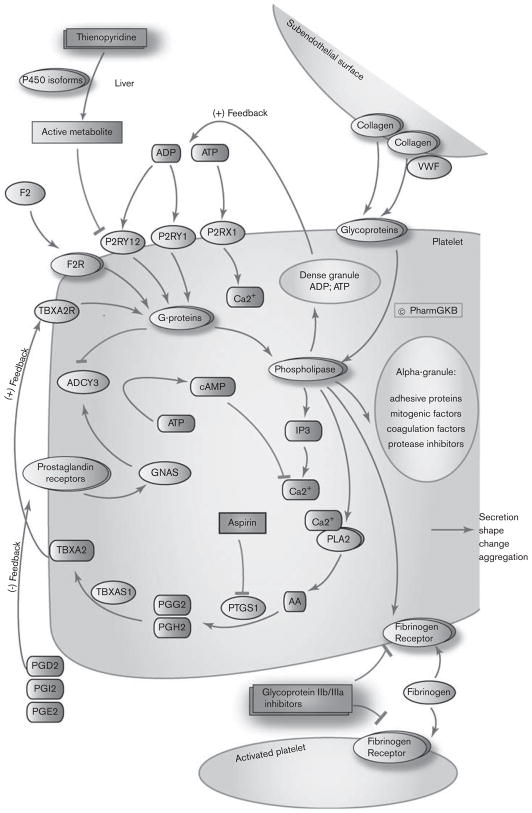
Platelet activation and coagulation normally do not occur in an intact blood vessel. After blood vessel wall injury, platelet plug formation is initiated by the adherence of the platelets to subendothelial collagen [1,2]. In high shear arterial blood, platelets are first slowed down from their blood flow velocity by interacting with the collagen-bound von Willebrand factor and are subsequently stopped by binding directly to the collagen by their glycoprotein (GP) receptor complex [2,3]. The activation of these collagen receptors on platelets after their binding to the collagen activates phospholipase C-mediated cascades (Fig. 1) [1–3]. This results in the mobilization of calcium from the dense tubular system [4,5]. An increase in intracellular calcium is associated with the activation of several kinases necessary for morphologic change, the presentation of the procoagulant surface, the secretion of platelet granular content, the activation of GPs, and the activation of phospholipase A2 (see Fig. 1) [2,5–7]. The presentation of the procoagulant surface results in the colocalization of different coagulation factors on the surface of the activated platelet, which triggers a series of zymogen conversions, resulting in the release of active thrombin from prothrombin [8]. Adenosine diphosphate (ADP), adenosine triphosphate, and serotonin are released from the dense platelet granule. Activated phospholipase A2 enzymes release arachidonic acid (AA) by the cleaving of fatty acids, especially phosphatidylcholine and phosphatidylethanolamine, at their sn-2 position [9–11]. AA is a precursor for thromboxane A2 (TBXA2) synthesis. In the first step in platelets, prostaglandin (PG)-endoperoxide synthase 1 (PTGS1; also known as cyclooxygenase 1) catalyzes the transformation of AA into cyclic endoperoxide PG G2 and H2 [9]. In platelets, PGG2 and PGH2 are then mainly converted by TBXA synthase into TBXA2 [9].
Fig. 1.
Effects of antiplatelet drugs in platelet aggregation pathway. (PA154444041; http://www.pharmgkb.org/do/serve?objId=PA154444041&objCls=Pathway). AA, arachidonic acid; cAMP, cyclic AMP; GNAS, guanine nucleotide binding protein a s; IP3, inositol 1,4,5-trisphosphate; PGD2, prostaglandin D2; PGE2, prostaglandin E2; PGG2, prostaglandin G2, PGH2, prostaglandin H2; PGI2, prostaglandin I2; PTGS1, prostaglandin (PG)-endoperoxide synthase 1; PLA2, phospholipase A2; TBXA2, thromboxane A2; TBXA2R, TBXA2 receptor; VWF, von Willebrand factor.
The mechanism of action of aspirin is the inhibition of PTGS1, thereby preventing the production of PGs and, particularly in platelets, inhibiting TBXA2 production [10–12]. In ex vivo platelet aggregation testing, aspirin affects predominantly AA-stimulated platelet aggregation through a direct pathway, and also collagen-stimulated platelet aggregation through indirect pathways. A review by Lopez Farre et al. [12] discusses further mechanisms associated with platelet response to aspirin.
The processes described above result in the local accumulation of molecules such as thrombin, TBXA2, and ADP, which are important for the further recruitment of platelets and the amplification of activation signals as described above. The secreted agonists activate their respective G protein-coupled receptors: coagulation factor II (thrombin) receptors (F2R also known as protease-activated receptor 1; F2RL3 also known as protease-activated receptor 4), TBXA2 receptor (TBXA2R), and ADP receptors (P2RY1 and P2RY12) [10,11,13–15]. The P2RY12 receptor couples to Gi, and when activated by ADP, inhibits adenylate cyclase [16]. This interaction counteracts the stimulation of cyclic AMP formation by endothelial-derived PGs, which alleviates the inhibitory effect of cyclic AMP on inositol 1,4,5-trisphosphate-mediated calcium release [14,16–20]. P2RY12 has a major role in arterial thrombosis and pharmacologic targeting of this receptor, which is an important strategy in the treatment of cardiovascular diseases [21]. Thienopyridines (ticlopidine, clopidogrel, prasugrel), a class of oral anti-platelet agents, permanently inhibit P2RY12 signaling by irreversibly binding the receptor and blocking ADP-induced platelet activation and aggregation [22].
