This report concludes that there is no evidence to recommend routine closure of 5-mm trocar incisions; the choice should be left to the discretion of the individual surgeon.
Keywords: Trocar hernia, Trocar-site hernia, Laparoscopic hernia, Trocar port-site hernia, Laparoscopic port-site hernia, Trocar fascia closure
Abstract
Objective:
To evaluate the evidence for fascial closure of 5-mm laparoscopic trocar sites.
Methods:
We conducted electronic database searches of PubMed and the Cochrane Library for articles published between November 2008 and December 2010. We used the keywords trocar hernia, trocar-site hernia, laparoscopic hernia, trocar port-site hernia, laparoscopic port-site hernia. Prospective and retrospective case series, randomized trials, literature reviews, and randomized animal studies of trocar hernias on abdominal wall defects from gynecologic, urologic, and general surgery literature were reviewed. The Cochrane Database was reviewed for pertinent studies. Metaanalysis was not possible due to the significant heterogeneity between studies and lack of randomized trials large enough to assess the incidence of this rare complication.
Results:
Trocar-site hernias are a rare but known complication of laparoscopic surgery. Trocar size ≥10mm is associated with an increased rate of hernia development. Currently, the accepted gynecologic surgical practice is closure of fascial incisions ≥10mm, while incisions <10mm do not require closure. However, large prospective and retrospective case series reports from general surgery and urology literature support nonclosure of blunt or radially dilating trocars in paramedian sites. Expert opinion and small case reports suggest that in cases of prolonged manipulation of 5-mm trocar sites the surgeon should consider fascial closure, because extension of the initial incision may have occurred.
Conclusion:
There is no evidence to recommend routine closure of 5-mm trocar incisions; the choice should continue to be left to the discretion of the individual surgeon.
INTRODUCTION
The case presented herein is of a 5-mm trocar-site incisional hernia. This is a rare complication, because most trocar-site hernias reported in the gynecologic, urology, and general surgery literature have developed at incisions ≥10mm. The incidence of trocar hernias ranges from 0.2% to 3.1% in large case series and reviews (Table 1) 1–5 and has been correlated to trocar size.1,4,5 Trocar hernias at a 5-mm port site are infrequently reported in the literature. There have been 10 published case reports in adults of 5-mm trocar hernias (Table 2).6–9 The largest number of 5-mm cases was published by Nezhat2 in 1997 for a total of 5 of 11 trocar-site hernias in a retrospective case review of approximately 5300 patients. Factors that may be involved in the development of hernias that were addressed in the literature include trocar size, location, trocar type, trocar manipulation, entry and closure techniques, and preexisting fascial defects. The objective of this review was to analyze the evidence for closure of 5-mm fascial incisions.
Table 1.
| Author | Study Type | Fascial Closure Hernia Development | Non Closure Hernia Development | % Umbilical | % Extra-umbilical | Incidence, Size Related |
|---|---|---|---|---|---|---|
| Kadar1 | Retrospective, 3560 operative gynecologic laparoscopies | 5-mm 0/8771 | 0 | 100% | 5-mm 0% | |
| 10-mm 0/175 | 10-mm 1/254 | 10-mm (1) 0.23% | ||||
| 12-mm 3/136 | 12-mm 2/25 | 12-mm (5) 3.1% | ||||
| Nezhat2 | Retrospective, 5,300 gynecologic laparoscopies | 10-mm 6 sites | 5-mm 5 sites | All 10-mm | All 5-mm | 0.2% overall |
| Azurin3 | Retrospective, 1,300 laparoscopic cholecystectomies | 10/1,300 | N/A | 10/10, 10-mm | N/A | 0.77% overall |
| Montz4 | Survey, 933 reported gynecologic cases (840 size known) | 167/933 | 766/933 | 76% | 24% | .021% overall estimated -86% ≥ 10-mm |
| Lajer5 | Literature review, 62 gynecologic cases (55 size known) | 53/55 | 96% ≥ 10-mm | 27% | 73% | n/a |
Table 2.
5-mm Trocar Hernia Case Reports
| Author | Procedure | Location | Comments |
|---|---|---|---|
| Nezhat2 | Hysterectomy adhesiolysis | Left lower quadrant 5 | Extensive manipulation at trocar sites where hernias developed |
| Plaus6 | Diagnostic for pelvic pain, biliary colic | Midline supra-pubic 2 | Para-median sites may be preferred over midline |
| Reardon7 | Para-esophageal hernia repair | Left abdomen 1 | Hernia developed at site of active manipulation with repetitive movements in long procedure |
| Matter8 | cholecystectomy | Right upper lateral 1 | Reinsertion of cannula may widen initial fascial defect |
| Toub9 | Radical hysterectomy for cervical carcinoma | Left lower quadrant 1 | Began chemotherapy postoperative day #3 |
CASE REPORT
A 43-year-old gravida 2 para 2 woman underwent a laparoscopic hysterectomy with removal of a 20-week size fibroid uterus. An 11-mm umbilical radially expanding trocar was placed using the Veress needle, followed by 3 accessory 5-mm ports in the right, left, and suprapubic regions under direct visualization. The umbilical port site was expanded to 14-mm for morcellation, and the fascia was later closed with 2 interrupted 0 polygalactin suture using the Carter-Thomason. The 5-mm fascial incisions were not closed. The uterine weight was 1505g.
