The mildest inflammatory changes postoperatively were found in the staple group followed by those in the Hem-O-Lok group.
Keywords: Laparoscopic appendectomy, Hem-o-lok clip, Endoloop, Stapler
Abstract
Background and Objectives:
The standard technique for securing the base of the appendix during laparoscopic appendectomy is by absorbable endoloop ligature, although clinical reports favor the use of the stapler. Nonabsorbable Hem-o-lok clips have been shown to be an alternative technique to this. However, it is currently not clear whether nonabsorbable clips have any effects on the intestine or promote infection in the surgical area.
Materials and Methods:
Sixty Wistar albino rats were randomized into 3 treatment groups: group I (n=20) the base of the appendix was secured by endoloop 2-0 ligature; group II (n=20) dissection of the appendix was performed by a 45-mm thick stapler; and group III (n=20) the base of the appendix was secured by a Hem-o-lok plastic clip. The animals were sacrificed on the 14th and 28th days after surgery. The secured stump was used for histopathological examination.
Results:
There were no significant differences in histopathological changes observed on the 14th postoperative day between the groups. On the 28th postoperative day, it was proved that mild and moderate inflammation is more frequent in the endoloop and Hem-o-lok groups than in the stapler group. Reaction to a foreign body is more frequent in the endoloop than in stapler and Hem-o-lok groups.
Conclusion:
The mildest postoperative inflammatory changes were seen in the stapler group, followed by the Hem-o-lok group. However, because of the price of the plastic clip and the simplicity of its application, its use is still favored during laparoscopic appendectomy.
INTRODUCTION
The standard technique for securing the base of the appendix during laparoscopic appendectomy is by absorbable endoloop ligature,1 although clinical evidence favors the use of the stapler.2,3 Nonabsorbable polymer locking Hem-o-lok clips are an alternative technique, because laparoscopic appendectomy can be performed faster and cheaper in this way than the standard technique.4,5 However, currently there is no literature examining the effects of the use of a nonabsorbable clip on the intestine or whether it promotes infection in the surgical area. Absorbable suture materials lead to various levels of inflammation and foreign body reactions,6 but nonabsorbable sutures lead to a milder tissue reaction, especially if nylon and wire sutures are used.7 Consequently, we hypothesized that nonabsorbable polymer Hem-o-lok clips would cause a milder reaction in the tissue after appendectomy than absorbable endoloop Vicryl ligatures and nonabsorbable titanium staples cause.
MATERIALS AND METHODS
The study was initiated after approval by the Ethics Review Committee of the Faculty of Veterinary Medicine, University of Sarajevo. Wistar albino rats weighing 100g to 150g were kept under standard laboratory conditions before surgery, placed in freestanding cages, and acclimatized to standard laboratory conditions (temperature from 20C to 24C, 12 hours of light, 12 hours of dark, and the food was withdrawn for 24 hours before the surgery). Sixty rats were randomized into 3 groups: group I (endoloop) in which appendectomy was performed using endoloop ligature, group II (stapler) in which appendectomy was performed with the stapler, and group III (Hem-o-lok) in which appendectomy was performed using Hem-o-lok clips.
Surgical Procedure
After the rats were anesthetized with ketamine (50mg/kg), they were secured with an adhesive band and placed on the surgical table in the supine position. The abdomen of the animal was shaved and disinfected by povidone-iodine solution and dried with gauze. Laparotomy was performed using a median incision. The cecum, a dead-end pouch similar to the appendix in humans, was located and then dissected.
In group I (n=20), cecum (approximately 0.7 cm in length) was ligated with Vicryl 2-0 ligature (Vicryl, Ethicon) and divided (Figure 1).
Figure 1.
Endoloop on stump.
In group II (n=20), cecum was divided by using a 45-mm stapler (thick charge) (Ethicon, Endosurgery, Cincinnati, OH) (Figure 2).
Figure 2.
Stapler line on stump.