F2R, TBXA2R, and P2RY1 couple to Gq-phospholipase C–inositol 1,4,5-trisphosphate–Ca2+ pathway, inducing shape change and platelet aggregation [14,23,24]. In addition, receptor signaling by G12/13 (F2R; TBXA2R) contributes to morphologic changes through the activation of kinases [23,24]. Platelet adhesion, cytoskeletal reorganization, secretion, and amplification loops are all different steps toward the formation of a platelet plug. These cascades finally result in the activation of the fibrinogen receptor (GPIIb/GPIIIa) expressed on platelet cells [14,25,26]. This activation results in the exposure of the binding sites for fibrinogen, which are not available in inactive platelets. The binding of fibrinogen results in the linkage of the activated platelets through fibrinogen bridges, thereby mediating aggregation [3]. The inhibition of this receptor by GPIIb/GPIIIa inhibitors blocks platelet aggregation induced by any agonist [27,28].
The individual platelet response is variable because of polymorphisms in genes involved in the activation and aggregation of platelets, in conjunction with environmental factors, and contributes to diseases such as arterial thrombosis ([29–33], and http://www.bloodomics.org/web/). In addition to the variation in platelet physiology, platelet sensitivity to drugs targeting platelet activation and aggregation is also influenced by gene polymorphisms and clinical and environmental variables [29,31,34].
Variability in platelet response to aspirin
Not all individuals respond equally to aspirin therapy and cardiovascular events may occur during aspirin therapy, which is often referred to as ‘clinical aspirin resistance’ [12]. The term aspirin resistance has also been used in the laboratory context. Here, aspirin resistance describes persistent platelet reactivity in vitro, despite the use of aspirin, measured by various platelet function tests such as measurement of serum and urinary thromboxane metabolites, and AA-induced platelet aggregation, collagen-induced platelet aggregation, or ADP-induced platelet aggregation [35,36]. One limitation of the assessment of the various functional indexes of platelet capacity that can be measured ex vivo with in-vitro tests is the largely unknown translational relevance to the actual occurrence of platelet activation and inhibition in vivo [37]. Several studies have shown that diabetes mellitus [38–41] and obesity [35,42] are related to aspirin variability. Furthermore, polymorphisms in different genes have been associated with variability to aspirin response. The review by Feher et al. [34] found that the role of single nucleotide polymorphisms (SNPs) in PTGS1, PTGS2 (also known as cyclooxygenase 2), GPIb α (GP1BA), GPIa (ITGA2), GPIIIa (ITGB3), ADP receptor (P2RY1), and uridine 5′-diphospho-glucuronosyltransferase 1 family, polypeptide A6 (UGT1A6) in the context of aspirin resistance. The investigators concluded that the results are difficult to replicate between different research groups partially explained by the use of different platelet functions tests and that larger, population-based studies are needed to fully clarify the variability in platelet response [34]. Another recent review by Zuern et al. [29] summarized the pharmacogenomics of aspirin based on several studies investigating the effects of SNPs in PTGS1, PTGS2, ITGB3, P2RY1, and GPVI (GP6) genes with the conclusion that the reasons for insufficient response to aspirin are diverse and are still not well understood. Recent studies suggest that variants in the platelet endothelial aggregation receptor 1 (PEAR1) gene may influence agonist-stimulated platelet aggregation [43,44] and response to aspirin [43].
Variability in platelet response to clopidogrel
Clopidogrel must be metabolized into an active metabolite by liver cytochrome P-450 enzymes. Functional variants in CYP2C19 have been associated with decreased active metabolite, decreased inhibition of platelet aggregation ex vivo, and increased cardiovascular event rates in patients on clopidogrel (see also Clopidogrel PK pathway at PharmGKB PA154424674, http://www.pharmgkb.org/do/serve?objId=PA154424674&objCls=Pathway, [45]). The CYP2C19*2 loss-of-function variant was significantly associated with lower exposure to active metabolite in patients treated with clopidogrel [46,47]. Furthermore, CYP2C19*2 and other loss-of-function variants have been associated with decreased platelet responsiveness to clopidogrel ex vivo [47–49]. The decreased responsiveness and high on-clopidogrel platelet reactivity have been associated with increased cardiovascular event rates in patients on clopidogrel [47,50–54]. The large amount of evidence regarding the heterogeneity of clopidogrel response led the US Food and Drug Agency to modify the label of clopidogrel to include information regarding CYP2C19 pharmacogenetics and a boxed warning. Several recent studies discuss the value of an implementation of CYP2C19 genotyping to guide antiplatelet therapy [55–58]. Studies by Sibbing et al. [59] found that the carrier status of the gain-of-function variant CYP2C19*17 was significantly associated with enhanced response to clopidogrel and an increased risk of bleeding [60]. However, not all studies have found an independent effect of the CYP2C19*17 allele. Early candidate gene and clinical studies implicated variants in other genes involved in the metabolism and transport of clopidogrel, such as CYP3A4 [61], CYP2C9 [46,62,63], ABCB1 [51,64], and CYP2B6 [47], with clopidogrel response. However, these studies were not consistently replicated.
