The spleen appears to be at increased risk for injury during hand-assisted, bilateral laparoscopic renal procedures when the patient is placed in the “airplanes” supine position.
Keywords: Laparoscopy, Kidney, Supine position
Abstract
Objective:
We evaluated the safety of simultaneous bilateral renal procedures performed using hand-assisted laparoscopy (HAL) with the patient in the supine position.
Materials and Methods:
After securely strapping the patient to the table, a hand-port device is placed via a 7-cm supraumbilical or peri-umbilical incision with two to four 5-mm to 12-mm trocars placed bilaterally. During a 3-year period, 8 bilateral HAL renal operations were initiated (upper pole partial nephrectomies, 3 nephroureterectomies, 3 bilateral nephrectomies, and right nephrectomy with left adrenalectomy).
Results:
Mean patient age was 41 years. One patient with ADPKD required conversion to open due to failure to progress secondary to excessive perirenal fat and 22-cm kidneys. The other 7 were completed successfully with a mean operative time of 417 minutes and mean EBL of 336cc. Two patients received transfusions. Two small splenic lacerations, managed conservatively, were the only complications.
Conclusions:
Bilateral hand-assisted laparoscopic renal surgery with the patient in the supine position (rolling the table side to side) is feasible in the majority of patients. However, very large kidneys (eg, ADPKD) may be better approached with the patient in the lateral decubitus position or via an open subcostal incision. Importantly, the spleen appears to be at increased risk for capsular injury due to apparent increased difficulty of left colon mobilization in the “rolled” or “airplaned” supine position.
INTRODUCTION
During the last decade, multiple investigators have reported that bilateral hand-assisted laparoscopic nephrectomy is feasible and safe, even for patients with autosomal dominant polycystic kidney disease (ADPKD) (Table 1).1–10 Other investigators have further reported that single-setting bilateral HAL partial nephrectomy, ureterolysis, and nephroureterectomy are also feasible and safe.11–14 Although some surgeons in these prior series repositioned the patient to maintain the advantage of performing laparoscopy with the patientin the lateral decubitus position, most positioned the patient supine (dorsal decubitus) and rolled the table from side to side, elevating the kidney 30° to 45°, to operate on each kidney without the need to reposition the patient.
Table 1.
Published Series of Bilateral Hand-Assisted Laparoscopic Nephrectomy
| Report | Patient Population | Case no. | Lateral Decubitus Procedure + Repositioning | Supine Procedure, No Repositioning | Position Angle | Mean Total OR Time (min) | Mean Estimated Blood Loss (mL) | Complications |
|---|---|---|---|---|---|---|---|---|
| Schmidlin et al, 20001 | ESRD, UTI | 1 | 1 | 0 | 60° | 210 | 300 | 0 |
| Rehman et al, 20012 | ADPKD | 3 | 1 (3rd case) | 2 | 40–50° | 330 (395, 300) | <200 | 0 |
| Troxel & Das, 20013 | ESRD, UTI, DK, ADPKD | 2 | 2 | 0 | 90° | 360 | 400 | 1 AV fistula thrombosis |
| Jenkins et al, 20024 | ADPKD | 4 | 4 | 0 | 90° | 286 | 338 | 1 ATN; 1 postop percutaneous drain placement; 1 retroperitonea I hematoma |
| Lee & Clayman, 20045 | ADPKD | 3 | 0 | 3 | 40° (30–45°) | 390 | 100–200 | NS |
| Tan et al, 20046 | Chronic infection | 2 | 2 | 0 | 60° | 265 | NS | NS |
| Zaman et al, 20057 | ADPKD | 6 | 0 | 6 | NS | 185 | 345 | 0 |
| Tobias-Machado et al, 20058 | >20 cm ADPKD | 3 | 0 | 3 | NS | 190 | NS | 1 pneumothorax; 1 conversion; 1 transfusion |
| Whitten et al, 20069 | ADPKD | 10 | 0 | 10 | 30° | 194 | 203 | 1 AV fistula thrombosis; 1 reintubation |
| Lipke et al, 200710 | ADPKD | 18 | 0 | 18 (+/−gel roll under one flank) | NS | 315 | 350 | 5 complications; 4 conversions; 2 transfusions |
ESRD = end-stage renal disease, UTI = unrinary tract infection, DK =, ADPKD = autosomal dominant polycystic kidney disease; AV = Arteriovenous, ATN = acute tubular necrosis, NS = not significant.
