SUMMARY
Actigraphy is increasingly used in the assessment and treatment of various clinical conditions, being a convenient and cost-effective method of capturing bodily movements over long periods of time. This study examined the use of actigraphy in the measurement of sleep of patients with depression and insomnia. Fifty four patients diagnosed with a current major depressive episode and chronic insomnia underwent a baseline overnight study with concurrent actigraphic and polysomnography (PSG) monitoring, as well as subjective sleep diaries. Agreement between PSG, actigraphy and sleep diary measurements was evaluated using two-tailed t-tests, Pearson’s correlations, and the Bland-Altman concordance technique. The only significant difference found between actigraphy and PSG was in latency to persistent sleep, in which actigraphy underestimated sleep latency relative to PSG (p<0.05). There were moderate positive correlations between actigraphy and PSG for all variables. In contrast, significant differences were observed between sleep diaries and PSG for all sleep variables. Bland-Altman concordance diagrams also demonstrated that, while bias was limited between PSG and the other two measurement types, there were somewhat broad 95% limits of agreement for all sleep variables with both sleep diaries and actigraphy. In summary, actigraphic measurements of sleep more closely approximated those of PSG than did sleep diaries in this sample of depressed insomniacs.
Keywords: actigraphy, polysomnography, sleep logs, depression, insomnia
INTRODUCTION
Polysomnography (PSG) has long been considered the “gold standard” for the measurement of sleep because it is able to objectively measure not only wake and sleep time, but also sleep architecture. However, PSG is limited by cost and inconvenience as a method for long-term, continuous sleep monitoring. (Ancoli-Israel et al. 2003)Because of its noninvasiveness and relatively low cost, actigraphy is emerging as a viable alternative to PSG for long-term sleep-wake cycle monitoring. Whereas PSG is often performed in a clinic or laboratory setting to record various physiological characteristics over a limited period of time, actigraphy is a non-invasive method of capturing body movements that can be used over longer periods of time in the natural sleep setting of the patient.
Published reports on the validity of actigraphy have indicated that sleep cycles measured using actigraphy scoring algorithms are relatively consistent with PSG-scored sleep in some clinical populations.(Ancoli-Israel et al. 2003;Kushida et al. 2001;Standards of Practice Committee of the American Sleep Disorders Association 2007)However, the accuracy of actigraphy in the measurement of certain sleep-wake parameters is controversial, especially in populations exhibiting disturbed sleep, and in those whose insomnia is associated with psychiatric disease.(Hauri and Wisbey 1992)Some of the larger discrepancies involve transitions from wake-to-sleep and sleep-to-wake. In some populations, periods of quiet wakefulness may be classified as sleep rather than waking by actigraphy algorithms, resulting in underestimation of sleep latency and overestimation of total sleep time.(Lichstein et al. 2006;Sadeh and Acebo 2002;Verbeek et al. 1994)The validity of actigraphy versus PSG and sleep diaries has not been extensively analyzed in patients with concurrent depression and insomnia.
Many studies on the use of actigraphy in insomniacs have also explicitly excluded patients with psychiatric disorders, such as depression. Although insomnia and depression may present separate challenges in the actigraphic measurement of sleep, it has been shown that they are frequently comorbid conditions, with over 90% of depressed patients suffering from sleep complaints. (Lichstein et al. 2000;Thase 1999)Patients with depression and insomnia tend to have lower reported quality of life, higher rates of recurrence of depression, and higher rates of suicidal ideation than those without insomnia.(McCall et al. 2010a;McCall et al. 2010b;McCall et al. 2000;Moos and Cronkite 1999)Therefore it is of great clinical value to determine whether actigraphy is a viable method of measuring sleep in patients with concurrent insomnia and depression.
The aim of this study was to analyze differences between actigraphy, PSG, and sleep diary reports for measuring sleep-wake cycles in subjects with major depressive episode (MDE) and insomnia.
METHODS
This is a post-hoc analysis of a clinical trial whose primary endpoint was quality of life; full details of the research protocol are described elsewhere. (McCall et al. 2010b) Briefly, 54 patients diagnosed with both insomnia and MDE underwent one night of laboratory monitoring by polysomnography (PSG), actigraphy, and sleep diaries timed to coincide with their normal sleep schedule.
