16.Dong M, Anda RF, Felitti VJ, et al. Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Pediatr Adolesc Med. 2005;159(12):1104–1110 [DOI] [PubMed] [Google Scholar]
- 17.Bures RM. Childhood residential stability and health at midlife. Am J Public Health. 2003;93(7):1144–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US General Accounting Office Elementary School Children: Many Change Schools Frequently, Harming Their Education. Washington, DC: US General Accounting Office; 1994:1–18 General Accounting Office publication GAO/HEHS-94-45 [Google Scholar]
- 19.Rumberger RW. The causes and consequences of student mobility. J Negro Educ. 2003;72(1):6–21 [Google Scholar]
- 20. United States Housing Act of 1937, Pub L No. 93-383, 88 Stat 653.
- 21.Joint Center for Housing Studies of Harvard University The State of the Nation's Housing, 2010. Cambridge, MA: Joint Center for Housing Studies of Harvard University; 2010. Available at: http://www.jchs.harvard.edu/publications/markets/son2010/son2010.pdf. Accessed June 23, 2010 [Google Scholar]
- 22.Wight VR, Chau M. Basic Facts About Low-Income Children, 2008: Children Under Age 18. New York, NY: National Center for Children in Poverty, Mailman School of Public Health, Columbia University; 2009. Available at: http://www.nccp.org/publications/pdf/download_307.pdf. Accessed July 2, 2010 [Google Scholar]
- 23.Nord M, Andrews MS, Carlson S. Household Food Security in the United States, 2007. Washington, DC: Economic Research Service, US Dept of Agriculture; 2008. Food Assistance and Nutrition Research report ERR-66. Available at: http://www.ers.usda.gov/Publications/ERR66/ERR66b.pdf. Accessed October 1, 2009 [Google Scholar]
- 24.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security: Revised 2000. Alexandria, VA: US Dept of Agriculture, Food and Nutrition Service; 2000. Available at: http://www.fns.usda.gov/fsec/FILES/FSGuide.pdf. Accessed October 1, 2009 [Google Scholar]
- 25.Anderson SA, ed Core indicators of nutritional state for difficult-to-sample populations. J Nutr. 1990;120(suppl 11):1559–1600 [DOI] [PubMed] [Google Scholar]
- 26.Nord M, Hopwood H. Recent advances provide improved tools for measuring children's food security. J Nutr. 2007;137(3):533–536 [DOI] [PubMed] [Google Scholar]
- 27. US Census Bureau 2010 Census questionnaire reference book. Available at: http://2010.census.gov/partners/pdf/langfiles/qrb_English.pdf. Accessed August 25, 2010
- 28.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey 1988–94. Section D, question HDY1-1507 Atlanta, GA: Centers for Disease Control and Prevention; 1994 [Google Scholar]
- 29.Monette S, Séquin L, Gauvin L, Nikiéma B. Validation of a measure of maternal perception of the child's health status. Child Care Health Dev. 2007;33(4):472–481 [DOI] [PubMed] [Google Scholar]
- 30.Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children's health. Pediatrics. 2008;121(2):337–344 [DOI] [PubMed] [Google Scholar]
- 31.Alaimo K, Olson CM, Frongillo EA, Jr., Briefel RR. Food insufficiency, family income, and health in US preschool and school-aged children. Am J Public Health. 2001;91(5):781–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kemper KJ, Babonis TR. Screening for maternal depression in pediatric clinics. Am J Dis Child. 1992;146(7):876–878 [DOI] [PubMed] [Google Scholar]
- 33.Glascoe FP. Collaborating With Parents: Using Parents’ Evaluation of Developmental Status to Detect and Address Developmental and Behavioral Problems. Nashville, TN: Ellsworth & Vandermeer Press; 1998 [Google Scholar]
- 34.American Academy of Pediatrics, Committee on Children with Disabilities Developmental surveillance and screening of infants and young children. Pediatrics. 2001;108(1):192–196 [DOI] [PubMed] [Google Scholar]