In group III (n=20), a Hem-o-lok XL clip (Hem-o-lock, Weck Closure Systems, Research Triangle Park, NC, USA) was attached to the cecum, and the distal part was divided (Figure 3).
Figure 3.
Hem-o-lok clip on stump.
Laparotomy and suturing of the skin was performed using a 3-0 continuous suture. No antibiotic treatment was used before, during, or after the experiment. During the entire observational period, all animals were controlled and underwent clinical examination to check local and systemic complications. On the 14th day and 28th day after the surgical procedures, 10 animals from each group were sacrificed, and the stump containing the clip, endoloop, and the staples was taken for histopathological evaluation.
Histopathological Procedure
Bioptical material was formalin fixed, paraffin embedded, and was cut into standard 5μ cuts and colored by applying according to the standard procedure for H&E (hematoxylin eosin) staining, and then mounted by using Canada balsam. Microscopic analysis was performed with an Olympus BX41 microscope.
Statistical Analysis
The Fisher exact probability test was used for the analysis of differences between distributions of histopathological changes. Differences were considered significant for p<0.05.
RESULTS
All the rats that we operated on exhibited a 100% survival rate accompanied by normal food and water intake. No other complications were observed, including infection of the wound, volvulus, intestinal obstruction, abscess, or wound dehiscence.
Histopathological Assessment
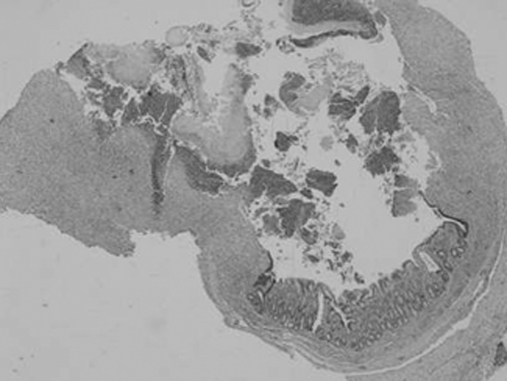
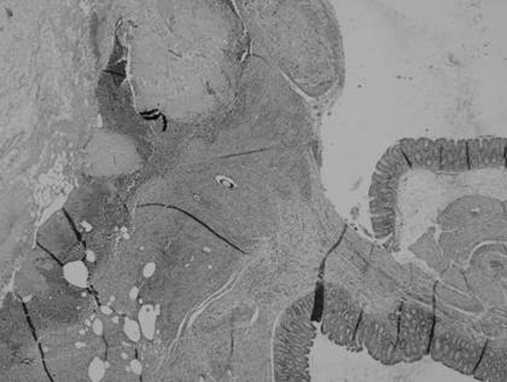
We analyzed the tissue reaction in the field just around the endoloop suture, staples, or the plastic clip. Under the light microscope, on the 14th postoperative day in group I (endoloop), moderate mucosal inflammation (4/10) was seen in general, with some erosions, ulcers, and granulation tissue with absceding necrotizing purulent inflammation on serosa and partly in muscular layer (3/10) (Figure 4).
Figure 4.
Endoloop 14th day: HEx4, moderate inflammation with erosions and ulcerations on the surface, with granulation tissue by type of absceding, necrotizing inflammation in the serosa and part of the muscular layer.