Subjects
Fifty four participants aged 19–64 years participated in the study. This protocol was approved by the local institutional review board, and all participants provided signed, informed consent. At baseline, participants reported experiencing either a) sleep latency >30 minutes and sleep efficiency <85% at least four nights per week, or b) met Research Diagnostic Criteria (RDC) for insomnia at least four nights per week. (Edinger et al. 2004)
A confirmation diagnosis of unipolar MDE per Structural Clinical Interview for DSM-IV (SCID) was made during the first face-to-face visit after >7 days of abstinence from all psychotropic medications (4 weeks for fluoxetine). (American Psychiatric Association 1994) Participants with clinically significant sleep apnea (apnea-hypopnea index (AHI) > 15) or clinically significant periodic limb movement (PLM) disorder (PLM-arousal index (PLMAI) of > 15) were excluded. (McCall et al. 2009)
Measurements of sleep
The measurements of sleep for this study included self-reported sleep diaries and objective measures of actigraphy and PSG.
PSG
Participants completed one night of eight-hour PSG data collection. At this time participants were free of psychotropic medications for >2 weeks. PSG was started at their median bedtime as defined from the prospective diary collection. The PSG montage included four EEG channels (C3-A2, C4-A1, C3-O1, and C4-O2), left and right EOG, chin EMG, right and left anterior tibialis EMG, EKG, nasal thermistor, oral thermistor, respiratory effort, and pulse oximetry. The PSG data were digitally collected on a VIASYS SomnoStar® system. Scoring was completed according to standard criteria, and was blind to participant identity. (Iber et al. 2007) The PSG parameters measured in this study include latency to the onset of the first sleep epoch (SOL), latency to persistent sleep (LPS), sleep efficiency (SE), wakefulness after sleep onset (WASO), and total sleep time (TST). LPS was defined as the time from “lights out” to the first epoch of 10 consecutive minutes of uninterrupted sleep.
Sleep diaries
Participants were instructed to keep prospective, daily sleep diary entries of their bedtime, sleep latency, number of awakenings, WASO, TST, and rising time during the week before the laboratory night and on the laboratory monitoring night. The median bedtime recorded in the prospective sleep diaries was used as the starting time for the laboratory monitoring period. Participants also completed the Insomnia Severity Index (ISI) at their laboratory visit. Higher scores on the ISI represent greater degrees of insomnia.(Bastien et al. 2001)
Actigraphy
Participants continuously wore a Mini Mitter actigraphy monitor (AW64 Actiwatch®) on their non-dominant wrist for the laboratory monitoring night. The AW64 output was scored using the proprietary Actiware® Software, version 5.0. The medium sensitivity setting at 30-second epochs was used for actigraphic data in order to mirror the PSG 30-second epoch. The laboratory monitoring period began at each participant’s median bedtime as defined from prospective diary collection of the week prior. Sleep variables were measured starting at the time set by laboratory technicians for “lights out”, and ending eight hours later.
Analysis
Post-hoc analyses of differences of sleep measurement methods between sleep variables were performed using SAS JMP® (version 8.0) data analysis software. For all analyses, a two-tailed p-value <0.05 was considered statistically significant. Basic analytic approaches included Pearson’s test for correlation, two-tailed paired t-tests to calculate whether the difference between measurement methods were different from ‘0’, and the Bland and Altman concordance technique. (McCall et al. 2010b)
Certain variables such as latency to persistent sleep (LPS) and sleep efficiency (SE) were not acquired in all measurement methods. Only PSG provided a measurement of LPS; for comparisons involving LPS, the sleep onset latency (SOL) value was used for actigraphy and sleep diaries. Sleep efficiency was not captured in sleep diaries; therefore, calculations for sleep efficiency were performed for PSG and actigraphy only.
RESULTS
An analysis of subject demographics and baseline symptoms was performed and reported elsewhere. (McCall et al. 2010b) The overall randomized sample was middle-aged, two-thirds women, and 20% minorities. The baseline severity of insomnia as reflected by the Insomnia Severity Index (ISI) was in the moderate range, while depression severity as reflected by the HRSD was in the moderate to severe range. Most participants experienced MDE of the melancholic subtype. (Table 1)
Table 1.