The patient's recovery was unremarkable. She did have nausea and vomiting in the immediate recovery period that resolved with medication and went home the evening of post-operative day one. On postoperative day 4, she developed nausea and vomiting and presented to the gynecology clinic having passed one bowel movement. Upon examination, she was found to be afebrile, have a soft, mildly distended abdomen with normal bowel sounds and tenderness over the right lower quadrant incision. The incisions were intact without drainage or erythema. She had a normal leukocyte count. Computed tomography of her abdomen and pelvis showed a spigelian hernia in the right lateral abdominal wall at the level of the iliac crest, with a herniated loop of small bowel (Figure 1). She was immediately taken to the operating room.
Figure 1.

Herniated loop of small bowel through Spigelian fascia.
Intraoperatively, the herniated small bowel was found to be viable and was manually reduced into the abdomen. The peritoneum and fascia were closed with a 3-0-polygalactin running stitch. The patient did well and went home the next morning. This patient's hernia development may have been related to the extensive trocar manipulation that was required to operate on a 1505g myomatous uterus that resulted in expansion of the fascial incision.
METHODS
Prospective and retrospective case series, randomized trials, literature reviews, and randomized animal studies of trocar hernias on abdominal wall defects from gynecologic, urologic, and general surgery studies were reviewed. Metaanalysis was not possible due to the significant heterogeneity between studies and lack of randomized trials large enough to assess the incidence of this rare complication. The studies were organized by (1) incidence of incisional hernia development via large case series, (2) hernia development by trocar type and location, (3) animal studies on abdominal wall defects from trocar types, (4) pre-existing fascial defects, and (5) trocar manipulation.
RESULTS
Location
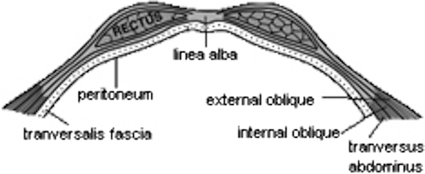
Para-median locations versus median locations (including the umbilicus) have been associated with conflicting rates of trocar hernias reported in the literature (Table 1).1–5 The linea alba, including the umbilicus, lacks the muscle support in spontaneous fascial closure due to the lack of rectus muscle. Paramedian incisions have been shown in animal studies to be supported by muscle re-opposition after blunt trocars were used (Table 3).10,11 Para-median incisions have also been shown in Level 2 general surgery studies not to require fascial closure when blunt trocars are used (Table 4).12–17 The arcuate line may also demarcate an inherent weakness of the abdominal fascia. It is the place where the fascia of the internal oblique and the transversus abdominus of the posterior rectus sheath migrate to join the anterior sheath, leaving only the transversalis fascia and peritoneum for closure support deep to the rectus muscle (Figures 2 and 3).
Table 3.
| Author | Study | Trocar type | Difference in Defect Surface Area | Comments |
|---|---|---|---|---|
| Tarnay10 | Randomized, observer blinded swine abdominal wall | Cutting Conical Pyramidal | Conical fascial defect 57–68% smaller than cutting | Conical split muscles, which later re-opposed with fascia |
| Conical fascial defect 32–62% smaller than pyramidal | ||||
| Bhoyrul11 | 12 swine abdominal, not blinded | Cutting Blunt radially dilating | Radially dilating 52% narrower muscle defect than cutting | Muscles split rather than cut |
Table 4.
