Abstract
Endothelin (ET) is one of the most investigated molecules in vascular biology. Since its discovery two decades ago, several ET isoforms, receptors, signaling pathways, agonists and antagonists have been identified. ET functions as a potent endothelium-derived vasoconstrictor, but could also play a role in vascular relaxation. In endothelial cells, preproET and big ET are cleaved by ET converting enzymes into ET-1, −2, −3 and −4. These ET isoforms bind with different affinities to ETA and ETB receptors in vascular smooth muscle (VSM), and in turn increase [Ca2+]i, protein kinase C and mitogen-activated protein kinase and other signaling pathways of VSM contraction and cell proliferation. ET also binds to endothelial ETB receptors and stimulates the release of nitric oxide, prostacyclin and endothelium-derived hyperpolarizing factor. ET, via endothelial ETB receptor, could also promote ET re-uptake and clearance. While the effects of ET on vascular reactivity and growth have been thoroughly examined, its role in the regulation of blood pressure and the pathogenesis of hypertension is not clearly established. Elevated plasma and vascular tissue levels of ET have been identified in salt-sensitive hypertension and in moderate to severe hypertension, and ET receptor antagonists have been shown to reduce blood pressure to variable extents in these forms of hypertension. The development of new pharmacological and genetic tools could lead to more effective and specific modulators of the vascular ET system for treatment of hypertension and related cardiovascular disease.
Keywords: endothelium, nitric oxide, smooth muscle, calcium, blood pressure
INTRODUCTION
The endothelium is an integral component of the vascular wall and a major regulator of vascular reactivity and blood pressure. The endothelium releases vasodilator factors such as nitric oxide (NO), prostacyclin (PGI2) and endothelium-derived hyperpolarizing factors (EDHFs) [1–4]. A decrease in the release of endothelium-derived vasodilators reduces vascular relaxation and consequently increases vascular resistance and blood pressure and leads to hypertension (HTN). The endothelium also releases vasoconstrictor factors such as thromboxane A2, angiotensin II (AngII) and endothelin (ET), one of the most potent vasoconstrictors described [5]. Since its discovery in 1988, several ET isoforms and ET receptor subtypes have been identified in the kidney and blood vessels and have been shown to affect sodium balance and vascular function [5–8]. While the prominent effects of ET on renal sodium absorption and vasoconstriction are expected to increase blood pressure, the role of ET and its receptors in the pathogenesis of HTN has not been clearly defined. Importantly, the plasma and vascular tissue levels of ET are elevated in some but not all forms of experimental and human HTN [9,10]. ET receptor antagonists may decrease blood pressure in experimental HTN [11]. Also some studies have demonstrated significant antihypertensive activity of ET antagonists such as bosentan in essential HTN [12], highlighting the importance of studying the effects of modulators of the ET system in the regulation of blood pressure and in HTN.
This review will discuss reports published in the PubMed database to provide insight into the role of ET and vascular ET receptors in the regulation of vascular function and blood pressure, and how alterations in their expression and signaling mechanisms could lead to HTN. The review will first describe the various ET isoforms, their plasma and vascular tissue levels and the various pathways involved in their synthesis and metabolism. The ET receptor subtypes, their vascular tissue distribution and signaling pathways will then be described. We will finally discuss the pathophysiological changes in ET metabolism and function in specific forms of experimental HTN and the potential use of ET receptor antagonists in the management of human HTN.
ET Synthesis, Metabolism and Clearance
The ET peptide family includes the 21-amino acid peptides ET-1, −2, −3, and −4, and several 31-amino acid forms. ET-1 is mainly released from the endothelium and acts in an autocrine or paracrine fashion on ET receptors in endothelial cells and vascular smooth muscle (VSM) to stimulate vascular contraction and cell growth [13]. ET-1 is also produced by airway epithelial cells, cardiomyocytes, fibroblasts, neurons and macrophages [14]. ET-2 is produced by intestinal epithelial cells. ET-3 is produced by intestinal epithelial cells, renal tubular epithelial cells and neurons. ET-4 is produced by the intestinal, lung and renal epithelial cells [15,16].
In endothelial cells, ET synthesis is initiated from preproET gene transcription (Fig. 1), which can be regulated by c-fos, c-jun, nuclear factor-1, AP-1 and GATA-2 [17]. The translation of preproET mRNA produces long 203-amino acid proteins called preproETs. PreproETs are then cleaved by furin-like protease to biologically inactive 37- to 41-amino acid big ETs. Big ET-1 and big ET-2 are cleaved at Trp21-Val22 by ET converting enzyme-1 (ECE-1) and ECE-2 to produce ET-11–21 and ET-21–21, respectively. Mast cell chymases could also cleave big ET-1 and big ET-2 at Tyr31-Gly32 to produce ET-11–31 and ET-21–31, respectively. Big ET-3 is cleaved at Trp21-lle22 by ECE-1, −2 and −3 to produce ET-31–21, and at Gly31-Leu32 by chymases to form ET-31–31 [13].
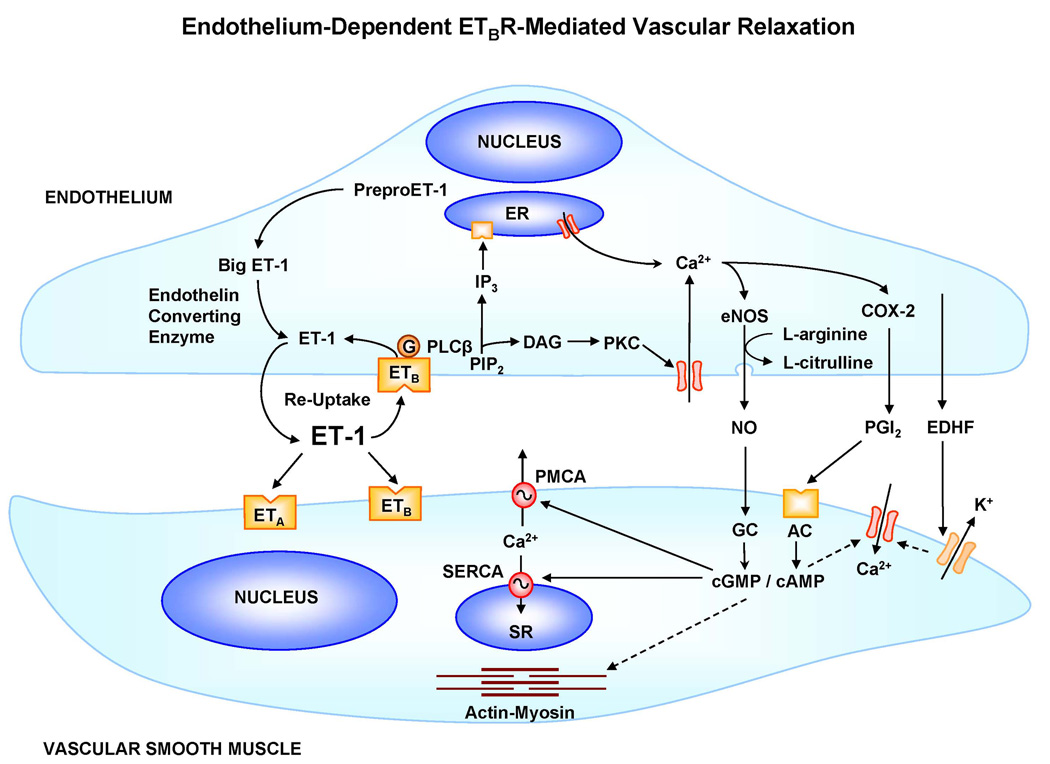
Fig. 1.
Endothelium-dependent ETBR-mediated pathways of vascular relaxation. ET binds to ETBR in endothelial cells to stimulate ET re-uptake and clearance. ETBR also activates PLCβ and increases the hydrolysis of PIP2 into IP3 and diacylglycerol (DAG). IP3 induces Ca2+ release from the endoplasmic reticulum (ER). The increased [Ca2+]i activates eNOS, which in turn converts L-arginine to L-citrulline and increases NO production. NO diffuses into VSM, where it stimulates guanylate cyclase (GC) and increases cGMP production. cGMP decreases VSM [Ca2+]i by decreasing Ca2+ entry via Ca2+ channels and increasing Ca2+ removal via plasmalemmal (PMCA) and sarcoplasmic reticulum Ca2+ ATPase (SERCA). cGMP also decreases the actin-myosin myofilament force sensitivity to Ca2+ and thereby causes vascular relaxation. Endothelial ETBR is also coupled to stimulation of cyclooxygenases (COX-2) and increased prostacyclin (PGI2) production. PGI2 activates adenylate cyclase (AC) and increases the production of cAMP, which causes VSM relaxation by mechanisms similar to those of cGMP. Activation of endothelial ETBR is also associated with increased release of EDHF, which activates K+ channels and causes hyperpolarization and relaxation of VSM. Dashed arrows indicate inhibition.