Baseline Demographics and Measures of Depression and Insomnia (N=54) N (%) or Mean ± Standard Deviation
| Characteristic | Total sample |
|---|---|
| Gender | |
| Male | 18 (33.3) |
| Female | 36 (66.7) |
| Age | 41.3 ± 12.9 |
| Race | |
| Caucasian | 43(79.6) |
| African-American | 10(18.5) |
| Other | 1 (1.9) |
| Body Mass Index (BMI) | 27.7 ± 5.0 |
| Mini Mental State Exam (MMSE) | 29.4 ± 0.9 |
| 24-item Hamilton Rating Scale for Depression | 27.3 ± 3.9 |
| ISI Total Score | 20.5 ± 4.0 |
There were no significant differences between actigraphy and PSG measurements for any variables except LPS, in which actigraphy measured a shorter mean latency time than PSG (t=2.27, DF=53, p<0.05). Moderate correlations (from 0.31 for sleep onset latency to 0.59 for WASO, p<0.05) were found between actigraphy and PSG for all variables. (Table 2)
Table 2.
Actigraphy vs. PSG
| Variables | Means (Minutes) ± Std Deviation | Mean Difference ± Std Error (Two-Tailed) (Minutes) | Pairwise Correlation | |
|---|---|---|---|---|
| ACT | PSG | |||
| SLO | 24.2 ± 28.0 | 28.4 ± 36.9 | 4.19 ± 5.3(NS) | 0.31(p<0.05) |
| LPS | 24.2 ± 28.0 | 35.2 ± 37.6 | 11.0 ± 4.8(p<0.05) | 0.44(p<0.001) |
| SE | 82.7 ± 9.8 | 80.7 ± 13.4 | 2.0 ± 1.7(NS) | 0.48 (p<0.001) |
| WASO | 61.2 ± 40.2 | 61.1 ± 52.8 | 0.1 ± 6.0 (NS) | 0.59(p<0.001) |
| TST | 400.4 ± 41.9 | 387.5 ± 64.5 | 12.8 ± 7.5(NS) | 0.54(p<0.001) |
In contrast, between PSG and sleep diaries, significant differences were found for all variables recorded, with diaries recording a significantly longer mean latency (SOL and LPS) and WASO, and a shorter mean TST. However, all variables were moderately correlated (ranging from 0.33 in total sleep time to 0.45 for LPS, p<0.05). (Table 3) Significant differences were found between actigraphy and sleep diaries for all variables. WASO and TST were moderately correlated. (Table 4)
Table 3.
PSG vs. Sleep Diaries
| Variables | Means (Minutes) ± Std Deviation | Mean Difference ± Std Error (Two-Tailed) (Minutes) | Pairwise Correlation | |
|---|---|---|---|---|
| PSG | Diary | |||
| SLO | 28.4 ± 36.9 | 64.3 ± 59.4 | 35.8 ± 7.4(p<0.001) | 0.44 (p<0.001) |
| LPS | 35.2 ± 37.6 | 64.3 ± 58.3 | 29.1 ± 7.4(p<0.001) | 0.45 (p<0.001) |
| WASO | 61.1 ± 51.8 | 85.4 ± 84.0 | 24.3 ± 10.8(p<0.05) | 0.40 (p<0.005) |
| TST | 387.5 ± 64.5 | 333.1 ± 105.1 | 54.5 ± 14.1(p<0.001) | 0.33 (p<0.05) |
Table 4.