SNPs in the ADP receptors (P2RY1 and P2RY12), the target of clopidogrel, have also been studied in connection with platelet response variability to clopidogrel. Much of the work so far has been contradictory or has failed to identify genetic variants as significantly associated with response. No association between response to clopidogrel and P2RY1 polymorphisms was found [65,66]. The influence of P2RY12 genetic polymorphisms on clopidogrel response is not clear yet [29]. Initially, a study by Ziegler et al. [67] suggested that a genetic variation of the P2RY12 gene (34C > T, no rs number) is associated with higher numbers of cerebrovascular events in patients with peripheral artery disease receiving clopidogrel therapy. A recent study by Simon et al. [51], found no association between polymorphisms of P2RY12 and clinical outcomes in patients with acute myocardial infarction, who were treated with clopidogrel, and is in accordance with a number of other studies failing to show functional effect of P2RY12 SNPs in patients treated with clopidogrel [49,65,68–71]. Contrary to those results, a study of patients with coronary artery disease suggested a contribution of the homozygote H2 haplotype (as measured by the tagging SNP 52G > T, rs6809699) to clopidogrel resistance [72]. Another study in patients with coronary artery disease also found that common variation in the P2RY12 gene is a significant determinant of the interindividual variability in residual on-clopidogrel platelet reactivity measured by ADP-induced light transmittance aggregometry and the VerifyNow P2RY12 assay [73]. Haplotype F (tagging SNP rs2046934, i-T744C) was associated with significantly lower residual on-clopidogrel platelet reactivity compared with the reference haplotype A (tagging SNP rs6798347) [73]. The PlA2 polymorphism in the ITGB3 gene, which encodes the platelet membrane GPIIIa, was also found to modulate clopidogrel-mediated antiplatelet effects [74,75].
Several methods of ex vivo platelet aggregation used to define responsiveness to clopidogrel have been established, including ADP-induced light transmission aggregation, platelet function analyzer, multiple electrode aggregometry, Verify Now assay, and analysis of the degree of vasodilator-stimulated phosphoprotein phosphorylation [76]. The high assay variability and lack of standardization and definition of nonresponsiveness makes it difficult to decide which methodology reflects the true platelet activity of a patient and to evaluate the effect of genetic polymorphisms on the ex vivo platelet reactivity of antiplatelet drugs. The popular study (Do Platelet Function Assays Predict Clinical Outcomes in Clopidogrel-Pretreated Patients Undergoing Elective PCI) compared five different platelet function tests with the result that only the light transmittance aggregometry, Verify-Now, and Platelet works assays were significantly associated with the primary end point, defined as nonfatal acute myocardial infarction, stent thrombosis, and ischemic stroke, occurring more frequently in patients with high on-treatment platelet reactivity [77]. In addition to genetic factors, demographic and clinical variables, such as age [49,50,53,78], diabetes mellitus [50,78], obesity [50,53,79], smoking [80,81], acute coronary syndromes, poor left ventricular function, and renal failure [78], have been shown to influence variation in platelet function in response to clopidogrel.
Variability in platelet response to glycoprotein IIb/IIIa inhibitors
Only a small number of studies have investigated the pharmacogenomics of GPIIb/IIIa inhibitors and there are limited data available to support the relevance of genetic variants in response to these inhibitors [29]. All the studies have examined the well-known ITGB3 SNP PlA1/A2, also known as human platelet antigen-1 PIA and rs5918. Michelson et al. [82] found that heterozygotes for PlA1/A2 were more sensitive to abciximab compared with other genotypes. Wheeler et al. [83] found reduced inhibition by abciximab in platelets in patients with the PlA2 SNP. A study by Sirotkina et al. [84] supports an association between this SNP and sensitivity to GPIIb/IIIa antagonists. Weber et al. [85] failed to find any association between this genotype and the inhibition of fibrinogen binding by abciximab or eptifibatide. Similarly, Schrör and Weber [86] showed that the human platelet antigen-1 genotype did not influence the inhibition of fibrinogen binding by GPIIb/IIIa receptor antagonists (abciximab, eptifibatide, and tirofiban) in healthy volunteers or patients with stable coronary heart disease.
Acknowledgments
PharmGKB and AR Shuldiner are supported by the NIH/ NIGMS (GM61374 and U01 HL072515).