Inflammatory renal conditions added to the difficulty and operative time.6,8 Bilateral nephrectomies to remove large ADPKD were the most challenging procedures overall, with the longest operative times and the greatest chance for open conversion.8,10 All of these prior investigators concluded that bilateral HAL renal surgery was safe, even with the patients positioned supine throughout the procedure and rolled or “airplaned” in each direction to operate on each kidney. While it would seem probable that bowel mobilization would be more difficult in this latter situation, to our knowledge, no prior investigators have reported an increased rate of splenic capsule injury. The aim of this study was to evaluate our experience with performing simultaneous renal procedures using HAL with the patient in the supine position, specifically focusing on safety and occurrence of adjacent organ injury.
MATERIALS AND METHODS
The patients were securely strapped to the table in the supine position with 3-inch tape criss-crossing the chest, across the hips, thighs, and lower extremities. A hand-port device was placed via a midline 7-cm supraumbilical (extending to or skirting the upper left umbilicus) in 5 patients and via a peri-umbilical incision (for 3 nephroureterectomy patients, Figure 1) with two to four 5-mm to 12-mm trocars placed bilaterally. The table was rolled or “airplaned” maximally side-to-side to allow for bowel and hepatic/splenic flexure mobilization and surgery in each retroperitoneum.
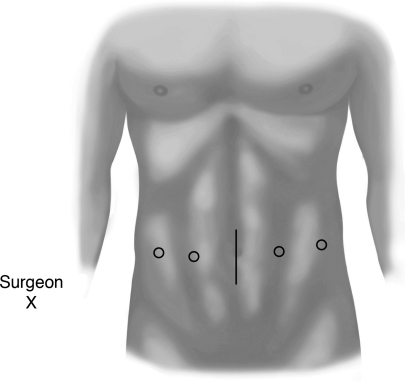
Figure 1.
Periumbilical hand-port and laparoscopic trocar placement sites.
We initiated 8 bilateral HAL renal operations (upper pole partial nephrectomies, 3 bilateral nephroureterectomies, 3 bilateral nephrectomies, and a right nephrectomy with left adrenalectomy) as treatment for incontinence secondary to ectopic vaginal ureters, end-stage renal disease (ESRD) with left renal tumor, ESRD with vesicoureteral reflux (VUR; 3 cases), ESRD with Goodpasture's disease and refractory hypertension, ESRD with neurogenic bladder and VUR and ESRD with ADPKD. Resident surgeons actively participated as operative surgeons during cases. Patient demographic data, operative times, estimated blood loss (EBL), blood transfusions, conversion rates, and complications were recorded.
RESULTS
All 8 patients were female with a mean age of 41 years. Seven cases (87.5%) were completed successfully with a mean operative time of 417 minutes (median, 407) and mean EBL of 336mL (median, 250). One ADPKD patient underwent attempted bilateral HAL nephrectomies and required open conversion due to failure to progress secondary to excessive perirenal fat and 22-cm kidneys.
The mean preoperative serum hemoglobin was 11.4mg/dL (median, 11.2). The mean postoperative hemoglobin level was 9.2mg/dL (median, 8.8). Two patients received red blood cell transfusions. The only complications identified were 2 small splenic capsular lacerations, both of which were managed conservatively. There were no other intraoperative or postoperative complications identified.
DISCUSSION
Several prior investigators have reported that simultaneous bilateral HAL nephrectomy is safe and effective, even when performed with the patient in the supine position (Table 1).1–10 Additionally, bilateral HAL partial nephrectomy and ureterolysis have been demonstrated to be feasible and without excessive morbidity.11,12 In the partial nephrectomy series, the patients were in the lateral decubitus position and repositioned during the operation, but in the ureterolysis series, the patients was secured to the operative table supine and the table was rolled to each side.