Actigraphy vs. Sleep Diaries
| Variables | Means (Minutes) ± Std Deviation | Mean Difference ± Std Error (Two-Tailed) (Minutes) | Pairwise Correlation | |
|---|---|---|---|---|
| ACT | Diary | |||
| SLO | 24.2 ± 28.0 | 64.3 ± 59.4 | 340.0 ± 8.3(p<0.001) | 0.22 (NS) |
| WASO | 61.2 ± 40.2 | 85.4 ± 84.0 | 24.2 ± 9.3(p<0.05) | 0.59(p<0.001) |
| TST | 400.4 ± 41.9 | 333.1 ± 105.1 | 67.3 ± 13.1(p<0.001) | 0.40(p<0.005) |
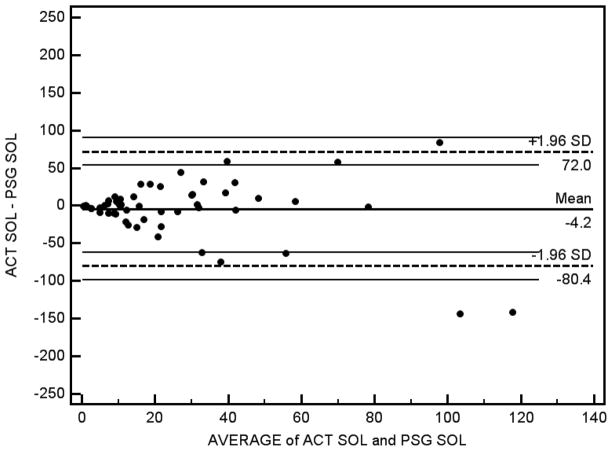
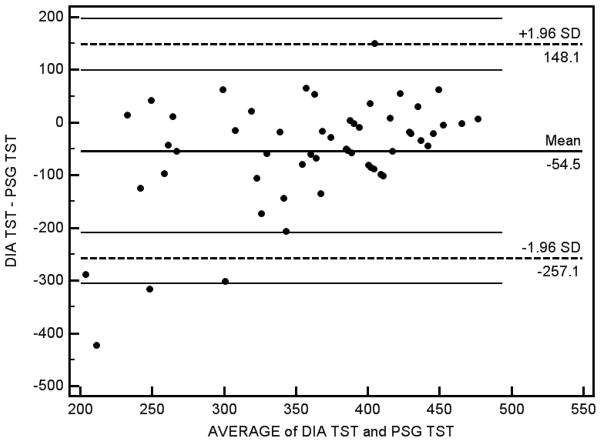
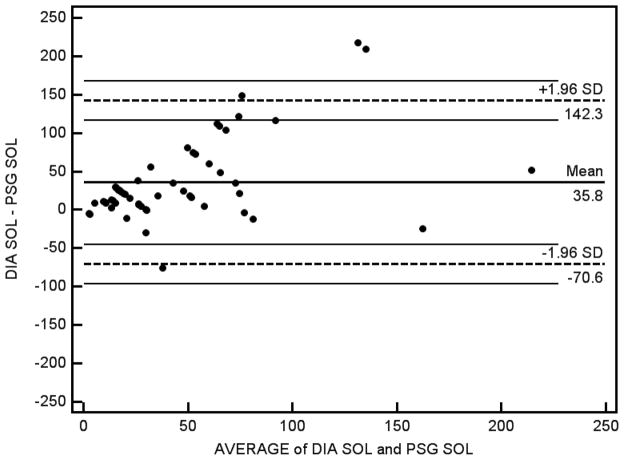
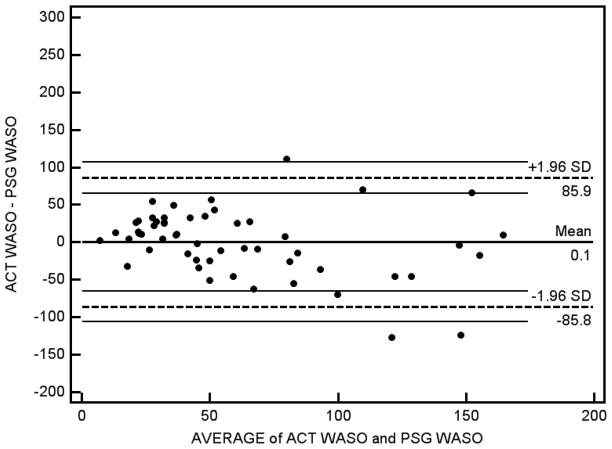
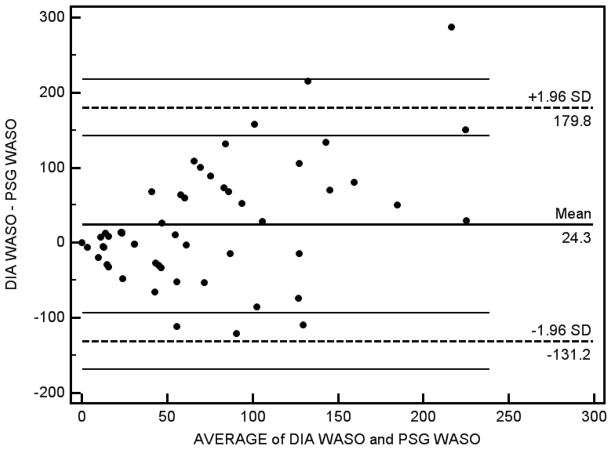
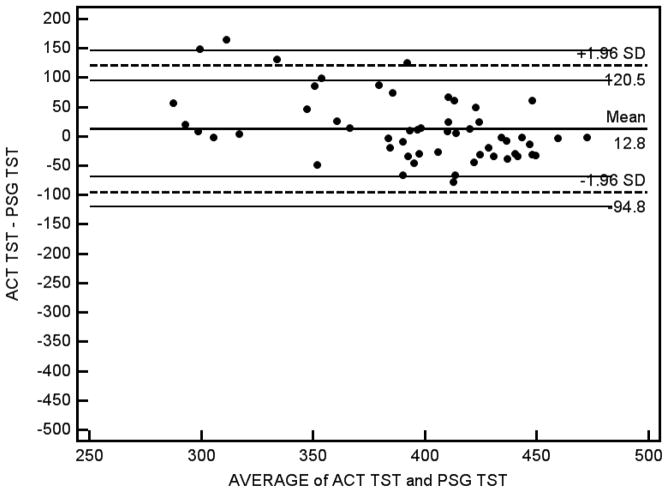
The Bland-Altman concordance technique was also used to compare actigraphy and sleep diaries to PSG in measurements of SOL, WASO, and TST. The results of this analysis confirmed our paired t-test findings demonstrating that the mean difference between PSG and actigraphy was smaller than the mean difference between PSG and sleep diaries for each of these variables. Although the bias was limited in the comparison between PSG and the other measurement modalities, the 95% limits of agreement were nevertheless somewhat broad, indicating some disagreement with both actigraphy and PSG. For SOL and WASO, it appears that as the average value of SOL or WASO increased, the disagreement between measurement modalities also increased. Bland and Altman difference plots for these measurements between PSG and the other two methods are presented in Figures 1 to 6.
Figure 1.
Sleep Onset Latency (Actigraphy – PSG)
Figure 6.
Total Sleep Time (Sleep Diaries – PSG)
DISCUSSION
