This study was conducted to determine if lysis of bowel adhesions has a role in the surgical management of adhesions for treating complex abdominal and pelvic pain syndrome.
Keywords: Adhesions, Laparoscopy, Abdominal pain, Pelvic pain
Abstract
Abdominal pains secondary to adhesions are a common complaint, but most surgeons do not perform surgery for this complaint unless the patient suffers from a bowel obstruction. The purpose of this evaluation was to determine if lysis of bowel adhesions has a role in the surgical management of adhesions for helping treat abdominal pain. The database of our patients with complex abdominal and pelvic pain syndrome (CAPPS) was reviewed to identify patients who underwent a laparoscopic lysis of adhesion without any organ removal and observe if they had a decrease in the amount of abdominal pain after this procedure. Thirty-one patients completed follow-up at 3, 6, 9, and 12 months. At 6, 9, and 12 months postoperation, there were statistically significant decreases in patients' analog pain scores. We concluded that laparoscopic lysis of adhesions can help decrease adhesion-related pain. The pain from adhesions may involve a more complex pathway toward pain resolution than a simple cutting of scar tissue, such as “phantom pain” following amputation, which takes time to resolve after this type of surgery.
INTRODUCTION
The surgical treatment of abdominal adhesions for chronic abdominal pain is a topic that has garnered significant attention. Surgeons, gynecologists, urologists, primary care doctors, psychiatrists, and physical therapists, all work with patients who present with similar complaints of chronic pain but without a definitive test or imaging to support such claims. Complex abdominal and pelvic pain syndrome (CAPPS) is an old disease process that often leads patients through an exhaustive course of tests and studies without a clear diagnosis or treatment plan and is often dismissed as drug seeking or malingering. Determining the cause of chronic abdominal and pelvic pain has proven to be a very difficult task for all surgical practitioners. The literature has attempted to address the issue of surgical intervention for pain associated with adhesions, but treatment success has varied from 0%1 to 88%.2–28 Depending on the source reviewed, diagnostic laparoscopy with lysis of adhesions for pelvic pain has gained traction in the gynecological literature, but its acceptance in mainstream surgical literature and practice has been slow at best.3–9 The lack of definitive replicable tests or studies to identify the source of the pain coupled with our inability to predict the severity of surgical adhesion formation or prevention of reoccurrence following treatment has long complicated this problem.
We retrospectively report our experience with the surgical management of CAPPS using diagnostic laparoscopy and lysis of adhesions. The intent of this study was to see whether a laparoscopic lysis of adhesions alone would have any impact on the patients' preoperative complaint of pain on an otherwise “negative” surgical workup for having abdominal pain. Our “team” approach is used because of the complex nature of our patients' complaints. Most of our patients are female with associated gynecologic problems, such as ovarian remnants and endometriosis. The proactive approach of involving surgery and gynecology from the patient's initial visit allows us to plan our operative procedure accordingly after their evaluation. Additionally, pre- and postoperative care may include psychology, pain management, and physical therapy with additional expertise in pelvic floor and abdominal wall rehabilitation. This study specifically looked at the operative procedures and did not involve additional service lines to limit the variables in this review. Included in this study are patients', pre- and postoperative analog pain scores, and narcotic medication use over 12 months of follow-up.
METHODS
The Department of Surgery at Florida Hospital, Celebration Health, requested and received approval from our institutional review board to conduct a retrospective chart review of a single institution practice involving the surgical treatment of adhesions for patients (n=31) with abdominal and pelvic pain following prior abdominal surgery(s) from 2006 to 2008. Approval was given for 106 patients to be analyzed for the study who underwent treatment of adhesion- related disease. Thirty-one patients were included in this study who had undergone lysis of adhesions as part of their surgical procedure and did not undergo additional removal of any organs. Patients who had undergone any organ removal, resection, or repairs were excluded from the study.