ECEs are members of the metalloprotease family. ECE-1 is produced by many cells including endothelial cells, has peak activity at neutral pH, and is processed both intracellularly and on the cell surface. ECE-1 expression is regulated by protein kinase C (PKC), ETB receptor, ets-1 transcription factor, and cytokines. The specificity of ECE-1 may provide a target to alter ET-1 production in certain cardiovascular disease such as HTN [18]. ECE-2 is produced by several cells including neurons and has peak activity at pH 5.8, suggesting intracellular processing. ECE-1 and ECE-2 show preference for big ET-1 over big ET-2 and big ET-3. Interestingly, ECE-1 and ECE-2 deficient mice have high levels of mature ET peptides, suggesting that ECE-3 or another unidentified enzyme may carry out the final processing step of ET [13,19].
Regulation of the ET system takes place mainly at the gene transcription level. PreproET-1 mRNA is upregulated during cardiovascular stress and in response to vasopressors and vasoactive agents such as AngII, norepinephrine, vasopressin, and thrombin as well as inflammatory cytokines such as tumor necrosis factor-α, interleukins and transforming growth factor-β [8,20,21]. PreproET-1 mRNA expression is upregulated by hypocapnia, and may be downregulated by hypoxia [22]. In endothelial cells, PreproET-1 mRNA expression initially increases then decreases by mechanical shear stress [23]. On the other hand, NO, PGI2 and atrial natriuretic factor decrease PreproET-1 mRNA expression and ET-1 release from endothelial cells [24,25]. The synthesized ET-1 is stored in elongated Weibel-Palade bodies in endothelial cells. During endothelial cell activation, the Weibel-Palade bodies relocate from the cytoplasm towards the plasma membrane and release ET-1 by exocytosis [26].
The plasma and vascular tissue levels of ET-1 are very low. In healthy adults, plasma ET-1 levels range between 0.7 and 5 pg/mL [27]. In normal Wistar rats, plasma ET-1 levels range between 0.7 and 4.9 fmol/mL [28]. In isolated aorta of Sprague-Dawley rats, ET levels are 120 pg/g tissue [29]. The low plasma/vascular tissue levels of ET could be due to its continuous metabolism/clearance. In normal adults, the 24-hour urinary ET excretion show marked variability between 1.7 pg/mL and 6.8 ng/mL [30,31]. In the kidney, neutral endopeptidase restricts ET-1 turnover, and endopeptidase inhibitors increase urinary ET levels [32,33]. ET clearance may also be achieved by its reuptake by certain endothelial ETB receptors (ETBR) called “clearance receptors” (Fig. 1) [32].
ET Receptors
ET receptors include ETAR and ETBR. ETAR and ETBR are widely expressed in numerous tissues including the kidney and blood vessels [8,32,34,35]. ETAR mediates vasoconstriction and VSM cell proliferation, whereas ETBR is involved in endothelial cell survival, ET re-uptake and clearance, and release of NO and PGI2 (Fig. 1), as well as the inhibition of ECE-1. Pharmacological studies suggest the presence of two ETBR subtypes in endothelial cells and VSM; however, there is no molecular evidence to support this sub-classification. ETAR and ETBR are encoded by distinct genes located on chromosomes 4 and 13, respectively, and the receptors share 63% amino acid identity [9]. In Western blot analysis of vascular tissues ETAR is detected as a prominent immunoreactive band at 59 kDa, and less dense bands at 44 and 32 kDa. ETBR is often detected as two immunoreactive bands at 64 and 44 kDa.
ETAR is expressed in VSM of most blood vessels (Table 1), and in airway smooth muscle, cardiomyocytes, liver stellate cells, hepatocytes, neurons, osteoblasts, melanocytes, keratinocytes, adipocytes and the reproductive system [8,20,32]. In VSM, ETAR is upregulated by insulin and NO [36,37]. While ETBR predominates in endothelial cells, it is also present in VSM of some vascular beds [38,39] (Table 1). ETBR has been identified in the aorta, coronary arteries, mesenteric arteries, and veins of experimental animals and in human mammary arteries [40,41]. ETBR is also present in the brainstem glia and neurons, atrial and ventricular myocardium and the atrioventricular conducting tissue [38,42]. ETBR have also been localized in renal tubules and collecting duct epithelial cells, airway smooth muscle, liver hepatocytes, osteoblasts, central and peripheral neurons, multiple endocrine tissues and the reproductive tract [32,42]. In endothelial cells, ETBR is upregulated by tumor necrosis factor-α and basic fibroblast growth factor [32]. Both ETAR and ETBR are widely distributed in blood vessels, the nervous systems, and the renal arterioles, glomerular capillaries and inner medullary collecting ducts [34,43]. Immunohistochemical analyses have identified ETAR and ETBR in the plasmalemma and cytosol of several cell types. ETBR has also been identified in the nuclear envelope and nucleoplasm [44] (Table 1).
Table 1.
Examples of endothelin receptor distribution, function, and signaling pathways in the vascular system
| ETAR | Endothelial ETBR | VSM ETBR | |
|---|---|---|---|
| Molecular Weight | Mainly 59 kDa | 64/44 kDa | 64/44 kDa |
| Vascular Distribution | |||
| Coronary Artery | + | + | |
| Subcutaneous Arteries | + | + | + |
| Pulmonary Artery | + | + | + |
| Mammary Artery | + | + | + |
| Veins | + | + | + |
| Glomerular Capillaries | + | + | + |
| Cellular Distribution | |||
| Endothelial Cells | + | ||
| VSM | + | + | |
| Sub-Cellular Distribution | |||
| Cytosol / Plasmalemma | + | + | + |
| Nucleus | + | ||
| Function | VSM Contraction | VSM Relaxation | VSM Contraction |
| Vasoconstriction | Vasodilatation | Vasoconstriction | |
| VSM Growth | |||
| Vascular Remodeling | |||
| Signaling Pathways | - Heterotrimeric G Protein | - G Protein | - G Protein |
| - PLCβ, PLD | - Increased [Ca2+]i | - PLCβ, PLD | |
| - Increased [Ca2+]i | - NO | - Increased [Ca2+]i | |
| - PKC | - PGI2 | - PKC | |
| - MAPK | - EDHF | - MAPK | |
ET Receptor-Mediated Signaling
ET-1 administration in experimental animals in vivo is associated with a transient vasodilator and blood pressure depressor response [5], and these effects are likely due to activation of endothelial ETBR. In endothelial cells, ETBR is coupled to activation of signaling pathways that increase the release of relaxing factors such as NO, PGI2 and EDHF (Fig. 1). NO and NO donors may inhibit ET-1 release or counteract its renal effects and vasoconstrictor effects on VSM [6]. This may explain why in vivo administration of NOS inhibitors such as L-NAME could enhance ET-1 release from endothelial cells. ETBR may also be involved in the release of other endothelium-derived vasodilators such as PGI2 and EDHF [45–47] (Fig. 1).
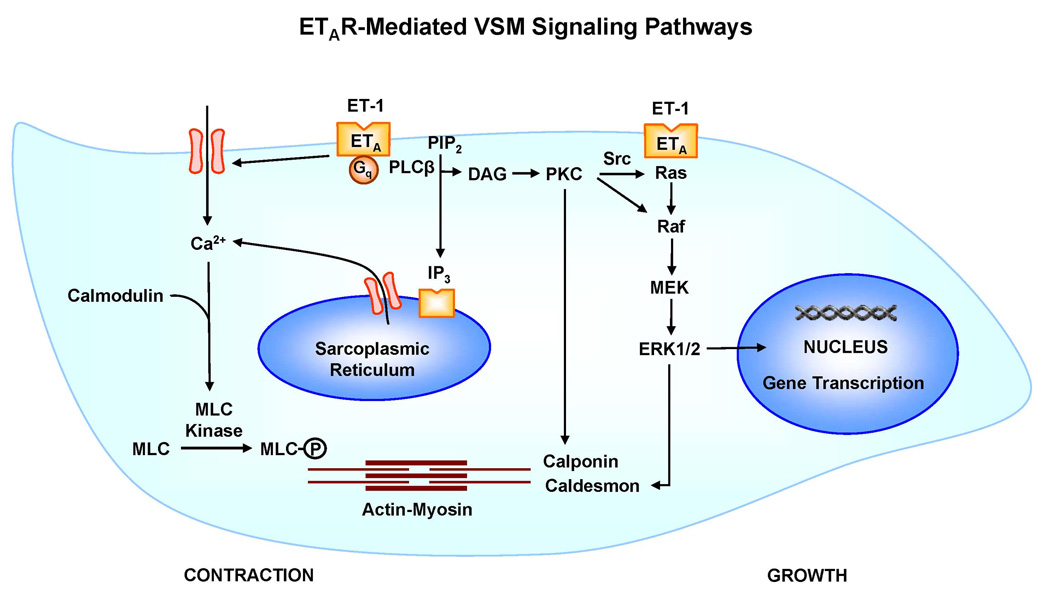
In VSM, ETAR is coupled to Gq/11 protein to activate phospholiphase C-β (PLC-β), resulting in the breakdown of phosphatidylinositol 4,5-bisphosphate and the generation of inositol 1,4,5-trisphosphate (IP3) and diacylglycerol [48] (Fig. 2). IP3 stimulates Ca2+ release from the intracellular Ca2+ stores in the sarcoplasmic reticulum. ET also stimulates Ca2+ influx from the extracellular space through plasmalemmal Ca2+ channels [49,50]. The ET/ETAR-induced increase in diacylglycerol stimulates PKC activity [51–53]. Other ETAR-mediated signaling pathways include phospholipase D with generation of diacylglycerol, phospholipase A2 with release of arachidonic acid, the Na+/H+ exchanger, Src-family tyrosine kinases, phosphatidylinositol 3-kinase (PI3K), mitogen-activated protein kinase (MAPK), p38 MAPK, and c-Jun-NH2-terminal kinase (JNK) [9,20,32,54].