The results of this analysis found few statistically or clinically significant differences between PSG and actigraphy measurements in this sample of depressed insomniacs. Actigraphic measurements were more accurate than sleep diaries when compared to PSG, with significant correlations between actigraphy and PSG on most variables. In contrast, significant differences were observed between sleep diaries and PSG. These results suggest that actigraphy may be an appropriate method for the assessment of sleep in patients with depression and insomnia. Our findings support the practice parameters of the American Academy of Sleep Medicine, which state that actigraphy is indicated as a method to characterize sleep patterns in individuals with insomnia and depression; this has not been previously demonstrated in comparison to a reference standard of PSG or sleep logs. (Standards of Practice Committee of the American Sleep Disorders Association 2007)
However, despite the limited bias between actigraphy and PSG found in the Bland-Altman concordance analysis, the broad 95% limits of agreement suggest that there may still be disparities between these measurement modalities in individual cases. This was especially true for sleep onset latency and WASO; as the average value for these sleep variables increased, there appeared to be less agreement between the measurements. In the case of sleep latency, this suggests that actigraphy may be less accurate with longer sleep latencies than with shorter sleep latencies. With patients in this study for whom actigraphy measured much shorter sleep latency than PSG, actigraphy may have falsely reported long periods of quiet wakefulness as sleep. However, in other patients, actigraphically-measured latency was much longer than PSG-measured latency. In these cases, patients may have exhibited body movements or disturbed sleep for long periods. These discrepancies suggest that while actigraphy is an accurate method for measuring sleep in most patients with depression and insomnia, there may be significant discrepancies for some individuals.