References
- 1.Clemetson KJ, Clemetson JM. Platelet collagen receptors. Thromb Haemost. 2001;86:189–197. [PubMed] [Google Scholar]
- 2.Jurk K, Kehrel BE. Platelets: physiology and biochemistry. Semin Thromb Hemost. 2005;31:381–392. doi: 10.1055/s-2005-916671. [DOI] [PubMed] [Google Scholar]
- 3.Timmons S, Kloczewiak M, Hawiger J. ADP-dependent common receptor mechanism for binding of von Willebrand factor and fibrinogen to human platelets. Proc Natl Acad Sci U S A. 1984;81:4935–4939. doi: 10.1073/pnas.81.15.4935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen D, Bernstein AM, Lemons PP, Whiteheart SW. Molecular mechanisms of platelet exocytosis: role of SNAP-23 and syntaxin 2 in dense core granule release. Blood. 2000;95:921–929. [PubMed] [Google Scholar]
- 5.Rendu F, Brohard-Bohn B. The platelet release reaction: granules’ constituents, secretion and functions. Platelets. 2001;12:261–273. doi: 10.1080/09537100120068170. [DOI] [PubMed] [Google Scholar]
- 6.Kramer RM, Roberts EF, Manetta JV, Hyslop PA, Jakubowski JA. Thrombin-induced phosphorylation and activation of Ca(2+)-sensitive cytosolic phospholipase A2 in human platelets. J Biol Chem. 1993;268:26796–26804. [PubMed] [Google Scholar]
- 7.Lemons PP, Chen D, Whiteheart SW. Molecular mechanisms of platelet exocytosis: requirements for alpha-granule release. Biochem Biophys Res Commun. 2000;267:875–880. doi: 10.1006/bbrc.1999.2039. [DOI] [PubMed] [Google Scholar]
- 8.Coughlin SR. Protease-activated receptors in hemostasis, thrombosis and vascular biology. J Thromb Haemost. 2005;3:1800–1814. doi: 10.1111/j.1538-7836.2005.01377.x. [DOI] [PubMed] [Google Scholar]
- 9.Stassen JM, Arnout J, Deckmyn H. The hemostatic system. Curr Med Chem. 2004;11:2245–2260. doi: 10.2174/0929867043364603. [DOI] [PubMed] [Google Scholar]
- 10.Patrono C. Aspirin as an antiplatelet drug. N Engl J Med. 1994;330:1287–1294. doi: 10.1056/NEJM199405053301808. [DOI] [PubMed] [Google Scholar]
- 11.Yasuda O, Takemura Y, Kawamoto H, Rakugi H. Aspirin: recent developments. Cell Mol Life Sci. 2008;65:354–358. doi: 10.1007/s00018-007-7449-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez Farre AJ, Tamargo J, Mateos-Caceres PJ, Azcona L, Macaya C. Old and new molecular mechanisms associated with platelet resistance to antithrombotics. Pharm Res. 2010 doi: 10.1007/s11095-010-0209-4. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.McLaughlin JN, Mazzoni MR, Cleator JH, Earls L, Perdigoto AL, Brooks JD, et al. Thrombin modulates the expression of a set of genes including thrombospondin-1 in human microvascular endothelial cells. J Biol Chem. 2005;280:22172–22180. doi: 10.1074/jbc.M500721200. [DOI] [PubMed] [Google Scholar]
- 14.Tolhurst G, Vial C, Leon C, Gachet C, Evans RJ, Mahaut-Smith MP. Interplay between P2Y(1), P2Y(12), and P2X(1) receptors in the activation of megakaryocyte cation influx currents by ADP: evidence that the primary megakaryocyte represents a fully functional model of platelet P2 receptor signaling. Blood. 2005;106:1644–1651. doi: 10.1182/blood-2005-02-0725. [DOI] [PubMed] [Google Scholar]
- 15.Hollopeter G, Jantzen HM, Vincent D, Li G, England L, Ramakrishnan V, et al. Identification of the platelet ADP receptor targeted by antithrombotic drugs. Nature. 2001;409:202–207. doi: 10.1038/35051599. [DOI] [PubMed] [Google Scholar]
- 16.Hardy AR, Jones ML, Mundell SJ, Poole AW. Reciprocal cross-talk between P2Y1 and P2Y12 receptors at the level of calcium signaling in human platelets. Blood. 2004;104:1745–1752. doi: 10.1182/blood-2004-02-0534. [DOI] [PubMed] [Google Scholar]
- 17.Den Dekker E, Gorter G, Heemskerk JW, Akkerman JW. Development of platelet inhibition by cAMP during megakaryocytopoiesis. J Biol Chem. 2002;277:29321–29329. doi: 10.1074/jbc.M111390200. [DOI] [PubMed] [Google Scholar]
- 18.Eigenthaler M, Nolte C, Halbrugge M, Walter U. Concentration and regulation of cyclic nucleotides, cyclic-nucleotide-dependent protein kinases and one of their major substrates in human platelets. Estimating the rate of cAMP-regulated and cGMP-regulated protein phosphorylation in intact cells. Eur J Biochem. 1992;205:471–481. doi: 10.1111/j.1432-1033.1992.tb16803.x. [DOI] [PubMed] [Google Scholar]
- 19.Jakobs KH, Watanabe Y, Bauer S. Interactions between the hormone-sensitive adenylate cyclase system and the phosphoinositide-metabolizing pathway in human platelets. J Cardiovasc Pharmacol. 1986;8 (Suppl 8):S61–S64. doi: 10.1097/00005344-198600088-00013. [DOI] [PubMed] [Google Scholar]