Fig. 2.
ETAR-mediated pathways of VSM contraction and growth. The interaction of ET with ETAR in VSM leads to activation of PLCβ and increased production of IP3 and DAG. IP3 stimulates Ca2+ release from the sarcoplasmic reticulum. ET also stimulates Ca2+ entry from the extracellular space through Ca2+ channels. Ca2+ binds calmodulin to form a complex, which causes activation of myosin light chain (MLC) kinase, increased MLC phosphorylation, actin-myosin interaction and VSM contraction. DAG activates PKC, which could phosphorylate the actin binding protein calponin or initiate a protein kinase cascade involving Raf, MAPK kinase (MEK) and MAPK (ERK1/2), leading to phosphorylation of the actin-binding protein caldesmon and thereby increases the myofilament force sensitivity to Ca2+. ETAR-mediated activation of MAPK could also induce gene transcription and VSM growth and proliferation.
ET/ET Receptors-Mediated Responses
ET-mediated cellular responses are dependent on both the ET agonist and the ET receptor subtype. ET-1 activates ETAR in VSM and produces strong vasoconstriction, as well as proinflammatory, fibrosis and mitogenic effects, which could play a role in vascular injury and remodeling [32] (Fig. 2). ET-1, −2 and −3 could also enhance vascular contraction by activating ETBR in VSM [55]. Activation of both ETAR and ETBR in the renal vasculature could promote renal vasoconstriction and increase [Ca2+]i signaling in preglomerular VSM cells [56]. Also, the use of selective ET receptor agonists and antagonists have suggested the presence of small number of the vasoconstrictor ETBR in human subcutaneous and rat mesenteric and pulmonary arteries, and therefore ETBR agonists could elicit vasoconstriction in vivo and ETBR-mediated contraction in isolated blood vessels [57,58].
Recent studies suggest an equally important role for endothelial ETBR in the regulation of vascular tone, sodium balance and blood pressure [5]. ET-1 may produce vasodilatation via activation of endothelial ETBR and enhanced eNOS activity and NO release [6] (Fig. 1). Activation of endothelial ETBR could also produce blood pressure depressor effects via the release of PGI2 in rabbit systemic vessels [45] and enhance vascular relaxation by releasing EDHF in rat mesenteric artery [46]. The role of ETBR in the regulation of blood pressure is supported by the observation that ETBR heterozygous (+/−) mice are hypertensive, possibly due to unbalanced activation of ETAR by endogenous ET-1 [59]. The vascular ETBR may also promote favorable inhibitory effects on vascular remodeling after injury [60]. ETBR are also abundant in tubular epithelium and the renal medulla and ET-1 induced activation of ETBR may inhibit sodium and water reabsorption [6,34]. Also, big ET-1 increases medullary blood flow in rats on a high salt diet consistent with a potential ETBR-mediated natriuretic response to high salt intake, and a role for ET in regulating sodium excretion through activation of ETBR [61].
ETBR may also function as “clearance receptors” (Fig. 1). Studies have shown that the ETBR selective antagonist BQ788 inhibits accumulation of intravenously administered radiolabeled ET-1 in the lungs and kidneys possibly by slowing its clearance from the circulation [32]. ETBR deficient rats demonstrate increased plasma ET-1 levels and ETAR expression, but decreased ET-1/ETAR-mediated contraction in mesenteric arteries. This is likely due to desensitization and uncoupling of the ETAR due to the high levels of circulating ET-1 [55].
Modulators of ET Receptors
ET Receptor Agonists
ETAR and ETBR have different ligand specificity (Table 2) as well as affinity. ETAR has subnanomolar affinity for ET-1 and ET-2 and markedly lower affinity for ET-3. ETBR has equal subnanomolar affinities for ET-1, −2 and −3 [32]. The chymase-derived peptide ET-1(1–31) is a relatively selective agonist of ETAR [62].
Table 2.
Examples of ET Receptor Agonists and Antagonists and Their Selectivity to ET Receptor Subtypes
| Compound | Chemistry | Receptor Specificity |
|---|---|---|
| Agonists | ||
| ET1 | Cys-Ser-Cys-Ser-Ser-Leu-Met-Asp-Lys-Glu-Cys-Val-Tyr-Phe- Cys-His-Leu-Asp-Ile-Ile-Trp | ETA, ETB |
| ET2 | ETA, ETB | |
| ET3 | ETB | |
| IRL 1620 | Suc-Asp-Glu-Glu-Ala-Val-Tyr-Phe-Ala-His-Leu-Asp-Ile-Ile-Trp | ETB |
| S6c | Cys-Thr-Cys-Asn-Asp-Met-Thr-Asp-Glu-Glu-Cys-Leu-Asn-Phe- Cys-His-Gln-Asp-Val-Ile-Trp | ETB |
| Antagonists | ||
| A127722 | 2-(4-methoxyphenyl)-4-(1,3-benzodioxol-5-yl)-1-(((dibutyl amino)carbonyl) methyl)pyrrolidine-3-carboxylic acid | ETA |
| ABT627 | (2R,3R,4S)-1-[(dibutyl carbamoyl)methyl]-2-(p-methoxyphenyl)- 4[3,4-(methylenedioxy)phenyl]-3-pyrrolidinecarboxylic acid | ETA |
| Ambrisentan | (2S)-2-[(4,6-dimethylpyrimidin-2-yl)oxy]-3-methoxy- 3,3- diphenylpropanoic acid | ETA |
| BMS182874 | 5-(dimethylamino)-N-(3,4-dimethyl-5-isoxazolyl)-1- naphthalenesulfonamide | ETA |
| Bosentan | 4-t-butyl-N-(6-(2-hydroxyethoxy)-5-(2-methoxyphenoxy)-2,2’- bipyrimidin-4-yl)benzenesulfonamide | ETA, ETB |
| BQ123 | Cyclo(D-α-aspartyl-L-prolyl-D-valyl-L-leucyl-D-tryptophyl) | ETA |
| BQ610 | Homopiperidinyl-CO-Leu-D-Trp(CHO)-D-Trp-OH | ETA |
| BQ788 | N-cis-2,6-dimethylpiperidinocarbonyl-γ-methylleucyl- tryptophyl(COOMe)-norleucine | ETB |
| LU135252 | 2-(4,6-dimethoxypyrimidin-2-yloxy)-3-methoxy-3,3- diphenylpropionic acid | ETA |
| PD142893 | Ac-D-(3,3-diphenylalanine)-leu-Asp-Ile-Ile-Trp-OH | ETA, ETB |
| PD145065 | Ac-D-(5H–dibenzo[a,d]cycloheptene-5-glycine)-Leu-Asp-Ile-Ile- Trp-OH | ETA, ETB |
| PD147953 (FR139317) | N-(N-(N-((hexahydro-1H–azepin-1-yl)carbonyl)-L-leucyl)-1- methyl-D-tryptophyl)-3-(2-pyridinyl)-2-((1-(hexahydro-1H- azepinyl)carbonyl)amino-4-methyl-pentanoyl)-3-(-(1-methyl-1H-indolyl)propionyl)amino-3-(2-pyridyl)propionic acid | ETA |
| PD156707 | Sodium 2-benzo[1,3]dioxol-5-yl-4-(4-methoxy-phenyl)-4-oxo-3- (3,4,5-trimethoxy-benzyl)-but-2-enoate | ETA |
| RES701-1 | L-Tryptophan, glycyl-L-asparaginyl-L-tryptophyl-L-histidylglycyl- L-threonyl-L-alanyl-L-prolyl-L-α-aspartyl-L-tryptophyl-L- phenylalanyl-L-phenylalanyl-L-asparaginyl-L- tyrosyl-L-tyrosyl-, cyclic (9-1)-peptide | ETB |
| SB209670 | 3-(2-(carboxymethoxy)-4-methoxyphenyl)-1-(3,4-(methylene dioxy)phenyl)-5-(prop-1-yloxy)indan-2-carboxylic acid | ETA, ETB |
| TAK044 | cyclo(D-alpha-aspartyl-3-((4-phenylpiperazin-1-yl)carbonyl)-L- alanyl-L-alpha-aspartyl-D-2-(2-thienyl)glycyl-L-leucyl-D- tryptophyl) disodium salt | ETA, ETB |
| YM598 | (E)-N-[6-methoxy-5-(2-methoxyphenoxy)[2,2’-bipyrimidin]-4-yl]- 2-phenylethenesulfonamide monopotassium salt | ETA |
ETBR agonists such as sarafotoxin 6c (S6c) induce small contraction in resistance vessels isolated from human subcutaneous fat and rat mesentery. S6c–induced contraction remains is not affected by ETAR antagonists such as BQ610, and is slightly enhanced in the presence of the NOS inhibitor L-NAME and in endothelium-denuded vessels. These findings support that the vasoconstrictor ETBR may partly contribute to the ET-mediated constriction in resistance vessels of human subcutaneous fat and in rat mesentery. In contrast, in isolated mouse vessels treated with L-NAME, S6c induces a minimal <5% contraction, suggesting a little role of ETBR in the vasoconstriction of mouse vessels [63]. ET-3 has high affinity for ETBR.