| Author | Study Type/Size | Trocar type, Location | Fascia Closed | Follow up Time | Hernia Incidence | Conclusion/Comments |
|---|---|---|---|---|---|---|
| Bhoyrul12 | Randomized/244 general surgery procedures | Cutting & Blunt | ≥10-mm cutting >10-mm blunt (3%) | 6–18 months | Cutting 125 C 0% Blunt 119 NC: 0% | Radially expanding trocar sites do not require routine closure |
| Liu13 | Prospective/110 sites, general surgery procedures | Blunt, para-median | None | 11 months | 10-mm 0% 12-mm 0% | Closure not required with blunt trocars at para-median sites above arcuate line, residual fascial defect 6–8mm |
| Johnson14 | Retrospective/747 Roux-en-Y gastric bypass | Blunt, para-median | None | 20 months | 1494 12-mm 0% 2241 5-mm 0% | Para-median blunt (radially dilating) sites do not require closure |
| Shalhav15 | Retrospective/92 renal procedures | Blunt, para-median | 62 closed, 28 non- closed | 4.8 months | 12-mm C: 0% 12-mm NC: 0% | Closure not required on para-median blunt trocars, NC excluded malnutrition, renal failure, chronic steroid use |
| Siqueira16 | Retrospective/350 sites, donor nephrectomies | Blunt, para median | None | 36 months | 140 12-mm 0% 210 5-mm 0% | Closure not required on para-median blunt trocars even at 12-mm |
| Mahmoud17 | Prospective/405 Nissen fundoplication | Cutting, para median, above arcuate line | None | 1 month up to 6 years | 810 10-mm 0% | Para-median trocar sites do not require closure |
Figure 2.
Abdominal fascia above the arcuate line. The posterior rectus sheath is made up of the internal oblique, transversus abdominous, and transversalis fascia. Image reprinted from Netter's, public domain courtesy of Wikipedia.com.
Figure 3.
Abdominal fascia below the arcuate line. The posterior rectus sheath is made up of only the transversalis fascia. Image reprinted from Netter's, public domain courtesy of Wikipedia. com.
Trocar Type
Blunt (conical, pyramidal, radially dilating, nonbladed) have been shown to have the benefit of decreased length and surface area of fascial defects over bladed or cutting trocars in animal studies with muscle splitting instead of cutting (Table 3). This evidence supports nonclosure of 5-mm fascial defects made with blunt trocars.
Manipulation
Extensive manipulation of the trocar port site may widen a port-site incision beyond the initial length. Fascial and peritoneal stretching of the original incision may occur from several causes: specimen removal, multiple reinsertions of the sheath, advanced surgical difficulty requiring increased force and torque on the fascia, and prolonged operative time. Nezhat's review2 reported that the substantial manipulation of the 5-mm operative port sites required for the surgeries resulted in trocar-site hernias. All 5 cases were associated with advanced surgical complications: extensive adhesions, severe endometriosis, large uterine leiomyomata.2 All cases occurred in the left supra-pubic location where the bulk of manipulation was performed and no closure was performed.
Pre-existing Fascial Defects
Ramachandran18 found an 18% incidence of pre-existing umbilical fascial defects in 2100 patients undergoing laparoscopic surgery for various gynecologic and general surgery indications. All identified defects were repaired, and a relationship was not found between the repaired pre-existing fascial defect and the development of a hernia.18 In contrast, in a report on 1300 laparoscopic cholecystectomies, Azurin3 reported 9 of 10 trocar hernias developed in patients who had been diagnosed with a pre-existing hernia preoperatively despite intraoperative repair. Trocar incisions at sites of pre-existing hernias should be carefully evaluated to confirm adequate closure.
Insertion and Closure Techniques
A Cochrane review from 2008 that evaluated different entry techniques reported no advantage in using any single technique over another to prevent major complications.19 They did not report data relating to laparoscopic trocar hernias.
Only one randomized trial20 conducted an intraoperative evaluation of laparoscopic closure techniques. Elashry et al20 looked at closure of 95 twelve-mm trocar port sites in 32 patients and compared the Carter-Thomason (CT-NP) needle point suture device (CooperSurgical, Inc, Trumbull, CT) with the Maciol suture needle set (Specialty Surgical Instrumentation, Nashville, TN), eXit disposable puncture closure device (Progressive Medical, St. Louis, MO), the Endoclose device (Covidien Surgical, Norwalk, CT), a 14-gauge angiocatheter, Lowsley retractor (CS Surgical Inc, Slidell, LA) with hand-sutured closure, and standard hand-sutured closure. They found that the CT-NP device was faster (mean time 2.5 minutes) and had secure closure confirmed digitally and endoscopically, but they did not follow their patients for hernia development.20 This study was underpowered, so no definitive conclusions can be made about the benefit of one closure type over another in hernia development.
CONCLUSION
Trocar-site hernias are a known complication related to laparoscopic surgery. Trocar size is the primary measure by which most gynecologic surgeons decide to close fascial incisions; conventional practice is closure of 10-mm incisions and nonclosure of 5-mm incisions. Fascial closure does not prevent incisional hernia development. Paramedian location and blunt type trocars are 2 factors that have been extensively reported on in general surgery and urologic surgery Level II studies as measures by which fascial closure is not required 10-mm and 12-mm incisions. We would recommend surgeons consider fascial closure in 5-mm incisions where extensive, prolonged manipulation occurred that may have extended or widened the initial defect.