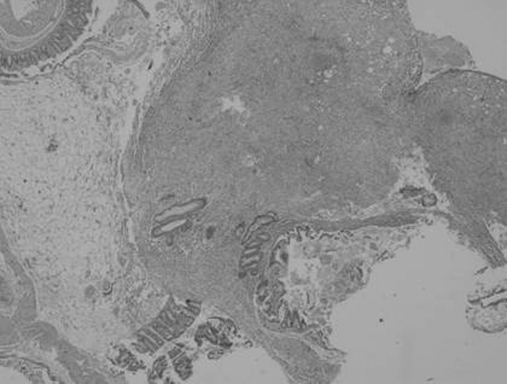
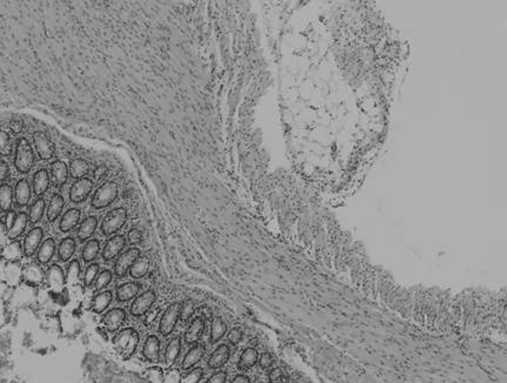
In group II (staples): moderate mucosal inflammation with granulation tissue in the serosa and partly in the muscular layer (7/10) was observed (Figure 5); in only one specimen absceding and necrotizing purulent inflammation was observed. In 3 specimens (3/10), there was some mild inflammation with minimal inflammatory infiltrating cells and edema.
Figure 5.
Stapler 14th day, HEx4: moderate dense inflammatory infiltrate, which partly eroded the mucosa, most of the serosa with nonspecific granulation tissue, and foreign body granuloma.
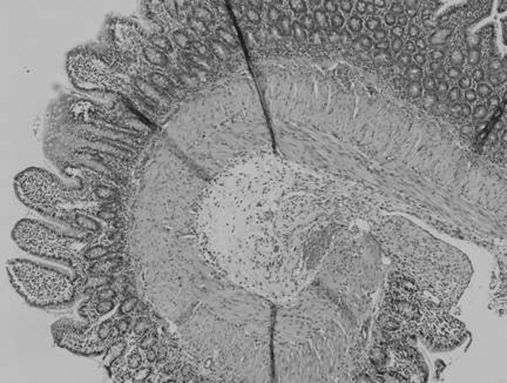
In group III (Hem-o-lok): moderate mucosal inflammation with granulation tissue and necrotizing inflammation on serosa was observed (6/10) accompanied by mild mucosal inflammation and granulation tissue (4/10) (Figure 6). In only one specimen, a cluster of siderophages was seen as a sign of old bleeding (Figure 7) and clearance of the affected area (Table 1).
Figure 6.
Hem-o-look 14th day, HEx4: nonspecific granulation tissue with moderate inflammatory infiltrate in the serosa.
Figure 7.
Hem-o-look 14th day, HEx4: absceding, partly necrotizing inflammation in serosa with small fields of bleeding.
Table 1.
Histopathological Findings of the Cecum and Stumps on the 14th Postoperative Day
| Degree of inflammation | Endoloop | Stapler | Hem-o-lok |
|---|---|---|---|
| Mild mucosal inflammation and granulation tissue | 2 | 3 | 4 |
| 1a | |||
| Ulcer and granulation tissue | 3 b | 0 | 0 |
| Moderate severe mucosal inflammation and granulation tissue on serosa | 4c | 1c | 3a |
| 6 | 3 |
With necrotizing purulent inflammation in serosa.
With tiny focus of fibrinoid necrosis on mucosa + necrotizing purulent inflammation on serosa.
With necrotizing, purulent inflammation in muscular layer and serosa.
The frequency of mild and moderate inflammation between endoloop, stapler, and Hem-o-lok groups was compared using Fisher's exact test. We did not identify a statistical significance in the frequency of mild (p=1) and moderate inflammation (endoloop-stapler, p=0.00036, Hem-o-lok-stapler, p = 1, endoloop-Hem-o-lok, p=0,656) or in ulcer and granulation tissue (endoloop-stapler, p=0.21, endoloop-Hem-o-lok, p=0.21.)
Bonferroni correction factor (multiplying the level of significance p by 3) was not used, because we could conclude without it that there was no statistical significance.