ET Receptor Antagonists
Several ET receptor antagonists have been used to examine the role of ET receptor in the control of vascular function and other systems (Table 2). ABT627, BQ123, and BQ610 are more selective toward ETAR [64]. BQ123 and BQ610 inhibit ET-1 induced contraction in the mouse abdominal aorta, rat mesenteric vessels, and human subcutaneous vessels [38,63]. ETBR antagonists such as A192621 and BQ788 have also been developed (Table 2). We have found that chronic treatment of rats with the ETBR antagonist A192621 is associated with substantial increase in blood pressure, enhanced aortic contraction, and reduced endothelium-dependent aortic relaxation and NO production. The vasoconstrictive effects of A192621 were greater in rats on a high salt diet compared to those on normal salt diet, suggesting that endothelial ETBR could influence basal vascular tone particularly during high salt diet [65].
Role of ET in Hypertension
The prominent and long-acting vasoconstrictor effects of ET-1 have suggested that it may play a role in the regulation of blood pressure and the pathophysiology of HTN. Although increased plasma levels of ET-1 have been demonstrated in some hypertensive patients, most patients with HTN show normal or slightly increased ET-1 levels [38]. Among African-Americans, plasma ET levels are increased in hypertensive compared with normotensive controls. On the other hand, among individuals with similar severity of HTN plasma ET levels are not higher in African-Americans compared with Caucasians [57]. Upregulation of the ET system is more commonly observed in severe cases of HTN associated with coronary artery disease, heart failure, atherosclerosis and pulmonary HTN. For example, plasma levels of ET-1 (5.15 pg/mL) and big ET-1 (25.7 pg/mL) are markedly elevated in patients with heart failure compared with control subjects (0.75 pg/mL and 7.7 pg/mL, respectively) [31].
The discrepancy in the plasma ET levels among hypertensive patients may be related to the rapid ET-1 clearance from the bloodstream. Also, ET is mainly secreted in a polarized from the endothelial cells to the underling VSM, leading to minimal increases in circulating plasma ET. Measurement of ET levels in vascular tissues may provide a more reliable tool to determine the role of ET in HTN. For example, ET-1 mRNA expression is increased in the endothelium of subcutaneous resistance arteries from patients with moderate to severe HTN [38]. ET-1 tissue expression is also increased in other forms of human HTN including salt-sensitive HTN, low renin HTN, and obesity and insulin resistance-related HTN [66].
It is important to note that the tissue levels of ET-1 also show variability in animal models of HTN. ET-1 levels are elevated in the aortic wall of deoxycorticosterone acetate (DOCA)-salt hypertensive rats (730 pg/g) compared to control rats (120 pg/g) [29]. Also, the tissue levels of ET are markedly higher than the plasma levels, supporting the contention that ET tissue levels could be a better indicator of changes in the vascular ET system in HTN. ET-1 levels are also increased in the vascular wall of other salt-sensitive models of HTN such as DOCA-salt-treated spontaneously hypertensive rats (SHR) and salt-loaded stroke-prone SHR, Dahl salt-sensitive rats, AngII-infused rats and 1-kidney 1-clip Goldblatt hypertensive rats. In contrast, ET-1 vascular tissue levels are not increased in SHR, 2-kidney 1-clip hypertensive rats or L-NAME-treated rats [67].
The levels of ET in urine also show marked changes in HTN. For example, the 24 hour urinary excretion of ET-1 is markedly greater in hypertensive patients with heart failure (17.0 ng/g urinary creatinine or UC) as compared to control subjects (1.7 ng/g UC) [31].
ET Receptor-Mediated Responses in HTN
Both ETAR, which mediate vasoconstriction, and ETBR, which mediate vasodilation, could play a role in the regulation of blood pressure. An increase in the amount/activity of ETAR or a decrease in the amount/activity of ETBR is expected to cause an increase in blood pressure and HTN. However, the relationship between ETAR and ETBR in HTN is rather complex.
The number of vascular ET receptors could vary in different forms of HTN, and in various tissues isolated from subjects with the same form of HTN. For example, ETBR are upregulated in the kidneys of DOCA-salt hypertensive rats, consistent with a role for ETBR in the renal regulation of blood pressure [68]. ET receptors could also be downregulated by ET when a large amount of ET is produced in the vasculature. For instance, in DOCA-salt hypertensive rats the ET receptor density is reduced in some vascular beds, possibly due to increased vascular production of ET and consequent downregulation of ET receptors [69].
The variability in the ET system in HTN may not only involve the plasma and vascular tissue levels of ET and the amount of vascular ET receptors, but could also involve the vascular response to ET. Studies have shown that ET-1 induced contraction is increased in the coronaries of rat hearts during ischemia/reperfusion [70], and in the pulmonary artery of rat models of pulmonary HTN [71,72]. The augmented vascular reactivity to ET-1 in some forms of experimental HTN may be related to increased intracellular free Ca2+ concentration ([Ca2+]i) in VSM [56,73]. In contrast, ET-induced contraction is not enhanced in the aorta of SHR. ET-induced contraction is even decreased in the mesenteric arteries of DOCA-salt hypertensive rats and in ETBR deficient rats possibly due to reduced ETAR density as a result of its downregulation by the increased vascular ET production or decreased ETBR-mediated ET-1 clearance [55,69].
In milder forms of HTN, the VSM of resistance arteries are restructured around a smaller lumen without true hypertrophy, resulting in reduced circumference and amplification of pressor stimuli. An example of this structurally based amplification is the enhanced vasoconstriction in isolated microvessels of SHR and renovascular hypertensive rats [38]. In severe forms of HTN and in secondary HTN, hypertrophic remodeling of VSM occurs [66]. Large conduit artery such as the aorta may demonstrate thickened tunica media, increased collagen deposition and decreased compliance, leading to increased systolic blood pressure and pulse pressure. Because of the ET growth-promoting properties, it could play a role in the hypertrophy of VSM observed in severe HTN and in DOCA-salt hypertensive rats [38].
The responsiveness of endothelial ETBR may also change in HTN. ETBR-mediated vasorelaxation is greater in SHR and DOCA-salt hypertensive rats than normotensive rats. Thus while ETAR may play a role in the development of DOCA-salt–induced HTN, ETBR may protect against vascular and renal injury [74]. However, ET may decrease the release of endothelium-derived relaxing factor and thereby further enhance vasoconstriction in blood vessels of SHR [38]
ET Receptor Antagonists and Management of HTN
Because the effects of ET on vasoconstriction and VSM growth are mediated primarily via ETAR, it is often thought that treatment with ETAR antagonists would decrease blood pressure. However, the effects of ETAR antagonists on blood pressure vary in normotensive and hypertensive animals. In normotensive rats, chronic administration of ETAR antagonist does not affect blood pressure, suggesting that ET may not be involved in the regulation of normal blood pressure [75]. Also, some studies have shown that chronic treatment with the ETAR antagonist A127722 or BQ123 only slightly lowers blood pressure in SHR and DOCA-salt hypertensive rats, and has no effect in renovascular model of HTN, suggesting that ET plays little role in these forms of HTN [57,76]. Other studies have shown that acute administration of the selective ETAR antagonist ABT-627 markedly decreases blood pressure in DOCA-salt rats, and chronic treatment with ABT-627 suppresses the development of HTN [74]. Also, chronic treatment with the nonselective ETA/ETB antagonist bosentan decreases the development of HTN and vascular remodeling in DOCA-salt rats to a degree similar to that observed with ABT-627, suggesting that ETAR plays a major role in DOCA-salt-sensitive HTN [74]. The net benefits of ET receptor antagonists in HTN could depend in their effectiveness to suppress the vasoconstrictive and growth promoting effects of ET. For instance, in hypertensive rats overexpressing ET-1, selective ETAR antagonists lower blood pressure slightly, but markedly attenuate vascular hypertrophy, particularly in resistance arteries [67]. Similarly, treatment of SHR and DOCA-salt hypertensive rats with the nonselective ETA/B receptor antagonist bosentan reduces the blood pressure, but abolishes the vascular hypertrophy and remodeling of resistance arteries beyond what could be explained by the blood pressure lowering effect [38].