Methods for Diagnostic Laparoscopy and Adhesiolysis
The operative technique used in all of our institutions for patients undergoing lysis of adhesions is as follow:
Because all of the patients included in this study had prior surgery, the direct vision entry technique was performed using Ethicon Endopath XL 5-mm trocars. Left upper quadrant entry was performed into the peritoneal cavity under direct vision. After successful entry was obtained, a second trocar was then usually placed in the patient's left lower quadrant (also a 5-mm trocar). With these 2 trocars, dissection of peritoneal adhesion was continued towards the umbilicus where a third 5-mm optical trocar was placed. The laparoscope was then usually moved to the midline port and dissection was carried over to the right lower quadrant where a fourth 5-mm trocar was placed. Should it be needed, a fifth trocar would then be placed in the right upper quadrant to aid in adhesion dissection. Once all the visceral and parietal peritoneal adhesions were dissected off the abdominal wall, the patient was placed in a steep Trendelenburg position where all pelvic adhesions were then lysed.
A complete adhesiolysis of pelvic adhesion was defined as all small bowel and omental adhesions being dissected off and out of the pelvis, off the right and left pelvic side walls, off the uterus, bladder, and vagina should the female organs still be in place, fallopian tubes and ovaries included, and all bowel adhesions off the antimesenteric surface of the rectum and colon to the level of the sacral promontory. Interloop adhesions were not lysed specifically unless noted upon “running the bowel” or if a transition zone were evident that would signal a potential bowel obstruction. Specific attention was also given to the possibility of any internal hernias that would have been reduced at the time of the surgery. The specific types of adhesions were not recorded, ie, filmy, thick, among others, because this is a subjective variable.
For the purpose of this study, all patients requiring bowel resections or repairs were excluded to decrease the variables in this current study. No adhesion prevention solutions were used in any of our patients. All hemostasis for the dissection plane was performed with a Harmonic Ace (Ethicon Endo-Surgery; Cincinnati, OH) for vascular hemostasis. No mono- or bipolar electrocautery energy sources were used in any of our patients. Additionally, it is routine in all of our laparoscopy patients to use heated and humidified carbon dioxide insufflation using the Insuflow device (Lexion Medical, Minneapolis, MN).
At the completion of the lysis of adhesions, hemostasis was ensured in all of our patients and trocar sites were closed with 4-0 Vicryl in a subcuticular manner. Most patients were discharged home on the same day of the procedure. There were no operative complications in this group of patients.
The data set includes patient information obtained in the preoperative interview and the surgical postoperative follow-ups at 3-, 6-, and 12-month intervals. The data points include patient's age and sex, pain scale (0 to 10) at each interval, use of narcotics, and number of abdominal surgeries.
RESULTS
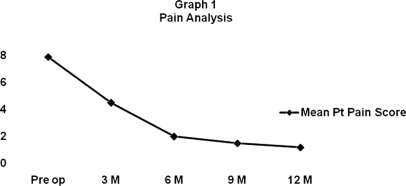
The findings from our study demonstrate that a majority of our pelvic pain patients are female (n=29). The patients ranged in age from 16 to 63 years with a mean of 41.67 years. The number of abdominal surgeries ranged from 1 to 7 with an average of 2.67. Other specific patient parameters were examined that included alcohol consumption, smoking history, or both, and these demonstrated no statistical differences. The postoperative pain scores reported by the patients were statistically significant. The mean preoperative pain score was 7.9; at 3 months it was 4.5, at 6 months 2.0, 9 months 1.5 (range, 0 to 5), and 12 months 1.2. Additionally, the change in subjective pain was statistically significant when comparing preoperative values to the 6 (P<0.05), 9 (P<0.05) and 12 (P<0.05) month follow-ups. The 3-month follow-up failed to reach statistical significance (P=.062). The mean pain level decreased with each interval with a final mean preoperative pain level of 7.9, and 12-month mean postoperative pain level of 1.2. Table 1 shows the summary of interval pain reduction over the 12-month time frame. Statistical analysis was performed using paired t tests.