On the 28th postoperative day, we observed the following:
In group I (endoloop): moderate inflammation with granulation tissue with absceding inflammation in the serosa (Figure 8) and partly in the muscular layer (4/10), and signs of repair (6/10) were seen with foreign body reaction in almost all specimens.
Figure 8.
Endoloop 28th day: HEx4: moderate dense inflammatory infiltrate with granulation tissue in the serosa and abscess.
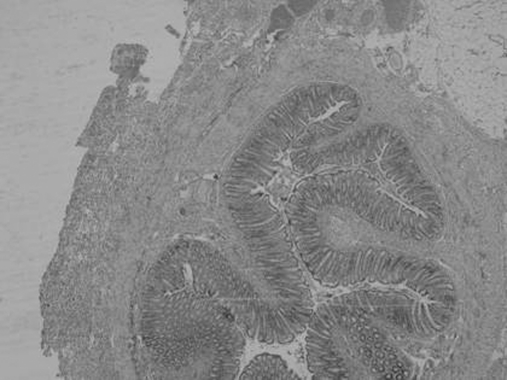
In group II (staples): the degree of inflammation in this phase varied from mild (8/10) (Figure 9) to moderate inflammation in the mucosa (1/10), while changes were more constant in the serosa, with foreign body reaction in 4 specimens (4/10). All of the above were of mild to moderate severity, uncomplicated tissue reaction to the damage.
Figure 9.
Stapler 28th day, HEx10: mild inflammation in the mucosa with focal mild fibrosis (almost normal wall).
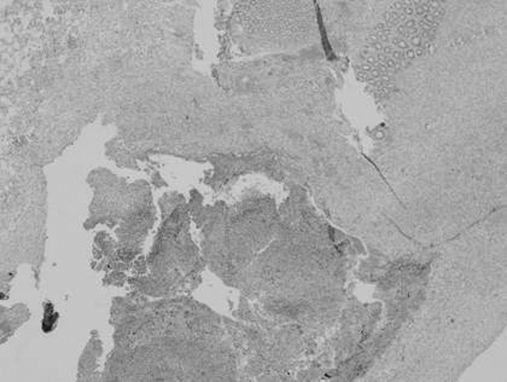
In group III (Hem-o-lok): moderate inflammation with signs of repair in the form of mild fibrosis and focal granulation tissue was seen (Figure 10), with foreign body reaction in 3 specimens (3/10) (Table 2).
Figure 10.
Hem-o-look 28th day, HEx10: moderate inflammation with signs of reparation in the form of mild fibrosis and focal granulation tissue.
Table 2.
Histopathological Findings of the Cecum and Stumps on the 28th Postoperative Day
| Degree of Inflammation | Endoloop | Stapler | Hem-o-lok |
|---|---|---|---|
| Mild mucosal inflammation | 0 | 6 | 1a |
| 3a | |||
| Ulcer and granulation tissue | 0 | 0 | 0 |
| Moderate severe mucosal inflammation and granulation tissue on serosa | 4b | 1 | 3d |
| 6c | 6b | ||
| Foreign body reaction | 10 | 4 | 3 |
With granulation tissue.
With abscess formation.
With signs or reparation in level of muscular layer and serosa.
With focal erosions and reparation in form of mild fibrosis.
Using Bonferroni correction factor, we identified a statistical significance in the frequency of mild and moderate inflammation when we compared the Endoloop-stapler (p=0.00036) and Hem-o-lok-stapler (p=0.0033) groups. There were no statistically significant differences when we compared endoloop with Hem-o-lok clip groups. We concluded from these data that mild and moderate inflammation is more frequent in endoloop and Hem-o-lok groups than in the stapler group.
With Bonferroni correction, a statistical significance was identified in the frequency of foreign body reaction between the endoloop and stapler groups (p=0.033) and endoloop and Hem-o-lok groups (p=0.009), but there were no statistically significant differences between the stapler and Hem-o-lok clip groups. Foreign body reaction is more frequent in the endoloop than in the stapler and Hem-o-lok groups.