Clinical trials in humans have shown that non-selective ET receptor antagonists such as bosentan and combined treatment with ETAR/ETBR antagonists significantly reduce blood pressure [12,66]. In a study involving mild cases of essential hypertensive patients, a 4-week trial of bosentan reduced blood pressure to the same extent as the angiotensin converting enzyme (ACE) inhibitor enalapril. Also, some studies have suggested that treatment with ET receptor antagonists may improve hemodynamics in hypertensive patients with chronic heart failure (CHF) [77,78]. ET-1 plasma levels are elevated in CHF, correlate with both hemodynamic severity and symptoms, and are strong independent predictors of mortality in CHF. Combined ETAR/ETBR antagonists and selective ETAR antagonists have been evaluated in patients with CHF showing considerable hemodynamic improvements, suggesting that ET receptor antagonists may have the potential to improve hemodynamics, symptoms, and prognosis in patients with CHF [77,78]. Despite these potential benefits and favorable short term effects on hemodynamics as suggested by some clinical trials, ET receptor antagonists have not been adopted for clinical management of CHF. ET receptor antagonists may also offer promise in primary pulmonary HTN [67]. For example, bosentan and ambrisentan have been shown to be effective in increasing 6 minute walk distance (6MWD) and exercise improvements and reducing symptoms in idiopathic pulmonary HTN [79,80]. Examination of both the short-term and long-term beneficial effects of ET antagonists in HTN is also needed. The ET antagonist blood pressure lowering effects that might be modest in magnitude in the short-term could have significant long-term consequences. In pulmonary HTN, for example, it has been reported that the magnitude of improvement with ambrisentan, an orally active highly selective ETAR antagonist with >4000-fold higher selectivity over ETBR, was relatively small in the short-term, but could be meaningful as one-year survival was improved [81]. Thus, targeting the ET system using ET receptor antagonists may not only decrease blood pressure in HTN, but could also prevent target organ damage and other cardiovascular complications associated with HTN such as heart failure, atherosclerosis, coronary heart disease, restenosis after angioplasty and primary pulmonary HTN [67].
ET and Other Control Mechanisms of Blood Pressure
Despite the well-recognized effects of ET on vasoconstriction and remodeling, its effects on blood pressure have not been consistent. Some studies have shown that ET infusion increases blood pressure in rats [82], while other studies have shown slight or no effect [49]. The difference in the results could be related to differences in the activity of the ET from different commercial sources and rapid metabolism of administered ET. Also, the ETAR- mediated vasoconstriction could be counterbalanced by ETBR-mediated increase in endothelium-derived vasodilators. The relative number of ETAR and ETBR could also vary in different vascular beds due to developmental differences in ET receptor expression. This is particularly evident in the pulmonary circulation. For example, studies in fetal sheep in utero have shown that ETAR activation may have a small role in maintaining basal fetal pulmonary vascular tone, while ETBR activation produces marked pulmonary vasodilation [83]. ET could also affect other vascular, neuronal and renal control mechanisms of blood pressure. Likewise, the pressor effects of ET could be influenced by other factors such as the endothelial NO pathway, oxidative stress, the sympathetic nervous system, dietary salt intake, and the renin-angiotensin system.
NO plays a major role in the regulation of vascular function, and inhibition of NO production causes elevation of blood pressure in experimental animals. Interestingly, in rats chronically treated with NOS inhibitors such as L-NAME, ETAR antagonists attenuate the early but not the late stages of HTN [75]. It has been suggested that ET may play a role in the development of early vascular lesions associated with NOS inhibition, at least within the kidney, possibly due to increased AngII activity. However, the mechanisms of the HTN associated with chronic NOS inhibition may be more complex and could vary with the animal species studied and the NOS inhibitor utilized [63].
Vascular oxidative stress is increased in parallel with the elevation of plasma ET levels in DOCA-salt hypertensive rats. Also, treatment of DOCA-salt hypertensive rats with ETAR antagonist is associated with reduction in oxidative stress and reactive oxygen species. Oxidative stress is known to affect numerous vascular signaling pathways and several responses in the cardiovascular system including endothelial cell function and VSM growth. Thus the cardiovascular changes observed in DOCA-salt HTN could be partly due to increases in oxidative stress as a result of increased ET-1 expression/actions in this model [84].
High-salt diet intensifies the increase in blood pressure in salt-dependent hypertensive subjects. Salt-sensitive HTN is often associated with low plasma renin activity and elevated plasma levels of ET and catecholamines, suggesting synergistic effects between the sympathetic system, sodium sensitivity and the ET system in the elevation of blood pressure [60]. Decreased endothelial NO production may also contribute to the development of salt-dependent HTN [85]. High salt diet is also associated with increased ET production, which in turn stimulates both ETAR-mediated vasoconstriction and ETBR-mediated vasodilation. In one study, chronic ETBR blockade was associated with increased blood pressure in rats on normal salt diet, and the HTN was markedly enhanced in rats on a high-salt diet [65]. These findings are consistent with a role for ET-1 in regulating blood pressure particularly during high dietary salt intake [68].
The renin-angiotensin system is a major control mechanism in the regulation of blood pressure. Some of the effects of AngII such as VSM growth are mediated by ET-1 and ETAR. Also, the stimulatory effects of AngII on ET production are more apparent in the blood vessels of SHR than normotensive rats [38].
Conclusions and Future Directions
The vascular ET system is an important modulator of vascular tone, growth, and the vascular control mechanisms of blood pressure. Although some studies suggest that ET infusion may cause elevation of blood pressure in some experimental animals, ET infusion does not always increase blood pressure, and not all animal models of HTN have high ET levels. ET appears to play a role in the elevation of blood pressure and vascular growth in moderate-to-severe HTN, salt-sensitive HTN, and in African-American subjects.
HTN is usually treated with diuretics, β-adrenergic blockers, ACE inhibitors, AngII receptor antagonists and long-acting Ca2+ channel blockers. However, in HTN the protracted increases in blood pressure are associated with progressive endothelial cell damage and consequent increases in ET-1 expression in blood vessels and the heart. ET in turn causes further elevation of blood pressure and promotes the progression of vascular and cardiac damage. Blocking the ET system may provide another approach to lower the blood pressure and to suppress the vascular and cardiac damage associated with HTN, and thereby improve the prognosis in hypertensive subjects. Currently available ET receptor antagonists reduce blood pressure in some forms of experimental HTN (Table 2). The effects of ET receptor antagonists in blunting vascular growth and endothelial dysfunction and in reducing the cardiovascular complications of HTN such as heart failure and stroke need to be further examined in clinical trials [67]. Since the final step of the biosynthesis of ET is catalyzed by ECEs, inhibitors of these enzymes may represent alternative therapeutic agents in HTN [18]. Another alternative way to modulate the ET system is to take a genetic approach and knock-out a specific ET isoform, ECE isozyme or ET receptor subtype. While the genetic approach has shown promising results in modulating cardiovascular disease in experimental animals, it remains to be validated in humans [57].
Finally, although the vascular ET system may play an important role in the vascular control mechanisms of blood pressure and the pathogenesis of some forms of HTN, the role of ET on the neuronal, hormonal and renal control mechanisms of the blood pressure should not be minimized. Also, HTN is a complex multifactorial disease that could involve abnormalities in several systems including ET, and modulating the ET system alone may not cure HTN. A multidisciplinary approach targeting the vascular ET system and the other neuronal, hormonal and renal pressor mechanisms should prove most effective in the management of HTN and associated cardiovascular disorders.
ACKNOWLEDGEMENTS
This work was supported by grants from National Heart, Lung, and Blood Institute (HL-65998, HL-70659, and HL-98724) and The Eunice Kennedy Shriver National Institute of Child Health and Human Development (HD-60702).