- 35.Halfon N, Regalado M, Sareen H, et al. Assessing development in the pediatric office. Pediatrics. 2004;113(suppl):1926–1933 [PubMed] [Google Scholar]
- 36.Glascoe FP. Early detection of developmental and behavioral problems. Pediatrics. 2000;21(8):272–280 [DOI] [PubMed] [Google Scholar]
- 37.National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention Use and interpretation of the CDC growth charts - an instructional guide. Available at: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/index.htm#interpretation. Accessed May 17, 2011
- 38.Kielmann AA, McCord C. Weight-for-age as an index of risk of death in children. Lancet. 1978;311(8076):1247–1250 [DOI] [PubMed] [Google Scholar]
- 39.Blake KS, Kellerson RL, Simic A. Measuring Overcrowding in Housing. Washington, DC: US Dept of Housing and Urban Development, Office of Policy Development and Research; 2007 [Google Scholar]
- 40.Pettit B, McLanahan S. Residential mobility and children's social capital: evidence from an experiment. Soc Sci Q. 2003;84(3):632–649 [Google Scholar]
- 41.Cook JT, Frank DA, Berkowitz C, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–1438 [DOI] [PubMed] [Google Scholar]
- 42.Rose-Jacobs R, Black MM, Casey PH, et al. Household food insecurity: associations with at-risk infant and toddler development. Pediatrics. 2008;121(1):65–72 [DOI] [PubMed] [Google Scholar]
- 43.Skalicky A, Meyers A, Adams W, Yang Z, Cook J, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10(2):177–185 [DOI] [PubMed] [Google Scholar]
- 44.Park K, Kersey M, Geppert J, Story M, Cutts D, Himes JH. Household food insecurity is a risk factor for iron-deficiency anaemia in a multi-ethnic, low-income sample of infants and toddlers. Public Health Nutr. 2009;12(11):2120–2128 [DOI] [PubMed] [Google Scholar]
- 45.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics. 2004;113(2):298–304 [DOI] [PubMed] [Google Scholar]
- 46.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868 [DOI] [PubMed] [Google Scholar]
- 47.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259 [DOI] [PubMed] [Google Scholar]
- 48.Pinderhughes EE, Nix R, Foster EM, Jones D; the Conduct Problems Prevention Research Group Parenting in context: impact of neighborhood poverty, residential stability, public services, social networks, and danger on parental behaviors. J Marriage Fam. 2007;63(4):941–953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kohen DE, Leventhal T, Dahinten VS, McIntosh CN. Neighborhood disadvantage: pathways of effects for young children. Child Dev. 2008;79(1):156–169 [DOI] [PubMed] [Google Scholar]
- 50.Frank DA, Neault NB, Skalicky A, et al. Heat or eat: the low income home energy assistance program and nutritional and health risks among children less than 3 years of age. Pediatrics. 2006;118(5):e1293–e1302 [DOI] [PubMed] [Google Scholar]
- 51.Meyers A, Cutts D, Frank DA, et al. Subsidized housing and children's nutritional status: data from a multisite surveillance study. Arch Pediatr Adolesc Med. 2005;159(6):551–556 [DOI] [PubMed] [Google Scholar]
- 52.Meyers A, Rubin D, Napoleone M, Nichols K. Public housing subsidies may improve poor children's nutrition. Am J Public Health. 1993;83(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mills G, Gubits D, Orr L, et al. Effects of Housing Vouchers on Welfare Families. Washington, DC: US Dept of Housing and Urban Development; 2006. Available at: http://www.huduser.org/Publications/pdf/hsgvouchers_1.pdf. Accessed October 1, 2009 [Google Scholar]
- 54.Rice D, Sard B. Decade of neglect has weakened federal low-income housing programs. Washington, DC: Center on Budget and Policy Priorities; February 24, 2009. Available at: http://www.cbpp.org/files/2-24-09hous.pdf. Accessed October 15, 2009 [Google Scholar]