Table 1.
Interval Pain Changes
| Preoperative Pain Score vs Months Postoperative Pain Scores | P Value |
|---|---|
| Preop vs 3 mo postop | 0.062 |
| Preop vs 6 mo postop | <0.05 |
| Preop vs 6 mo postop | <0.05 |
| Preop vs 9 mo postop | <0.05 |
| Preop vs 12 mo postop | <0.05 |
Statistical analysis is by paired t test. P value <0.05 significance.
Seventy-five patients were not included in this analysis of the initial 106 consented patients. Thirty-seven patients had rectal surgeries for endometriosis, 12 small bowel resections, and 26 bowel repairs not requiring resections. Ovarian remnants, hysterectomies, and other gynecologic-only procedures were not part of this study.
DISCUSSION
The major goal of this study was to evaluate whether our CAPPS patients experienced long-term pain relief following laparoscopic lysis of adhesions. Figure 1 shows that for each time period compared the average pain score decreased. Each of the time intervals was statistically significant except for the 3-month follow-up. The significant variable again demonstrates that pain or the use of pain medication decreased following the surgery. Other variables examining the number of abdominal surgeries, tobacco or ethanol history, was not statistically important in the patient's outcome.
Figure 1.
Pain analysis curve showing decrease in pain score at each time period.
Our hypothesis on the results is as follows:
Surgical lysis of adhesions for pain without organ removal or repair resolves in a different pathway than lysis of adhesions with removal or repair of surgical pathology. When an organ is repaired or resected with the immediate resolution of a partial bowel obstruction or removal of endometriosis, for example, the patient's body notices a correction of the pathology and the pain usually resolves quickly.
When there is no “organ removal, repair, or resection,” the chronic pain appears to be mediated through a spinal-thalamic pathway that takes longer to resolve, eg, phantom pain status after amputation or a mangled extremity. That is why patients with a lysis of adhesions alone take several months before resolution of their pain and not immediate relief of the pain.
The literature provides a unique and complicated discussion on handling chronic pelvic pain and at times may not provide a clear roadmap by which a standard of care can be developed and followed. The optimal study to prove the success of laparoscopic adhesiolysis would be a multi-center, prospective, randomized, double-blinded study with excellent patient follow-up; additionally, the development of a universally accepted scoring system for omental and visceral adhesions would allow surgeons to speak in one language when discussing their findings surgically. However, until this becomes a reality, we have implemented a multidisciplinary treatment algorithm that allows for the safe and ethical treatment of these patients including the use of diagnostic laparoscopy with lysis of adhesions (Figure 2).
Figure 2.
Complex abdominal pain treatment algorithm.
At our institution, a team-based and multidisciplinary approach has been taken to assess chronic pelvic pain among patients. Unlike other specific surgical processes, these patients require the expertise of multiple specialties (primarily general surgeons and gynecologists) to offer the best chance at surgical success.
Although our data are early and the enrollment numbers are low, we think that our results are encouraging. We continue to enroll patients in our CAPPS program and offer them a strictly adhered to regimented surgical treatment plan. We agree with earlier published reports related to the difficulty in preoperatively determining who benefits from diagnostic laparoscopy and lysis of adhesions. In addition, we acknowledge that there is no guarantee that similar adhesions will not reform and likely do reform. But our findings do show, at least initially, a statistical benefit for the surgical treatment of these patients.
There are many possible causes of CAPPS; the culprit examined in our study was surgical adhesions. Adhesions, whether from prior surgical procedures, endometriosis, or inflammatory bowel disease serve as a major source of trepidation for those who choose to perform surgery on these patients? There are several theories on the cause of adhesions and no proven treatment modality for their prevention. For small bowel obstructions secondary to adhesions, resistant to medical treatment, surgery is indicated. The use of lysis of adhesions for pain and partial obstructions is unknown. The gynecology literature touts the success of lysis of adhesions, but this may or may not be transferable to bowel lysis of adhesions.