List of abbreviations
- AngII
angiotensin II
- [Ca2+]i
intracellular free Ca2+ concentration
- DOCA
deoxycorticosterone acetate
- ECE
endothelin converting enzyme
- ET-1
endothelin-1
- ETAR
endothelin receptor A
- ETBR
endothelin receptor B
- HTN
hypertension
- MAPK
mitogen-activated protein kinase
- MLC
myosin light chain
- NO
nitric oxide
- PGI2
prostacyclin
- PKC
protein kinase C
- S6c
sarafotoxin 6c
- SHR
spontaneously hypertensive rat
- VSM
vascular smooth muscle
REFERENCES
- 1.Napoli C, Ignarro LJ. Nitric oxide and pathogenic mechanisms involved in the development of vascular diseases. Arch Pharm Res. 2009;32(8):1103–1108. doi: 10.1007/s12272-009-1801-1. [DOI] [PubMed] [Google Scholar]
- 2.Fleming I, Busse R. NO: the primary EDRF. J Mol Cell Cardiol. 1999;31(1):5–14. doi: 10.1006/jmcc.1998.0839. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell JA, Ali F, Bailey L, Moreno L, Harrington LS. Role of nitric oxide and prostacyclin as vasoactive hormones released by the endothelium. Exp Physiol. 2008;93(1):141–147. doi: 10.1113/expphysiol.2007.038588. [DOI] [PubMed] [Google Scholar]
- 4.Feletou M, Vanhoutte PM. Endothelium-derived hyperpolarizing factor: where are we now? Arterioscler Thromb Vasc Biol. 2006;26(6):1215–1225. doi: 10.1161/01.ATV.0000217611.81085.c5. [DOI] [PubMed] [Google Scholar]
- 5.Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature. 1988;332(6163):411–415. doi: 10.1038/332411a0. [DOI] [PubMed] [Google Scholar]
- 6.Pollock JS, Pollock DM. Endothelin and NOS1/nitric oxide signaling and regulation of sodium homeostasis. Curr Opin Nephrol Hypertens. 2008;17(1):70–75. doi: 10.1097/MNH.0b013e3282f34b02. [DOI] [PubMed] [Google Scholar]
- 7.Granger JP, Abram S, Stec D, Chandler D, LaMarca B. Endothelin, the kidney, and hypertension. Curr Hypertens Rep. 2006;8(4):298–303. doi: 10.1007/s11906-006-0068-x. [DOI] [PubMed] [Google Scholar]
- 8.Hynynen MM, Khalil RA. The vascular endothelin system in hypertension--recent patents and discoveries. Recent Pat Cardiovasc Drug Discov. 2006;1(1):95–108. doi: 10.2174/157489006775244263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiffrin EL. Vascular endothelin in hypertension. Vascul Pharmacol. 2005;43(1):19–29. doi: 10.1016/j.vph.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Pollock DM. Renal endothelin in hypertension. Curr Opin Nephrol Hypertens. 2000;9(2):157–164. doi: 10.1097/00041552-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Dhaun N, Pollock DM, Goddard J, Webb DJ. Selective and mixed endothelin receptor antagonism in cardiovascular disease. Trends Pharmacol Sci. 2007;28(11):573–579. doi: 10.1016/j.tips.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Krum H, Viskoper RJ, Lacourciere Y, Budde M, Charlon V. The effect of an endothelin-receptor antagonist, bosentan, on blood pressure in patients with essential hypertension. Bosentan Hypertension Investigators. N Engl J Med. 1998;338(12):784–790. doi: 10.1056/NEJM199803193381202. [DOI] [PubMed] [Google Scholar]
- 13.Luscher TF, Barton M. Endothelins and endothelin receptor antagonists: therapeutic considerations for a novel class of cardiovascular drugs. Circulation. 2000;102(19):2434–2440. doi: 10.1161/01.cir.102.19.2434. [DOI] [PubMed] [Google Scholar]
- 14.Rubanyi GM, Botelho LH. Endothelins. FASEB J. 1991;5(12):2713–2720. doi: 10.1096/fasebj.5.12.1916094. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto H, Suzuki N, Onda H, Fujino M. Abundance of endothelin-3 in rat intestine, pituitary gland and brain. Biochem Biophys Res Commun. 1989;164(1):74–80. doi: 10.1016/0006-291x(89)91684-7. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham ME, Huribal M, Bala RJ, McMillen MA. Endothelin-1 and endothelin-4 stimulate monocyte production of cytokines. Crit Care Med. 1997;25(6):958–964. doi: 10.1097/00003246-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Kawana M, Lee ME, Quertermous EE, Quertermous T. Cooperative interaction of GATA-2 and AP1 regulates transcription of the endothelin-1 gene. Mol Cell Biol. 1995;15(8):4225–4231. doi: 10.1128/mcb.15.8.4225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeng AY, Mulder P, Kwan AL, Battistini B. Nonpeptidic endothelin-converting enzyme inhibitors and their potential therapeutic applications. Can J Physiol Pharmacol. 2002;80(5):440–449. doi: 10.1139/y02-025. [DOI] [PubMed] [Google Scholar]
- 19.Yanagisawa H, Hammer RE, Richardson JA, Emoto N, Williams SC, Takeda S, Clouthier DE, Yanagisawa M. Disruption of ECE-1 and ECE-2 reveals a role for endothelin-converting enzyme-2 in murine cardiac development. J Clin Invest. 2000;105(10):1373–1382. doi: 10.1172/JCI7447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schiffrin EL, Touyz RM. Vascular biology of endothelin. J Cardiovasc Pharmacol. 1998;32 Suppl 3:S2–S13. [PubMed] [Google Scholar]
- 21.Emori T, Hirata Y, Imai T, Ohta K, Kanno K, Eguchi S, Marumo F. Cellular mechanism of thrombin on endothelin-1 biosynthesis and release in bovine endothelial cell. Biochem Pharmacol. 1992;44(12):2409–2411. doi: 10.1016/0006-2952(92)90687-e. [DOI] [PubMed] [Google Scholar]
- 22.Yoshimoto S, Ishizaki Y, Sasaki T, Murota S. Effect of carbon dioxide and oxygen on endothelin production by cultured porcine cerebral endothelial cells. Stroke. 1991;22(3):378–383. doi: 10.1161/01.str.22.3.378. [DOI] [PubMed] [Google Scholar]
- 23.Malek AM, Zhang J, Jiang J, Alper SL, Izumo S. Endothelin-1 gene suppression by shear stress: pharmacological evaluation of the role of tyrosine kinase, intracellular calcium, cytoskeleton, and mechanosensitive channels. J Mol Cell Cardiol. 1999;31(2):387–399. doi: 10.1006/jmcc.1998.0873. [DOI] [PubMed] [Google Scholar]
- 24.Boulanger C, Luscher TF. Release of endothelin from the porcine aorta. Inhibition by endothelium-derived nitric oxide. J Clin Invest. 1990;85(2):587–590. doi: 10.1172/JCI114477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kohno M, Yokokawa K, Horio T, Yasunari K, Murakawa K, Takeda T. Atrial and brain natriuretic peptides inhibit the endothelin-1 secretory response to angiotensin II in porcine aorta. Circ Res. 1992;70(2):241–247. doi: 10.1161/01.res.70.2.241. [DOI] [PubMed] [Google Scholar]
- 26.van Mourik JA, Romani de Wit T, Voorberg J. Biogenesis and exocytosis of Weibel-Palade bodies. Histochem Cell Biol. 2002;117(2):113–122. doi: 10.1007/s00418-001-0368-9. [DOI] [PubMed] [Google Scholar]
- 27.Shichiri M, Hirata Y, Ando K, Emori T, Ohta K, Kimoto S, Ogura M, Inoue A, Marumo F. Plasma endothelin levels in hypertension and chronic renal failure. Hypertension. 1990;15(5):493–496. doi: 10.1161/01.hyp.15.5.493. [DOI] [PubMed] [Google Scholar]
- 28.Abdel-Sayed S, Brunner HR, Nussberger J. Volume expansion enhances plasma endothelin-1. Am J Hypertens. 2003;16(12):1057–1061. doi: 10.1016/s0895-7061(03)01031-8. [DOI] [PubMed] [Google Scholar]
- 29.Zhao H, Joshua IG, Porter JP. Microvascular responses to endothelin in deoxycorticosterone acetate-salt hypertensive rats. Am J Hypertens. 2000;13(7):819–826. doi: 10.1016/s0895-7061(00)00260-0. [DOI] [PubMed] [Google Scholar]
- 30.Cantaro S, Milan Manani S, Marcon R, Bonfante L, Masiero M, D'Angelo A, Calo L. Urinary excretion of vasoactive substances in chronic renal failure. Clin Nephrol. 2001;55(5):393–399. [PubMed] [Google Scholar]