- 20.Rink TJ, Sage SO. Calcium signaling in human platelets. Annu Rev Physiol. 1990;52:431–449. doi: 10.1146/annurev.ph.52.030190.002243. [DOI] [PubMed] [Google Scholar]
- 21.Storey RF. Biology and pharmacology of the platelet P2Y12 receptor. Curr Pharm Des. 2006;12:1255–1259. doi: 10.2174/138161206776361318. [DOI] [PubMed] [Google Scholar]
- 22.Herbert JM, Savi P. P2Y12, a new platelet ADP receptor, target of clopidogrel. Semin Vasc Med. 2003;3:113–122. doi: 10.1055/s-2003-40669. [DOI] [PubMed] [Google Scholar]
- 23.Offermanns S, Laugwitz KL, Spicher K, Schultz G. G proteins of the G12 family are activated via thromboxane A2 and thrombin receptors in human platelets. Proc Natl Acad Sci U S A. 1994;91:504–508. doi: 10.1073/pnas.91.2.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jin J, Kunapuli SP. Coactivation of two different G protein-coupled receptors is essential for ADP-induced platelet aggregation. Proc Natl Acad Sci U S A. 1998;95:8070–8074. doi: 10.1073/pnas.95.14.8070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dorsam RT, Kim S, Jin J, Kunapuli SP. Coordinated signaling through both G12/13 and G(i) pathways is sufficient to activate GPIIb/IIIa in human platelets. J Biol Chem. 2002;277:47588–47595. doi: 10.1074/jbc.M208778200. [DOI] [PubMed] [Google Scholar]
- 26.Quinton TM, Ozdener F, Dangelmaier C, Daniel JL, Kunapuli SP. Glycoprotein VI-mediated platelet fibrinogen receptor activation occurs through calcium-sensitive and PKC-sensitive pathways without a requirement for secreted ADP. Blood. 2002;99:3228–3234. doi: 10.1182/blood.v99.9.3228. [DOI] [PubMed] [Google Scholar]
- 27.Kondo K, Umemura K. Clinical pharmacokinetics of tirofiban, a nonpeptide glycoprotein IIb/IIIa receptor antagonist: comparison with the monoclonal antibody abciximab. Clin Pharmacokinet. 2002;41:187–195. doi: 10.2165/00003088-200241030-00003. [DOI] [PubMed] [Google Scholar]
- 28.Proimos G. Platelet aggregation inhibition with glycoprotein IIb – IIIa inhibitors. J Thromb Thrombolysis. 2001;11:99–110. doi: 10.1023/a:1011216414539. [DOI] [PubMed] [Google Scholar]
- 29.Zuern CS, Schwab M, Gawaz M, Geisler T. Platelet pharmacogenomics. J Thromb Haemost. 2010 doi: 10.1111/j.1538-7836.2010.03791.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Salles II, Feys HB, Iserbyt BF, De Meyer SF, Vanhoorelbeke K, Deckmyn H. Inherited traits affecting platelet function. Blood Rev. 2008;22:155–172. doi: 10.1016/j.blre.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Marin F, Roldan V, Gonzalez-Conejero R, Corral J. The pharmacogenetics of antiplatelet drugs. Curr Opin Investig Drugs. 2007;8:213–218. [PubMed] [Google Scholar]
- 32.Ouwehand WH. Platelet genomics and the risk of atherothrombosis. J Thromb Haemost. 2007;5 (Suppl 1):188–195. doi: 10.1111/j.1538-7836.2007.02550.x. [DOI] [PubMed] [Google Scholar]
- 33.Khan Y, Faraday N, Herzog W, Shuldiner AR. Genetic determinants of arterial thrombosis. In: Roden D, editor. Cardiovascular genetics and genomics. Blackwell Publishing; 2009. [Google Scholar]
- 34.Feher G, Feher A, Pusch G, Lupkovics G, Szapary L, Papp E. The genetics of antiplatelet drug resistance. Clin Genet. 2009;75:1–18. doi: 10.1111/j.1399-0004.2008.01105.x. [DOI] [PubMed] [Google Scholar]
- 35.Bordeaux BC, Qayyum R, Yanek LR, Vaidya D, Becker LC, Faraday N, Becker DM. Effect of obesity on platelet reactivity and response to low-dose aspirin. Prev Cardiol. 2010;13:56–62. doi: 10.1111/j.1751-7141.2009.00058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grove EL, Hvas AM, Johnsen HL, Hedegaard SS, Pedersen SB, Mortensen J, Kristensen SD. A comparison of platelet function tests and thromboxane metabolites to evaluate aspirin response in healthy individuals and patients with coronary artery disease. Thromb Haemost. 2010;103:1245–1253. doi: 10.1160/TH09-08-0527. [DOI] [PubMed] [Google Scholar]
- 37.Maree AO, Fitzgerald DJ. Variable platelet response to aspirin and clopidogrel in atherothrombotic disease. Circulation. 2007;115:2196–2207. doi: 10.1161/CIRCULATIONAHA.106.675991. [DOI] [PubMed] [Google Scholar]