DISCUSSION
Unlike the standard classical appendectomy procedure, different methods of securing the stump of the appendix during laparoscopic appendectomy have been reported.1,4 However, use of different materials may vary in terms of inflammation, foreign body reaction, or rate of infection in the surgical area. Generally speaking, tissues respond to sutures as they would to any foreign material. If the body's response to the suture is intense, the suture itself may be broken down, or the tissue surrounding the suture may be destroyed. The possible consequences of a severe tissue reaction include edematous and friable tissue that has less holding capacity for the sutures, infection that enhances the inflammatory response and dehiscence. It would be ideal to utilize a suture material that would induce minimal tissue responses.8,9
In the study of Kosan et al,10 in which they compared Vicryl (polyglactin 910), PDS (polydyoxanone), and chromed catgut sutures in the rat model, the lowest level of inflammation was seen in the PDS group. However, in our study the mildest reactive changes were seen on the 28th postoperative day in the stapler group. Staples are made of titanium, which elicits minimal tissue reaction.
The foreign body reactions, characterized by the formation of foreign body giant cells, encapsulation of the foreign object, and chronic inflammation,11 were significantly different depending on the method used for securing of the stump of the appendix; thus, the stapler and Hem-o-lok clips reduced its frequency. Foreign body reaction was correlated with the duration of suture absorption, developing at the end of the absorption processes.12 Thus, one way that we can explain the lower level of foreign body reaction to these materials is that both Hem-o-lok clips and titanium stapler line are nonabsorbable materials.
There is currently only one report of encountered foreign body reaction associated with stapled human gastrointestinal anastomoses.13 In a porcine model, minimal fibrosis around the titanium staples was reported with only an occasional foreign-body giant-cell reaction.14 However, Klein et al,15 in the study in which a rat model was used, reported that there were no significant differences in fibrous tissue formation between titanium and absorbable polymeric surgical clips at any time.
Our study is the first to evaluate the effects of Hem-o-lok clips on the intestine. We observed that Hem-o-lok clips caused a milder reaction than endoloop clips did. Although a precise comparison cannot be made because this study was performed in a rat model, the reaction in humans is generally similar to but less intense than that observed in experimental animals.16
An ideal suture would provide high tensile strength and knot security, resist infection and contamination, and react minimally with the tissue in which it is embedded.17 Differences between the degree of inflammation and foreign body reaction to different suture materials used in our study were statistically significant. We observed the lowest degree of inflammation and foreign body reaction in the stapler group. Considering our results, it may be prudent to declare that titanium staples that cause a milder tissue reaction may be advantageous as a method of securing the base of the appendix in laparoscopic appendectomy. However, this is just one aspect of its use; Hem-o-lok nonabsorbable plastic clips also exhibited a mild reaction phenotype, whilst their price and simplicity of application, would give them a strong advantage for use in laparoscopic appendectomy.5 We could conclude that “perfect” suture material may never become available, and that surgeons will have to examine each surgical problem and select the appropriate materials accordingly.18
Acknowledgments
We thank the scrub-nurses Ankica Sedlar and Albina Hrvanovic, from the University Clinic Center Tuzla, for support and assistance during the experimental part of this study, and also Esmir Bajric from the Faculty of Veterinary Medicine, University of Sarajevo, for his technical help.
Contributor Information
Samir Delibegović, Department of Surgery, University Clinic Center Tuzla, Bosnia and Herzegovina..
Ermina Iljazović, Department of Pathology, University Clinic Center Tuzla, Bosnia and Herzegovina..
Muhamed Katica, Faculty of Veterinary Medicine, University of Sarajevo, Bosnia and Herzegovina..
Anhel Koluh, Cantonal hospital Zenica, Zenica, Bosnia and Herzegovina..