The prejudiced view that laparoscopic lysis of adhesions for abdominal and pelvic pain not being an indication for surgery is simply not true in our opinion. Many paradigm shifts have occurred in medicine and surgery, and it is only through progressive, sometimes controversial, decisions that progress is made. As laparoscopic surgeons, we have the ability to perform a diagnostic and potentially therapeutic procedure for these people and either repair the source of their pain or provide them guidance to the appropriate specialist in a cost-effective care model as described in this article.
Contributor Information
Gregory D. McClain, Department of General Surgery, Florida Hospital-Celebration Health, Celebration, Florida, USA..
Jay A. Redan, Department of General Surgery, Florida Hospital-Celebration Health, Celebration, Florida, USA..
Steven D. McCarus, Department of Gynecology, Center for Advanced Specialized Gynecology, Florida Hospital-Celebration Health, Celebration, Florida, USA..
Aileen Caceres, Department of Gynecology, Center for Advanced Specialized Gynecology, Florida Hospital-Celebration Health, Celebration, Florida, USA..
John Kim, Department of Gynecology, Center for Advanced Specialized Gynecology, Florida Hospital-Celebration Health, Celebration, Florida, USA..
References:
- 1. Swank DJ, Swank-Borderwijk SCG, Hop WCJ, et al. Laparoscopic adhesiolysis in patients with chronic abdominal pain: a blinded randomised controlled multi-centre trial. Lancet. 2003;361:1247–1251 [DOI] [PubMed] [Google Scholar]
- 2. Dunker MS, Bemelman WA, Vijn A, et al. Long term outcomes and quality of life after laparoscopic adhesiolysis for chronic abdominal pain. J Am Assoc Gynecol Laparosc. 2004;11(1):36–41 [DOI] [PubMed] [Google Scholar]
- 3. Shayani V, Siegert C, Favia P. The role of laparoscopic adhesiolysis in the treatment of patients with chronic abdominal pain or recurrent bowel obstruction. JSLS. 2002;(6):111–114 [PMC free article] [PubMed] [Google Scholar]
- 4. Klingensmith ME, Soybel DI, Brooks DC. Laparoscopy for chronic abdominal pain. Surg Endosc. 1996;10(11):1085–1087 [DOI] [PubMed] [Google Scholar]
- 5. Lavonius M, Gullichsen R, Laine S, Ovaska J. Laparoscopy for chronic abdominal pain. Surg Laparosc Endosc. 1999;9(1):42–44 [PubMed] [Google Scholar]
- 6. Chopra R. Laparoscopic lysis of adhesions. Am Surg. 2003;69:966–968 [PubMed] [Google Scholar]
- 7. Schietroma M, Carlei F, Altilia F, et al. The role of laparoscopic adhesiolysis in chronic abdominal pain. Minerva Chir. 2001;56:461–465 [PubMed] [Google Scholar]
- 8. Nezhat FR, Crystal RA, Nezhat CH, Nezhat CR. Laparoscopic adhesiolysis and relief of chronic pelvic pain. JSLS. 2000;4:281–285 [PMC free article] [PubMed] [Google Scholar]
- 9. Howard FM. The role of laparoscopy in chronic pelvic pain: promise and pitfalls. Obstet Gynecol Surv. 1993;48:357–387 [DOI] [PubMed] [Google Scholar]
- 10. Kresch AJ, Seifer DB, Sachs LB, Barrese I. Laparoscopy in 100 women with chronic pelvic pain. Obstet Gynecol. 1984;64:672–674 [PubMed] [Google Scholar]