- 38.Mortensen SB, Larsen SB, Grove EL, Kristensen SD, Hvas AM. Reduced platelet response to aspirin in patients with coronary artery disease and type 2 diabetes mellitus. Thromb Res. 2010 doi: 10.1016/j.thromres.2010.03.013. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 39.De Berardis G, Sacco M, Strippoli GF, Pellegrini F, Graziano G, Tognoni G, Nicolucci A. Aspirin for primary prevention of cardiovascular events in people with diabetes: meta-analysis of randomised controlled trials. BMJ. 2009;339:b4531. doi: 10.1136/bmj.b4531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belch J, MacCuish A, Campbell I, Cobbe S, Taylor R, Prescott R, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840. doi: 10.1136/bmj.a1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ertugrul DT, Tutal E, Yildiz M, Akin O, Yalcin AA, Ure OS, et al. Aspirin resistance is associated with glycemic control, the dose of aspirin, and obesity in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2010;95:2897–2901. doi: 10.1210/jc.2009-2392. [DOI] [PubMed] [Google Scholar]
- 43.Herrera-Galeano JE, Becker DM, Wilson AF, Yanek LR, Bray P, Vaidya D, et al. A novel variant in the platelet endothelial aggregation receptor-1 gene is associated with increased platelet aggregability. Arterioscler Thromb Vasc Biol. 2008;28:1484–1490. doi: 10.1161/ATVBAHA.108.168971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones CI, Bray S, Garner SF, Stephens J, De Bono B, Angenent WG, et al. A functional genomics approach reveals novel quantitative trait loci associated with platelet signaling pathways. Blood. 2009;114:1405–1416. doi: 10.1182/blood-2009-02-202614. [DOI] [PubMed] [Google Scholar]
- 45.Sangkuhl K, Klein TE, Altman RB. Clopidogrel pathway. Pharmacogenet Genomics. 2010;20:463–465. doi: 10.1097/FPC.0b013e3283385420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brandt JT, Close SL, Iturria SJ, Payne CD, Farid NA, Ernest CS, II, et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost. 2007;5:2429–2436. doi: 10.1111/j.1538-7836.2007.02775.x. [DOI] [PubMed] [Google Scholar]
- 47.Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, et al. Cytochrome P-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360:354–362. doi: 10.1056/NEJMoa0809171. [DOI] [PubMed] [Google Scholar]
- 48.Hulot JS, Bura A, Villard E, Azizi M, Remones V, Goyenvalle C, et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood. 2006;108:2244–2247. doi: 10.1182/blood-2006-04-013052. [DOI] [PubMed] [Google Scholar]
- 49.Giusti B, Gori AM, Marcucci R, Saracini C, Sestini I, Paniccia R, et al. Cytochrome P450 2C19 loss-of-function polymorphism, but not CYP3A4 IVS10+ 12G/A and P2Y12 T744C polymorphisms, is associated with response variability to dual antiplatelet treatment in high-risk vascular patients. Pharmacogenet Genomics. 2007;17:1057–1064. doi: 10.1097/FPC.0b013e3282f1b2be. [DOI] [PubMed] [Google Scholar]
- 50.Trenk D, Hochholzer W, Fromm MF, Chialda LE, Pahl A, Valina CM, et al. Cytochrome P450 2C19 681G > A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008;51:1925–1934. doi: 10.1016/j.jacc.2007.12.056. [DOI] [PubMed] [Google Scholar]
- 51.Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Meneveau N, et al. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009;360:363–375. doi: 10.1056/NEJMoa0808227. [DOI] [PubMed] [Google Scholar]
- 52.Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J, et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet. 2009;373:309–317. doi: 10.1016/S0140-6736(08)61845-0. [DOI] [PubMed] [Google Scholar]
- 53.Shuldiner AR, O’Connell JR, Bliden KP, Gandhi A, Ryan K, Horenstein RB, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA. 2009;302:849–857. doi: 10.1001/jama.2009.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sofi F, Giusti B, Marcucci R, Gori AM, Abbate R, Gensini GF. Cytochrome P450 2C19(*)2 polymorphism and cardiovascular recurrences in patients taking clopidogrel: a meta-analysis. Pharmacogenomics J. 2010 doi: 10.1038/tpj.2010.21. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 55.Gurbel PA, Tantry US, Shuldiner AR, Kereiakes DJ. Genotyping: one piece of the puzzle to personalize antiplatelet therapy. J Am Coll Cardiol. 2010;56:112–116. doi: 10.1016/j.jacc.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 56.Damani SB, Topol EJ. The case for routine genotyping in dual-antiplatelet therapy. J Am Coll Cardiol. 2010;56:109–111. doi: 10.1016/j.jacc.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 57.Roden DM, Shuldiner AR. Responding to the clopidogrel warning by the US food and drug administration real life is complicated. Circulation. 2010;122:445–448. doi: 10.1161/CIRCULATIONAHA.110.973362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Holmes DR, Jr, Dehmer GJ, Kaul S, Leifer D, O’Gara PT, Stein CM. ACCF/ AHA Clopidogrel clinical alert: approaches to the FDA ‘boxed warning’: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the American Heart Association. Circulation. 2010;122:537–557. doi: 10.1161/CIR.0b013e3181ee08ed. [DOI] [PubMed] [Google Scholar]