- 31.Modesti PA, Cecioni I, Costoli A, Poggesi L, Galanti G, Serneri GG. Renal endothelin in heart failure and its relation to sodium excretion. Am Heart J. 2000;140(4):617–622. doi: 10.1067/mhj.2000.109917. [DOI] [PubMed] [Google Scholar]
- 32.Kedzierski RM, Yanagisawa M. Endothelin system: the double-edged sword in health and disease. Annu Rev Pharmacol Toxicol. 2001;41:851–876. doi: 10.1146/annurev.pharmtox.41.1.851. [DOI] [PubMed] [Google Scholar]
- 33.Abassi ZA, Tate JE, Golomb E, Keiser HR. Role of neutral endopeptidase in the metabolism of endothelin. Hypertension. 1992;20(1):89–95. doi: 10.1161/01.hyp.20.1.89. [DOI] [PubMed] [Google Scholar]
- 34.Ponnuchamy B, Khalil RA. Cellular mediators of renal vascular dysfunction in hypertension. Am J Physiol Regul Integr Comp Physiol. 2009;296(4):R1001–R1018. doi: 10.1152/ajpregu.90960.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ohuchi T, Yanagisawa M, Gariepy CE. Renal tubular effects of endothelin-B receptor signaling: its role in cardiovascular homeostasis and extracellular volume regulation. Curr Opin Nephrol Hypertens. 2000;9(4):435–439. doi: 10.1097/00041552-200007000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Hopfner RL, Hasnadka RV, Wilson TW, McNeill JR, Gopalakrishnan V. Insulin increases endothelin-1-evoked intracellular free calcium responses by increased ET(A) receptor expression in rat aortic smooth muscle cells. Diabetes. 1998;47(6):937–944. doi: 10.2337/diabetes.47.6.937. [DOI] [PubMed] [Google Scholar]
- 37.Redmond EM, Cahill PA, Hodges R, Zhang S, Sitzmann JV. Regulation of endothelin receptors by nitric oxide in cultured rat vascular smooth muscle cells. J Cell Physiol. 1996;166(3):469–479. doi: 10.1002/(SICI)1097-4652(199603)166:3<469::AID-JCP1>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 38.Schiffrin EL. Endothelin: potential role in hypertension and vascular hypertrophy. Hypertension. 1995;25(6):1135–1143. doi: 10.1161/01.hyp.25.6.1135. [DOI] [PubMed] [Google Scholar]
- 39.Schneider MP, Boesen EI, Pollock DM. Contrasting actions of endothelin ET(A) and ET(B) receptors in cardiovascular disease. Annu Rev Pharmacol Toxicol. 2007;47:731–759. doi: 10.1146/annurev.pharmtox.47.120505.105134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watts SW. Endothelin receptors: what's new and what do we need to know? Am J Physiol Regul Integr Comp Physiol. 298(2):R254–R260. doi: 10.1152/ajpregu.00584.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tykocki NR, Gariepy CE, Watts SW. Endothelin ET(B) receptors in arteries and veins: multiple actions in the vein. J Pharmacol Exp Ther. 2009;329(3):875–881. doi: 10.1124/jpet.108.145953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gariepy CE, Ohuchi T, Williams SC, Richardson JA, Yanagisawa M. Salt-sensitive hypertension in endothelin-B receptor-deficient rats. J Clin Invest. 2000;105(7):925–933. doi: 10.1172/JCI8609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tostes RC, Touyz RM, He G, Chen X, Schiffrin EL. Contribution of endothelin-1 to renal activator protein-1 activation and macrophage infiltration in aldosterone-induced hypertension. Clin Sci (Lond) 2002;103 Suppl 48:25S–30S. doi: 10.1042/CS103S025S. [DOI] [PubMed] [Google Scholar]
- 44.Bkaily G, Choufani S, Sader S, Jacques D, d’Orleans-Juste P, Nader M, Kurban G, Kamal M. Activation of sarcolemma and nuclear membranes ET-1 receptors regulates transcellular calcium levels in heart and vascular smooth muscle cells. Can J Physiol Pharmacol. 2003;81(6):654–662. doi: 10.1139/y03-020. [DOI] [PubMed] [Google Scholar]
- 45.McMurdo L, Thiemermann C, Vane JR. The endothelin ETB receptor agonist, IRL 1620, causes vasodilatation and inhibits ex vivo platelet aggregation in the anaesthetised rabbit. Eur J Pharmacol. 1994;259(1):51–55. doi: 10.1016/0014-2999(94)90156-2. [DOI] [PubMed] [Google Scholar]
- 46.Nakashima M, Vanhoutte PM. Endothelin-1 and −3 cause endothelium-dependent hyperpolarization in the rat mesenteric artery. Am J Physiol. 1993;265(6 Pt 2):H2137–H2141. doi: 10.1152/ajpheart.1993.265.6.H2137. [DOI] [PubMed] [Google Scholar]
- 47.Tirapelli CR, Casolari DA, Yogi A, Montezano AC, Tostes RC, Legros E, D’Orleans-Juste P, de Oliveira AM. Functional characterization and expression of endothelin receptors in rat carotid artery: involvement of nitric oxide, a vasodilator prostanoid and the opening of K+ channels in ETB-induced relaxation. Br J Pharmacol. 2005;146(6):903–912. doi: 10.1038/sj.bjp.0706388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neylon CB. Vascular biology of endothelin signal transduction. Clin Exp Pharmacol Physiol. 1999;26(2):149–153. doi: 10.1046/j.1440-1681.1999.03013.x. [DOI] [PubMed] [Google Scholar]
- 49.Smith L, Payne JA, Sedeek MH, Granger JP, Khalil RA. Endothelin-induced increases in Ca2+ entry mechanisms of vascular contraction are enhanced during high-salt diet. Hypertension. 2003;41(3 Pt 2):787–793. doi: 10.1161/01.HYP.0000051643.05700.56. [DOI] [PubMed] [Google Scholar]
- 50.Chew DK, Orshal JM, Khalil RA. Elastase-induced suppression of endothelin-mediated Ca2+ entry mechanisms of vascular contraction. Hypertension. 2003;42(4):818–824. doi: 10.1161/01.HYP.0000086200.93184.8E. [DOI] [PubMed] [Google Scholar]
- 51.McNair LL, Salamanca DA, Khalil RA. Endothelin-1 promotes Ca2+ antagonist-insensitive coronary smooth muscle contraction via activation of epsilon-protein kinase C. Hypertension. 2004;43(4):897–904. doi: 10.1161/01.HYP.0000118520.92686.3b. [DOI] [PubMed] [Google Scholar]
- 52.Sirous ZN, Fleming JB, Khalil RA. Endothelin-1 enhances eicosanoids-induced coronary smooth muscle contraction by activating specific protein kinase C isoforms. Hypertension. 2001;37(2 Part 2):497–504. doi: 10.1161/01.hyp.37.2.497. [DOI] [PubMed] [Google Scholar]
- 53.Kanashiro CA, Altirkawi KA, Khalil RA. Preconditioning of coronary artery against vasoconstriction by endothelin-1 and prostaglandin F2alpha during repeated downregulation of epsilon-protein kinase C. J Cardiovasc Pharmacol. 2000;35(3):491–501. doi: 10.1097/00005344-200003000-00021. [DOI] [PubMed] [Google Scholar]
- 54.Cain AE, Tanner DM, Khalil RA. Endothelin-1--induced enhancement of coronary smooth muscle contraction via MAPK-dependent and MAPK-independent [Ca(2+)](i) sensitization pathways. Hypertension. 2002;39(2 Pt 2):543–549. doi: 10.1161/hy0202.103129. [DOI] [PubMed] [Google Scholar]
- 55.Perry MG, Molero MM, Giulumian AD, Katakam PV, Pollock JS, Pollock DM, Fuchs LC. ET(B) receptor-deficient rats exhibit reduced contraction to ET-1 despite an increase in ET(A) receptors. Am J Physiol Heart Circ Physiol. 2001;281(6):H2680–H2686. doi: 10.1152/ajpheart.2001.281.6.H2680. [DOI] [PubMed] [Google Scholar]
- 56.Schroeder AC, Imig JD, LeBlanc EA, Pham BT, Pollock DM, Inscho EW. Endothelin-mediated calcium signaling in preglomerular smooth muscle cells. Hypertension. 2000;35(1 Pt 2):280–286. doi: 10.1161/01.hyp.35.1.280. [DOI] [PubMed] [Google Scholar]
- 57.Schiffrin EL. Role of endothelin-1 in hypertension and vascular disease. Am J Hypertens. 2001;14(6 Pt 2):83S–89S. doi: 10.1016/s0895-7061(01)02074-x. [DOI] [PubMed] [Google Scholar]