Acknowledgments
The authors wish to thank Dr. Misa Perron-Burdick and the Kaiser Permanente Oakland Library staff, Mare Gehrke and Angela Hudson, for their assistance.
References:
- 1. Kadar Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol. 1993. May;168(5):1493–1495 [DOI] [PubMed] [Google Scholar]
- 2. Nezhat C. Incisional hernias after operative laparoscopy. J Laparoendosc Adv Surg Tech A. 1997. April;7(2):111–115 [DOI] [PubMed] [Google Scholar]
- 3. Azurin DJ. Trocar site herniation following laparoscopic cholecystectomy and the significance of an incidental preexisting umbilical hernia. Am Surg. 1995;8:718–20 [PubMed] [Google Scholar]
- 4. Montz FJ. Incisional hernia following laparoscopy: a survey of the American Association of Gynecologic Laparoscopists. Obstet Gynecol. 1994. November;84(5):881–884 [PubMed] [Google Scholar]
- 5. Lajer H. Hernias in trocar ports following abdominal laparoscopy, a review. Acta Obstet Gynecol Scand. 1997. May;76(5):389–393 [DOI] [PubMed] [Google Scholar]
- 6. Plaus WJ. Laparoscopic trocar site hernias. J Laparoendosc Surg. 1993. December;3(6):567–570 [DOI] [PubMed] [Google Scholar]
- 7. Reardon P. Hernia at 5-mm laparoscopic port site presenting as early postoperative small bowel obstruction. J Laparoendosc & Adv Surg Tech A. 1999. December;9(6):523–525 [DOI] [PubMed] [Google Scholar]
- 8. Matter I. Incisional hernia via a lateral 5mm trocar port following laparoscopic cholecystectomy. Isr J Med Sci. 1996. September;32(9):790–791 [PubMed] [Google Scholar]
- 9. Toub D. Omental herniation through a 5-mm laparoscopic cannula site. J Am Assoc Gyncol Laparosc. 1994. August;1(4 Pt 1):413–414 [DOI] [PubMed] [Google Scholar]
- 10. Tarnay CM. Incisional characteristics associated with six laparoscopic trocar-cannula systems: a randomized, observer-blinded comparison. Obstet Gynecol. 1999. July;94(1):89–93 [DOI] [PubMed] [Google Scholar]
- 11. Bhoyrul S. Radially expanding dilatation. A superior method of laparoscopic trocar access. Surg Endosc. 1996. July;10(7):775–778 [DOI] [PubMed] [Google Scholar]
- 12. Bhoyrul S, Payne J, Steffes B, Swanstrom L, Way LW. A randomized, prospective study of radially expanding trocars in laparoscopic surgery. J Gastrointest Surg. 2000. Jul-Aug;4(4):392–397 [DOI] [PubMed] [Google Scholar]
- 13. Liu CD. Laparoscopic port sites do not require fascial closure when nonbladed trocars are used. Am Surg. 2000. September;66(9):853–854 [PubMed] [Google Scholar]
- 14. Johnson WH. VersaStep trocar hernia rate in unclosed fascial defects in bariatric patients. Surg Endosc. 2006. October;20(10):1584–1586 [DOI] [PubMed] [Google Scholar]
- 15. Shalhav A. Transperitoneal laparoscopic renal surgery using blunt 12-mm trocar without fascial closure. J Endourol. 2002. February;16(1):43–46 [DOI] [PubMed] [Google Scholar]
- 16. Siqueira T. The use of blunt-tipped 12-mm trocars without fascial closure in laparoscopic live donor nephrectomy. JSLS. 2004. Jan-Mar;8(1):47–50 [PMC free article] [PubMed] [Google Scholar]
- 17. Mahmoud Uslu HY. Cannula site insertion technique prevents incisional hernia in laparoscopic fundoplication. Surg Laparosc Endosc Percut Tech. 2007. August;17(4):267–270 [DOI] [PubMed] [Google Scholar]
- 18. Ramachandran CS. Umbilical hernial defects encountered before and after abdominal laparoscopic procedures. Int Surg. 1998. Apr-Jun;83(2):171–173 [PubMed] [Google Scholar]
- 19. Ahmad G, Duffy JMN, Phillips K, Watson A. Laparoscopic entry techniques. Cochrane Database Syst Rev 2008, Issue 2 Art. No.: CD006583. DOI: 10.1002/14651858.CD006583.pub2 [DOI] [PubMed] [Google Scholar]
- 20. Elashry OM. Comparative clinical study of port-closure techniques following laparoscopic surgery. J Am Coll Surg. 1996. October;183(4):335–344 [PubMed] [Google Scholar]