- 59.Sibbing D, Koch W, Gebhard D, Schuster T, Braun S, Stegherr J, et al. Cytochrome 2C19*17 allelic variant, platelet aggregation, bleeding events, and stent thrombosis in clopidogrel-treated patients with coronary stent placement. Circulation. 2010;121:512–518. doi: 10.1161/CIRCULATIONAHA.109.885194. [DOI] [PubMed] [Google Scholar]
- 60.Sibbing D, Gebhard D, Koch W, Braun S, Stegherr J, Morath T, et al. Isolated and interactive impact of common CYP2C19 genetic variants on the antiplatelet effect of chronic clopidogrel therapy. J Thromb Haemost. 2010 doi: 10.1111/j.1538-7836.2010.03921.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 61.Lau WC, Gurbel PA, Watkins PB, Neer CJ, Hopp AS, Carville DG, et al. Contribution of hepatic cytochrome P450 3A4 metabolic activity to the phenomenon of clopidogrel resistance. Circulation. 2004;109:166–171. doi: 10.1161/01.CIR.0000112378.09325.F9. [DOI] [PubMed] [Google Scholar]
- 62.Gladding P, White H, Voss J, Ormiston J, Stewart J, Ruygrok P, et al. Pharmacogenetic testing for clopidogrel using the rapid INFINITI analyzer: a dose-escalation study. J Am Coll Cardiol Cardiovasc Interv. 2009;2:1095–1101. doi: 10.1016/j.jcin.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 63.Harmsze A, Van Werkum JW, Bouman HJ, Ruven HJ, Breet NJ, Ten Berg JM, et al. Besides CYP2C19*2, the variant allele CYP2C9*3 is associated with higher on-clopidogrel platelet reactivity in patients on dual antiplatelet therapy undergoing elective coronary stent implantation. Pharmacogenet Genomics. 2010;20:18–25. doi: 10.1097/FPC.0b013e328333dafe. [DOI] [PubMed] [Google Scholar]
- 64.Taubert D, Von Beckerath N, Grimberg G, Lazar A, Jung N, Goeser T, et al. Impact of P-glycoprotein on clopidogrel absorption. Clin Pharmacol Ther. 2006;80:486–501. doi: 10.1016/j.clpt.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 65.Lev EI, Patel RT, Guthikonda S, Lopez D, Bray PF, Kleiman NS. Genetic polymorphisms of the platelet receptors P2Y(12), P2Y(1) and GP IIIa and response to aspirin and clopidogrel. Thromb Res. 2007;119:355–360. doi: 10.1016/j.thromres.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 66.Sibbing D, Von Beckerath O, Schomig A, Kastrati A, Von Beckerath N. P2Y1 gene A1622G dimorphism is not associated with adenosine diphosphate-induced platelet activation and aggregation after administration of a single high dose of clopidogrel. J Thromb Haemost. 2006;4:912–914. doi: 10.1111/j.1538-7836.2006.01869.x. [DOI] [PubMed] [Google Scholar]
- 67.Ziegler S, Schillinger M, Funk M, Felber K, Exner M, Mlekusch W, et al. Association of a functional polymorphism in the clopidogrel target receptor gene, P2Y12, and the risk for ischemic cerebrovascular events in patients with peripheral artery disease. Stroke. 2005;36:1394–1399. doi: 10.1161/01.STR.0000169922.79281.a5. [DOI] [PubMed] [Google Scholar]
- 68.Von Beckerath N, Von Beckerath O, Koch W, Eichinger M, Schomig A, Kastrati A. P2Y12 gene H2 haplotype is not associated with increased adenosine diphosphate-induced platelet aggregation after initiation of clopidogrel therapy with a high loading dose. Blood Coagul Fibrinolysis. 2005;16:199–204. doi: 10.1097/01.mbc.0000164429.21040.0a. [DOI] [PubMed] [Google Scholar]
- 69.Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Ramirez C, Sabate M, Jimenez-Quevedo P, et al. Influence of aspirin resistance on platelet function profiles in patients on long-term aspirin and clopidogrel after percutaneous coronary intervention. Am J Cardiol. 2006;97:38–43. doi: 10.1016/j.amjcard.2005.07.106. [DOI] [PubMed] [Google Scholar]
- 70.Smith SM, Judge HM, Peters G, Armstrong M, Fontana P, Gaussem P, et al. Common sequence variations in the P2Y12 and CYP3A5 genes do not explain the variability in the inhibitory effects of clopidogrel therapy. Platelets. 2006;17:250–258. doi: 10.1080/09537100500475844. [DOI] [PubMed] [Google Scholar]
- 71.Cuisset T, Frere C, Quilici J, Morange PE, Saut N, Lambert M, et al. Role of the T744C polymorphism of the P2Y12 gene on platelet response to a 600-mg loading dose of clopidogrel in 597 patients with non-ST-segment elevation acute coronary syndrome. Thromb Res. 2007;120:893–899. doi: 10.1016/j.thromres.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 72.Staritz P, Kurz K, Stoll M, Giannitsis E, Katus HA, Ivandic BT. Platelet reactivity and clopidogrel resistance are associated with the H2 haplotype of the P2Y12-ADP receptor gene. Int J Cardiol. 2009;133:341–345. doi: 10.1016/j.ijcard.2007.12.118. [DOI] [PubMed] [Google Scholar]