- 11. Steege JF, Stout AL. Resolution of chronic pain after laparoscopic lysis of adhesions. Am J Obstet Gynecol. 1991;165:278–283 [DOI] [PubMed] [Google Scholar]
- 12. Malik E, Berg C, Meyhofer-Malik A, Haider S, Rossmanith WG. Subjective evaluation of the therapeutic value of laparoscopic adhesiolysis. Surg Endosc. 2000;14:79–81 [DOI] [PubMed] [Google Scholar]
- 13. Howard FM. The role of laparoscopy as a diagnostic tool in chronic pelvic pain. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14:467–494 [DOI] [PubMed] [Google Scholar]
- 14. Rosenthal RH, Ling FW, Rosenthal TL, McNeeley SG. Chronic pelvic pain: psychological features and laparoscopic findings. Psychosomatic. 1984;25:833–841 [DOI] [PubMed] [Google Scholar]
- 15. Levitan Z, Eibschitz I, de Vries K, Hakim M, Sharf M. The value of laparoscopy in women with chronic pelvic pain and a “normal pelvis.” Int J Gyecol Obstet. 1985;23:71–74 [DOI] [PubMed] [Google Scholar]
- 16. Bahary CM, Gorodeski IG. The diagnostic value of laparoscopy in women with chronic pelvic pain. Ann Surg. 1987;11:672–674 [PubMed] [Google Scholar]
- 17. Howard FM. Laparoscopic evaluation and treatment of women with chronic pelvic pain. J Am Assoc Gynecol Laparosc. 1994;1:325–331 [DOI] [PubMed] [Google Scholar]
- 18. Cheong YC, Laird SM, Li TC, Shelton JB, Ledger WL, Cooke ID. Peritoneal healing and adhesions formation/reformation. Hum Reprod Update. 2001;7:556–566 [DOI] [PubMed] [Google Scholar]
- 19. Diamond MP, DeCherney AH. Pathogenesis of adhesion formation/reformation: application to reproductive pelvic surgery. Microsurgery. 1987;8:103–107 [DOI] [PubMed] [Google Scholar]
- 20. Duffy DM, diZerga GS. Adhesion controversies. Pelvic pain as a cause of adhesions, crystalloids in preventing them. J Reprod Med. 1996;41:19–26 [PubMed] [Google Scholar]
- 21. Peters AAW, Trimbos-Kemper GCM, Admiral C, Trimbos JB. A randomized clinical trial on the benefit of adhesiolysis in patients with intraperitoneal adhesions and chronic pelvic pain. Br J Obstet Gynecol. 1992;99:59–62 [DOI] [PubMed] [Google Scholar]
- 22. Daniell JF. Laparoscopic enterolysis for chronic abdominal pain. J Gynecol Surg. 1989;5:61–66 [Google Scholar]
- 23. Fayez JA, Clark RR. Operative laparoscopy for the treatment of localized chronic pelvic abdominal pain caused by postoperative adhesions. J Gynecol Surg. 1994;10:79–83 [DOI] [PubMed] [Google Scholar]
- 24. Bremers AJ, Ringers J, Vijn A, Janss RAJ, Bemelman WA. Laparoscopic adhesiolysis for chronic abdominal pain: an objective assessment. J Laparoendosc Adv Surg Tech A. 2000;10:199–202 [DOI] [PubMed] [Google Scholar]
- 25. Hakenberg OW, Wirth PAW. Chronic pelvic pain in men. Urol Int. 2002;68:138. [DOI] [PubMed] [Google Scholar]
- 26. Zermann D, Ishigooka M, Doggwiler-Wiygul R, Schubert J, Schmidt RA. The male chronic pelvic pain syndrome. World J Urol. 2001;19:173–179 [DOI] [PubMed] [Google Scholar]
- 27. Alexander-Williams J. Do adhesions cause pain? Br Med J (Clin Res Ed). 1987;294:659–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hammoud A, Gogo A. Adhesions in patients with chronic pelvic pain: a role for adhesiolysis. Fertil Steril. 2004;82(6):1483–1490 [DOI] [PubMed] [Google Scholar]