- 58.McCulloch KM, MacLean MR. EndothelinB receptor-mediated contraction of human and rat pulmonary resistance arteries and the effect of pulmonary hypertension on endothelin responses in the rat. J Cardiovasc Pharmacol. 1995;26 Suppl 3:S169–S176. [PubMed] [Google Scholar]
- 59.Berthiaume N, Yanagisawa M, D’Orleans-Juste P. Contribution of endogenous endothelin-1 and endothelin-A-receptors to the hypertensive state of endothelin-B heterozygous (+/−) knockout mice. J Cardiovasc Pharmacol. 2000;36(5 Suppl 1):S72–S74. [PubMed] [Google Scholar]
- 60.Murakoshi N, Miyauchi T, Kakinuma Y, Ohuchi T, Goto K, Yanagisawa M, Yamaguchi I. Vascular endothelin-B receptor system in vivo plays a favorable inhibitory role in vascular remodeling after injury revealed by endothelin-B receptor-knockout mice. Circulation. 2002;106(15):1991–1998. doi: 10.1161/01.cir.0000032004.56585.2a. [DOI] [PubMed] [Google Scholar]
- 61.Vassileva I, Mountain C, Pollock DM. Functional role of ETB receptors in the renal medulla. Hypertension. 2003;41(6):1359–1363. doi: 10.1161/01.HYP.0000070958.39174.7E. [DOI] [PubMed] [Google Scholar]
- 62.Maguire JJ, Kuc RE, Davenport AP. Vasoconstrictor activity of novel endothelin peptide, ET-1(1 – 31), in human mammary and coronary arteries in vitro. Br J Pharmacol. 2001;134(6):1360–1366. doi: 10.1038/sj.bjp.0704384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou Y, Dirksen WP, Zweier JL, Periasamy M. Endothelin-1-induced responses in isolated mouse vessels: the expression and function of receptor types. Am J Physiol Heart Circ Physiol. 2004;287(2):H573–H578. doi: 10.1152/ajpheart.01170.2003. [DOI] [PubMed] [Google Scholar]
- 64.Watts SW, Fink GD, Northcott CA, Galligan JJ. Endothelin-1-induced venous contraction is maintained in DOCA-salt hypertension; studies with receptor agonists. Br J Pharmacol. 2002;137(1):69–79. doi: 10.1038/sj.bjp.0704831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Giardina JB, Green GM, Rinewalt AN, Granger JP, Khalil RA. Role of endothelin B receptors in enhancing endothelium-dependent nitric oxide-mediated vascular relaxation during high salt diet. Hypertension. 2001;37(2 Part 2):516–523. doi: 10.1161/01.hyp.37.2.516. [DOI] [PubMed] [Google Scholar]
- 66.Touyz RM, Schiffrin EL. Role of endothelin in human hypertension. Can J Physiol Pharmacol. 2003;81(6):533–541. doi: 10.1139/y03-009. [DOI] [PubMed] [Google Scholar]
- 67.Schiffrin EL. Endothelin and endothelin antagonists in hypertension. J Hypertens. 1998;16(12 Pt 2):1891–1895. doi: 10.1097/00004872-199816121-00007. [DOI] [PubMed] [Google Scholar]
- 68.Pollock DM, Pollock JS. Evidence for endothelin involvement in the response to high salt. Am J Physiol Renal Physiol. 2001;281(1):F144–F150. doi: 10.1152/ajprenal.2001.281.1.F144. [DOI] [PubMed] [Google Scholar]
- 69.Nguyen PV, Parent A, Deng LY, Fluckiger JP, Thibault G, Schiffrin EL. Endothelin vascular receptors and responses in deoxycorticosterone acetate-salt hypertensive rats. Hypertension. 1992;19(2 Suppl) doi: 10.1161/01.hyp.19.2_suppl.ii98. II98-104. [DOI] [PubMed] [Google Scholar]
- 70.de Groot MC, Illing B, Horn M, Urban B, Haase A, Schnackerz K, Neubauer S. Endothelin-1 increases susceptibility of isolated rat hearts to ischemia/reperfusion injury by reducing coronary flow. J Mol Cell Cardiol. 1998;30(12):2657–2668. doi: 10.1006/jmcc.1998.0822. [DOI] [PubMed] [Google Scholar]
- 71.Barman SA. Vasoconstrictor effect of endothelin-1 on hypertensive pulmonary arterial smooth muscle involves Rho-kinase and protein kinase C. Am J Physiol Lung Cell Mol Physiol. 2007;293(2):L472–L479. doi: 10.1152/ajplung.00101.2006. [DOI] [PubMed] [Google Scholar]
- 72.McCulloch KM, Docherty C, MacLean MR. Endothelin receptors mediating contraction of rat and human pulmonary resistance arteries: effect of chronic hypoxia in the rat. Br J Pharmacol. 1998;123(8):1621–1630. doi: 10.1038/sj.bjp.0701785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tostes RC, Wilde DW, Bendhack LM, Webb RC. Calcium handling by vascular myocytes in hypertension. Braz J Med Biol Res. 1997;30(3):315–323. doi: 10.1590/s0100-879x1997000300004. [DOI] [PubMed] [Google Scholar]
- 74.Matsumura Y, Hashimoto N, Taira S, Kuro T, Kitano R, Ohkita M, Opgenorth TJ, Takaoka M. Different contributions of endothelin-A and endothelin-B receptors in the pathogenesis of deoxycorticosterone acetate-salt-induced hypertension in rats. Hypertension. 1999;33(2):759–765. doi: 10.1161/01.hyp.33.2.759. [DOI] [PubMed] [Google Scholar]
- 75.Pollock DM. Chronic studies on the interaction between nitric oxide and endothelin in cardiovascular and renal function. Clin Exp Pharmacol Physiol. 1999;26(3):258–261. doi: 10.1046/j.1440-1681.1999.03027.x. [DOI] [PubMed] [Google Scholar]
- 76.Larouche I, Schiffrin EL. Cardiac microvasculature in DOCA-salt hypertensive rats : effect of endothelin ET(A) receptor antagonism. Hypertension. 1999;34(4 Pt 2):795–801. doi: 10.1161/01.hyp.34.4.795. [DOI] [PubMed] [Google Scholar]
- 77.Luscher TF, Enseleit F, Pacher R, Mitrovic V, Schulze MR, Willenbrock R, Dietz R, Rousson V, Hurlimann D, Philipp S, Notter T, Noll G, Ruschitzka F. Hemodynamic and neurohumoral effects of selective endothelin A (ET(A)) receptor blockade in chronic heart failure: the Heart Failure ET(A) Receptor Blockade Trial (HEAT) Circulation. 2002;106(21):2666–2672. doi: 10.1161/01.cir.0000038497.80095.e1. [DOI] [PubMed] [Google Scholar]
- 78.Hurlimann D, Enseleit F, Noll G, Luscher TF, Ruschitzka F. Endothelin antagonists and heart failure. Curr Hypertens Rep. 2002;4(1):85–92. doi: 10.1007/s11906-002-0058-6. [DOI] [PubMed] [Google Scholar]
- 79.Jacobs W, Boonstra A, Brand M, Rosenberg DM, Schaaf B, Postmus PE, Vonk Noordegraaf A. Long-term outcomes in pulmonary arterial hypertension in the first-line epoprostenol or first-line bosentan era. J Heart Lung Transplant. 29(10):1150–1158. doi: 10.1016/j.healun.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 80.Blalock SE, Matulevicius S, Mitchell LC, Reimold S, Warner J, Peshock R, Torres F, Chin KM. Long-term outcomes with ambrisentan monotherapy in pulmonary arterial hypertension. J Card Fail. 16(2):121–127. doi: 10.1016/j.cardfail.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Croxtall JD, Keam SJ. Ambrisentan. Drugs. 2008;68(15):2195–2204. doi: 10.2165/00003495-200868150-00008. [DOI] [PubMed] [Google Scholar]
- 82.Mortensen LH, Fink GD. Captopril prevents chronic hypertension produced by infusion of endothelin-1 in rats. Hypertension. 1992;19(6 Pt 2):676–680. doi: 10.1161/01.hyp.19.6.676. [DOI] [PubMed] [Google Scholar]
- 83.Wong J, Fineman JR, Heymann MA. The role of endothelin and endothelin receptor subtypes in regulation of fetal pulmonary vascular tone. Pediatr Res. 1994;35(6):664–670. doi: 10.1203/00006450-199406000-00008. [DOI] [PubMed] [Google Scholar]
- 84.Callera GE, Touyz RM, Teixeira SA, Muscara MN, Carvalho MH, Fortes ZB, Nigro D, Schiffrin EL, Tostes RC. ETA receptor blockade decreases vascular superoxide generation in DOCA-salt hypertension. Hypertension. 2003;42(4):811–817. doi: 10.1161/01.HYP.0000088363.65943.6C. [DOI] [PubMed] [Google Scholar]
- 85.Sullivan JC, Pollock DM, Pollock JS. Altered nitric oxide synthase 3 distribution in mesenteric arteries of hypertensive rats. Hypertension. 2002;39(2 Pt 2):597–602. doi: 10.1161/hy0202.103286. [DOI] [PubMed] [Google Scholar]