- 73.Rudez G, Bouman HJ, Van Werkum JW, Leebeek FW, Kruit A, Ruven HJ, et al. Common variation in the platelet receptor P2RY12 gene is associated with residual on-clopidogrel platelet reactivity in patients undergoing elective percutaneous coronary interventions. Circ Cardiovasc Genet. 2009;2:515–521. doi: 10.1161/CIRCGENETICS.109.861799. [DOI] [PubMed] [Google Scholar]
- 74.Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Alfonso F, Sabate M, Fernandez C, et al. PlA polymorphism and platelet reactivity following clopidogrel loading dose in patients undergoing coronary stent implantation. Blood Coagul Fibrinolysis. 2004;15:89–93. doi: 10.1097/00001721-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 75.Motovska Z, Widimsky P, Kvasnicka J, Petr R, Bilkova D, Hajkova J, et al. High loading dose of clopidogrel is unable to satisfactorily inhibit platelet reactivity in patients with glycoprotein IIIA gene polymorphism: a genetic substudy of PRAGUE-8 trial. Blood Coagul Fibrinolysis. 2009;20:257–262. doi: 10.1097/mbc.0b013e328325455b. [DOI] [PubMed] [Google Scholar]
- 76.Combescure C, Fontana P, Mallouk N, Berdague P, Labruyere C, Barazer I, et al. Clinical implications of clopidogrel non-response in cardiovascular patients: a systematic review and meta-analysis. J Thromb Haemost. 2010;8:923–933. doi: 10.1111/j.1538-7836.2010.03809.x. [DOI] [PubMed] [Google Scholar]
- 77.Breet NJ, Van Werkum JW, Bouman HJ, Kelder JC, Ruven HJ, Bal ET, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010;303:754–762. doi: 10.1001/jama.2010.181. [DOI] [PubMed] [Google Scholar]
- 78.Geisler T, Grass D, Bigalke B, Stellos K, Drosch T, Dietz K, et al. The residual platelet aggregation after deployment of intracoronary stent (PREDICT) score. J Thromb Haemost. 2008;6:54–61. doi: 10.1111/j.1538-7836.2007.02812.x. [DOI] [PubMed] [Google Scholar]
- 79.Bonello-Palot N, Armero S, Paganelli F, Mancini J, De Labriolle A, Bonello C, et al. Relation of body mass index to high on-treatment platelet reactivity and of failed clopidogrel dose adjustment according to platelet reactivity monitoring in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2009;104:1511–1515. doi: 10.1016/j.amjcard.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 80.Bliden KP, Dichiara J, Lawal L, Singla A, Antonino MJ, Baker BA, et al. The association of cigarette smoking with enhanced platelet inhibition by clopidogrel. J Am Coll Cardiol. 2008;52:531–533. doi: 10.1016/j.jacc.2008.04.045. [DOI] [PubMed] [Google Scholar]
- 81.Jeong YH, Cho JH, Kang MK, Koh JS, Kim IS, Park Y, et al. Smoking at least 10 cigarettes per day increases platelet inhibition by clopidogrel in patients with ST-segment-elevation myocardial infarction. Thromb Res. 2010 doi: 10.1016/j.thromres.2010.03.020. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 82.Michelson AD, Furman MI, Goldschmidt-Clermont P, Mascelli MA, Hendrix C, Coleman L, et al. Platelet GP IIIa Pl(A) polymorphisms display different sensitivities to agonists. Circulation. 2000;101:1013–1018. doi: 10.1161/01.cir.101.9.1013. [DOI] [PubMed] [Google Scholar]
- 83.Wheeler GL, Braden GA, Bray PF, Marciniak SJ, Mascelli MA, Sane DC. Reduced inhibition by abciximab in platelets with the PlA2 polymorphism. Am Heart J. 2002;143:76–82. doi: 10.1067/mhj.2002.119763. [DOI] [PubMed] [Google Scholar]
- 84.Sirotkina OV, Khaspekova SG, Zabotina AM, Shimanova YV, Mazurov AV. Effects of platelet glycoprotein IIb-IIIa number and glycoprotein IIIa Leu33Pro polymorphism on platelet aggregation and sensitivity to glycoprotein IIb-IIIa antagonists. Platelets. 2007;18:506–514. doi: 10.1080/09537100701326739. [DOI] [PubMed] [Google Scholar]
- 85.Weber AA, Jacobs C, Meila D, Weber S, Zotz RB, Scharf RE, et al. No evidence for an influence of the human platelet antigen-1 polymorphism on the antiplatelet effects of glycoprotein IIb/IIIa inhibitors. Pharmacogenetics. 2002;12:581–583. doi: 10.1097/00008571-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 86.Schrör K, Weber AA. Comparative pharmacology of GP IIb/IIIa antagonists. J Thromb Thrombolysis. 2003;15:71–80. doi: 10.1023/b:thro.0000003308.63022.8d. [DOI] [PubMed] [Google Scholar]