Additionally, the feasibility of HAL bilateral nephroureterectomy (HALBNU) has recently been demonstrated. Investigators from the National Taiwan University in Taipei reported the first HALBNU in 2002 and subsequently published a review of 33 HALBNU patients (compared to 16 open BNU patients) treated for clinically localized presumed upper tract transitional cell carcinoma.13,14 Their HALBNU cases took 38 minutes longer on average (309 vs 271 minutes) with lower transfusion (42% vs 75%) and complication (12% vs 19%) rates. Importantly, while they positioned the patient supine and rolled the table rather than reposition, they used alternating inflation cuffs to further elevate the flank. Additionally, the distal ureteral dissections were performed through the 7-cm HAL incision by using an open technique.
Our series includes patients undergoing bilateral HAL nephrectomy, a bilateral upper pole partial nephrectomy plus 3 bilateral nephroureterectomies. The latter cases were to treat 3 patients with ESRD from vesicoureteral reflux (VUR). Unlike Chueh and colleagues,13 we used no technique such as inflation devices to further elevate the flank. Additionally in these procedures for benign disease, the ureters were divided at the level of the bladder (without taking a bladder cuff) using an entirely HAL surgical approach.
Our mean operative time of 417 minutes was longer than the mean operative times of prior reports of bilateral HAL nephrectomies (194 to 330 minutes), HALBNU (309 minutes) and partial nephrectomies (246 minutes).2,4,6,9,11,14 The reason for our increased operative times is unclear, but the relatively low volume of widely varying procedures and significant active resident participation in all cases were likely contributing factors. Our mean EBL of 336mL, however, was on par with prior reports (<350mL).2,5,11 The need to transfuse 2 patients and to convert our large ADPKD case to open was also consistent with prior reports of bilateral HAL surgery to treat ADPKD.8,10 In these series, 1 of 3 and 4 of 18 ADPKD patients required open conversion.
Unique to this study, however, was the occurrence of splenic capsular lacerations in 25% (2 of 8) of the procedures. This complication, to our knowledge, has not been previously reported and raises concern regarding the safety of colonic splenic flexure mobilization when the patient is positioned totally supine on the table. In this position, even with the table tilted maximally, we observed suboptimal medial bowel displacement and found that a greater than normal amount of hand traction to mobilize the colon (rather than displacement by gravity) was required, when subjectively compared to HAL renal procedures in the full lateral decubitus position.
We acknowledge that a significant limitation to this study is the small number of patients and the performance of several different bilateral hand-assisted procedures. We also acknowledge that bilateral HAL surgery in the nearly supine position, with a gel roll or balloon elevating the left flank 10% to 15% and removed mid-case prior to switching to the right side, can be successfully performed. Further, HAL and pure laparoscopic renal surgery to the left kidney in a modified (30°) flank position has been widely reported, and although splenic injury is a known complication, the incidence is generally very low.
Therefore, we believe the main finding of this study is that performance of bilateral HAL renal surgery with the patient in the totally supine position (and without any form of flank elevation) provides suboptimal exposure to the kidneys and adrenal glands, which may lead to longer operative times and a higher complication rate. While there are special situations in which bilateral HAL procedures are appropriate, utilization of some form of left flank elevation should be strongly considered. Additionally, staged procedures, optimal lateral decubitus repositioning of the patient between sides, and early conversion to open surgery in the case of failure to progress are all reasonable alternatives to the described technique.
CONCLUSION
Bilateral hand-assisted laparoscopic renal procedures with the patient in the supine position (rolling the table side to side) are feasible but may put the spleen at increased risk (25% in this series) for a capsular injury. Additionally, while complex diseases may be handled, very large kidneys (eg, ADPKD, >20cm) are at significant risk for open conversion, and we believe are better approached in the lateral decubitus position or via an open subcostal incision. The senior author has abandoned this supine approach and currently favors repositioning or staging the renal procedures, performed with the patient in the lateral decubitus position.