Choice of actigraphy product and accompanying proprietary algorithm, sensitivity level, use of non-dominant versus dominant wrist, and the analysis of the first night in the sleep lab may also have affected our actigraphic findings in this study. These findings pertain only to patients with both depression and insomnia who are not undergoing medical treatment for these disorders, and may not be relevant to normal or non-depressed insomniacs. Further research is needed to promote standardization of actigraphic protocol in research and clinical use for patients with depression and insomnia.
Figure 2.
Sleep Onset Latency (Sleep Diaries – PSG)
Figure 3.
Wake Time After Sleep Onset (Actigraphy – PSG)
Figure 4.
Wake Time After Sleep Onset (Sleep Diaries – PSG)
Figure 5.
Total Sleep Time (Actigraphy – PSG)
Acknowledgments
NIH MH70821 and M01-RR07122, as well as funding and medications from Sepracor, and funding and material support from Mini Mitter
Footnotes
ClinicalTrials.gov Identifier: NCT00247624
Disclosures: Dr. W. Vaughn McCall is on the Speaker Bureau for Sepracor and Merck and has received research support from Sealy, Sepracor, Mini Mitter, Corcept, and Sanofi. He is an advisor to Sealy. No other authors report any disclosures.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 Washington, DC: 1994. [Google Scholar]
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollack C. The Role of Actigraphy in the Study of Sleep and circadian Rhythms. Sleep. 2003;26:342–359. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Bonnet MH, Bootzin RR, Doghramji K, Dorsey CM, Epsie C, Jamieson A, McCall V, Morin CM, Stepanski E. Derivation of research diagnostic criteria for insomnia: Report of an American Academy of Sleep Medicine work group. Sleep. 2004;27:1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- Hauri P, Wisbey J. Wrist actigraphy in insomnia. Sleep. 1992;15:293–300. doi: 10.1093/sleep/15.4.293. [DOI] [PubMed] [Google Scholar]
- Iber C, Ancoli-Israel S, Chesson A, Quan S. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. American Academy of Sleep Medicine; 2007. [Google Scholar]
- Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Medicine. 2001:389–396. doi: 10.1016/s1389-9457(00)00098-8. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Stone KC, Donaldson J, Nau SD, Soeffling JP, Murray D, Lester K, Aguillard R. Actigraphy validation with insomnia. Sleep. 2006;29:232–239. [PubMed] [Google Scholar]
- Lichstein KL, Wilson NM, Johnson CT. Psychological treatment of secondary insomnia. Psychol Aging. 2000;15:232–240. doi: 10.1037//0882-7974.15.2.232. [DOI] [PubMed] [Google Scholar]
- McCall WV, Blocker JN, D’Agostino R, Jr, Kimball J, Boggs N, Lasater B, Rosenquist PB. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Medicine. 2010a;11:822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Blocker JN, D’Agostino RB, Jr, Kimball J, Boggs N, Lasater B, Haskett R, Krystal A, McDonald WM, Rosenquist PB. Treatment of insomnia in depressed insomniacs: effects on health-related quality of life, objective and self-reported sleep, and depression. Journal of Clinical Sleep Medicine. 2010b;6:322–329. [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Kimball J, Boggs N, Lasater B, D’Agostino RB, Jr, Rosenquist PB. Prevalence and prediction of primary sleep disorders in a clinical trial of depressed patients with insomnia. Journal of Clinical Sleep Medicine. 2009;5:454–458. [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Reboussin BA, Cohen W. Subjective measurement of insomnia and quality of life in depressed inpatients. J Sleep Res. 2000;9:43–48. doi: 10.1046/j.1365-2869.2000.00186.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Cronkite RC. Symptom-based predictors of a 10-year chronic course of treated depression. J Nerv Ment Dis. 1999;187:360–368. doi: 10.1097/00005053-199906000-00005. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Medicine Reviews. 2002;6:113–124. doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- Standards of Practice Committee of the American Sleep Disorders Association. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: An update for 2007. Sleep. 2007;30:519–529. [Google Scholar]
- Thase ME. Antidepressant treatment of the depressed patient with insomnia. J Clin Psychiatry. 1999;60 (Suppl):28–31. [PubMed] [Google Scholar]
- Verbeek I, Arends J, Declerck G, Beecher L. Wrist actigraphy in comparison with polysomnography and subjective evaluation in insomnia. Sleep-Wake Research in the Netherlands. 1994;5:163–169. [Google Scholar]