References:
- 1. Neugebauer EAM, Troidl H, Kum CK, Eypasch E, Miserez M, Paul A. The EAES clinical practice guidelines on laparoscopic cholecystectomy, appendectomy, and hernia repair (1994). In: Neugebauer EAM, Sauerland S, Fingerhut A, Millat B, Buess G. eds. EAES Guidelines for Endoscopic Surgery. Berlin Heidelberg: Springer; 2006;265–289 [Google Scholar]
- 2. Beldi G, Vorburger SA, Bruegger LE, Kocher T, Inderbitzin D, Candinas D. Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg. 2006;93:1390–1393 [DOI] [PubMed] [Google Scholar]
- 3. Kazemier G, in't Hof KH, Saad S, Bonjer HJ, Sauerland S. Securing the appendiceal stump in laparoscopic appendectomy: evidence for routine stapling? Surg Endosc. 2006;20:1473–1476 [DOI] [PubMed] [Google Scholar]
- 4. Hanssen A, Plotnikov S, Dubois R. Laparoscopic appendectomy using a polymeric clip to close the appendicular stump. JSLS. 2007;11:59–62 [PMC free article] [PubMed] [Google Scholar]
- 5. Delibegović S, Matović E. Hem-o-lok plastic clips in securing of the base of the appendix during laparoscopic appendectomy. Surg Endosc. 2009;23:2851–2854 [DOI] [PubMed] [Google Scholar]
- 6. Baker SR. Wound closure techniques. In: Baker SR. Local Flaps in Facial Reconstruction. Mosby Elsevier; 2007;41–64 [Google Scholar]
- 7. Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Ann Surg. 1975;181:144–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stashak TS, Titurraspe DJ. Considerations for selection of suture materials. Vet Surg. 1978;7:48–55 [Google Scholar]
- 9. Varma S, Johnson LW, Ferguson HI, Lumb WV. Tissue reaction to non absorbable suture materials in infected surgical wounds - a histological evaluation. Am J Vet Res. 1981;42:563–570 [PubMed] [Google Scholar]
- 10. Kosan M, Gonulalan U, Ozturk B, Kulacoglu S, Erguder I, Akdemir O, Cetinkaya M. Tissue reactions of suture materials (polyglactine 910, chromed catgut and polydioxa-none) on rat bladder wall and their role in bladder stone formation. Urol Res. 2008;36:43–49 [DOI] [PubMed] [Google Scholar]
- 11. Anderson JM, Rodriguez, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20:86–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hanke PR, Timm P, Falk G, Kramer W. Behavior of different suture materials in the urinary bladder of the rabbit with special reference to wound healing, epithelization and crystallization. Urol Int. 1994;52:26–33 [DOI] [PubMed] [Google Scholar]
- 13. Lim CB, Goldin RD, Darzi A, Hanna GB. Characterization of materials eliciting foreign body reaction in stapled human gastrointestinal anastomoses. Br J Surg. 2008;95:1044–1050 [DOI] [PubMed] [Google Scholar]
- 14. Venkatesh R, Rehman J, Landman J, Lee D, Ragab EM, Sundaram PC. Determination of cell viability after laparoscopic tissue stapling in a porcine model. J Endourol. 2005;19:744–747 [DOI] [PubMed] [Google Scholar]
- 15. Klein RD, Jessup G, Ahari F, Connolly RJ, Schwaitzberg SD. Comparison of titanium and absorbable polymeric surgical clips for use in laparoscopic cholecystectomy. Surg Endosc. 1994;8:753–758 [DOI] [PubMed] [Google Scholar]
- 16. Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Ann Surg. 1975;144–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fossum TW. Biomaterials, suturing and hemostasis. In: Small Animal Surgery. St. Louis: Mosby Year Book; 1997;42–56 [Google Scholar]
- 18. Greenwaid D, Shumway S, Albear P, Gottlieb L. Mechanical comparison of ten suture materials before and after in vivo incubation. J Surg Res. 1994;56:372–377 [DOI] [PubMed] [Google Scholar]