References:
- 1. Schmidlin FR, Iselin CE. Hand-assisted laparoscopic bilateral nephrectomy. Urology. 2000;56:153. [DOI] [PubMed] [Google Scholar]
- 2. Rehman J, Landman J, Andreoni C, McDougall EM, Clayman RV. Laparoscopic bilateral hand assisted nephrectomy for autosomal dominant polycystic kidney disease: initial experience. J Urol. 2001;166:42–47 [PubMed] [Google Scholar]
- 3. Troxel S, Das S. Hand-assisted laparoscopic approach to multiple-organ removal. J Endourol. 2001;15:895–897 [DOI] [PubMed] [Google Scholar]
- 4. Jenkins MA, Crane JJ, Munch LC. Bilateral hand-assisted laparoscopic nephrectomy for autosomal dominant polycystic kidney disease using a single midline HandPort incision. Urology. 2002;59:32–36 [DOI] [PubMed] [Google Scholar]
- 5. Lee DI, Clayman RV. Hand-assisted laparoscopic nephrectomy in autosomal dominant polycystic kidney disease. J Endourol. 2004;18:379–382 [DOI] [PubMed] [Google Scholar]
- 6. Tan YH, Siddiqui K, Preminger GM, Albala DM. Hand-assisted laparoscopic nephrectomy for inflammatory renal conditions. J Endourol. 2004;18:770–774 [DOI] [PubMed] [Google Scholar]
- 7. Zaman F, Nawabi A, Abreo KD, Zibari GB. Pretransplant bilateral hand-assisted laparoscopic nephrectomy in adult patients with polycystic kidney disease. JSLS. 2005;9:262–265 [PMC free article] [PubMed] [Google Scholar]
- 8. Tobias-Machado M, Tavares A, Forseto PH, Jr., Zambon JP, Juliano RV, Wroclawski ER. Hand-assisted laparoscopic nephrectomy as a minimally invasive option in the treatment of large renal specimens. Int Braz J Urol. 2005;31:526–533 [DOI] [PubMed] [Google Scholar]
- 9. Whitten MG, Van der Werf W, Belnap L. A novel approach to bilateral hand-assisted laparoscopic nephrectomy for autosomal dominant polycystic kidney disease. Surg Endosc. 2006;20:679–684 [DOI] [PubMed] [Google Scholar]
- 10. Lipke MC, Bargman V, Milgrom M, Sundaram CP. Limitations of laparoscopy for bilateral nephrectomy for autosomal dominant polycystic kidney disease. J Urol. 2007;177:627–631 [DOI] [PubMed] [Google Scholar]
- 11. Madi R, Wolf JS., Jr Single-setting bilateral hand-assisted laparoscopic partial nephrectomy. J Endourol. 2009;23:929–932 [DOI] [PubMed] [Google Scholar]
- 12. Brown JA, Garlitz CJ, Hubosky SG, Gomella LG. Hand-assisted laparoscopic ureterolysis to treat ureteral obstruction secondary to idiopathic retroperitoneal fibrosis: assessment of a novel technique and initial series. Urology. 2006;68:46–49 [DOI] [PubMed] [Google Scholar]
- 13. Chueh SC, Chen J, Hsu WT, Hsieh MH, Lai MK. Hand assisted laparoscopic bilateral nephroureterectomy in 1 session without repositioning patients is facilitated by alternating inflation cuffs. J Urol. 2002;167:44–47 [PubMed] [Google Scholar]
- 14. Tai HC, Lai MK, Chung SD, Huang KH, Chueh SC, Yu HJ. Intermediate-term oncological outcomes of hand-assisted laparoscopic versus open bilateral nephroureterectomy for dialysis and kidney transplant patients with upper urinary tract urothelial carcinoma. J Endourol. 2009;23:1139–1144 [DOI] [PubMed] [Google Scholar]